Chromosomal Integration of HHV-6 in a Preterm Neonate: A Rare Case of Hyperleukocytosis and Clinical Implications
Abstract
1. Introduction
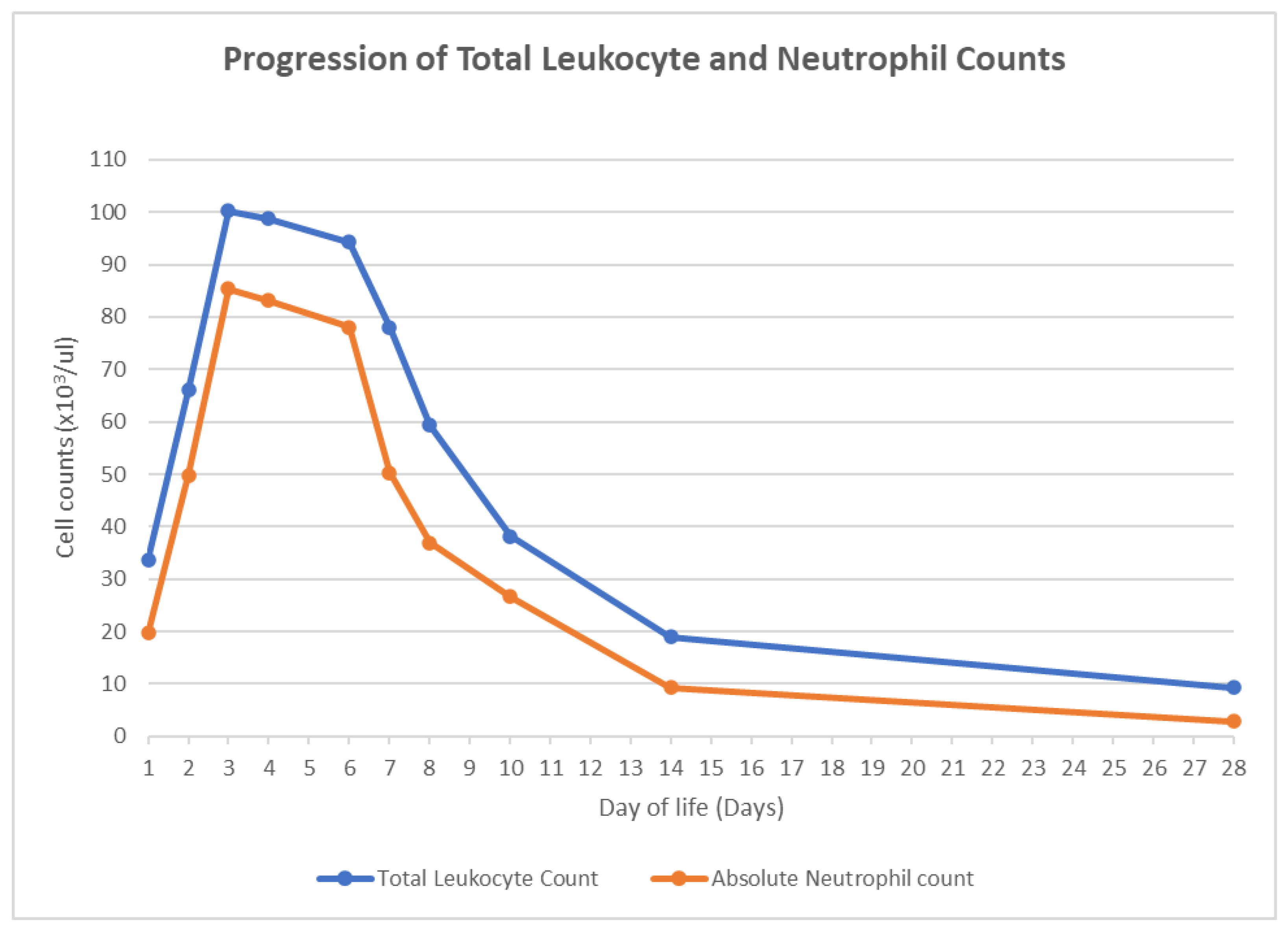
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ortega, L.; Ramzanali, S.; Mora, P.; Kaylani, S.-Z.; Adesanya, O. Extreme Hyperleukocytosis in an Extremely Preterm Infant. J. Rare Dis. Orphan Drugs 2022, 3, 6–10. [Google Scholar] [CrossRef]
- Jansen, E.; Emmen, J.; Mohns, T.; Donker, A. Extreme hyperleucocytosis of the premature. BMJ Case Rep. 2013, 2013, bcr2012008385. [Google Scholar] [CrossRef] [PubMed]
- Parvez, Y.; Mathew, A.G. Hyperleukocytosis in newborn: A diagnosis of concern. Indian J. Hematol. Blood Transfus. 2014, 30 (Suppl. S1), 131–132. [Google Scholar] [CrossRef] [PubMed]
- Sakka, V.; Tsiodras, S.; Giamarellos-Bourboulis, E.J.; Giamarellou, H. An update on the etiology and diagnostic evaluation of a leukemoid reaction. Eur. J. Intern. Med. 2006, 17, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Ablashi, D.; Agut, H.; Alvarez-Lafuente, R.; Clark, D.A.; Dewhurst, S.; DiLuca, D.; Flamand, L.; Frenkel, N.; Gallo, R.; Gompels, U.A.; et al. Classification of HHV-6A and HHV-6B as distinct viruses. Arch. Virol. 2014, 159, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Agut, H.; Bonnafous, P.; Gautheret-Dejean, A. Update on infections with human herpesviruses 6A, 6B, and 7. Med. Mal. Infect. 2017, 47, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Stone, R.C.; Micali, G.A.; Schwartz, R.A. Roseola infantum and its causal human herpesviruses. Int. J. Dermatol. 2014, 53, 397–403. [Google Scholar] [CrossRef]
- Zerr, D.M. Human Herpesvirus 6B in the Transplant Recipient: When to Worry, When to Act. J. Pediatric Infect. Dis. Soc. 2018, 7 (Suppl. S2), S75–S78. [Google Scholar] [CrossRef]
- Pantry, S.N.; Medveczky, P.G. Latency, Integration, and Reactivation of Human Herpesvirus-6. Viruses 2017, 9, 194. [Google Scholar] [CrossRef] [PubMed]
- Aimola, G.; Beythien, G.; Aswad, A.; Kaufer, B.B. Current understanding of human herpesvirus 6 (HHV-6) chromosomal integration. Antiviral Res. 2020, 176, 104720. [Google Scholar] [CrossRef] [PubMed]
- Kaufer, B.B.; Flamand, L. Chromosomally integrated HHV-6: Impact on virus, cell and organismal biology. Curr. Opin. Virol. 2014, 9, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.A. Clinical and laboratory features of human herpesvirus 6 chromosomal integration. Clin. Microbiol. Infect. 2016, 22, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.B.; Caserta, M.T.; Schnabel, K.; Shelley, L.M.; Marino, A.S.; Carnahan, J.A.; Yoo, C.; Lofthus, G.K.; McDermott, M.P. Chromosomal integration of human herpesvirus 6 is the major mode of congenital human herpesvirus 6 infection. Pediatrics 2008, 122, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Tanaka-Taya, K.; Sashihara, J.; Kurahashi, H.; Amo, K.; Miyagawa, H.; Kondo, K.; Okada, S.; Yamanishi, K. Human herpesvirus 6 (HHV-6) is transmitted from parent to child in an integrated form characterization of cases with chromosomally integrated HHV-6 DNA. J. Med. Virol. 2004, 73, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kosugi, S.; Koide, R.; Kawamura, Y.; Ito, J.; Miura, H.; Matoba, N.; Matsuzaki, M.; Fujita, M.; Kamada, A.J.; et al. Endogenization and excision of human herpesvirus 6 in human genomes. PLoS Genet. 2020, 16, e1008915. [Google Scholar] [CrossRef] [PubMed]
- Flamand, L.; Komaroff, A.L.; Arbuckle, J.H.; Medveczky, P.G.; Ablashi, D.V. Review, part 1: Human herpesvirus-6-basic biology, diagnostic testing, and antiviral efficacy. J. Med. Virol. 2010, 82, 1560–1568. [Google Scholar] [CrossRef] [PubMed]
| Laboratory Test | Day of Life (DOL) Collected | Laboratory Value |
|---|---|---|
| CSF HHV-6 PCR | DOL 4 | 1600 copies/mL |
| Plasma/Serum HHV-6 PCR | DOL 7 | 470,000 copies/mL |
| Whole-Blood HHV-6 PCR | DOL 7 | 5,500,000 copies/mL |
| Whole-Blood HHV-6 DNA Copies to Nucleated Cell Count Ratio | DOL 7 | 0.96 |
| Serum HHV-6 IgG | DOL 7 | Positive |
| Serum HHV-6 IgM | DOL 7 | Negative |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balasundaram, P.; Sakr, M. Chromosomal Integration of HHV-6 in a Preterm Neonate: A Rare Case of Hyperleukocytosis and Clinical Implications. Pediatr. Rep. 2024, 16, 432-437. https://doi.org/10.3390/pediatric16020037
Balasundaram P, Sakr M. Chromosomal Integration of HHV-6 in a Preterm Neonate: A Rare Case of Hyperleukocytosis and Clinical Implications. Pediatric Reports. 2024; 16(2):432-437. https://doi.org/10.3390/pediatric16020037
Chicago/Turabian StyleBalasundaram, Palanikumar, and Mohamed Sakr. 2024. "Chromosomal Integration of HHV-6 in a Preterm Neonate: A Rare Case of Hyperleukocytosis and Clinical Implications" Pediatric Reports 16, no. 2: 432-437. https://doi.org/10.3390/pediatric16020037
APA StyleBalasundaram, P., & Sakr, M. (2024). Chromosomal Integration of HHV-6 in a Preterm Neonate: A Rare Case of Hyperleukocytosis and Clinical Implications. Pediatric Reports, 16(2), 432-437. https://doi.org/10.3390/pediatric16020037







