Postoperative Cast Immobilization Might Be Unnecessary after Pelvic Osteotomy for Children with Developmental Hip Dysplasia: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Article Selection and Methodological Quality
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
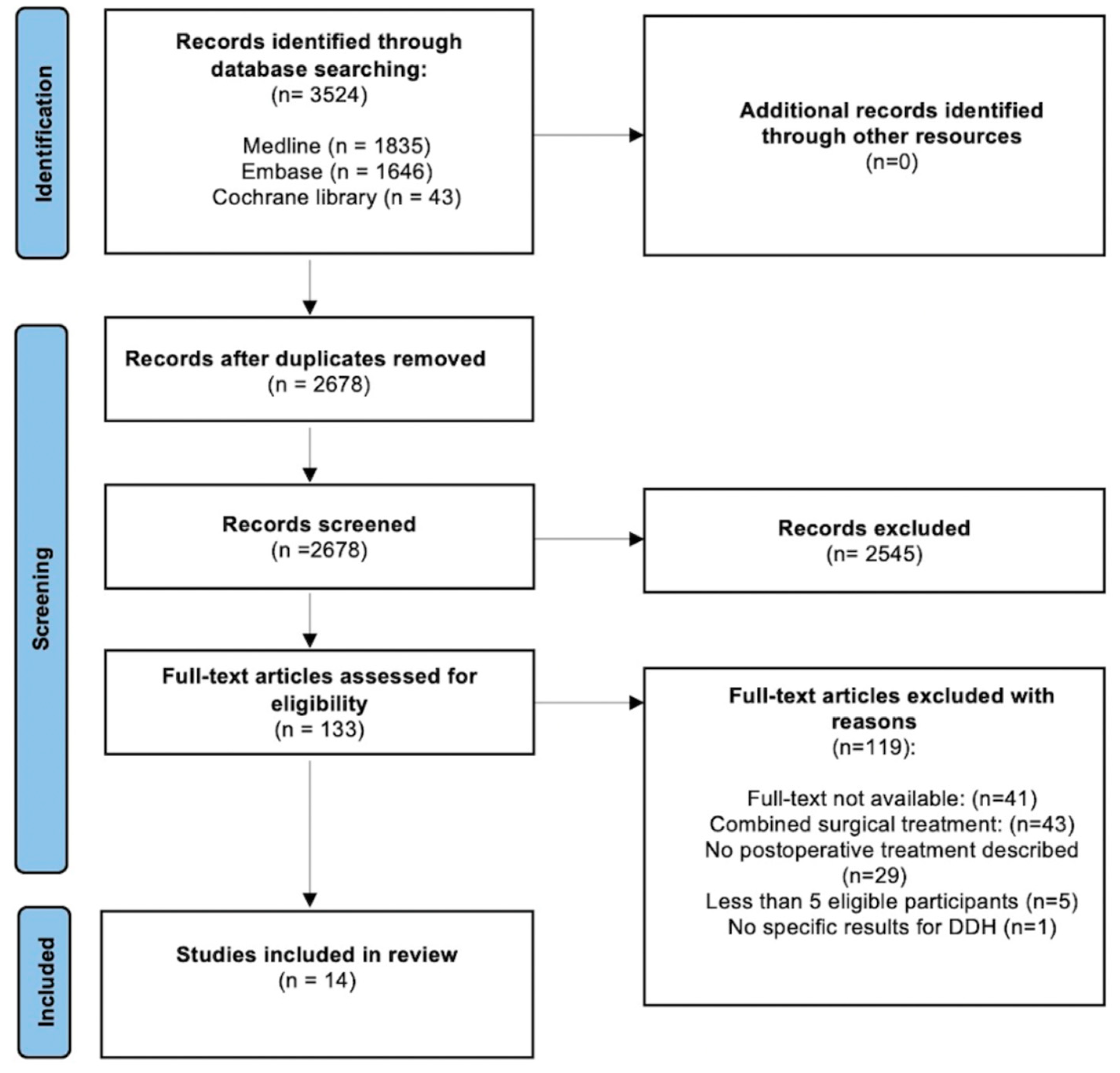
3.1. Literature Search Process
3.2. Study Characteristics and Methodological Quality
3.3. Surgical Treatment
3.4. Postoperative treatment
3.5. Clinical Outcomes
3.6. Complications
3.7. Radiological Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| Pubmed: | |
| #1 | ((Osteotomy[Mesh:NoExp] OR osteom*[tiab] AND (hip[tiab] OR pelvi*[tiab] OR acetabul*[tiab])) OR “Acetabuloplasty”[Mesh] OR Acetabuloplast*[tiab] OR “acetabulum plasty”[tiab] OR Salter[tiab] OR Pemberton[tiab] OR Dega[tiab] OR “hip reconstruction*”[tiab] NOT arthroplast*[tiab] |
| #2 | “Developmental Dysplasia of the Hip”[Mesh] OR “Hip Dislocation, Congenital”[Mesh] OR DDH[tiab] OR ((hip[tiab]) AND (dislocat*[tiab] OR luxation[tiab] OR dysplasia[tiab] OR displacement[tiab] AND (congenital[tiab] OR development[tiab])) |
| Embase: | |
| #1 | ‘Pelvis osteotomy’/de OR ((osteotom*:ti,ab,kw) AND (hip:ti,ab,kw OR pelvi*:ti,ab,kw OR acetabul*:ti,ab,kw)) OR ‘acetabuloplasty’/exp OR acetabuloplast*:ti,ab,kw OR ‘acetabulum plasty’:ti,ab,kw OR Salter:ti,ab,kw OR Pemberton:ti,ab,kw, OR Dega:ti,ab,kw OR ‘hip reconstruction’:ti,ab,kw NOT arthroplast*”ti,ab,kw |
| #2 | ‘Hip dysplasia’/exp OR ‘congenital hip dislocation’/exp OR ddh:ti,ab,kw OR ((hip:ti,ab,kw) AND (dislocat*:ti,ab,kw OR luxation:ti,ab,kw OR dysplasia:ti,ab,kw OR displacement:ti,ab,kw) AND (congenital:ti,ab,kw OR developmental:ti,ab,kw)) |
| #3 | NOT ‘conference abstract’/it |
| Cochrane: | |
| #1 | ((Osteotom*:ti,ab,kw) AND (hip:ti,ab,kw OR pelvi*:ti,ab,kw OR acetabul*:ti,ab,kw)) OR acetabuloplast*:ti,ab,kw OR “acetabulum plasty”:ti,ab,kw OR Salter:ti,ab,kw OR Pemberton:ti,ab,kw OR Dega:ti,ab,kw OR “hip reconstruction”:ti,ab,kw NOT artrhoplast*:ti,ab,kw |
| #2 | DDH:ti,ab,kw OR ((hip:ti,ab,kw) AND (dislocat*:ti,ab,kw OR luxation:ti,ab,kw OR dysplasia:ti,ab,kw OR displacement:ti,ab,kw) AND (congenital:ti,ab,kw OR developmental:ti,ab,kw)) |
References
- de Witte, P.B.; van Bergen, C.J.; de Geest, B.L.; Willeboordse, F.; van Linge, J.H.; den Hartog, Y.M.; Foreman-van Drongelen, M.; Pereboom, R.M.; Robben, S.G.F.; Burger, B.J.; et al. Treatment of decentered developmental dysplasia of the hip under the age of 1 year: An evidence-based clinical practice guideline—Part 2. EFORT Open Rev. 2022, 7, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Kotlarsky, P.; Haber, R.; Bialik, V.; Eidelman, M. Developmental dysplasia of the hip: What has changed in the last 20 years? World J. Orthop. 2015, 6, 886–901. [Google Scholar] [CrossRef] [PubMed]
- Hauk, L. Developmental Dysplasia of the Hip in Infants: A Clinical Report from the AAP on Evaluation and Referral. Am. Fam. Physician 2017, 96, 196–197. [Google Scholar] [PubMed]
- van Bergen, C.J.; de Witte, P.B.; Willeboordse, F.; de Geest, B.L.; Foreman-van Drongelen, M.; Burger, B.J.; den Hartog, Y.M.; van Linge, J.H.; Pereboom, R.M.; Robben, S.G.F.; et al. Treatment of centered developmental dysplasia of the hip under the age of 1 year: An evidence-based clinical practice guideline—Part 1. EFORT Open Rev. 2022, 7, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Fillingham, Y.A.; Erickson, B.J.; Hellman, M.D.; Cvetanovich, G.; Kogan, M. Surgical Technique: Pavlik Harness and Closed Reduction for Developmental Dysplasia of the Hip. In Hip Arthroscopy and Hip Joint Preservation Surgery; Nho, S., Leunig, M., Larson, C., Bedi, A., Kelly, B., Eds.; Springer: New York, NY, USA, 2014; pp. 415–428. [Google Scholar]
- Pisecky, L.; Großbötzl, G.; Gahleitner, M.; Haas, C.; Gotterbarm, T.; Klotz, M.C. Results after Spica cast immobilization following hip reconstruction in 95 cases: Is there a need for alternative techniques? Arch. Orthop. Trauma Surg. 2021, 142, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Schams, M.; Labruyère, R.; Zuse, A.; Walensi, M. Diagnosing developmental dysplasia of the hip using the Graf ultrasound method: Risk and protective factor analysis in 11,820 universally screened newborns. Eur. J. Pediatr. 2017, 176, 1193–1200. [Google Scholar] [CrossRef]
- Ionescu, A.; Dragomirescu, M.-C.; Herdea, A.; Ulici, A. Developmental Dysplasia of the Hip: How Many Risk Factors Are Needed? Children 2023, 10, 968. [Google Scholar] [CrossRef]
- Zhang, S.; Doudoulakis, K.J.; Khurwal, A.; Sarraf, K.M. Developmental dysplasia of the hip. Br. J. Hosp. Med. 2020, 81, 1–8. [Google Scholar] [CrossRef]
- Vaquero-Picado, A.; González-Morán, G.; Gil Garay, E.; Moraleda, L. Developmental dysplasia of the hip: Update of management. EFORT Open Rev. 2019, 4, 548–556. [Google Scholar] [CrossRef]
- Alassaf, N. Treatment of developmental dysplasia of the hip (DDH) between the age of 18 and 24 months. Eur. J. Orthop. Surg. Traumatol. 2019, 30, 637–641. [Google Scholar] [CrossRef]
- Venkatadass, K.; Prasad, V.D.; Al Ahmadi, N.M.M.; Rajasekaran, S. Pelvic osteotomies in hip dysplasia: Why, when and how? EFORT Open Rev. 2022, 7, 153–163. [Google Scholar] [CrossRef]
- Abdullah, E.-S.A.H.; Razzak, M.Y.A.; Hussein, H.T.K.; El-Adwar, K.L.; Abdel-Razek Youssef, A. Evaluation of the results of operative treatment of hip dysplasia in children after the walking age. Alex. J. Med. 2012, 48, 115–122. [Google Scholar] [CrossRef]
- Feeley, I.H.; Green, C.J.; Rowan, F.E.; Moore, D.P. International variance in the treatment of developmental dysplasia of the hip. J. Child. Orthop. 2014, 8, 381–386. [Google Scholar] [CrossRef]
- Pisecky, L.; Großbötzl, G.; Gahleitner, M.; Stadler, C.; Stevoska, S.; Haas, C.; Gotterbarm, T.; Klotz, M.C.M. Foam Splint versus Spica Cast—Early Mobilization after Hip Reconstructive Surgery in Children—Preliminary Data from a Prospective Randomized Clinical Trial. Children 2022, 9, 288. [Google Scholar] [CrossRef]
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Prill, R.; Karlsson, J.; Ayeni, O.R.; Becker, R. Author guidelines for conducting systematic reviews and meta-analyses. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2739–2744. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.; Phillips, M. Rayyan for systematic reviews. J. Electron. Resour. Libr. 2018, 30, 46–48. [Google Scholar] [CrossRef]
- Reiswig, J. Mendeley. J. Med. Libr. Assoc. 2010, 98, 193–194. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Kwong, J.S.; Zhang, C.; Li, S.; Sun, F.; Niu, Y.; Du, L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef]
- Mckay, D. A Comparison of the Innominate and the Pericapsular Osteotomy in the Treatment of Congenital Dislocation of the Hip. Clin. Orthop. Relat. Res. 1974, 98, 124–132. [Google Scholar] [CrossRef]
- Trevor, D.; Johns, D.; Fixsen, J. Acetabuloplasty in the treatment of congenital dislocation of the hip. J. Bone Jt. Surg. Br. 1975, 57, 167–174. [Google Scholar] [CrossRef]
- Akman, B.; Ozkan, K.; Cift, H.; Akan, K.; Eceviz, E.; Eren, A. Treatment of Tönnis type II hip dysplasia with or without open reduction in children older than 18 months: A preliminary report. J. Child. Orthop. 2009, 3, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Aksoy, C.; Yilgor, C.; Demirkiran, G.; Caglar, O. Evaluation of a 308 cetabular development after Dega acetabuloplasty in developmental dysplasia of the hip. J. Pediatr. Orthop. 2013, 22, 91–95. [Google Scholar] [CrossRef]
- Chukwunyerenwa, C.K.; Sehgal, R.; Vioreanu, M.; Doyle, F.; Molony, D.; McCormack, D. Less invasive innominate osteotomy. J. Pediatr. Orthop. 2010, 19, 318–322. [Google Scholar] [CrossRef]
- Ezirmik, N.; Yildiz, K. Advantages of single-stage surgical treatment with Salter innominate osteotomy and Pemberton Pericapsular osteotomy for developmental dysplasia of both hips. J. Int. Med. Res. 2012, 40, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Hedelin, H.; Larnert, P.; Hebelka, H.; Brisby, H.; Lagerstrand, K.; Laine, T. Innominate Salter osteotomy using resorbable screws: A retrospective case series and presentation of a new concept for fixation. J. Child. Orthop. 2019, 13, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Kamegaya, M.; Shinohara, Y.; Shinada, Y.; Moriya, H.; Koizumi, W.; Tsuchiya, K. The use of a hydroxyapatite block for innominate osteotomy. J. Bone Jt. Surg. Br. 1994, 76, 123–126. [Google Scholar] [CrossRef]
- Nakamura, Y.; Kimura, M.; Ohishi, H.; Kishiya, M.; Toh, S. Salter innominate osteotomy using T-saw for developmental dysplasia of the hip. Curr. Orthop. Pract. 2011, 22, 447–450. [Google Scholar] [CrossRef]
- Rampal, V.; Klein, C.; Arellano, E.; Boubakeur, Y.; Seringe, R.; Glorion, C.; Wicart, P. Outcomes of modified Dega acetabuloplasty in acetabular dysplasia related to developmental dislocation of the hip. Orthop. Traumatol. Surg. Res. 2014, 100, 207–211. [Google Scholar] [CrossRef][Green Version]
- Synder, M.; Forlin, E.; Xin, S.; Bowen, J.R. Results of the KALAMCHI modification of Salter osteotomy in the treatment of developmental dysplasia of the hip. J. Pediatr. Orthop. 1992, 12, 449–453. [Google Scholar] [CrossRef]
- Vedantam, R.; Capelli, A.M.; Schoenecker, P.L. Pemberton osteotomy for the treatment of developmental dysplasia of the hip in older children. J. Pediatr. Orthop. 1998, 18, 254–258. [Google Scholar] [CrossRef]
- Wada, A.; Fujii, T.; Takamura, K.; Yanagida, H.; Taketa, M.; Nakamura, T. Pemberton osteotomy for developmental dysplasia of the hip in older children. J. Pediatr. Orthop. 2003, 23, 508–513. [Google Scholar] [CrossRef]
- Wang, C.-W.; Wu, K.-W.; Wang, T.-M.; Huang, S.-C.; Kuo, K.N. Comparison of 333 acetabular anterior coverage after Salter osteotomy and Pemberton acetabuloplasty: A long-term followup. Clin. Orthop. Relat. Res. 2014, 472, 1001–1009. [Google Scholar] [CrossRef][Green Version]
- Wada, A.; Sakalouski, A.; Nakamura, T.; Kubota, H.; Matsuo, A.; Taketa, M.; Nakura, A.; Lee, Y. Angulated Salter osteotomy in the treatment of developmental dysplasia of the hip. J. Pediatr. Orthop. 2021, 31, 254–259. [Google Scholar] [CrossRef]
- Shin, C.H.; Yoo, W.J.; Park, M.S.; Kim, J.H.; Choi, I.H.; Cho, T.-J. Acetabular Remodeling and Role of Osteotomy After Closed Reduction of Developmental Dysplasia of the Hip. J. Bone Jt. Surg. 2016, 98, 952–957. [Google Scholar] [CrossRef]
- Salter, R. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J. Bone Jt. Surg. Br. 1961, 43, 518–539. [Google Scholar] [CrossRef]
- Gather, K.S.; von Stillfried, E.; Hagmann, S.; Müller, S.; Dreher, T. Outcome after early mobilization following hip reconstruction in children with developmental hip dysplasia and luxation. World J. Pediatr. 2018, 14, 176–183. [Google Scholar] [CrossRef]
- Miller, F.; Girardi, H.; Lipton, G.; Ponzio, R.; Klaumann, M.; Dabney, K.W. Reconstruction of the Dysplastic Spastic Hip with Peri-ilial Pelvic and Femoral Osteotomy Followed by Immediate Mobilization. J. Pediatr. Orthop. 1997, 17, 592–602. [Google Scholar] [CrossRef]
| Study Authors | Study Design | Number of Hips | Mean Age in Months at Treatment (Range) | Mean Follow-Up in Months (Range) | MINORS |
|---|---|---|---|---|---|
| Akman et al. [23] | Prospective | 15 | 22.4 (N.R.) | 48.8 (N.R.) | 9/24 |
| |15 of 47 hips valid| | |||||
| |Surgical technique: Salter| | |||||
| |Postoperative treatment: hip spica cast 6–8 weeks, afterwards abduction orthosis 3 months| | |||||
| |Male: Female (2:13)| | |||||
| Aksoy et al. [24] * | Retrospective | 23 | 32.7 (18.0–63.0) | 41.7 (12.0–107.0) | 5/16 |
| |23 of 35 hips valid| | |||||
| |Surgical technique: Dega| | |||||
| |Postoperative treatment: hip spica cast| | |||||
| |Male: Female (5:18)| | |||||
| Chukwunyerenwa et al. [25] | Retrospective | 49 | 24.0 (18.0–54.0) | 24.0 (12.0–60.0) | 8/16 |
| |49 of 49 hips valid| | |||||
| |Surgical technique: Less invasive Salter| | |||||
| |Postoperative treatment: abduction brace 6 weeks| | |||||
| |Male: Female (3:46)| | |||||
| Ezirmik et al. [26] | Retrospective | 110 | 23.0 (N.R.) | 70.7 (N.R.) | 10/24 |
| |110 of 220 hips valid| | |||||
| |Surgical technique: Salter; Pemberton| | |||||
| |Postoperative treatment: spica cast 6 weeks| | |||||
| |Male: Female (5:50)| | |||||
| |Hospitalization: 11.5 days| | |||||
| Hedelin et al. [27] | Retrospective | 7 | 68.4 (43.2–134.4) | N.R. | 7/16 |
| |7 of 21 hips valid| | |||||
| |Surgical technique: Salter| | |||||
| |Postoperative treatment: avoidance full weightbearing (n = 6); spica cast (n = 1); 6 weeks| | |||||
| |Male: Female (1:7)| | |||||
| |Hospitalization: 7 days| | |||||
| Kamegaya et al. [28] | Prospective | 13 | 56.7 (26.0–69.0) | 28.8 (12.0–47.0) | 7/24 |
| |13 of 19 hips valid| | |||||
| |Surgical technique: Salter| | |||||
| |Postoperative treatment: hip spica cast 6 weeks| | |||||
| |Male: Female (1:12)| | |||||
| Nakamura et al. [29] | Prospective | 8 | 63.6 (36.0–84.0) | 34.0 (3.0–72.0) | 3/16 |
| |8 of 8 hips valid| | |||||
| |Surgical technique: Salter| | |||||
| |Postoperative treatment: 1 ½ leg Spica 4–6 weeks| | |||||
| |Male: Female (1:7)| | |||||
| Rampal et al. [30] | Retrospective | 7 | 41.16 (24.0–72.0) | 84.0 (N.R.) | 7/16 |
| |7 of 16 hips valid| | |||||
| |Surgical technique: modified Dega| | |||||
| |Postoperative treatment: hip spica cast 6 weeks| | |||||
| |Male: Female (N.R.) | |||||
| Synder et al. [31] | Retrospective | 10 | 55.4 (37.2–74.4) | 37.68 (24.0–72.0) | 9/24 |
| |10 of 30 hips valid| | |||||
| |Surgical technique: Kalamchi Salter| | |||||
| |Postoperative treatment: spica 6–8 weeks, afterwards physical therapy| | |||||
| |Male: Female (3:7)| | |||||
| Vendantam et al. [32] | Retrospective | 5 | 116.4 (97.0–161.0) | 71.2 (28.0–100.0) | 6/16 |
| |5 of 16 hips valid| | |||||
| |Surgical technique: Pemberton| | |||||
| |Postoperative treatment: spica 6 weeks| | |||||
| |Male: Female (N.R.)| | |||||
| Wada et al. [33] | Retrospective | 5 | 106.56 (85.2–122.4) | 121.2 (97.2–141.6) | 5/16 |
| |5 of 17 hips valid| | |||||
| |Surgical technique: Pemberton| | |||||
| |Postoperative treatment: hip spica cast 3–4 weeks, afterwards physical therapy| | |||||
| |Male: Female(0:5)| | |||||
| Wang et al. [34] | Retrospecitve | 42 | 12/24 | ||
| |42 of 42 hips valid| | |||||
| |Surgical technique: Salter; Pemberton| | |||||
| |Postoperative treatment: 1 ½ spica 6 weeks| | |||||
| Salter: n = 14 | 19.2 (N.R.) | 264.0 (N.R.) | |||
| |Male: Female (0:14)| | |||||
| Pemberton: n = 28 | 20.4 (N.R.) | 192.0 (N.R.) | |||
| |Male: Female (5:23)| | |||||
| Wada et al. [35] * | Retrospective | 61 | 8/24 | ||
| |61 of 61 hips valid| | |||||
| |Surgical technique: (Angulated) Salter osteotomy (ASO; SO)| | |||||
| |Postoperative treatment: 1 ½ hip spica cast 5 weeks| | |||||
| Angulated Salter: n = 41 | 64.8 (50.4–94.8) | 39.6 (13.2–80.4) | |||
| |Male: Female (2:39)| | |||||
| |Spica hip abduction and flexion 10–20 degrees| | |||||
| Salter: n = 20 | 64.8 (34.8–81.6) | 34.8 (27.6–42.0) | |||
| |Male: Female (2:18)| | |||||
| |Spica hip abduction and flexion 10–20 degrees| | |||||
| Shin et al. [36] ** | Retrospective | 12 | 12/24 | ||
| |12 of 84 hips valid| | |||||
| |Surgical technique: Salter; Pemberton; Dega| | |||||
| |Postoperative treatment: hips spica cast| | |||||
| Salter: n = 4 | 34.8 (26.0–58.0) | 176.3 (157.0–204.0) | |||
| |Spica hip abduction 25–45° and flexion 40–70°| | |||||
| |Male: Female (2:2)| | |||||
| Pemberton: n = 3 | 28.7 (24.0–31.0) | 196.3 (112.0–253.0) | |||
| |Spica hip abduction and flexion N.R.| | |||||
| |Male: Female (1:2)| | |||||
| Dega: n = 5 | 35.8 (27.0–53.0) | 93.2 (71.0–106.0) | |||
| |Spica hip abduction 30° and flexion 30°| | |||||
| |Male: Female (0:5)| |
| Salter | Pemberton | Dega | Total | |
|---|---|---|---|---|
| Hip spica cast [23,24,26,27,28,29,30,31,32,33,34,35,36] (n = 312) | ||||
| Clinical outcomes | ||||
| McKay’s criteria | ||||
| Excellent | n = 59 (18.9%) | n = 64 (20.5%) | N/A | n = 123 (91.1%) |
| Good | n = 6 (1.9%) | n = 6 (1.9%) | N/A | n = 12 (8.9%) |
| Trevor clinical score | ||||
| Excellent | n = 53 (17%) | n = 53 (17%) | N/A | n = 106 (96.4%) |
| Good | n = 2 (0.6%) | n = 2 (0.6%) | N/A | n = 4 (3.6%) |
| Complications | ||||
| AVN | n = 14 * (4.5%) | n = 23 * (7.4%) | n = 1 (0.3%) | n = 49 * (15.7%) |
| Pain | n = 6 (1.9%) | n = 28 (9.0%) | N.R. | n = 34 (10.9%) |
| Fracture | N.R. | N.R. | n = 1 (0.3%) | n = 1 (0.3%) |
| Loss of hip position | n = 1 (0.3%) | N.R. | N.R. | n = 1 (0.3%) |
| Greater trochanteric overriding | N.R. | N.R. | n = 1 (0.3%) | n = 1 (0.3%) |
| Superficial infections | N.S. * | N.S. * | N.R. | n = 3 * (1.0%) |
| Graft displacements | N.R. | N.R. | N.R. | N.R. |
| Radiological outcome | ||||
| Severin score * | ||||
| I | n = 52 (17%) | n = 53 (17%) | n = 4 (1.3%) | n = 109 (76.8%) |
| II | n = 13 (4.2%) | n = 5 (1.6%) | n = 1 (0.3%) | n = 19 (13.4%) |
| III | n = 4 (1.3%) | n = 6 (1.9%) | n = 10 (7.0%) | |
| IV | n = 4(1.3%) | n = 4 (2.8%) | ||
| Abduction brace [25] (n = 49) | ||||
| Clinical outcomes | ||||
| Satisfaction with postoperative treatment | All parents and children were satisfied | N/A | N/A | n = 49 (100%) |
| Complications | N/A | N/A | ||
| AVN | n = 0 | |||
| Pain | n = 0 | |||
| Fracture | n = 0 | |||
| Loss of hip position | n = 0 | |||
| Greater trochanteric overriding | n = 0 | |||
| Superficial infections | n = 2 (4.1%) | n = 2 (4.1%) | ||
| Graft displacements | n = 0 | |||
| Radiological outcome | N/A | N/A | N/A | N/A |
| Severin score | ||||
| Avoidance of weightbearing [27] (n = 6) | ||||
| Clinical outcomes | N/A | N/A | N/A | N/A |
| Complications | N/A | N/A | N/A | |
| AVN | n = 0 | |||
| Pain | n = 0 | |||
| Fracture | n = 0 | |||
| Loss of hip position | n = 0 | |||
| Greater trochanteric overriding | n = 0 | |||
| Superficial infections | n = 0 | |||
| Graft displacements | n = 0 | |||
| Radiological outcomes | N/A | N/A | N/A | N/A |
| Severin score |
| Radiological Acetabular Correction | Salter | Dega | ||
|---|---|---|---|---|
| Hip Spica Cast [27,30] n = 8 | Abduction Brace [25] n = 49 | Avoidance of Weightbearing [27] n = 6 | Hip Spica Cast [24,30] n = 30 | |
| Mean preoperative AI | 30.5° | 35.1° | 26.3° | 32.8° |
| Mean first postoperative AI | 20.3° | 18.4° | 14.2° | 18.8° |
| Mean final postoperative AI | 12.4° | 14.9° | 12.2° | 12.7° |
| Mean preoperative CEA | 8.8° | N/A | 14.5° | 7.7° |
| Mean first postoperative CEA | 25.4° | N/A | 24.7° | 23.7° |
| Mean final postoperative CEA | 29.9° | N/A | 28.5° | 28.7° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mai, M.; van Stralen, R.A.; Moerman, S.; van Bergen, C.J.A. Postoperative Cast Immobilization Might Be Unnecessary after Pelvic Osteotomy for Children with Developmental Hip Dysplasia: A Systematic Review. Surg. Tech. Dev. 2024, 13, 9-21. https://doi.org/10.3390/std13010002
Mai M, van Stralen RA, Moerman S, van Bergen CJA. Postoperative Cast Immobilization Might Be Unnecessary after Pelvic Osteotomy for Children with Developmental Hip Dysplasia: A Systematic Review. Surgical Techniques Development. 2024; 13(1):9-21. https://doi.org/10.3390/std13010002
Chicago/Turabian StyleMai, Mohamed, Renée A. van Stralen, Sophie Moerman, and Christiaan J. A. van Bergen. 2024. "Postoperative Cast Immobilization Might Be Unnecessary after Pelvic Osteotomy for Children with Developmental Hip Dysplasia: A Systematic Review" Surgical Techniques Development 13, no. 1: 9-21. https://doi.org/10.3390/std13010002
APA StyleMai, M., van Stralen, R. A., Moerman, S., & van Bergen, C. J. A. (2024). Postoperative Cast Immobilization Might Be Unnecessary after Pelvic Osteotomy for Children with Developmental Hip Dysplasia: A Systematic Review. Surgical Techniques Development, 13(1), 9-21. https://doi.org/10.3390/std13010002








