-
 Impact of Peritoneal Closure on Inguinal Hernia Incidence After Robot-Assisted Radical Prostatectomy
Impact of Peritoneal Closure on Inguinal Hernia Incidence After Robot-Assisted Radical Prostatectomy -
 Surgeon Training in the Era of Computer-Enhanced Simulation Robotics and Emerging Technologies: A Narrative Review
Surgeon Training in the Era of Computer-Enhanced Simulation Robotics and Emerging Technologies: A Narrative Review -
 Laparoscopic-Assisted Percutaneous Cryoablation of Abdominal Wall Desmoid Fibromatosis: Case Series and Local Experience
Laparoscopic-Assisted Percutaneous Cryoablation of Abdominal Wall Desmoid Fibromatosis: Case Series and Local Experience
Journal Description
Surgical Techniques Development
Surgical Techniques Development
is an international, peer-reviewed, open access journal on the latest progressive techniques and advanced technologies in the field of surgeries, published quarterly online by MDPI (from Volume 11, Issue 1 - 2022). The Italian Association of Aesthetic Plastic Surgery (AICPE) is affiliated with Surgical Techniques Development and its members receive discounts on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Embase, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 30.3 days after submission; acceptance to publication is undertaken in 4.9 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
0.3 (2024)
Latest Articles
Clinical Outcomes After Endoscopic Retrograde Cholangiopancreatography Using Balloon-Assisted Enteroscopy for Benign Anastomotic Stricture of Choledochojejunostomy: A Retrospective Study
Surg. Tech. Dev. 2025, 14(3), 24; https://doi.org/10.3390/std14030024 - 23 Jul 2025
Abstract
►
Show Figures
Background/Objectives: Benign choledochojejunal anastomotic stricture (CJS) is a major late adverse event (AE) after choledochojejunostomy. An endoscopic method using balloon-assisted enteroscopy endoscopic retrograde cholangiopancreatography (BAE-ERCP) was recently developed for CJS. Methods: We retrospectively reviewed 45 patients (98 cases) who underwent BAE-ERCP
[...] Read more.
Background/Objectives: Benign choledochojejunal anastomotic stricture (CJS) is a major late adverse event (AE) after choledochojejunostomy. An endoscopic method using balloon-assisted enteroscopy endoscopic retrograde cholangiopancreatography (BAE-ERCP) was recently developed for CJS. Methods: We retrospectively reviewed 45 patients (98 cases) who underwent BAE-ERCP for benign CJS. The primary endpoint was the success rate of ERCP. The secondary endpoints were AEs and the recurrence rate of benign CJS. Results: ERCP was successful in 36 patients (80%). Balloon dilation of the anastomosis was performed in all 36 patients in whom ERCP was successful, and temporary plastic stent (PS) placement was performed in 20 of these patients (55.6%). Three cases of PS migration and one case of portal vein thrombosis occurred as mild AEs. However, one case of intestinal perforation required emergency surgery for repair. In univariate analysis, proficiency in ERCP procedures (p = 0.019) and surgery at our hospital (p = 0.010) emerged as major factors affecting the procedural success. In univariate analysis, only the early onset of CJS within 400 days after choledochojejunostomy was extracted as a significant factor for the early recurrence of CJS after ERCP (p = 0.036). Conclusions: To ensure successful BAE-ERCP for CJS, it is essential to have proficiency in the ERCP and collect as much detailed information about prior surgery as possible before the procedure. Additionally, the risk of CJS recurrence might be high in patients in whom CJS develops early after surgery.
Full article
Open AccessArticle
The Treatment of Three-Part Fractures of Humeral Head: A Retrospective Study to Compare Nail vs. Plate
by
Francesco Roberto Evola, Michele Vecchio, Marco Vacante and Giuseppe Evola
Surg. Tech. Dev. 2025, 14(3), 23; https://doi.org/10.3390/std14030023 - 12 Jul 2025
Abstract
►▼
Show Figures
Background: There are no clear guidelines to support management decisions for patients with three-part fractures of the proximal humerus. The aim of the study is to identify the treatment used and to assess the functional and radiological outcomes at follow-up. Methods: A total
[...] Read more.
Background: There are no clear guidelines to support management decisions for patients with three-part fractures of the proximal humerus. The aim of the study is to identify the treatment used and to assess the functional and radiological outcomes at follow-up. Methods: A total of 126 patients were retrospectively included in the study and were divided into two groups based on the type of surgery: plate and nail group. We collected data on the patient’s sex, age, fracture type, surgery duration, fracture healing, initial and final neck–shaft angles, shoulder joint score, and complications. Results: A total of 69 patients received locking-plate internal fixation, while 77 patients underwent fixation with intramedullary nail. The two groups were comparable, with no significant differences observed in age, sex, or the number of patients. The average operation time for the locking-plate group (88.7 ± 10.5 min) was significantly longer compared to the intramedullary nail group (70.2 ± 8.3 min). The Constant–Murley score was 91.2 ± 6.7 (range 79–98) in the plate group and 90.5 ± 7.7 (range 80–98) in the nail group, with no statistically significant difference. Complications were observed in 16 patients (23.2%) of the locking-plate group and in 7 patients (9.1%) of the intramedullary nail group, with significant difference. Conclusions: Our assessment revealed no significant differences in fracture healing times, loss of reduction, or Constant–Murley scores between two groups. However, our results suggest that intramedullary nails have an advantage over locking plates in terms of reduced operation time and complications.
Full article

Figure 1
Open AccessReview
Advances in 3D-Printed Implants for Facial Plastic Surgery
by
Joan Birbe Foraster
Surg. Tech. Dev. 2025, 14(3), 22; https://doi.org/10.3390/std14030022 - 1 Jul 2025
Abstract
Facial reconstruction presents complex challenges due to the intricate nature of craniofacial anatomy and the necessity for individualized treatment. Conventional reconstructive methods—such as autologous bone grafts and prefabricated alloplastic implants—pose limitations, including donor site morbidity, implant rejection, and suboptimal aesthetic results. The emergence
[...] Read more.
Facial reconstruction presents complex challenges due to the intricate nature of craniofacial anatomy and the necessity for individualized treatment. Conventional reconstructive methods—such as autologous bone grafts and prefabricated alloplastic implants—pose limitations, including donor site morbidity, implant rejection, and suboptimal aesthetic results. The emergence of 3D printing technology has introduced patient-specific implants (PSIs) that enhance anatomical fit, functional restoration, and biocompatibility. This review outlines the evolution of 3D-printed implants, key materials, computer-assisted design (CAD), and their applications across trauma, oncology, congenital conditions, and aesthetics. It also addresses current challenges and explores future directions, such as bioprinting, smart implants, and drug-eluting coatings.
Full article
(This article belongs to the Special Issue New Insights into Plastic Aesthetic and Regenerative Surgery)
►▼
Show Figures

Figure 1
Open AccessReview
Surgeon Training in the Era of Computer-Enhanced Simulation Robotics and Emerging Technologies: A Narrative Review
by
Simon Keelan, Mina Guirgis, Benji Julien, Peter J. Hewett and Michael Talbot
Surg. Tech. Dev. 2025, 14(3), 21; https://doi.org/10.3390/std14030021 - 27 Jun 2025
Abstract
Background: Teaching methodology has recently undergone significant evolution from traditional apprenticeship models as we adapt to ever-increasing rates of technological advancement. Big data, artificial intelligence, and machine learning are on the precipice of revolutionising all aspects of surgical practice, with far-reaching implications.
[...] Read more.
Background: Teaching methodology has recently undergone significant evolution from traditional apprenticeship models as we adapt to ever-increasing rates of technological advancement. Big data, artificial intelligence, and machine learning are on the precipice of revolutionising all aspects of surgical practice, with far-reaching implications. Robotic platforms will increase in autonomy as machine learning rapidly becomes more sophisticated, and therefore training requirements will no longer slow innovation. Materials and Methods: A search of published studies discussing surgeon training and computer-enhanced simulation robotics and emerging technologies using MEDLINE, PubMed, EMBASE, Scopus, CRANE, CINAHL, and Web of Science was performed in January 2024. Online resources associated with proprietary technologies related to the subject matter were also utilised. Results: Following a review of 3209 articles, 91 of which were published, relevant articles on aspects of robotics-based computer-enhanced simulation, technologies, and education were included. Publications ranged from RCTs, cohort studies, meta-analysis, and systematic reviews. The content of eight medical technology-based websites was analysed and included in this review to ensure the most up-to-date information was analysed. Discussion: Surgeons should aim to be at the forefront of this revolution for the ultimate benefit of patients. Surgical exposure will no longer be due to incidental experiences. Rather, surgeons and trainees will have access to a complete database of simulated minimally invasive procedures, and procedural simulation certification will likely become a requisite from graduation to live operating to maintain rigorous patient safety standards. This review provides a comprehensive outline of the current and future status of surgical training in the robotic and digital era.
Full article
Open AccessTechnical Note
Laparoscopic-Assisted Percutaneous Cryoablation of Abdominal Wall Desmoid Fibromatosis: Case Series and Local Experience
by
Kadhim Taqi, Jaymie Walker, Cecily Stockley, Antoine Bouchard-Fortier, Stefan Przybojewski and Lloyd Mack
Surg. Tech. Dev. 2025, 14(3), 20; https://doi.org/10.3390/std14030020 - 24 Jun 2025
Abstract
►▼
Show Figures
Background: Desmoid tumors (DTs) are rare, non-metastatic but locally aggressive connective tissue neoplasms. While standard treatments include surgery, radiation, and ablation, current guidelines advocate active surveillance unless tumors progress or symptoms worsen. Cryotherapy has shown promise in treating DTs; however, its application in
[...] Read more.
Background: Desmoid tumors (DTs) are rare, non-metastatic but locally aggressive connective tissue neoplasms. While standard treatments include surgery, radiation, and ablation, current guidelines advocate active surveillance unless tumors progress or symptoms worsen. Cryotherapy has shown promise in treating DTs; however, its application in rectus abdominis DTs has been limited due to proximity to critical intra-abdominal structures. Methods: This case series describes a novel approach involving laparoscopic-assisted cryoablation in three patients with rectus abdominis DTs. Laparoscopic visualization was employed to improve tumor localization and procedural safety during percutaneous cryoablation. Results: The average tumor size was 7.4 cm, and a mean of 14 cryoprobes were used per case. All patients experienced complete symptom resolution. One patient developed a complication—injury to the inferior epigastric artery—requiring embolization. Follow-up imaging at three months showed significant tumor shrinkage and necrosis in two patients. The third patient had increased lesion volume due to post-procedural hematoma, although radiological markers of cryoablation efficacy were present. Conclusions: Laparoscopic-assisted cryoablation appears to be a feasible and effective technique for treating rectus abdominis DTs, providing symptom relief and favorable early tumor response. Further studies are warranted to evaluate long-term outcomes and validate this approach in broader clinical settings.
Full article

Figure 1
Open AccessCase Report
Endless-Loop Craniotomy for Revision Surgery After the Burr-Hole Evacuation of Chronic Subdural Hematoma—A Technical Note
by
Artem Rafaelian, Sae-Yeon Won, Thomas M. Freiman, Florian Gessler and Daniel Dubinski
Surg. Tech. Dev. 2025, 14(3), 19; https://doi.org/10.3390/std14030019 - 21 Jun 2025
Abstract
►▼
Show Figures
Background and Importance: Chronic subdural hematoma (cSDH) is a common and complex neurosurgical problem, particularly in elderly patients. Revision surgery for chronic subdural hematoma can be challenging, particularly in cases with inhomogeneous, firm consistency and extensive adhesions. Clinical Presentation: In this article, we
[...] Read more.
Background and Importance: Chronic subdural hematoma (cSDH) is a common and complex neurosurgical problem, particularly in elderly patients. Revision surgery for chronic subdural hematoma can be challenging, particularly in cases with inhomogeneous, firm consistency and extensive adhesions. Clinical Presentation: In this article, we present our endless-loop craniotomy technique, which offers a novel approach to address these challenges by performing the wide, curved exposure of the subdural space utilizing the already-present burr hole. This technique allows for a wide, unobstructed view of the subdural space, enabling the access and evacuation of this chronic and often adhesive subdural hematoma. Conclusion: We believe that endless-loop craniotomy is a valuable addition to the neurosurgeon’s armamentarium for managing complex cases of revision surgery in chronic subdural hematomas.
Full article
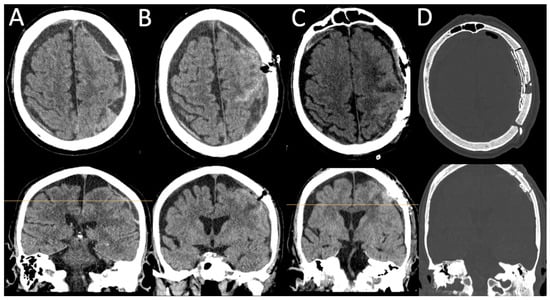
Figure 1
Open AccessCase Report
Left-Sided Bochdalek Hernia with Bowel Strangulation in 42-Year-Old Male: Successful Minimally Invasive Repair Using Right Lateral Decubitus Positioning
by
Fahim Kanani, Nir Messer, Moshe Kamar and Narmin Zoabi
Surg. Tech. Dev. 2025, 14(2), 18; https://doi.org/10.3390/std14020018 - 10 Jun 2025
Abstract
►▼
Show Figures
Adult Bochdalek hernias represent a rare clinical entity that often presents diagnostic challenges due to their non-specific symptomatology. We report the case of a 42-year-old male who presented with acute abdominal pain and was found to have a left-sided Bochdalek hernia with strangulated
[...] Read more.
Adult Bochdalek hernias represent a rare clinical entity that often presents diagnostic challenges due to their non-specific symptomatology. We report the case of a 42-year-old male who presented with acute abdominal pain and was found to have a left-sided Bochdalek hernia with strangulated small bowel. The patient underwent a successful laparoscopic repair using right lateral decubitus positioning, which facilitated optimal access to the diaphragmatic defect. The herniated bowel was reduced and found to be viable, and the defect was closed primarily with mesh reinforcement. This case highlights the importance of maintaining a high index of suspicion for diaphragmatic hernias in adults with vague abdominal and respiratory symptoms, the value of prompt imaging in establishing the diagnosis, and the efficacy of minimally invasive surgical techniques with innovative patient positioning for definitive management. The patient recovered well, with complete resolution of symptoms and no recurrence at the 4-year follow-up.
Full article

Figure 1
Open AccessArticle
Minimally Invasive Techniques for Large-Volume Benign Prostatic Hyperplasia: A Comparative Study Between HoLEP and Robotic Simple Prostatectomy
by
Silvia Juste-Alvarez, Claudia Zaccaro, Javier Gil-Moradillo, Javier Romero-Otero, Ignacio Moncada, Alfredo Rodríguez-Antolín and Borja Garcia-Gomez
Surg. Tech. Dev. 2025, 14(2), 17; https://doi.org/10.3390/std14020017 - 28 May 2025
Abstract
►▼
Show Figures
Background/Objectives: The aim of this research was to compare perioperative outcomes, functional results, quality of life, and complications between robot-assisted simple prostatectomy (RASP) and holmium laser prostate enucleation (HoLEP) as minimally invasive techniques for treating benign prostatic hyperplasia (BPH) in large prostates
[...] Read more.
Background/Objectives: The aim of this research was to compare perioperative outcomes, functional results, quality of life, and complications between robot-assisted simple prostatectomy (RASP) and holmium laser prostate enucleation (HoLEP) as minimally invasive techniques for treating benign prostatic hyperplasia (BPH) in large prostates (>150 cm3). Methods: This retrospective, multicenter, observational study (2007–2023) included patients with >150 cm3 prostate volumes who underwent either HoLEP or robot-assisted prostatectomy. Primary outcomes: success rate (complete enucleation, without transfusion or reintervention), good postoperative quality of life (IPSS 8th question score: 0–2), and continence at 6 months (no pads). Secondary outcomes: operative and catheterization time, hospital stay, enucleated gland weight, PSA reduction, Qmax improvement, and perioperative complications. Results: We included 95 HoLEP and 50 RASP patients with similar demographics and prostate volume (HoLEP: 187.72 cm3; RASP: 203.38 cm3). The success rate (HOLEP: 83.2%; RASP: 74%), continence rate (HoLEP: 85.1%; RASP: 86%), and quality of life (HoLEP: 83.2%; RASP 94%) were similar (p = 0.275, p = 1, and p = 0.075, respectively). HoLEP had a shorter operative time (97.58 vs. 122.4 min) and catheterization duration, with similar hospitalization duration (HoLEP: 3.46 days; RASP: 4.22 days). Although there was no significant difference in enucleated gland weight, HoLEP was more efficient (1.28 g/min vs. 1.06 g/min). Complication rates were similar (HOLEP: 15.5%; RASP: 26%; p = 0.12). Conclusions: Both RASP and HoLEP are safe for treating BPH in prostates >150 cm3, reporting similar success and continence rates and good quality of life after surgery. However, HoLEP achieved results with shorter operative time and catheterization duration.
Full article

Figure 1
Open AccessTechnical Note
Mini Abdomen Experience: A Novel Approach for Mini-Abdominoplasty Minimally Invasive (MAMI) Abdominal Contouring
by
Rodrigo Ferraz Galhego, Tulio Martins, Alvaro Cota Carvalho, Marco Faria-Correa and Raquel Nogueira
Surg. Tech. Dev. 2025, 14(2), 16; https://doi.org/10.3390/std14020016 - 9 May 2025
Abstract
Purpose: Our aim is to offer an additional surgical option for patients with rectus diastasis, with or without associated abdominal wall hernias, through a minimally invasive approach with endoscopic surgical correction, presenting a new method for abdominal contouring via minimally invasive mini-abdominoplasty (MAMI).
[...] Read more.
Purpose: Our aim is to offer an additional surgical option for patients with rectus diastasis, with or without associated abdominal wall hernias, through a minimally invasive approach with endoscopic surgical correction, presenting a new method for abdominal contouring via minimally invasive mini-abdominoplasty (MAMI). Ideas: According to the European Hernia Society (EHS) classification for RD, a widening greater than 2 cm of the linea alba is generally considered an indication for surgical correction. Recent approaches, such as MILA and SCOLA, are indicated for patients with a body mass index (BMI) of up to 28, based solely on height and weight. However, some authors consider this insufficient for determining the best surgical indication. Despite advances in skin retraction, there is still no evidence on how these devices affect postoperative outcomes when added to these techniques, as they depend on multiple factors such as age, skin firmness, number of passes, applied energy, etc. Consequently, even patients with a BMI of up to 28 may present significant flaccidity both above and below the umbilicus, as well as poor skin quality (thin, lax, with stretch marks), making SCOLA or MILA surgery alone unsuitable due to possible skin redundancy after surgery. Similarly, even patients with a high-positioned umbilicus, moderate flaccidity, and rectus diastasis, who in the past would have been strictly indicated for abdominoplasty, may benefit from mini-abdominoplasty with a minimally invasive approach (MAMI). Discussion: The main objective of this study is to provide another surgical option for patients who would otherwise be indicated for abdominoplasty and also for those undergoing MILA or SCOLA who still require minor skin removal to enhance the surgical result. Based on our experience, mini-abdominoplasty with a minimally invasive approach (MAMI) has the potential to serve a larger number of patients, since most present degrees of skin laxity that, even after using technologies, require skin excision. In addition to complementing the results, it reduces complications, results in smaller scars, allows a better correction and visualization of the diastasis, avoids periumbilical scars, and offers faster recovery compared to abdominoplasty. Conclusions: MAMI surgery has proven to be a safe and reproducible approach for selected women who wish to restore feminine body features after pregnancy and achieve a quick recovery. It yields satisfactory esthetic results due to the minimized scar, preservation of the natural umbilical scar, and improved surgical correction of rectus diastasis.
Full article
(This article belongs to the Special Issue New Insights into Plastic Aesthetic and Regenerative Surgery)
►▼
Show Figures

Figure 1
Open AccessArticle
Bilateral Stylopharyngeus Transection Alters Respiratory Airflow in Conscious Rats
by
Eriko Hamada, Thomaz Fleury Curado, Kingman Strohl and Yee-Hsee Hsieh
Surg. Tech. Dev. 2025, 14(2), 15; https://doi.org/10.3390/std14020015 - 7 May 2025
Abstract
►▼
Show Figures
Background/Objectives: Upper airway patency is a key pathophysiological factor in obstructive sleep apnea (OSA). Research has primarily focused on the role of the genioglossus muscle in maintaining airway patency in OSA. However, hypoglossal nerve stimulation (HNS) therapy, which activates the genioglossus muscle, has
[...] Read more.
Background/Objectives: Upper airway patency is a key pathophysiological factor in obstructive sleep apnea (OSA). Research has primarily focused on the role of the genioglossus muscle in maintaining airway patency in OSA. However, hypoglossal nerve stimulation (HNS) therapy, which activates the genioglossus muscle, has been associated with poor outcomes in patients with lateral oropharyngeal collapse. The stylopharyngeus muscle is an upper airway dilator muscle that supports the lateral pharyngeal wall. Its role in maintaining upper airway patency and its effect on normal respiratory airflow is unclear. We hypothesize that bilateral transection of the stylopharyngeus muscles disrupts normal breathing. Currently, no animal model depicting lateral pharyngeal collapse has been reported. This study aims to introduce a novel rodent model with bilateral transection of the stylopharyngeus muscles to examine its effect on respiratory airflow and tracing. Methods: Adult male Sprague Dawley rats were divided into two groups: (1) bilateral stylopharyngeus muscle transection (n = 4) and (2) sham surgery (n = 2). Under anesthesia, the stylopharyngeus muscle was transected bilaterally in the transection group, while only exposure of the muscle was performed in the sham group. Respiratory airflow was measured using whole-body plethysmography before and after surgery, and airflow tracings were analyzed. Results: Significant alterations in respiratory airflow and tracings, particularly a flattening in inspiratory flow and sharp expiratory peaks, were observed on the first post-operative day in the transection group. The flattening of the inspiratory flow persisted over 3 days. No significant changes were noted in the sham group. Conclusions: Bilateral stylopharyngeus muscle transection alters normal airflow in a conscious rodent model, supporting the hypothesis that stylopharyngeus muscle plays a vital role in shaping respiratory airflow. The flattening of the inspiratory airflow is an indication of flow limitations through the upper airway patency due to the loss of stylopharyngeus function.
Full article

Figure 1
Open AccessSystematic Review
Efficacy and Clinical Applicability of Impar Ganglion Block in the Treatment of Pudendal Neuralgia: A Systematic Review
by
Joelington Dias Batista, Gabrielly Santos Pereira, Jobson Dias Batista, Ludimila Dias Silva, Josie Resende Torres da Silva and Marcelo Lourenço da Silva
Surg. Tech. Dev. 2025, 14(2), 14; https://doi.org/10.3390/std14020014 - 1 May 2025
Abstract
►▼
Show Figures
Background/Objectives: Pudendal neuralgia (PN) is a debilitating chronic pain condition resulting from injury, inflammation, or entrapment of the pudendal nerve. It significantly affects patients’ quality of life and poses challenges to treatment due to its complex etiology. Conventional therapies often provide limited or
[...] Read more.
Background/Objectives: Pudendal neuralgia (PN) is a debilitating chronic pain condition resulting from injury, inflammation, or entrapment of the pudendal nerve. It significantly affects patients’ quality of life and poses challenges to treatment due to its complex etiology. Conventional therapies often provide limited or temporary relief. The impar ganglion block (IGB) has emerged as a potential intervention for managing refractory pelvic pain syndromes. This systematic review aimed to evaluate the clinical efficacy, safety, and applicability of IGB in treating patients with PN. Methods: This systematic review evaluates the efficacy and clinical applicability of IGBs in treating PN. Following PRISMA-P 2020 guidelines, a systematic search was conducted in PubMed/MEDLINE, Embase, LILACS, and Cochrane Library. Eligible studies included RCTs, observational studies, and case series assessing pain reduction and quality of life post-IGB. Non-neuropathic pelvic pain studies were excluded. The ROBVIS tool assessed the risk of bias. Results: Of 306 articles screened, 16 met eligibility criteria. Studies showed that the IGB provides significant pain relief, particularly for refractory cases. Image-guided techniques enhanced precision and reduced complications. Combination therapies with corticosteroids yielded longer-lasting analgesia. However, methodological inconsistencies and varied patient selection limited generalizability. Conclusions: The IGB is a minimally invasive, effective option for managing PN. Further high-quality RCTs are needed to standardize protocols, optimize patient selection, and evaluate long-term efficacy. A multidisciplinary approach remains essential.
Full article

Figure 1
Open AccessCase Report
Endoscopic Treatment of Symptomatic Septum Pellucidum Cyst in an Adult Patient—Case Report and Technical Notes
by
Daniel Ilie Rotariu, Bogdan Florin Iliescu, Razvan Buga and Bogdan Costachescu
Surg. Tech. Dev. 2025, 14(2), 13; https://doi.org/10.3390/std14020013 - 22 Apr 2025
Abstract
►▼
Show Figures
Background: Midline cysts of the brain are comprised of the following entities, septum pellucidum cysts, cavum vergae cysts and velum interpositum cysts. These lesions are uncommon and often asymptomatic; nonetheless, certain clinical manifestations may be linked to midline cysts, including headaches, signs of
[...] Read more.
Background: Midline cysts of the brain are comprised of the following entities, septum pellucidum cysts, cavum vergae cysts and velum interpositum cysts. These lesions are uncommon and often asymptomatic; nonetheless, certain clinical manifestations may be linked to midline cysts, including headaches, signs of elevated intracranial pressure, neurological deficits, or alterations in mental status. Controversy persists in the therapy of symptomatic cases, mostly due to the challenge of establishing a correlation between the symptomatology and the presence of the cyst. Case description: We present the case of a 64-year-old female known with type—1 neurofibromatosis that associated a midline cyst. The cyst was treated endoscopically, in the initial stage (single wall perforation) showed no clinical or imagistic improvement. The incriminated symptoms in these cases are caused not only by compression or obstruction of the CSF flow but also to a complex alteration of CSF dynamics, in this case the stoma was found permeable at the second surgery but there was no obvious communication on the preoperative evaluation by ventriculocisternostomy. A second surgery was performed, with bilateral perforation and subsequent improvement of symptomatology and decrease of cyst dimensions. A literature review is presented concerning clinical presentation, therapeutic options, and possible outcomes. Conclusions: Endoscopic fenestration is an efficacious method for treating midline cysts, with bilateral wall fenestration representing the standard practice. Understanding the anatomical and developmental specifics of the septal region, together with cerebrospinal fluid dynamics, is essential for effective treatment of this condition.
Full article

Figure 1
Open AccessArticle
Impact of Peritoneal Closure on Inguinal Hernia Incidence After Robot-Assisted Radical Prostatectomy
by
Naoki Imasato, Shugo Yajima, Ryo Andy Ogasawara, Minoru Inoue, Kohei Hirose, Ken Sekiya, Madoka Kataoka, Yasukazu Nakanishi and Hitoshi Masuda
Surg. Tech. Dev. 2025, 14(2), 12; https://doi.org/10.3390/std14020012 - 18 Apr 2025
Abstract
►▼
Show Figures
Background/Objectives: Inguinal hernia (IH) is a common complication after robot-assisted radical prostatectomy (RARP), significantly impacting patients’ quality of life. This study aimed to evaluate whether peritoneal closure reduces the incidence of IH after RARP. Methods: A retrospective analysis was conducted on 772 patients
[...] Read more.
Background/Objectives: Inguinal hernia (IH) is a common complication after robot-assisted radical prostatectomy (RARP), significantly impacting patients’ quality of life. This study aimed to evaluate whether peritoneal closure reduces the incidence of IH after RARP. Methods: A retrospective analysis was conducted on 772 patients who underwent transperitoneal RARP between April 2018 and March 2023. Patients with a history of IH surgery were excluded. Peritoneal closure, introduced in December 2021, was performed during the final steps of RARP in 144 patients. The incidence of IH was compared between patients with and without peritoneal closure. Multivariate analysis was performed to identify significant predictors of IH. Results: IH occurred in 73 patients (9.5%)—5 (3.5%) in the peritoneal closure group and 68 (10.8%) in the no peritoneal closure group. Multivariate analysis revealed that the absence of peritoneal closure (hazard ratio [HR] = 4.55, p = 0.04) and low body mass index (BMI < 23 kg/m2; HR = 2.51, p = 0.001) were significant predictors of IH. The two-year IH-free survival rate was 96.5% in the peritoneal closure group and 89.2% in the no peritoneal closure group. Conclusions: Peritoneal closure significantly reduces the incidence of IH after RARP. This simple and effective technique may serve as a valuable preventive measure against postoperative IH, potentially improving surgical outcomes and patient quality of life. Further studies are warranted to confirm these results in diverse patient populations.
Full article
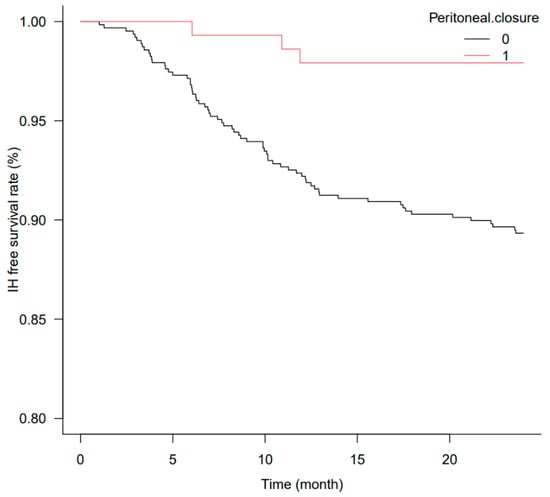
Figure 1
Open AccessCase Report
Endoscopic Injection of BioGlue for the Treatment of a Ureterocolic Fistula After Radical Cystectomy
by
Chiara Re, Pietro Scilipoti, Giuseppe Rosiello, Nicola Leggio, Giulio Avesani, Rayan Matloob, Andrea Salonia, Francesco Montorsi and Roberto Bertini
Surg. Tech. Dev. 2025, 14(2), 11; https://doi.org/10.3390/std14020011 - 1 Apr 2025
Abstract
►▼
Show Figures
Background/Objectives: An 80-year-old man was admitted to our department after a salvage radical cystectomy for actinic cystitis due to radiotherapy for prostate cancer. He presented with a two-month history of feculent debris in the right stoma and deteriorated general conditions, after a long
[...] Read more.
Background/Objectives: An 80-year-old man was admitted to our department after a salvage radical cystectomy for actinic cystitis due to radiotherapy for prostate cancer. He presented with a two-month history of feculent debris in the right stoma and deteriorated general conditions, after a long past medical history of recurrent complicated urinary infections. Methods: Computer tomography (CT) of the abdomen revealed a ureterocolic fistula along the right ureteral pelvic tract. A right percutaneous nephrostomy tube was placed. Due to multiple previous surgeries, several lines of intravenous antibiotic therapies and the overall condition of the patient, a conservative management was preferred. Results: A bovine serum albumin-glutaraldehyde (BioGlue®) adhesive was inoculated into the right ureter through the stoma to close the fistula. After 24 months, the patient remained asymptomatic with negative follow-up imaging. Conclusions: Given the uniqueness of the management of a ureterocolic fistula, this case offers insight into conservative treatment in frail patients not suitable for major surgery.
Full article
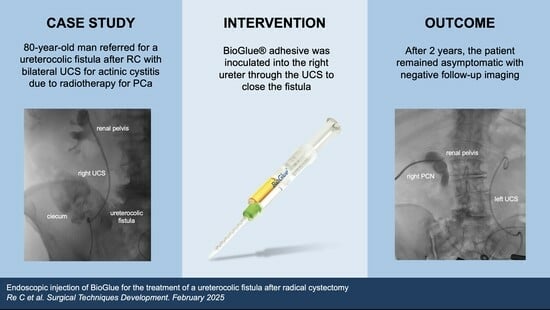
Graphical abstract
Open AccessArticle
The Orthopedic Strategy for Patients with Larsen Syndrome
by
Ali Al Kaissi, Alexander Gubin, Sergey Ryabykh, Vasileios Dougales, Hamza Al Kaissi, Susanne Gerit Kircher and Franz Grill
Surg. Tech. Dev. 2025, 14(2), 10; https://doi.org/10.3390/std14020010 - 25 Mar 2025
Abstract
►▼
Show Figures
Background: Facial features are the first basic sign of medical knowledge of children and adults with congenital malformations. Children born with multiple contractures almost always receive the misdiagnosis of arthrogryposis multiplex. Larsen syndrome can easily be diagnosed at birth via the proper interpretations
[...] Read more.
Background: Facial features are the first basic sign of medical knowledge of children and adults with congenital malformations. Children born with multiple contractures almost always receive the misdiagnosis of arthrogryposis multiplex. Larsen syndrome can easily be diagnosed at birth via the proper interpretations of its characteristic facial features and multiple dislocations. Comprehensive clinical diagnosis can facilitate an orthopedic strategy for early treatment and can enhance the recognition of unreported craniocervical malformation complexes. Material and Methods: Six children (four boys and two girls, with ages ranging from a few months to 7 years old) were referred to our department for diagnosis and treatment. All children received their first misdiagnosis by the pediatricians as manifesting arthrogryposis multiplex congenita. The clinical phenotype was our first decisive tool for diagnosis. All children exhibited the classical phenotype of dish-like facies associated with multiple joint dislocations. Radiological phenotypic characteristics confirmed our clinical diagnosis of Larsen syndrome. Three children out of six showed unpleasant cervical spine deformities. The first child, a 2-year-old, became tetraplegic after minor trauma. One child presented with progressive rigid cervical kyphosis. The third child was a product of a first-relative marriage and was born with congenital tetraplegia. A genotype was carried out for confirmation. Results: Three children underwent open reduction for congenital hip and knee dislocations. One child underwent spinal fusion CO-C7 because of tetraplegia. A 3D-reformatted and reconstruction CT scan of the craniocervical junction showed two forms of unusual dys-segmentation, firstly along C2-3 effectively causing the development of acute-angle cervical kyphosis. Secondly, an infant with congenital tetraplegia showed a serious previously undescribed atlanto–axial malformation complex. Namely, atlanto–axial maldevelopment (dys-segmentation) of (C1/C2) was associated with hypoplasia of the anterior and the posterior rings of the atlas. Genetic tests of these children were compatible with the autosomal dominant type of Larsen syndrome and manifested a heterozygous mutation in FLNB mapped 3p14.3, encoding an actin-binding protein, filamin B. The child with congenital tetraplegia showed no mutations in FLNB, though his clinical and radiological phenotype and his family history of first-relative marriage were totally compatible with the diagnosis of the autosomal recessive type of Larsen syndrome. Conclusions: Our strategy was and still is based on a coherent clinical and radiological diagnosis, which is based on comprehensive clinical and radiological phenotypic characterizations. We implemented a 3D-reformatted CT scan to further understand the craniocervical junction pathology in three children. Strikingly, prenatal onset of lethal maldevelopment (dys-segmentation) of the atlanto–axial spine segments has been diagnosed in an infant with congenital tetraplagia. A less serious cervical spine malformation was detected in two children who presented with progressive acute-angle cervico and cervico-thoracic kyphosis. Our clinical strategy can form the basis for a thorough clinical assessment for infants and children born with multiple malformation complexes and can lead to recognition of novel understandings.
Full article
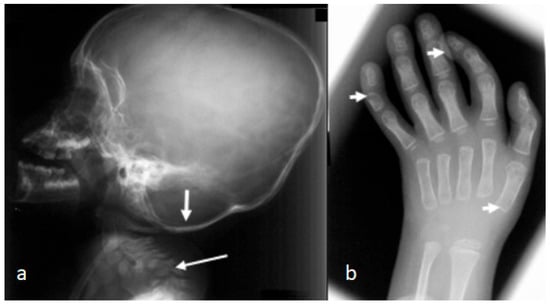
Figure 1
Open AccessArticle
The Mini-Pig as an Animal Model for Focal Cartilage Treatment of the Knee—A Comparison to the Domestic Pig
by
Halah Kutaish, Vannary Tieng and Philippe Matthias Tscholl
Surg. Tech. Dev. 2025, 14(2), 9; https://doi.org/10.3390/std14020009 - 21 Mar 2025
Abstract
►▼
Show Figures
Aim: This study aims to assess the suitability of the Göttingen Mini-pig (G-MP) as a large animal model for preclinical research on articular cartilage treatment procedures. Additionally, this study compares the G-MP to the domestic pig (DP) regarding surgical anatomy, postoperative care, and
[...] Read more.
Aim: This study aims to assess the suitability of the Göttingen Mini-pig (G-MP) as a large animal model for preclinical research on articular cartilage treatment procedures. Additionally, this study compares the G-MP to the domestic pig (DP) regarding surgical anatomy, postoperative care, and the challenges associated with the follow-up period. Materials and methods: Six G-MPs and four DPs underwent a two-stage surgical procedure: first, cartilage was harvested using a superolateral approach, followed by cartilage implantation via a medial parapatellar tendon approach. Results: The superolateral approach exposed 11% (SD ± 5) of the trochlea in G-MPs and 20% in DPs. The medial parapatellar tendon approach exposed 63% (SD ± 4) of the trochlear surface and 34% (SD ± 13) of the medial femoral condyle in G-MPs, allowing for the creation of four 6 mm trochlear lesions and one medial condyle lesion in four out of six G-MPs and all DPs. Cartilage thickness was less than 1 mm in G-MPs, compared to over 2 mm in DPs. Weight gain was +4 kg/week in DPs and +0.2 kg/week in G-MPs. Conclusion: Overall, the G-MP proves to be a viable model for cartilage research, offering sufficient joint access via the dual approach, which allows for 4–5 lesions of 6 mm each. However, the thinner cartilage in G-MPs should be taken into account.
Full article
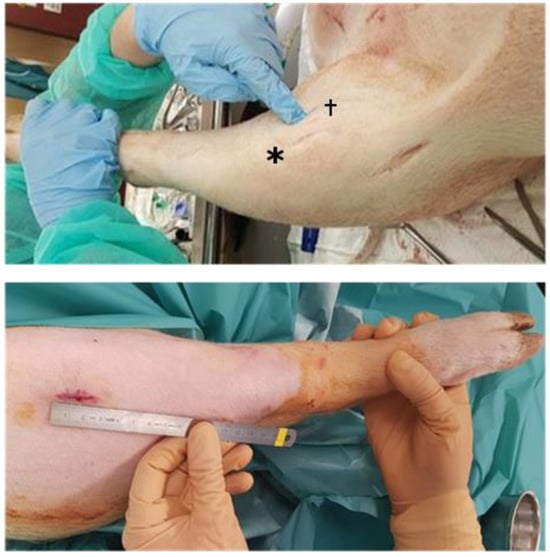
Figure 1
Open AccessArticle
Impact of Negative Pressure Wound Therapy on Outcomes Following Pancreaticoduodenectomy: An NSQIP Analysis of 14,044 Patients
by
Jeremy Peabody, Sukhdeep Jatana, Kevin Verhoeff, A. M. James Shapiro, David L. Bigam, Blaire Anderson and Khaled Dajani
Surg. Tech. Dev. 2025, 14(1), 8; https://doi.org/10.3390/std14010008 - 4 Mar 2025
Cited by 1
Abstract
►▼
Show Figures
Background: Despite ongoing efforts to improve the pancreaticoduodenectomy technique and perioperative care, surgical site infection (SSI) remains a contributor to morbidity. Efforts to reduce SSI include the use of negative pressure wound therapy (NPWT), but studies and meta-analyses have been met with
[...] Read more.
Background: Despite ongoing efforts to improve the pancreaticoduodenectomy technique and perioperative care, surgical site infection (SSI) remains a contributor to morbidity. Efforts to reduce SSI include the use of negative pressure wound therapy (NPWT), but studies and meta-analyses have been met with conflicting results. We aimed to provide an up-to-date large-scale cohort study to assess the impact of NPWT on SSIs. Methods: Utilizing the National Surgical Quality Improvement Program database, we included patients undergoing a pancreaticoduodenectomy between 2017 and 2021 and divided patients into the NPWT and non-NPWT cohorts. A bivariate analysis was performed to compare baseline characteristics and complication rates between the cohorts. Multivariate logistic regression analysis was performed to assess the independent effect of NPWT on 30-day serious complication, 30-day mortality, and the development of deep or superficial SSI. A priori sensitivity analyses were performed in high-risk and malignancy cohorts. Results: Of the 14,044 included patients, 1689 (12.0%) patients had a prophylactic NPWT device, while 12,355 (88.0%) did not. Patients were more likely to have NPWT if they had higher ASA scores, had diabetes, were dialysis-dependent, or had a hard pancreas, but they were less likely if they were a smoker, had steroid use, or had a bleeding disorder. Most complications occurred similarly between the two cohorts, including superficial and deep SSI, but NPWT patients had a longer length of stay (10.4 d vs. 9.5 d, p < 0.001) and higher organ space SSI (22.6% vs. 17.4%, p < 0.001). Following multivariable modeling to control for demographic differences, NPWT was not independently associated with a difference in likelihood of SSI (aOR 0.94, p = 0.691) or serious complications (aOR 0.958, p = 0.669). Furthermore, the sensitivity analyses of both high-risk and malignant subgroup also did not see an independent association of NPWT on the rate of SSI (aOR 0.98, p = 0.898 and 0.96, p = 0.788, respectively). Conclusion: NPWT is used infrequently and is not significantly associated with improved outcomes including in the high-risk or malignant subgroups based on multivariable analysis for surgical site infections nor did it improve the outcomes of 30-day serious complications in these subgroups. Considering this and other studies showing the limited benefit of NPWT in all-comers and in high-risk cohorts, it remains unclear whether NPWT offers benefits following PD.
Full article

Graphical abstract
Open AccessSystematic Review
Pseudo-Obstruction After Reversal of Ileostomy
by
Kirsten R. Carlaw, Aizat Drahman and Angelina Di Re
Surg. Tech. Dev. 2025, 14(1), 7; https://doi.org/10.3390/std14010007 - 21 Feb 2025
Abstract
►▼
Show Figures
Background: Acute colonic pseudo-obstruction (ACP) is a life-threatening, rare condition of non-mechanical colon dilatation that can result in bowel ischaemia and perforation. The aetiology is relatively unknown but includes older age coupled with high comorbidity, decreased parasympathetic activity, certain medications, chemoradiotherapy and recent
[...] Read more.
Background: Acute colonic pseudo-obstruction (ACP) is a life-threatening, rare condition of non-mechanical colon dilatation that can result in bowel ischaemia and perforation. The aetiology is relatively unknown but includes older age coupled with high comorbidity, decreased parasympathetic activity, certain medications, chemoradiotherapy and recent surgery. There are limited research data on ACP following reversal of ileostomy after ultra-low anterior resections (ULAR), thus this systematic review included cases from various types of bowel surgeries. Methods: A comprehensive literature search of relevant articles was conducted using the EMBASE, Medline, PubMed, Cochrane, and Scopus databases. Two cases of ACP following ileostomy reversal after ULAR for rectal cancer were also reported from the authors’ rural institution. This systematic review was conducted according to PRISMA 2020 guidelines. Results: A total of 522 studies were screened of which five case reports were included. Two case series (six patients) and the two patients from the authors’ rural institution developed ACP following reversal of ileostomy post-ULAR with potential causes being the > 6 months’ time from initial surgery to reversal causing prolonged colonic mucosal inflammation and reduced wall contractile strength. Anastomotic leak and chemoradiotherapy were other considerations. One of the rural patients developed right colon ischaemia and perforation needing urgent laparotomy, right hemicolectomy and formation of end ileostomy and mucous fistula. Conservative treatment included aperients, enemas, flatus tube, bedside or endoscopic decompression, and neostigmine. Conclusions: Early recognition is vital to treat ACP with medical therapy and decompression to prevent bowel ischaemia and perforation. Further research is needed to better characterise the aetiology, incidence and management strategies for this rare condition.
Full article

Figure 1
Open AccessTechnical Note
Open Deep Venous Arterialization for No-Option Chronic Limb-Threatening Ischemia: A Variable and Adaptable Technique
by
Yaman Alsabbagh, Young Erben and Houssam Farres
Surg. Tech. Dev. 2025, 14(1), 6; https://doi.org/10.3390/std14010006 - 8 Feb 2025
Abstract
►▼
Show Figures
Background: Patients with no-option chronic limb-threatening ischemia (NoCLTI), lacking suitable distal arteries for conventional revascularization, face major limb amputation. The 1-year mortality rate after major amputation is 48.3%, increasing to 70.9% in 3 years. Open deep venous arterialization (DVA) offers a promising alternative
[...] Read more.
Background: Patients with no-option chronic limb-threatening ischemia (NoCLTI), lacking suitable distal arteries for conventional revascularization, face major limb amputation. The 1-year mortality rate after major amputation is 48.3%, increasing to 70.9% in 3 years. Open deep venous arterialization (DVA) offers a promising alternative for limb salvage, achievable through open, endovascular, or hybrid approaches. We aim to provide a comprehensive, step-by-step guide to performing open DVA in NoCLTI patients, addressing preoperative and postoperative considerations as well as the technical details of the procedure. Methods: Patient selection for open DVA focuses on individuals with NoCLTI at high risk for amputation. Preoperative assessments include evaluating risk factors, determining limb threat severity using the Wound, Ischemia, and foot Infection (WIfI) score, and mapping anatomical patterns via the Global Limb Anatomic Staging System (GLASS). The procedure involves identifying the target artery using Doppler ultrasound, performing microdissection to expose the artery and vein, ligating proximal vein branches, and creating a side-to-side anastomosis. Venous valves are disrupted with a valvulotome to allow antegrade flow. A proximal bypass graft may be applied if necessary. Results: Postoperatively, patients are monitored for 2–4 days with frequent Doppler assessments. Anticoagulation therapy begins with a heparin drip, transitioning to oral agents and/or dual antiplatelet therapy. Wound care includes deferred debridement for 2–4 weeks and may involve negative-pressure therapy. Follow-up involves weekly visits for the first month, and then at 3 months, and every 6 months thereafter, with surveillance using transcutaneous oxygen measurement, the toe–brachial index, and arterial duplex ultrasound. Conclusions: Open DVA represents a viable limb salvage option for patients with NoCLTI, potentially avoiding major amputations and improving quality of life. Success depends on careful patient selection, a meticulous surgical technique, and comprehensive postoperative care.
Full article

Figure 1
Open AccessTechnical Note
Gloveport-Assisted Retroperitoneal Pyeloplasty (GARP)
by
Javier Arredondo Montero and María Rodríguez Ruiz
Surg. Tech. Dev. 2025, 14(1), 5; https://doi.org/10.3390/std14010005 - 7 Feb 2025
Abstract
►▼
Show Figures
Introduction: Single-port video-assisted techniques, such as one-trocar-assisted pyeloplasty (OTAP) or Round-Traction-Assisted Pyeloplasty (RoTAP), have proven helpful for correcting congenital ureteropelvic junction obstruction (UPJO), especially in infants. Surgical Technique: This manuscript presents a technical variation based on the gloveport system that allows bimanual endocavitary
[...] Read more.
Introduction: Single-port video-assisted techniques, such as one-trocar-assisted pyeloplasty (OTAP) or Round-Traction-Assisted Pyeloplasty (RoTAP), have proven helpful for correcting congenital ureteropelvic junction obstruction (UPJO), especially in infants. Surgical Technique: This manuscript presents a technical variation based on the gloveport system that allows bimanual endocavitary dissection and protects the surgical wound during the procedure without increasing the cost or technical difficulty. Comment: This new technique, called gloveport-assisted retroperitoneal pyeloplasty (GARP), could be a valuable alternative for this pathology.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Surgical Techniques Development
Contemporary Surgical Strategies, Advanced Imaging, and Intelligent Technologies in Head and Neck Surgery
Guest Editor: Maciej ChęcińskiDeadline: 31 March 2026






