The Inheritance of Hearing Loss and Deafness: A Historical Perspective
Abstract
1. Introduction
2. Hybridists and Hereditarists
3. Inheritance and Genetics in Humans
4. The Inheritance of Hearing Loss and Deafness
5. The Birth of Otology
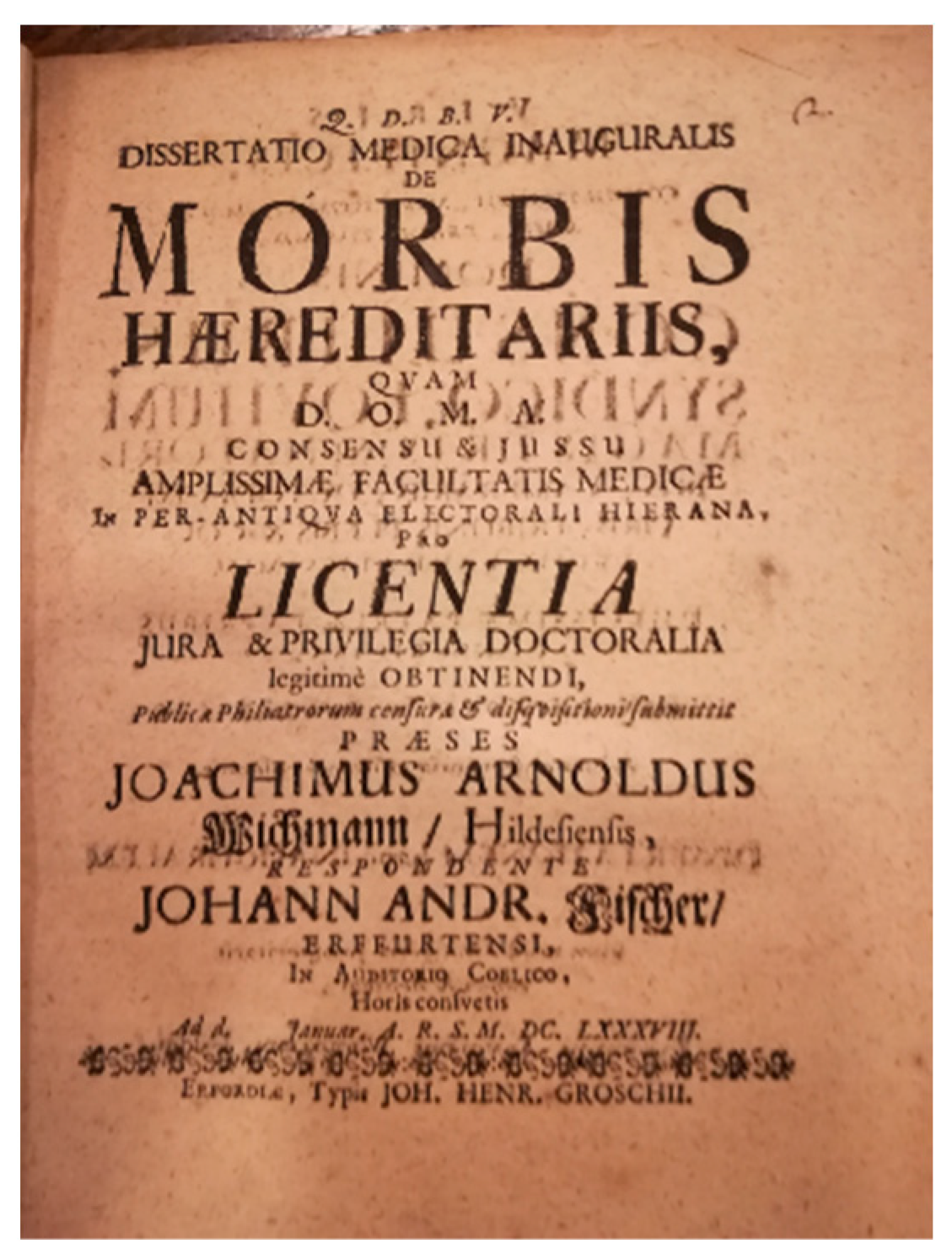
6. Deaf-Mutism
7. Consanguinity
8. Heredity of Deafness
9. The Audiometer and the Audiogram Phenotype
10. Molecular Genetics and Epigenetics
11. A Look at the Future: The “Omics Sciences” and Artificial Intelligence
11.1. Genomics
11.2. Proteomics
11.3. Transcriptomics
11.4. Metabolomics
11.5. Artificial Intelligence
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zeberg, H.; Pääbo, S. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature 2020, 587, 610–612. [Google Scholar] [CrossRef]
- Breno, M.; Noris, N.; Rubis, N.; Parvanova, A.I.; Martinetti, D.; Gamba, S.; Liguori, L.; Mele, C.; Piras, R.; Orisio, S.; et al. A GWAS in the pandemic epicenter highlights the severe COVID-19 risk locus introgressed by Neanderthals. iScience 2023, 26, 107629. [Google Scholar] [CrossRef]
- Genetics|History, Biology, Timeline, & Facts|Britannica. Available online: https://www.britannica.com/science/genetics (accessed on 5 November 2023).
- Devoto, G. Avviamento Alla Etimologia Italiana: Dizionario Etimologico, 3rd ed.; Le Monnier: Firenze, Italy, 1968. [Google Scholar]
- Montanari, F. Vocabolario Della Lingua Greca; Loescher: Torino, Italy, 1995. [Google Scholar]
- Johannsen, W. Elemente der Exakten Erblichkeitslehre; Fischer: Jena, Germany, 1909. [Google Scholar]
- Roll-Hansen, N. The Genotype Theory of Wilhelm Johannsen and its Relation to Plant Breeding and the Study of Evolution. Centaurus 1979, 22, 201–235. [Google Scholar] [CrossRef]
- Darwin, C. The Variation of Animals and Plants under Domestication; John Murray: London, UK, 1868. [Google Scholar]
- Liu, Y. A new perspective on Darwin’s Pangenesis. Biol. Rev. Camb. Philos. Soc. 2008, 83, 141–149. [Google Scholar] [CrossRef]
- Vries, H. De Intracellular Pangenesis; Gustav Fischer: Jena, Germany, 1889. [Google Scholar]
- Stamhuis, I.H.; Meijer, O.G.; Zevenhuizen, E.J. Hugo de Vries on heredity, 1889–1903. Statistics, Mendelian laws, pangenes, mutations. Isis. Int. Rev. Devoted Hist. Sci. Its Cult. Influ. 1999, 90, 238–267. [Google Scholar] [CrossRef]
- Di Trocchio, F. L’Ottocento: Biologia. Studi sull’ereditarietà. In Storia Della Scienza; Treccani: Roma, Italy, 2003. [Google Scholar]
- Enerstvedt, R. The Legacy of the Past: Those Who Are Gone but Have Not Left; Basis-Tryk: Dronninglund, Denmark, 1996. [Google Scholar]
- Van Camp, G.; Smith, R.J.H. Hereditary Hearing Loss Homepage. Available online: https://hereditaryhearingloss.org (accessed on 14 September 2021).
- Mudry, A. The History of Otology: A Tribute to Adam Politzer; Wayenborgh: Peribebuy, Paragauy, 2015. [Google Scholar]
- Eulenburg, A. Real-Encyklopädie der Gesammten Heilkunde: Medizinisch-Chirurgisches Handwörterbuch für Praktische Ärzte; Urban & Schwarzenberg: Wien und Leipzig, Germany, 1890; Volume 12. [Google Scholar]
- Cozza, A.; Di Pasquale Fiasca, V.M.; Martini, A. Congenital Deafness and Deaf-Mutism: A Historical Perspective. Children 2024, 11, 51. [Google Scholar] [CrossRef] [PubMed]
- Ménière, P. Du mariage entre parents, considéré comme cause de la surdimutité congénitale. Gaz. Méd. 1856, 3, 303–306. [Google Scholar]
- Liebreich, R. Abkunft aus Ehen unter Blutsverwandten als Grund von Retinitis Pigmentosa; Deutsche Klinik: Berlin, Germany, 1861. [Google Scholar]
- Boudin, J.C.M. Dangers des Unions Consanguines et Nécessité des Croisements dans L’espèce Humaine et Parmi les Animaux; Baillière: Paris, France, 1862. [Google Scholar]
- Knapp, H.; Moos, S. Archiv für Augen und Ohrenheilkunde; Wood: Ney York, NY, USA, 1870. [Google Scholar]
- Hartmann, A. Taubstummenheit und Taubstummenbildung nach den Vorhandenen Quellen, Sowie Nach e Igenen Beobochtungen und Erfahrungen; Enke: Stuttgart, Germany, 1880. [Google Scholar]
- Uchermann, V. Sordità e Sordomutismo. Ricerche Sperimentali. Versione con Proemio di Giulio Ferrari; Tipografia S. Bernardino: Siena, Italy, 1899. [Google Scholar]
- Schmaltz, H. Die Taubstummenim Königreich Sachsen; Breitkopf & Härtel: Leipzig, Germany, 1884. [Google Scholar]
- Wilde, W.R.W. Practical Observations on Aural Surgery and the Nature and Treatment of Diseases of the Ear; Churchill: Dublin, Ireland, 1853. [Google Scholar]
- Lent, Statistik der Taubstummen des Reg-Bez; DuMont Schauberg: Köln, Germany, 1869.
- Politzer, A. Lehrbuch der Ohrenheilkunde fur Practische Arzte und Studirende; Enke: Stuttgart, Germany, 1882. [Google Scholar]
- Reardon, W. Genetic deafness. J. Med. Genet. 1992, 29, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Gradenigo, G. Sur la pathogénie de l’otite sclérosante et de l’Ankylose stapedio-vestibulaire. Boll. Mal Orecch. 1887, 5, 136. [Google Scholar]
- Mygind, H. Deaf-Mutism; Rebman: London, UK, 1894. [Google Scholar]
- Gradenigo, G. La Surdite Familiale. In Monographies Oto-Rhino-Laryngologiques Internationales; 3, Legrand: Paris, France, 1921. [Google Scholar]
- Uchermann, V. De Dovstumme i Norge; Cammermeyer: Christiana, Norway, 1869. [Google Scholar]
- Von Graefe, A. Vereinzelte Beobachtungen und Bemerkungen: Exceptionelles Verhalten des Gesichtfeldes bei Pigmententartung der Netzhaut. Arch. Opthalmol. 1858, 4, 250–253. [Google Scholar]
- Paget, J. Cases of branchial fistulae in the external ears. Med. Chir. Trans. 1878, 61, 41–50. [Google Scholar] [CrossRef]
- Pendred, V. Deaf-mutism and goitre. Lancet 1856, 2, 532. [Google Scholar] [CrossRef]
- Berry, G. Note on a congenital defect (coloboma?) of the lower lid. Lond. Ophthalmol. Hosp. Rep. 1899, 21, 255–257. [Google Scholar]
- Treacher Collins, E. Case with symmetrical notches in the outer-part of each lower lid and defective development of the malar bone. Trans. Ophthalmol. Soc. UK 1990, 20, 190–192. [Google Scholar]
- Dent, C. Case of fragilitas ossium. Trans. Med. Soc. Lond. 1897, 20, 339–342. [Google Scholar]
- Fisch, L. The aetiology of congenital deafness and audiometric patterns. J. Laryngol. Otol. 1955, 69, 479–493. [Google Scholar] [CrossRef]
- Fraser, G. The causes of profound deafness in childhood. In Sensorineural Hearing Loss; Churchill: London, UK, 1970; pp. 3–35. [Google Scholar]
- Konigsmark, B.W. Syndromal approaches to the nosology of hereditary deafness. Birth Defects Orig. Artic. Ser. 1971, 7, 2–17. [Google Scholar]
- Konigsmark, B.; Gorlin, R. Genetic and Metabolic Deafness; W. B. Saunders Company: Philadelphia, PA, USA, 1976. [Google Scholar]
- McKusick, V. Mendelian Inheritance in Man: Catalogs of Autosomal Dominant, Autosomal Recessive and X-Linked Phenotypes; Johns Hopkins University Press: Baltimore, MD, USA, 1966. [Google Scholar]
- McKusick, V. Mendelian Inheritance in Man: A Catalog of Human Genes and Genetic Disorders; Johns Hopkins University Press: Baltimore, MD, USA, 1994. [Google Scholar]
- Hamosh, A.; Scott, A.F.; Amberger, J.; Valle, D.; McKusick, V.A. Online Mendelian Inheritance in Man (OMIM). Hum. Mutat. 2000, 15, 57–61. [Google Scholar] [CrossRef]
- Brunner, H.G.; van Bennekom, C.A.; Lambermon, E.; Oei, T.L.; Cremers, C.W.R.J.; Wieringa, B.; Ropers, H.-H. The gene for X-linked progressive mixed deafness with perilymphatic gusher during stapes surgery (DFN3) is linked to PGK. Qual. Life Res. 1988, 80, 337–340. [Google Scholar] [CrossRef]
- Wallis, C.; Ballo, R.; Wallis, G.; Beighton, P.; Goldblatt, J. X-linked mixed deafness with stapes fixation in a Mauritian kindred: Linkage to Xq probe pDP34. Genomics 1988, 3, 299–301. [Google Scholar] [CrossRef]
- De Kok, Y.J.; van der Maarel, S.M.; Bitner-Glindzicz, M.; Huber, I.; Monaco, A.P.; Malcolm, S.; Pembrey, M.E.; Ropers, H.H.; Cremers, F.P. Association between X-linked mixed deafness and mutations in the POU domain gene POU3F4. Science 1995, 267, 685–688. [Google Scholar] [CrossRef]
- Leon, P.E.; Raventos, H.; Lynch, E.; Morrow, J.; King, M.-C. The gene for an inherited form of deafness maps to chromosome 5q31. Proc. Natl. Acad. Sci. USA 1992, 89, 5181–5184. [Google Scholar] [CrossRef]
- Lynch, E.D.; Lee, M.K.; Morrow, J.E.; Welcsh, P.L.; León, P.E.; King, M.-C. Nonsyndromic Deafness DFNA1 Associated with Mutation of a Human Homolog of the Drosophila Gene diaphanous. Science 1997, 278, 1315–1318. [Google Scholar] [CrossRef] [PubMed]
- Guilford, P.; Ben Arab, S.; Blanchard, S.; Levilliers, J.; Weissenbach, J.; Belkahia, A.; Petit, C. A non–syndromic form of neurosensory, recessive deafness maps to the pericentromeric region of chromosome 13q. Nat. Genet. 1994, 6, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Kelsell, D.P.; Dunlop, J.; Stevens, H.P.; Lench, N.; Liang, J.N.; Parry, G.; Mueller, R.F.; Leigh, I.M. Connexin 26 mutations in hereditary non-syndromic sensorineural deafness. Nat. Cell Biol. 1997, 387, 80–83. [Google Scholar] [CrossRef]
- Online Mendelian Inheritance in Man, OMIM®; McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University: Baltimore, MD, USA. Available online: http://omim.org (accessed on 1 January 2024).
- Waddington, C.H. The epigenotype. Int. J. Epidemiol. 2012, 41, 10–13. [Google Scholar] [CrossRef]
- Dupont, C.; Armant, D.R.; Brenner, C.A. Epigenetics: Definition, mechanisms and clinical perspective. Semin. Reprod. Med. 2009, 27, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.D.; Crick, F.H.C. Molecular Structure of Nucleic Acids: A Structure for Deoxyribose Nucleic Acid. Nature 1953, 171, 737–738. [Google Scholar] [CrossRef] [PubMed]
- Nanney, D.L. Epigenetic control systems. Proc. Natl. Acad. Sci. USA 1958, 44, 712–717. [Google Scholar] [CrossRef]
- Deans, C.; Maggert, K.A. What Do You Mean, “Epigenetic”? Genetics 2015, 199, 887–896. [Google Scholar] [CrossRef]
- Henikoff, S.; Matzke, M. Exploring and explaining epigenetic effects. Trends Genet. 1997, 13, 293–295. [Google Scholar] [CrossRef]
- Egger, G.; Liang, G.; Aparicio, A.; Jones, P. Epigenetics in human disease and prospects for epigenetic therapy. Nature 2004, 429, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Gemmati, D.; Longo, G.; Gallo, I.; Silva, J.A.; Secchiero, P.; Zauli, G.; Hanau, S.; Passaro, A.; Pellegatti, P.; Pizzicotti, S.; et al. Host genetics impact on SARS-CoV-2 vaccine-induced immunoglobulin levels and dynamics: The role of TP53, ABO, APOE, ACE2, HLA-A, and CRP genes. Front. Genet. 2022, 13, 1028081. [Google Scholar] [CrossRef] [PubMed]
- Boison, D.; Rho, J.M. Epigenetics and epilepsy prevention: The therapeutic potential of adenosine and metabolic therapies. Neuropharm 2020, 167, 107741. [Google Scholar] [CrossRef] [PubMed]
- Tisato, V.; Zauli, G.; Rimondi, E.; Gianesini, S.; Brunelli, L.; Menegatti, E.; Zamboni, P.; Secchiero, P. Inhibitory effect of natural anti-inflammatory compounds on cytokines released by chronic venous disease patient-derived endothelial cells. Mediat. Inflamm. 2013, 2013, 423407. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Obri, A.; Serra, D.; Herrero, L.; Mera, P. The role of epigenetics in the development of obesity. Biochem. Pharmacol. 2020, 177, 113973. [Google Scholar] [CrossRef]
- Shamsi, M.B.; Firoz, A.S.; Imam, S.N.; Alzaman, N.; Samman, M.A. Epigenetics of human diseases and scope in future therapeutics. J. Taibah. Univ. Med. Sci. 2017, 12, 205–211. [Google Scholar] [CrossRef]
- Davis, K.N.; Qu, P.P.; Ma, S.; Lin, L.; Plastini, M.; Dahl, N.; Plazzi, G.; Pizza, F.; O’Hara, R.; Wong, W.H.; et al. Mutations in human DNA methyltransferase DNMT1 induce specific genome-wide epigenomic and transcriptomic changes in neurodevelopment. Hum. Mol. Genet. 2023, 17, 3105–3120. [Google Scholar] [CrossRef]
- Riccardi, V.M. Cell--cell interaction as an epigenetic determinant in the expression of mutant neural crest cells. Birth Defects Orig. Artic. Ser. 1979, 15, 89–98. [Google Scholar]
- Xiao, Y.; Li, D. The role of epigenetic modifications in sensory hair cell development, survival, and regulation. Front. Cell. Neurosci. 2023, 14, 1210279. [Google Scholar] [CrossRef]
- Nguyen, J.D.; Llamas, J.; Shi, T.; Crump, J.G.; Groves, A.K.; Segil, N. DNA methylation in the mouse cochlea promotes maturation of supporting cells and contributes to the failure of hair cell regeneration. Proc. Natl. Acad. Sci. USA 2023, 15, e2300839120. [Google Scholar] [CrossRef]
- Zou, S.; Zheng, Q.; Sun, Y.; Fu, X.; Zhou, W.; He, Z. Editorial: Hearing loss: From pathogenesis to treatment, volume II. Front. Cell. Neurosci. 2023, 23, 1309592. [Google Scholar] [CrossRef]
- Tisato, V.; Castiglione, A.; Ciorba, A.; Aimoni, C.; Silva, J.A.; Gallo, I.; D’Aversa, E.; Salvatori, F.; Bianchini, C.; Pelucchi, S.; et al. LINE-1 global DNA methylation, iron homeostasis genes, sex and age in sudden sensorineural hearing loss (SSNHL). Hum. Genom. 2023, 14, 112. [Google Scholar] [CrossRef] [PubMed]
- Gemmati, D.; Tisato, V. Chapter 15—Genetics and epigenetics of the one-carbon metabolism pathway in autism spectrum disorder: Role of a sex-specific brain epigenome. In Sex, Gender, and Epigenetics; Legato, M.J., Feldberg, D., Glezerman, M., Eds.; Academic Press: Cambridge, UK, 2023; pp. 181–191. [Google Scholar]
- Gemmati, D.; Tisato, V. Chapter 24—Genomic and epigenomic signature at the branch-point among genome, phenome, and sexome in health and disease: A multiomics approach. In Principles of Gender-Specific Medicine; Academic Press: Cambridge, UK, 2023; pp. 393–408. [Google Scholar]
- Tisato, V.; Silva, J.A.; Longo, G.; Gallo, I.; Singh, A.V.; Milani, D.; Gemmati, D. Genetics and epigenetics of one-carbon metabolism pathway in autism spectrum disorder: A sex-specific brain epigenome? Genes 2021, 12, 782. [Google Scholar] [CrossRef]
- Zhou, Q.; Xiong, Y.; Qu, B.; Bao, A.; Zhang, Y. DNA methylation and recurrent pregnancy loss: A mysterious compass? Front. Immunol. 2021, 12, 738962. [Google Scholar] [CrossRef] [PubMed]
- Gemmati, D.; Tognazzo, S.; Serino, M.L.; Fogato, L.; Carandina, S.; De Palma, M.; Izzo, M.; De Mattei, M.; Ongaro, A.; Scapoli, G.L.; et al. Factor XIII V34L polymorphism modulates the risk of chronic venous leg ulcer progression and extension. Wound Repair. Regen. 2004, 12, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Seker Yildiz, K.; Durmus, K.; Donmez, G.; Arslan, S.; Altuntas, E.E. Studying the association between sudden hearing loss and DNA N-methyltransferase 1 (DNMT1) genetic polymorphism. J. Int. Adv. Otol. 2017, 13, 313–317. [Google Scholar] [CrossRef]
- Ma, P.W.; Wang, W.L.; Chen, J.W.; Yuan, H.; Lu, P.H.; Gao, W.; Ding, X.-R.; Lun, Y.-Q.; Liang, R.; He, Z.-H.; et al. Treatment with the ferroptosis inhibitor ferrostatin-1 attenuates noise-induced hearing loss by suppressing ferroptosis and apoptosis. Oxid. Med. Cell. Longev. 2022, 2022, 3373828. [Google Scholar] [CrossRef]
- Gemmati, D.; Castiglione, A.; Vigliano, M.; Ciorba, A.; Aimoni, C. Sudden sensorineural hearing loss and polymorphisms in iron homeostasis genes. In Handbook of Hearing Disorders Research; Nova Science Publishers: New York, NY, USA, 2015; pp. 77–84. [Google Scholar]
- Wilson, B.S.; Tucci, D.L.; Moses, D.A.; Chang, E.F.; Young, N.M.; Zeng, F.-G.; Lesica, N.A.; Bur, A.M.; Kavookjian, H.; Mussatto, C.; et al. Harnessing the Power of Artificial Intelligence in Otolaryngology and the Communication Sciences. J. Assoc. Res. Otolaryngol. 2022, 23, 319–349. [Google Scholar] [CrossRef]
- National Human Genome Research Institute. A Brief Guide to Genomics. Available online: https://www.genome.gov (accessed on 10 January 2024).
- Cho, S.H.; Yun, Y.; Lee, D.H.; Cha, J.H.; Lee, S.M.; Lee, J.; Suh, M.H.; Lee, J.H.; Oh, S.H.; Park, M.K.; et al. Novel autosomal dominant TMC1 variants linked to hearing loss: Insight into protein-lipid interactions. BMC Med. Genom. 2023, 16, 320. [Google Scholar] [CrossRef]
- Sethukumar, P.; Mandavia, R.; Yildirim, O.; Hazell, G.; Devakumar, H.; Ahmed, M.; Stragier, E.; Duran, M.J.; Schilder, A.G.M.; Mehta, N. Cataloging Existing Hearing Loss Cohort Data to Guide the Development of Precision Medicine for Sensorineural Hearing Loss: A Systematic Review of Hearing Repositories. J. Int. Adv. Otol. 2023, 19, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wen, J.; Liu, X.; Chen, A.; Li, S.; Liu, J.; Sun, J.; Gong, W.; Kang, X.; Feng, Z.; et al. Gene regulation analysis of patient-derived iPSCs and its CRISPR-corrected control provides a new tool for studying perturbations of ELMOD3 c.512A>G mutation during the development of inherited hearing loss. PLoS ONE 2023, 18, e0288640. [Google Scholar] [CrossRef] [PubMed]
- Azaiez, H.; Booth, K.T.; Ephraim, S.S.; Crone, B.; Black-Ziegelbein, E.A.; Marini, R.J.; Shearer, A.E.; Sloan-Heggen, C.M.; Kolbe, D.; Casavant, T.; et al. Genomic Landscape and Mutational Signatures of Deafness-Associated Genes. Am. J. Hum. Genet. 2018, 103, 484–497. [Google Scholar] [CrossRef] [PubMed]
- Hahn, R.; Avraham, K.B. Gene Therapy for Inherited Hearing Loss: Updates and Remaining Challenges. Audiol. Res. 2023, 13, 952–966. [Google Scholar] [CrossRef]
- Wilkins, M.R.; Sanchez, J.C.; Gooley, A.A.; Appel, R.D.; Humphery-Smith, I.; Hochstrasser, D.F.; Williams, K.L. Progress with proteome projects: Why all proteins expressed by a genome should be identified and how to do it. Biotechnol. Genet. Eng. Rev. 1996, 13, 19–50. [Google Scholar] [CrossRef] [PubMed]
- Thalmann, I. Proteomics and the inner ear. Dis. Markers 2001, 17, 476738. [Google Scholar] [CrossRef] [PubMed]
- Jamesdaniel, S.; Salvi, R.; Coling, D. Auditory proteomics: Methods, accomplishments and challenges. Brain Res. 2009, 1277, 24–36. [Google Scholar] [CrossRef]
- Chance, M.R.; Chang, J.; Liu, S.; Gokulrangan, G.; Chen, D.H.; Lindsay, A.; Geng, R.; Zheng, Q.Y.; Alagramam, K. Proteomics, bioinformatics and targeted gene expression analysis reveals up-regulation of cochlin and identifies other potential biomarkers in the mouse model for deafness in Usher syndrome type 1F. Hum. Mol. Genet. 2010, 19, 1515–1527. [Google Scholar] [CrossRef]
- Dossena, S.; Nofziger, C.; Lang, F.; Valenti, G.; Paulmichl, M. The ESF meeting on “The proteomics, epigenetics and pharmacogenetics of pendrin”. Cell. Physiol. Biochem. 2011, 28, 377–784. [Google Scholar] [CrossRef]
- Mateo Sánchez, S.; Freeman, S.D.; Delacroix, L.; Malgrange, B. The role of post-translational modifications in hearing and deafness. Cell. Mol. Life Sci. 2016, 73, 3521–3533. [Google Scholar] [CrossRef]
- Zheng, Q.Y.; Rozanas, C.R.; Thalmann, I.; Chance, M.R.; Alagramam, K.N. Inner ear proteomics of mouse models for deafness, a discovery strategy. Brain Res. 2006, 1091, 113–121. [Google Scholar] [CrossRef]
- Cepeda, A.P.; Ninov, M.; Neef, J.; Parfentev, I.; Kusch, K.; Reisinger, E.; Jahn, R.; Moser, T.; Urlaub, H. Proteomic analysis reveals the composition of glutamatergic organelles of auditory inner hair cell. Mol. Cell. Proteom. 2023, 23, 100704. [Google Scholar] [CrossRef]
- Street, K.; Risso, D.; Fletcher, R.B.; Das, D.; Ngai, J.; Yosef, N.; Purdom, E.; Dudoit, S. Slingshot: Cell lineage and pseudotime inference for single-cell transcriptomics. BMC Genom. 2018, 19, 477. [Google Scholar] [CrossRef]
- Ma, X.; Guo, J.; Tian, M.; Fu, Y.; Jiang, P.; Zhang, Y.; Chai, R. Advance and Application of Single-cell Transcriptomics in Auditory Research. Neurosci. Bull. 2023. [Google Scholar] [CrossRef]
- Malesci, R.; Lombardi, M.; Abenante, V.; Fratestefano, F.; Del Vecchio, V.; Fetoni, A.R.; Troisi, J. A Systematic Review on Metabolomics Analysis in Hearing Impairment: Is It a Possible Tool in Understanding Auditory Pathologies? Int. J. Mol. Sci. 2023, 24, 15188. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Gao, Y.; Jiang, R. Diagnostic and Predictive Values of Serum Metabolic Profiles in Sudden Sensorineural Hearing Loss Patients. Front. Mol. Biosci. 2022, 9, 982561. [Google Scholar] [CrossRef] [PubMed]
- Miao, L.; Zhang, J.; Yin, L.; Pu, Y. Metabolomics Analysis Reveals Alterations in Cochlear Metabolic Profiling in Mice with Noise-Induced Hearing Loss. BioMed. Res. Int. 2022, 2022, 9548316. [Google Scholar] [CrossRef] [PubMed]
- Pierre, P.V.; Haglöf, J.; Linder, B.; Engskog, M.K.R.; Arvidsson, T.; Pettersson, C.; Fransson, A.; Laurell, G. Cisplatin-Induced Metabolome Changes in Serum: An Experimental Approach to Identify Markers for Ototoxicity. Acta. Oto-Laryngol. 2017, 137, 1024–1030. [Google Scholar] [CrossRef]
- Ishibashi, R.; Hirayama, K.; Watanabe, S.; Okano, K.; Kuroda, Y.; Baba, Y.; Kanayama, T.; Ito, C.; Kasahara, K.; Aiba, S.; et al. Imeglimin-mediated glycemic control in maternally inherited deafness and diabetes. Diabetes Investig. 2023, 14, 1419–1422. [Google Scholar] [CrossRef]
- Vila-Sanjurjo, A.; Mallo, N.; Atkins, J.F.; Elson, J.L.; Smith, P.M. Our current understanding of the toxicity of altered mito-ribosomal fidelity during mitochondrial protein synthesis: What can it tell us about human disease? Front. Physiol. 2023, 14, 1082953. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, Y.; LeCun, Y.; Sahani, M.; Precup, D.; Silver, D.; Sugiyama, M.; Uchibe, E.; Morimoto, J. Deep learning, reinforcement learning, and world models. Neural. Netw. 2022, 152, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Tang, F.; Hua, Y.; Li, X. In silico prediction of drug-induced ototoxicity using machine learning and deep learning methods. Chem. Biol. Drug. Des. 2021, 98, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Teng, L.; Zuo, W.; Zhong, S.; Xu, Y.; Sun, J. Deafness gene screening based on a multilevel cascaded BPNN model. BMC Bioinform. 2023, 24, 56. [Google Scholar] [CrossRef] [PubMed]
- Jin, F.Q.; Huang, O.; Kleindienst Robler, S.; Morton, S.; Platt, A.; Egger, J.R.; Emmett, S.D.; Palmeri, M.L. A Hybrid Deep Learning Approach to Identify Preventable Childhood Hearing Loss. Ear Heart 2023, 44, 1262–1270. [Google Scholar] [CrossRef]
- Parton, B.S. Sign language recognition and translation: A multidisciplined approach from the field of artificial intelligence. J. Deaf. Stud. Deaf. Educ. 2006, 11, 94–101. [Google Scholar] [CrossRef]
- Wen, F.; Zhang, Z.; He, T.; Lee, C. AI enabled sign language recognition and VR space bidirectional communication using triboelectric smart glove. Nat. Commun. 2021, 12, 5378. [Google Scholar] [CrossRef]
- Lin, B.; Ma, Y.; Wu, S. Multi-Omics and Artificial Intelligence-Guided Data Integration in Chronic Liver Disease: Prospects and Challenges for Precision Medicine. OMICS 2022, 26, 415–421. [Google Scholar] [CrossRef]
| Vegetable Hybridists | Hereditarists |
|---|---|
| Prospero Alpini (also known as Prosperus Alpinus, Prosper Alpinus, Prospero Alpinio) (Marostica 1553–Padua 1616) Adam Zaluziansky (Mnichov Hradiště 1558–Prague 1613) Nehemiah Grew (Atherstone 1641–London 1712) Rudolf Jakob Camerer (Tübingen 1665–Tübingen 1721) Carl von Linné (Råshult 1707–Uppsala 1778) Gottlieb Joseph Kölreuter (Sulz am Neckar 1733–Karlsruhe 1806) Thomas Andrew Knight (Wormsley 1759–London 1838) Augustin Sageret (Paris 1763–Paris 1851) Carl Friedrich von Gärtner (Göppingen 1772–Calw 1850) Henri Lecoq (Avesnes-sur-Helpe 1802–Clermont Ferrand 1871) Dominique Alexandre Godron (Hayange 1807–Nancy 1880) Charles-Victor Naudin (Autun 1815–Antibes 1899) Max Ernt Wichura (Neisse 1817–Berlin 1866) | William Wollaston (Coton–Clanford 1660–London 1724) Pierre-Louis Moreau de Maupertuis (Saint-Malo 1698–Basilea 1759) Georges-Louis Leclerc de Buffon (Montbard 1707–Paris1788) Charles Darwin (Shrewsbury 1809–Downe 1882) Karl Wilhelm von Nägeli (Kilchberg 1817–Munich 1891) Herbert Spencer (Derby 1820–Brighton 1903) Francis Galton (Sparkbrook 1822–Haslemere 1911) Thomas Henry Huxley (Ealing 1825–Eastbourn 1895) |
| French School | German School |
|---|---|
| Antoine Saissy (1756–1822) Jean Marc Gaspard Itard (1775–1838) Gilbert Breschet (1784–1845) Pierre-Marie Flourens (1794–1867) Nicholas Deleau the Younger (1797–1862) Prosper Menière (1798–1862) Marcellin Emile Hubert-Valleroux (1812–1884) Alexandre Louis Paul Blanchet (1819–1867) | Ernst Heinrich Weber (1795–1878) Emil Huschke (1797–1858) Wilhelm Kramer (1801–1875) Eduard Schmalz (1801–1871) Carl Gustav Lincke (1804–1849) Gabriel Gustav Valentin (1810–1883) Hermann von Helmholtz (1821–1894) Ernst Reissner (1824–1878) Anton Friedrich von Tröltsch (1828–1867) Otto Friedrich Karl Deiters (1834–1863) Ádám Politzer (1835–1920) Hermann Schwartze (1837–1910) |
| English school | Italian school |
| William Robert Wilde (1773–1860) John Cunningham Saunders (1773–1810) William Wright (1773–1860) Samuel Akery (1785–1845) Henry Jones Shrapnell (1792–1834) James Yearsley (1805–1869) Joseph Toynbee (1815–1866) | Carlo Giovanni Brugnone (1741–1816) Alfonso Corti (1822–1876) Demetrio Bargellini (1823–1899) Giuseppe Gradenigo (1859–1926) Vittorio Grazzi (1849–1929) Vincenzo Cozzolino (1853–1911) |
| Period | Discoveries |
|---|---|
| 1866 | Ernst Heinrich Haeckel (Potsdam 1834–Jena 1919), in 1866, proposed that the nucleus contained the factors responsible for the transmission of hereditary traits. |
| 1869 | Johann Friedrich Miescher (Basel 1844–Davos 1895) identified in 1869, inside the nuclei of human white blood cells, ‘nuclein’, the molecule now known as DNA |
| 1870s | Walther Flemming (Schwerin 1843–Kiel 1905) in the 1870s described the morphology of a fibrous structure within the nucleus of cells, named ‘chromatin’, now known as chromosomes. By observing this chromatin, Flemming correctly worked out how chromosomes separate during cell division, also known as mitosis. |
| since 1879 | Ludwig Karl Martin Leonhard Albrecht Kossel (Rostock 1853–Heidelberg 1927) made great progress in understanding the basic building blocks of nuclein. Kossel isolated the five nucleotide bases that are the building blocks of DNA and RNA: adenine, cytosine, guanine, thymine, and uracil. In 1881, Kossel identified nuclein as a nucleic acid and provided its present chemical name, deoxyribonucleic acid (DNA). |
| since the 1880s | Theodor Boveri (Bamberg 1862–Würzburg 1915) first presented the idea that the genetic material passed down from parent to child is within the chromosomes. |
| since 1905 | Walter Stanborough Sutton (Utica 1877–Kansas City 1916) expanded on Theodor’s observation. He found it was possible to distinguish individual chromosomes undergoing meiosis in the testes of the grasshopper and identified the sex chromosome. |
| since 1905 | Phoebus Aaron Theodor Levene (Sagor 1869–New York 1940), and his student J. A. Mandel, described a linear complex with a phosphoric acid and a base forming a subunit they called a mononucleotide, with two or more mononucleotides bound together to form what they called a polyphosphoric acid, or polynucleotide. |
| since 1910 | Thomas H. Morgan (Lexington 1866–Pasadena 1945) and his students (Alfred Sturtevant, Calvin Bridges, Hermann Muller, and others), provided the proof for the chromosomal theory of heredity, genetic linkage, and chromosomal crossing over and non-disjunction. |
| 1928 | Frederick Griffith (Prescott 1879–London 1941) performed important studies on Bacterial transformation. |
| 1944 | Oswald Avery (Halifax 1877–Nashville1955). In 1944, he and his colleagues Maclyn McCarty and Colin MacLeod reported that the transforming substance, the genetic material of the cell, was DNA. |
| 1950 | Erwin Chargaff (Černivci 1905–New York 2002) found that in DNA, the ratios of adenine (A) to thymine (T) and guanine (G) to cytosine (C) are equal. |
| 1951–1952 | Maurice Hugh Frederick Wilkins (Pongaroa 1916–London 2004) and Rosalind Franklin (Kensington 1920–Chelsea 1958), at King’s College London, used X-ray diffraction to study the structure of DNA in solution. They found that DNA could take two forms: crystalline or A form, and paracrystalline or B form, as «big helix with several chains, phosphates on outside, phosphate–phosphate interhelical bonds, disrupted by water». |
| 1953 | J. D. Watson, F. H. C. Crick. Molecular structure of nucleic acids. A Structure for Deoxyribose Nucleic Acid. Nature 4356 April 25: 737-38, 1953 M. H. F. Wilkins, A. R. Stokes, H. R. Wilson. Molecular Structure of Deoxypentose Nucleic Acids. Nature 4356 April 25: 738-40, 1953 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martini, A.; Cozza, A.; Di Pasquale Fiasca, V.M. The Inheritance of Hearing Loss and Deafness: A Historical Perspective. Audiol. Res. 2024, 14, 116-128. https://doi.org/10.3390/audiolres14010010
Martini A, Cozza A, Di Pasquale Fiasca VM. The Inheritance of Hearing Loss and Deafness: A Historical Perspective. Audiology Research. 2024; 14(1):116-128. https://doi.org/10.3390/audiolres14010010
Chicago/Turabian StyleMartini, Alessandro, Andrea Cozza, and Valerio Maria Di Pasquale Fiasca. 2024. "The Inheritance of Hearing Loss and Deafness: A Historical Perspective" Audiology Research 14, no. 1: 116-128. https://doi.org/10.3390/audiolres14010010
APA StyleMartini, A., Cozza, A., & Di Pasquale Fiasca, V. M. (2024). The Inheritance of Hearing Loss and Deafness: A Historical Perspective. Audiology Research, 14(1), 116-128. https://doi.org/10.3390/audiolres14010010








