Sleep Quality and Its Relationship to Anxiety and Hardiness in a Cohort of Frontline Italian Nurses during the First Wave of the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Methods
2.4. Outcome Measures
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Acknowledgments
Conflicts of Interest
References
- Baranwal, N.; Yu, P.K.; Siegel, N.S. Sleep physiology, pathophysiology, and sleep hygiene. Prog. Cardiovasc. Dis. 2023, 77, 59–69. [Google Scholar] [CrossRef]
- Zhang, C.; Yang, L.; Liu, S.; Ma, S.; Wang, Y.; Cai, Z.; Du, H.; Li, R.; Kang, L.; Su, M.; et al. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front. Psychiatry 2020, 11, 306. [Google Scholar] [CrossRef]
- Roman, P.; Perez-Cayuela, I.; Gil-Hernández, E.; Rodriguez-Arrastia, M.; Aparicio-Mota, A.; Ropero-Padilla, C.; Rueda-Ruzafa, L. Influence of Shift Work on The Health of Nursing Professionals. J. Pers. Med. 2023, 13, 627. [Google Scholar] [CrossRef]
- Zhang, L.; Sun, D.M.; Li, C.B.; Tao, M.F. Influencing Factors for Sleep Quality Among Shift-working Nurses: A Cross-Sectional Study in China Using 3-factor Pittsburgh Sleep Quality Index. Asian Nurs. Res. 2016, 10, 277–282. [Google Scholar] [CrossRef]
- Zangeneh Soroush, M.; Tahvilian, P.; Koohestani, S.; Maghooli, K.; Dabanloo, N.J.; Kadijani, M.S.; Jahantigh, S.; Zangeneh Soroush, M.; Saliani, A. Effects of COVID-19-related psychological distress and anxiety on quality of sleep and life in healthcare workers in Iran and three European countries. Front. Public Health 2022, 10, 997626. [Google Scholar] [CrossRef]
- Membrive-Jiménez, M.J.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Velando-Soriano, A.; Ariza, T.; De la Fuente-Solana, E.I.; Cañadas-De la Fuente, G.A. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 954. [Google Scholar] [CrossRef]
- Dos Santos, M.A.; Pereira, F.H.; DE Souza Caliari, J.; Oliveira, H.C.; Ceolim, M.F.; Andrechuk, C.R.S. Sleep and Professional Burnout in Nurses, Nursing Technicians, and Nursing Assistants During the COVID-19 Pandemic. J. Nurs. Res. 2022, 30, e218. [Google Scholar] [CrossRef]
- Li, J.; Vitiello, M.V.; Gooneratne, N.S. Sleep in Normal Aging. Sleep Med. Clin. 2022, 17, 161–171. [Google Scholar] [CrossRef]
- Xia, L.; Chen, C.; Liu, Z.; Luo, X.; Guo, C.; Liu, Z.; Zhang, K.; Liu, H. Prevalence of Sleep Disturbances and Sleep Quality in Chinese Healthcare Workers During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Front. Psychiatry 2021, 12, 646342. [Google Scholar] [CrossRef]
- Ielapi, N.; Andreucci, M.; Bracale, U.M.; Costa, D.; Bevacqua, E.; Bitonti, A.; Mellace, S.; Buffone, G.; Candido, S.; Provenzano, M.; et al. Insomnia Prevalence among Italian Night-Shift Nurses. Nurs. Rep. 2021, 11, 530–535. [Google Scholar] [CrossRef]
- Okechukwu, C.E.; Colaprico, C.; Di Mario, S.; Oko-oboh, A.G.; Shaholli, D.; Manai, M.V.; La Torre, G. The Relationship between Working Night Shifts and Depression among Nurses: A Systematic Review and Meta-Analysis. Healthcare 2023, 11, 937. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, S.; Liu, M.; Gan, G.; Qin, N.; Luo, X.; Zhang, C.; Xie, J.; Wang, K.; Cheng, A.S. The role of sleep quality and perceived stress on depressive symptoms among tertiary hospital nurses: A cross-sectional study. BMC Psychiatry 2023, 23, 416. [Google Scholar] [CrossRef]
- Park, E.; Lee, H.Y.; Park, C.S. Association between sleep quality and nurse productivity among Korean clinical nurses. J. Nurs. Manag. 2018, 26, 1051–1058. [Google Scholar] [CrossRef]
- Stimpfel, A.W.; Fatehi, F.; Kovner, C. Nurses’ sleep, work hours, and patient care quality, and safety. Sleep Health 2020, 6, 314–320. [Google Scholar] [CrossRef]
- Dragioti, E.; Tsartsalis, D.; Mentis, M.; Mantzoukas, S.; Gouva, M. Impact of the COVID-19 pandemic on the mental health of hospital staff: An umbrella review of 44 meta-analyses. Int. J. Nurs. Stud. 2022, 131, 104272. [Google Scholar] [CrossRef]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Ghasemi, H.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Khaledi-Paveh, B.; Hosseinian-Far, M. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: A systematic review and meta-analysis. Global Health 2020, 16, 92. [Google Scholar] [CrossRef]
- Aslan, S.; Dinç, M. Examining the relationship between nurses’ fear levels and insomnia during the COVID-19 pandemic in Turkey. Perspect. Psychiatr. Care 2022, 58, 54–60. [Google Scholar] [CrossRef]
- Da’she, A.; Obaid, O.; Rababa, M. Psychological impact of coronavirus disease on nurses exposed and non-exposed to disease. Int. J. Afr. Nurs. Sci. 2022, 17, 100442. [Google Scholar]
- Sis Çelik, A.; Sönmez, T. Comparison of the Fear Levels and Sleep Problems of Nurses Working in Wards Where Patients with and without COVID-19 Are Hospitalized: A Study from Turkey. Psychiatr. Danub. 2021, 33 (Suppl. S13), 357–363. [Google Scholar]
- Cho, O.H.; Yoon, J.; Kim, M. Influencing factors of fatigue among public health nurses during the COVID-19 pandemic: A cross-sectional study. Public Health Nurs. 2023, 40, 80–89. [Google Scholar] [CrossRef]
- Chutiyami, M.; Cheong, A.M.Y.; Salihu, D.; Bello, U.M.; Ndwiga, D.; Maharaj, R.; Naidoo, K.; Kolo, M.A.; Jacob, P.; Chhina, N.; et al. COVID-19 Pandemic and Overall Mental Health of Healthcare Professionals Globally: A Meta-Review of Systematic Reviews. Front. Psychiatry 2022, 12, 804525. [Google Scholar] [CrossRef]
- Danet Danet, A. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clin. 2021, 156, 449–458. [Google Scholar] [CrossRef]
- Staner, L. Sleep and anxiety disorders. Dialogues Clin. Neurosci. 2003, 5, 249–258. [Google Scholar] [CrossRef]
- Liu, X.; Xu, Y.; Xu, H.; Jiang, L.; Wang, T.; Chen, C.; Lee, A.; Zhu, P. Anxiety and sleep quality among front-line nurses treating first wave COVID-19 in China: The mediating role of mindfulness. Arch. Psychiatr. Nurs. 2022, 41, 341–347. [Google Scholar] [CrossRef]
- Chigwedere, O.C.; Sadath, A.; Kabir, Z.; Arensman, E. The Impact of Epidemics and Pandemics on the Mental Health of Healthcare Workers: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6695. [Google Scholar] [CrossRef]
- Kandula, U.R.; Wake, A.D. Assessment of Quality of Life Among Health Professionals During COVID-19: Review. J. Multidiscip. Healthc. 2021, 14, 3571–3585. [Google Scholar] [CrossRef]
- Altun Uğraş, G.; Yüksel, S.; Kettaş Dölek, E.; Erden, S.; Şirin, K. Health Problems and Reasons for Stress of Intensive Care Nurses During COVID-19. Florence Nightingale J. Nurs. 2022, 30, 55–63. [Google Scholar] [CrossRef]
- Jiménez-Fernández, R.; Corral-Liria, I.; Trevissón-Redondo, B.; Lopez-Lopez, D.; Losa-Iglesias, M.; Becerro-de-Bengoa-Vallejo, R. Burnout, resilience and psychological flexibility in frontline nurses during the acute phase of the COVID-19 pandemic (2020) in Madrid, Spain. J. Nurs. Manag. 2022, 30, 2549–2556. [Google Scholar] [CrossRef]
- Choi, H.J.; Yang, C.M.; Lee, S.Y.; Lee, H.J.; Jang, S.H. Mental Health and Quality of Life for Healthcare Workers in a University Hospital Under COVID-19. Psychiatry Investig. 2022, 19, 85–91. [Google Scholar] [CrossRef]
- Zakeri, M.A.; Ghaedi-Heidari, F.; Khaloobagheri, E.; Hossini Rafsanjanipoor, S.M.; Ganjeh, H.; Pakdaman, H.; Abbasifard, M.; Mehdizadeh, M.; Zakeri Bazmandeh, A.; Dehghan, M. The Relationship Between Nurse’s Professional Quality of Life, Mindfulness, and Hardiness: A Cross-Sectional Study During the COVID-19 Outbreak. Front. Psychol. 2022, 13, 866038. [Google Scholar] [CrossRef]
- Hwang, S.; Lee, J. The influence of COVID-19-related resilience on depression, job stress, sleep quality, and burnout among intensive care unit nurses. Front. Psychol. 2023, 14, 1168243. [Google Scholar] [CrossRef] [PubMed]
- Jose, S.; Dhandapani, M.; Cyriac, M.C. Burnout and Resilience among Frontline Nurses during COVID-19 Pandemic: A Cross-sectional Study in the Emergency Department of a Tertiary Care Center, North India. Indian J. Crit. Care Med. 2020, 24, 1081–1088. [Google Scholar]
- Labrague, L.J. Pandemic fatigue and clinical nurses’ mental health, sleep quality and job contentment during the COVID-19 pandemic: The mediating role of resilience. J. Nurs. Manag. 2021, 29, 1992–2001. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Lai, J.; Wang, Y.; Huang, J.; Hu, S.; Wang, H. Mental health outcome and resilience among aiding Wuhan nurses: One year after the COVID-19 outbreak in China. J. Affect Disord. 2022, 297, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Maddi, S.R. The story of hardiness: Twenty Years of theorizing, research, and practice. Consult. Psychol. J. Pract. Res. 2002, 54, 173–185. [Google Scholar] [CrossRef]
- Kobasa, S.C.; Maddi, S.R.; Puccetti, M.C. Personality and exercise as buffers in the stress-illness relationship. J. Behav. Med. 1982, 5, 391–404. [Google Scholar] [CrossRef]
- Daly, L.M. Resilience: An integrated review. Nurs. Sci. Q. 2020, 33, 330–338. [Google Scholar] [CrossRef]
- Baldassini Rodriguez, S.; Bardacci, Y.; El Aoufy, K.; Bazzini, M.; Caruso, C.; Giusti, G.D.; Mezzetti, A.; Bambi, S.; Guazzini, A.; Rasero, L. Promoting and Risk Factors of Nurses’ Hardiness Levels during the COVID-19 Pandemic: Results from an Italian Cohort. Int. J. Environ. Res. Public Health 2022, 19, 1523. [Google Scholar] [CrossRef]
- Picardi, A.; Bartone, P.T.; Querci, R.; Bitetti, D.; Tarsitani, L.; Roselli, V.; Maraone, A.; Fabi, E.; De Michele, F.; Gaviano, I.; et al. Development and validation of the Italian version of the 15-item dispositional resilience scale. Riv Psichiatr. 2012, 47, 231–237. [Google Scholar] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ (Clin. Res. Ed.) 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Pedrabissi, L.; Santinello, M. Verifica della validità dello STAI forma Y di Spielberger [Verification of the validity of the STAI, Form Y, by Spielberger]. Giunti Organ. Spec. 1989, 191–192, 11–14. [Google Scholar]
- Castronovo, V.; Galbiati, A.; Marelli, S.; Brombin, C.; Cugnata, F.; Giarolli, L.; Anelli, M.M.; Rinaldi, F.; Ferini-Strambi, L. Validation study of the Italian version of the Insomnia Severity Index (ISI). Neurol. Sci. 2016, 37, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- Bartone, P.T. Test-retest reliability of the dispositional resilience scale-15, a brief hardiness scale. Psychol. Rep. 2007, 101, 943–944. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y.; Fong, D.Y.; Choi, A.W.; Chan, C.K.; Tiwari, A.; Chan, K.L.; Lai, V.; Logan, T.; Bartone, P. Transcultural and psychometric validation of the Dispositional Resilience Scale (DRS-15) in Chinese adult women. Qual. Life Res. 2014, 23, 2489–2494. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D. State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Ramanaiah, N.V.; Franzen, M.; Schill, T. A psychometric study of the State-Trait Anxiety Inventory. J. Pers. Assess. 1983, 47, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Manzar, M.D.; Jahrami, H.A.; Bahammam, A.S. Structural validity of the Insomnia Severity Index: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 60, 101531. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Macintosh, Version 27.0; IBM Corp: Armonk, NY, USA, 2020. [Google Scholar]
- García-Vivar, C.; Rodríguez-Matesanz, I.; San Martín-Rodríguez, L.; Soto-Ruiz, N.; Ferraz-Torres, M.; Escalada-Hernández, P. Analysis of mental health effects among nurses working during the COVID-19 pandemic: A systematic review. J. Psychiatr. Ment. Health Nurs. 2023, 30, 326–340. [Google Scholar] [CrossRef] [PubMed]
- Simonetti, V.; Durante, A.; Ambrosca, R.; Arcadi, P.; Graziano, G.; Pucciarelli, G.; Simeone, S.; Vellone, E.; Alvaro, R.; Cicolini, G. Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: A large cross-sectional study. J. Clin. Nurs. 2021, 30, 1360–1371. [Google Scholar] [CrossRef] [PubMed]
- Booker, L.A.; Magee, M.; Rajaratnam, S.M.W.; Sletten, T.L.; Howard, M.E. Individual vulnerability to insomnia, excessive sleepiness and shift work disorder amongst healthcare shift workers. A systematic review. Sleep Med. Rev. 2018, 41, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Liu, S.; Zhu, L.; Li, D.; Huang, D.; Deng, H.; Guo, H.; Huang, D.; Liao, Y.; Mao, Z.; et al. Prevalence and Related Factors of Insomnia Among Chinese Medical Staff in the Middle and Late Stage of COVID-19. Front. Psychiatry 2020, 11, 602315. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.-Q.; Tian, Q.; Leng, H.-X.; Du, J.-L.; et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Nashwan, A.J.; Villar, R.C.; Al-Qudimat, A.R.; Kader, N.; Alabdulla, M.; Abujaber, A.A.; Al-Jabry, M.M.; Harkous, M.; Philip, A.; Ali, R.; et al. Quality of Life, Sleep Quality, Depression, Anxiety, Stress, Eating Habits, and Social Bounds in Nurses during the Coronavirus Disease 2019 Pandemic in Qatar (The PROTECTOR Study): A Cross-Sectional, Comparative Study. J. Pers. Med. 2021, 11, 918. [Google Scholar] [CrossRef] [PubMed]
- Lambert, C.E., Jr.; Lambert, V.A. Hardiness: Its development and relevance to nursing. Image J. Nurs. Sch. 1987, 19, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Heesakkers, H.; Zegers, M.; van Mol, M.M.C.; van den Boogaard, M. The impact of the first COVID-19 surge on the mental well-being of ICU nurses: A nationwide survey study. Intensive Crit. Care Nurs. 2021, 65, 103034. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2021, 88, 901–907. [Google Scholar] [CrossRef]
- Setti, I.; Argentero, P. Vicarious trauma: A contribution to the Italian adaptation of the Secondary Traumatic Stress Scale in a sample of ambulance operators. Appl. Psychon. Bull. 2012, 264, 58–64. [Google Scholar]
| Dimension | μ/f | σ/% | CI 95% | Welch t/χ2 |
|---|---|---|---|---|
| Gender | ||||
| Total Sample | 1167 | 81.2% (F) | ||
| Sample COVID Yes | 383 | 76.8% (F) | 7.48 ** | |
| Sample COVID No | 784 | 83.4% (F) | ||
| Age | ||||
| Total Sample | 42.4 | 10.7 | 41.7–43.0 | |
| Sample COVID Yes | 40.9 | 10.3 | 39.9–42.0 | 3.29 *** |
| Sample COVID No | 43.1 | 10.8 | 42.3–43.8 | |
| Length of service | ||||
| Total Sample | 17.9 | 11.6 | 17.2–18.6 | |
| Sample COVID Yes | 16.6 | 11.3 | 15.5–17.7 | 2.74 ** |
| Sample COVID No | 18.5 | 11.7 | 17.7–19.4 | |
| Ward/ department transfer | ||||
| Total Sample | 324/1167 | 27.8% | ||
| Sample COVID Yes | 109/383 | 28.5% | 0.14 | |
| Sample COVID No | 215/784 | 27.4% | ||
| Satisfaction levels about ward/department transfer | ||||
| Total Sample of transferees | 254/324 | 78.4% | ||
| Sample COVID Yes | 84/109 | 77.1% | 0.17 | |
| Sample COVID No | 170/215 | 79.1% | ||
| Perception of adequate PPE | ||||
| Total Sample | 608/1167 | 52.1% | ||
| Sample COVID Yes | 198/383 | 51.7% | 0.04 | |
| Sample COVID No | 410/784 | 52.3% | ||
| Dimension | μ | σ | CI 95% | Welch t/χ2 |
|---|---|---|---|---|
| STAI—Y2 (state) | ||||
| Total Sample | 47.0 | 12.4 | 46.3–47.7 | |
| Sample COVID Yes | 48.8 | 12.5 | 47.6–50.1 | −3.57 *** |
| Sample COVID No | 46.1 | 12.2 | 45.2–46.9 | |
| STAI—Y1 (trait) | ||||
| Total Sample | 42.6 | 10.1 | 42.0–43.2 | |
| Sample COVID Yes | 43.5 | 10.0 | 42.5–44.5 | −1.96 * |
| Sample COVID No | 42.2 | 10.2 | 41.5–42.9 |
| COVID Yes (383) | COVID No (784) | |||
|---|---|---|---|---|
| Insomnia Severity Index | Pre N (%) | Post N (%) | Pre N (%) | Post N (%) |
| No clinically significant insomnia | 220 (57.5) | 85 (22.2) | 461 (58.8) | 229 (29.2) |
| Sub-threshold insomnia | 133 (34.7) | 156 (40.7) | 265 (33.8) | 331 (42.2) |
| Clinical insomnia (moderate severity) | 30 (7.8) | 115 (30) | 52 (6.6) | 183 (23.4) |
| Clinical insomnia (severe) | 0 (0) | 27 (7.1) | 6 (0.8) | 41 (5.2) |
| Dimension | Pre | Post | Delta 1 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| μ(σ) | CI 95% | Welch t/χ2 | μ(σ) | CI 95% | Welch t/χ2 | μ(σ) | CI 95% | Welch t/χ2 | |
| DRS Total | |||||||||
| Total Sample | 28.0 (5.4) | 27.7–28.3 | 26.7 (6.7) | 26.3–27.1 | −1.3 (5.1) | −1.6; −1.0 | |||
| Sample COVID Yes | 28.0 (5.2) | 27.5; 28.5 | 0.14 | 26.0 (7.0) | 25.3; 26.7 | 2.30 * | −1.9 (5.4) | −2.5; −1.4 | 2.84 ** |
| Sample COVID No | 28.0 (5.5) | 27.6; 28.4 | 27.0 (6.6) | 26.6; 27.5 | −1.0 (4.9) | −1.4; −0.7 | |||
| DRS Commitment | |||||||||
| Total Sample | 10.1 (2.4) | 10.0–10.3 | 9.3 (3.0) | 9.1–9.4 | −0.9 (2.3) | −1.0; −0.7 | |||
| Sample COVID Yes | 10.1 (2.3) | 9.9; 10.4 | 0.15 | 9.1 (3.1) | 8.7; 9.4 | 1.68 | −1.1 (2.5) | −1.3; −0.8 | 1.97 * |
| Sample COVID No | 10.1 (2.4) | 10.0; 10.3 | 9.4 (3.0) | 9.2; 9.6 | −0.8 (2.2) | -0,9; −0.6 | |||
| DRS Challenge | |||||||||
| Total Sample | 8.4 (3.0) | 8.2–8.6 | 8.2 (3.2) | 8.0–8.4 | −0.2 (2.1) | −0.3; −0.1 | |||
| Sample COVID Yes | 8.3 (3.0) | 8.0; 8.6 | 0.69 | 7.9 (3.3) | 7.5; 8.2 | 2.46 ** | −0.5 (2.1) | −0.7; −0.2 | 2.86 ** |
| Sample COVID No | 8.5 (3.0) | 8.2; 8.7 | 8.4 (3.2) | 8.1; 8.6 | −0.1 (2.1) | −0.2; 0.1 | |||
| DRS Control | |||||||||
| Total Sample | 9.4 (2.2) | 9.3–9.6 | 9.2 (2.4) | 9.1–9.3 | −0.2 (2.0) | −0.4; −0.1 | |||
| Sample COVID Yes | 9.5 (2.0) | 9.3; 9.7 | −0.79 | 9.1 (2.4) | 8.9; 9.3 | 1.04 | −0.4 (2.0) | −0.6; −0.2 | 2.14 * |
| Sample COVID No | 9.4 (2.2) | 9.3; 9.6 | 9.3 (2.4) | 9.1; 9.4 | −0.2 (2.0) | −0.3; −0.1 | |||
| Insomnia | |||||||||
| Total Sample | 7.0 (4.7) | 6.7; 7.3 | 11.5 (6.0) | 11.2; 11.9 | 4.5 (5.2) | 4.2; 4.8 | |||
| Sample COVID Yes | 6.8 (4.8) | 6.4; 7.3 | 0.78 | 12.2 (6.1) | 11.6; 12.9 | −2.81 ** | 5.4 (5.8) | 4.8; 6.0 | −3.77 *** |
| Sample COVID No | 7.1 (4.7) | 6.7; 7.4 | 11.2 (6.0) | 10.8; 11.6 | 4.1 (4.8) | 3.8; 4.5 | |||
| Total Sample | COVID Yes | COVID No | Total Sample | COVID Yes | COVID No | |
|---|---|---|---|---|---|---|
| Dimension | Insomnia Post | Insomnia Delta | ||||
| State anxiety (STAI-Y 2) | 0.571 *** | 0.539 *** | 0.581 *** | 0.476 *** | 0.511 *** | 0.446 *** |
| Trait anxiety (STAI-Y 1) | 0.447 *** | 0.464 *** | 0.436 *** | 0.234 *** | 0.284 *** | 0.201 *** |
| Hardiness total (DRS15) | −0.324 *** | −0.290 *** | −0.336 *** | −0.295 *** | −0.341 *** | −0.254 *** |
| Hardiness comm (DRS15 com) | −0.306 *** | −0.291 *** | −0.309 *** | −0.324 *** | −0.350 *** | −0.301 *** |
| Hardiness contr (DRS15 con) | −0.195 *** | −0.229 *** | −0.219 *** | −0.226 *** | −0.282 *** | −0.186 *** |
| Hardiness chall (DRS15 chal) | −0.237 *** | −0.141 ** | −0.234 *** | −0.145 *** | −0.201 *** | −0.100 ** |
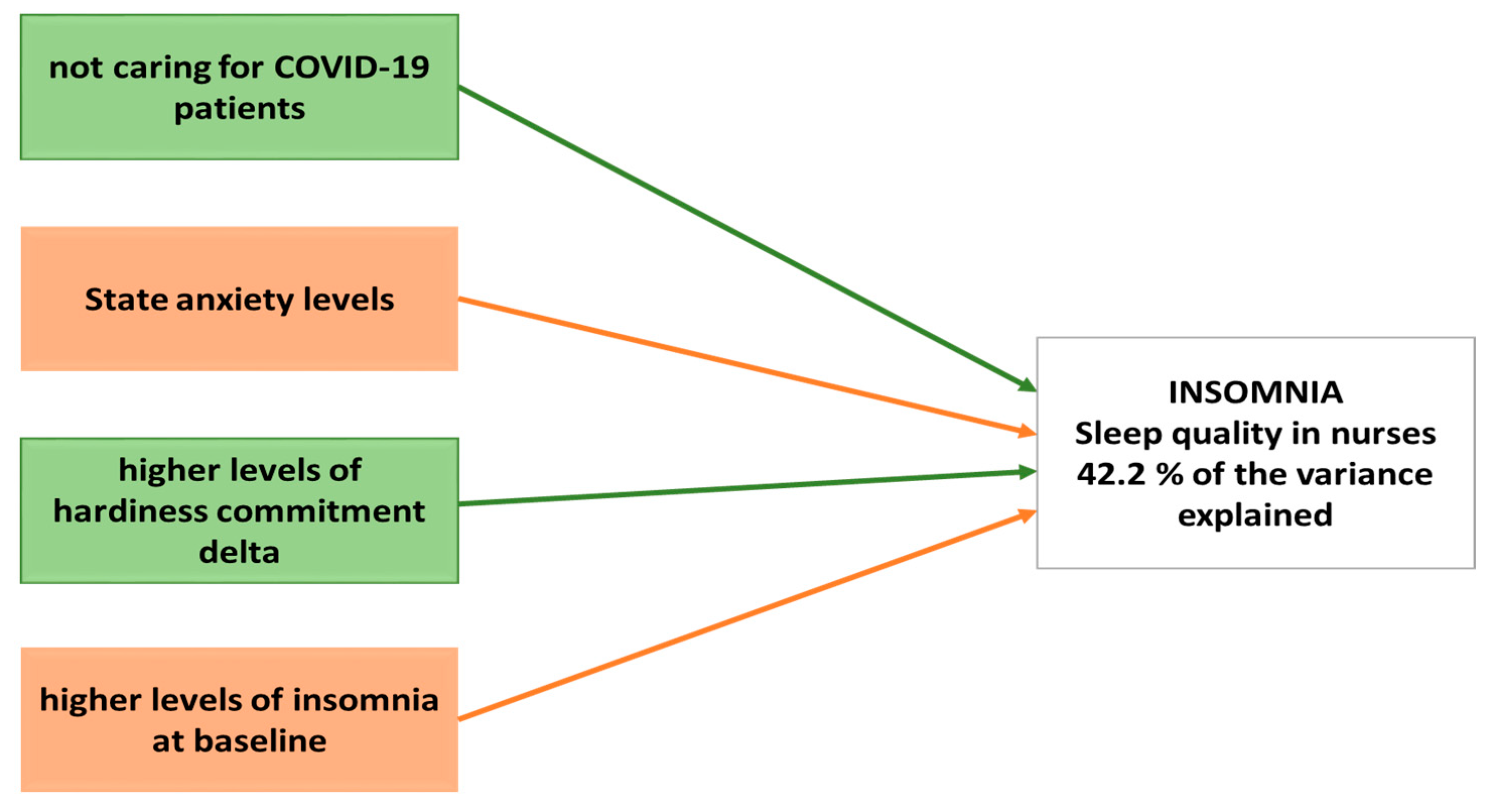
| Variable | Between Subjects Test | Parameters | |
|---|---|---|---|
| F | ß | t Test | |
| COVID Ward (No) | 4.46 * | −0.55 | −2.11 * |
| Anxiety (State) | 367.29 *** | 0.21 | 19.16 *** |
| Commitment (DSR-Delta) | 17.13 *** | −0.24 | −4.14 *** |
| Insomnia (Baseline) | 225.60 *** | −0.40 | −15.02 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baldassini Rodriguez, S.; Bardacci, Y.; El Aoufy, K.; Bazzini, M.; Caruso, C.; Giusti, G.D.; Mezzetti, A.; Lucchini, A.; Iozzo, P.; Guazzini, A.; et al. Sleep Quality and Its Relationship to Anxiety and Hardiness in a Cohort of Frontline Italian Nurses during the First Wave of the COVID-19 Pandemic. Nurs. Rep. 2023, 13, 1203-1215. https://doi.org/10.3390/nursrep13030103
Baldassini Rodriguez S, Bardacci Y, El Aoufy K, Bazzini M, Caruso C, Giusti GD, Mezzetti A, Lucchini A, Iozzo P, Guazzini A, et al. Sleep Quality and Its Relationship to Anxiety and Hardiness in a Cohort of Frontline Italian Nurses during the First Wave of the COVID-19 Pandemic. Nursing Reports. 2023; 13(3):1203-1215. https://doi.org/10.3390/nursrep13030103
Chicago/Turabian StyleBaldassini Rodriguez, Samuele, Yari Bardacci, Khadija El Aoufy, Marco Bazzini, Christian Caruso, Gian Domenico Giusti, Andrea Mezzetti, Alberto Lucchini, Pasquale Iozzo, Andrea Guazzini, and et al. 2023. "Sleep Quality and Its Relationship to Anxiety and Hardiness in a Cohort of Frontline Italian Nurses during the First Wave of the COVID-19 Pandemic" Nursing Reports 13, no. 3: 1203-1215. https://doi.org/10.3390/nursrep13030103
APA StyleBaldassini Rodriguez, S., Bardacci, Y., El Aoufy, K., Bazzini, M., Caruso, C., Giusti, G. D., Mezzetti, A., Lucchini, A., Iozzo, P., Guazzini, A., Magi, C. E., Iovino, P., Longobucco, Y., Rasero, L., & Bambi, S. (2023). Sleep Quality and Its Relationship to Anxiety and Hardiness in a Cohort of Frontline Italian Nurses during the First Wave of the COVID-19 Pandemic. Nursing Reports, 13(3), 1203-1215. https://doi.org/10.3390/nursrep13030103









