The Chem-Sex Inventory Scale (CSI): A Tool to Assess the Mental Health Risk of Chemsex Behaviors in Men Who Have Sex with Men
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Materials
2.3. Sample, Settings, and Procedure
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Factorial Structure of the CSI
3.2. Factorial Analyses
3.3. Reliability and Item Analysis
4. Discussion
4.1. Clinical Implications
4.2. Implications for Nursing
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
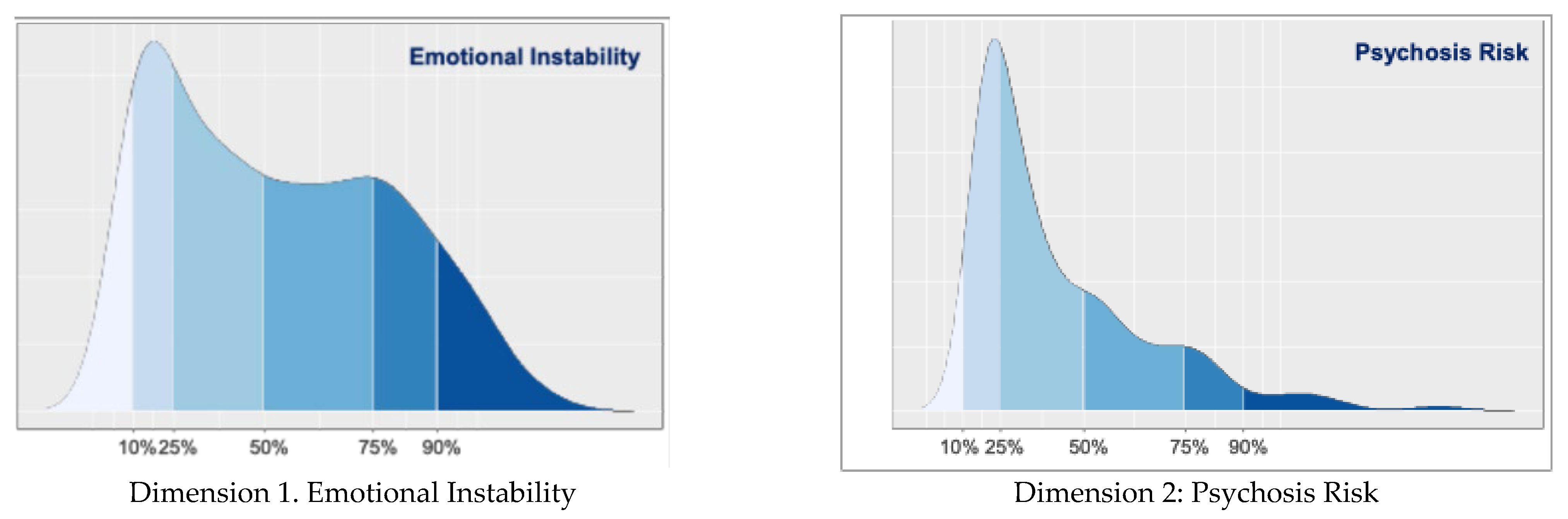
Appendix A. Percentile Chart
| Percentile Chart | ||||
| n = 563 | Dimension 1 | Dimension 2 | Dimension 3 | Dimension 4 |
| Percentile | ||||
| 10 | 15.0000 | 18.0000 | 5.0000 | 4.0000 |
| 25 | 20.0000 | 19.0000 | 7.0000 | 4.0000 |
| 50 | 33.0000 | 24.0000 | 11.0000 | 4.0000 |
| 75 | 48.0000 | 35.0000 | 16.0000 | 7.0000 |
| 90 | 57.0000 | 49.0000 | 21.0000 | 13.0000 |
| Dimension 1, Emotional instability. Dimension 2, Psychosis risk. Dimension 3, Altered body imagen perception. Dimension 4, Suicide risk | ||||
Appendix B. Final Version of the CSI
| Items CSI |
| 1. Have you felt nervous, anxious or very upset? |
| 2. Have you ever had difficulty relaxing? |
| 3. Have you been easily annoyed or irritated? |
| 4. Have you been afraid as if something terrible was going to happen? |
| 5. Have you had little interest or pleasure in doing things? |
| 6. Have you ever felt discouraged, depressed or hopeless? |
| 7. Have you ever felt tired or low energy? |
| 8. Have you had no appetite or, on the contrary, have you eaten too much? |
| 9. Have you ever felt bad about yourself, felt that you are a failure or that you are failing yourself? |
| 10. Have you had difficulty concentrating on doing everyday things, such as reading the newspaper or watching television? |
| 11. Have you ever had thoughts that you would be better off dead or harming yourself? |
| 12. Do familiar environments sometimes seem strange, confusing, threatening or unreal to you? |
| 13. Have you ever felt as if you were not in control of your own thoughts or ideas? |
| 14. Have ever had difficulty following your own conversation because you ramble or lose concentration too much when you talk? |
| 15. Have you ever had the feeling that other people are watching you or talking about you? |
| 16. Have you occasionally noticed any sensation on or under the skin, such as bugs? |
| 17.Have you ever worried that something might go wrong in your mind? |
| 18. Have you ever felt confused about whether something that happened to you was real or imaginary? |
| 19. Have you ever had feelings of distrust towards other people? |
| 20. Have you ever seen unusual things such as flashes, flames, glaring lights or geometric shapes? |
| 21. Have you ever seen things that other people cannot see? |
| 22. Do you have the feeling that people find it difficult to understand what you are saying? |
| 23. Have you ever had thoughts about your mind going faster than normal? |
| 24. In the last few days have you felt that you were acting impulsively? |
| 25. Do you feel restless in classes or lectures if you have to listen to someone talk for a long period of time |
| 26. Have you ever had chest pains? |
| 27. Have you ever felt that your heart was beating faster than usual? |
| 28. Have you ever felt short of breath? |
| 29. Have you had difficulty sleeping? |
| 30. Have you ever really had the idea of committing suicide? |
| 31. Have you thought about how you would carry it out?. |
| 32. Have you ever tried to take your own life? |
| 33. Have you ever felt that you have difficulty maintaining your attention, that you are easily distracted, or that you are unable to concentrate? |
| 34. Do you consider yourself a person with anger attacks that are difficult to predict? |
| 35. At any time have you considered yourself to be a person who changes moods frequently? |
| 36. Have you ever felt as if people were dropping hints or saying things with a double meaning? |
| 37. Have you ever felt that people look at you strangely because of your appearance? |
| 38. Have you ever felt as if your thoughts were being pulled out of your head? |
| 39. Have you ever felt as if your thoughts were not your own? |
| 40. Have you ever felt as if your thoughts were constantly repeating in your mind? |
| 41. Have you ever felt as if you were under the control of any external force or power? |
| 42. Have you ever heard voices when you were alone? |
References
- Dolengevich-Segal, H.; Salgado, B.R.; López, J.B.; Prado, R.M. Chemsex. Un fenómeno emergente. Rev. Adicciones 2017, 29, 207–209. [Google Scholar] [CrossRef]
- Ocón, R.S.; del Amo, J. Abordaje del fenómeno del Chemsex. Una propuesta desde el Plan Nacional sobre el SIDA. Rev. Esp. Salud Pública 2020, 94, 4. Available online: https://www.sanidad.gob.es/bibliotecaPub/repositorio/libros/28879_abordaje_del_fenomeno_del_chemsex.pdf (accessed on 5 July 2023).
- Ramos, J.C.; Dolengevich-Segal, H.; Ocón, R.S.; Egozcue, M.J.B. Documento Técnico: Abordaje de la Salud Mental Del Usuario Con Prácticas de Chemsex. Madrid. MSD 2020. Available online: https://www.sanidad.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/chemSex/docs/Abordaje_salud_mental_chemsex.pdf (accessed on 5 July 2023).
- Rodríguez, R.A.; Fernández, P.C.; Notario, J.C.; Dávila, P.F.; Balagué, S.R.; Mesquida, R.M.; Negró, L.V.; Chemsex Support. Una Respuesta Desde Y Para la Comunidad LGTB+. Stop Sida. Madrid. 2017. Available online: https://www.sidastudi.org/resources/inmagic-img/DD45606.pdf (accessed on 5 July 2023).
- Ocón, R.S. El fenómeno del chemsex: Claves para mejorar la respuesta institucional. Rev. Esp. Drogodepend. 2022, 47, 5–13. [Google Scholar]
- Madrid Salud. Plan de Adicciones de la Ciudad de Madrid. 2021/2022. 2022. Available online: https://madridsalud.es/pdf/PLAN%20DE%20ADICCIONES%2022-26.pdf (accessed on 28 August 2024).
- Íncera-Fernández, D.; Román, F.J.; Gámez-Guadix, M. Risky Sexual Practices, Sexually Transmitted Infections, Motivations, and Mental Health among Heterosexual Women and Men Who Practice Sexualized Drug Use in Spain. Int. J. Environ. Res. Public Health 2022, 19, 11–6387. [Google Scholar] [CrossRef]
- Coronado-Muñoz, M.; García-Cabrera, E.; Quintero-Flórez, A.; Román, E.; Vilches-Arenas, Á. Sexualized Drug Use and Chemsex among Men Who Have Sex with Men in Europe: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 1812. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Del Pozo-Herce, P.; Baca-García, E.; Martínez-Sabater, A.; Chover-Sierra, E.; Gea-Caballero, V.; Curto-Ramos, J.; Czapla, M.; Karniej, P.; Martínez-Tofe, J.; Sánchez-Barba, M.; et al. Descriptive study on substance uses and risk of sexually transmitted infections in the practice of Chemsex in Spain. Front. Public Health 2024, 12, 1391390. [Google Scholar] [CrossRef]
- Schmidt, A.J.; Bourne, A.; Weatherburn, P.; Reid, D.; Marcus, U.; Hickson, F. EMIS Network. Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). Int. J. Drug Policy 2016, 38, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, J.; Gertzen, M.; Rabenstein, A.; Straßburger, M.; Horstmann, A.; Pogarell, O.; Rüther, T.; Karch, S. What Chemsex does to the brain: Neural correlates (ERP) regarding decision making, impulsivity, and hypersexuality. Eur. Arch. Psychiatry Clin. Neurosci. 2024, 6, 1–14. [Google Scholar] [CrossRef]
- Pozo-Herce, P.D.; Martínez-Sabater, A.; Sanchez-Palomares, P.; Garcia-Boaventura, P.C.; Chover-Sierra, E.; Martínez-Pascual, R.; Gea-Caballero, V.; Saus-Ortega, C.; Ballestar-Tarín, M.L.; Karniej, P.; et al. Effectiveness of harm reduction interventions in Chemsex: A systematic review. Healthcare 2024, 12, 1411. [Google Scholar] [CrossRef]
- Amundsen, E.; Muller, A.E.; Reierth, E.; Skogen, V.; Berg, R.C. Chemsex among men who have sex with men: A systematic scoping review of research methods. J. Homosex. 2024, 71, 1392–1418. [Google Scholar] [CrossRef] [PubMed]
- Stuart, D. Chemsex: Origins of the word, a history of the phenomenon and a respect to the culture. Drugs Alcohol. Today 2019, 19, 3–10. [Google Scholar] [CrossRef]
- Rodríguez-Expósito, B.; Rieker, J.A.; Uceda, S.; Beltrán-Velasco, A.I.; Echeverry-Alzate, V.; Gómez-Ortega, M.; Positivo, A.; Reiriz, M. Psychological characteristics associated with chemsex among men who have sex with men: Internalized homophobia, conscientiousness, and serostatus as predictive factors. Int. J. Clin. Health Psychol. 2024, 24, 100465. [Google Scholar] [CrossRef] [PubMed]
- Glynn, R.W.; Byrne, N.; O’Dea, S.; Shanley, A.; Codd, M.; Keenan, E.; Ward, M.; Igoe, D.; Clarke, S. Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin, Ireland. Int. J. Drug Policy 2018, 52, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.; Shahmanesh, M.; Gafos, M. Chemsex behaviours among men who have sex with men: A systematic review of the literature. Int. J. Drug Policy 2019, 63, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Prestage, G.; Hammoud, M.; Jin, F.; Degenhardt, L.; Bourne, A.; Maher, L. Mental health, drug use and sexual risk behavior among gay and bisexual men. Int. J. Drug Policy 2018, 55, 169–179. [Google Scholar] [CrossRef]
- Bourne, A.; Weatherburn, P. Substance use among men who have sex with men: Patterns, motivations, impacts and intervention development need. Sex. Transm. Infect. 2017, 93, 342–346. [Google Scholar] [CrossRef]
- Ocón, R.S.; Redondo, S.; Torrecilla, C. PAUSA. Programa Piloto Sobre Chemsex [Internet]. Subdirección General de Adicciones. Instituto de Adicciones. Madrid Salud. 2020. Available online: https://madridsalud.es/wpcontent/uploads/2021/02/pausa.pdf (accessed on 17 July 2023).
- Hovaguimian, F.; Kouyos, R.D.; Kusejko, K.; Schmidt, A.J.; Tarr, P.E.; Bernasconi, E.; Braun, D.L.; Calmy, A.; Notter, J.; Stoeckle, M.; et al. Incidence of sexually transmitted infections and association with behavioural factors: Time-to-event analysis of a large pre-exposure prophylaxis (PrEP) cohort. HIV Med. 2024, 25, 117–128. [Google Scholar] [CrossRef]
- Íncera-Fernández, D.; Gámez-Guadix, M.; Ibarguchi, L.; García, A.; Zaro, I.; Alonso, A. Aproximación Al Chemsex 2021: Encuesta Sobre Hábitos Sexuales Y Consumo de Drogas en España Entre Hombres GBHSH. 2022 Madrid: Apoyo Positivo E Imagina Más. Available online: https://apoyopositivo.org/wp-content/uploads/2022/05/Aproximacion-al-Chemsex-2021.pdf (accessed on 19 July 2023).
- Del Pozo-Herce, P.; Martínez-Sabater, A.; Chover-Sierra, E.; Gea-Caballero, V.; Satústegui-Dordá, P.J.; Saus-Ortega, C.; Tejada-Garrido, C.I.; Sánchez-Barba, M.; Pérez, J.; Juárez-Vela, R.; et al. Application of the Delphi Method for Content Validity Analysis of a Questionnaire to Determine the Risk Factors of the Chemsex. Healthcare 2023, 5, 2905. [Google Scholar] [CrossRef]
- Hasson, F.; Keeney, S.; McKenna, H. Research guidelines for the Delphi survey technique. J. Adv. Nurs. 2000, 32, 1008–1015. [Google Scholar] [CrossRef]
- Linstone, H.; Turoff, M. The Delphi method: Techniques and applications. Technometrics 1975. Available online: http://www.foresight.pl/assets/downloads/publications/Turoff_Linstone.pdf (accessed on 15 September 2023).
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health. 2006, 29, 489–497. [Google Scholar] [CrossRef]
- Orts-Cortés, M.I.; Moreno-Casbas, T.; Squires, A.; Fuentelsaz-Gallego, C.; Maciá-Soler, L.; González-María, E. Content validity of the Spanish version of the Practice Environment Scale of the Nursing Work Index. Appl. Nurs. Res. 2013, 26, 5–9. [Google Scholar] [CrossRef]
- Squires, A.; Aiken, L.H.; Van den Heede, K.; Sermeus, W.; Bruyneel, L.; Lindqvist, R.; Schoonhoven, L.; Stromseng, I.; Busse, R.; Brzostek, T.; et al. A systematic survey instrument translation process for multi-country, comparative health workforce studies. Int. J. Nurs. Stud. 2013, 50, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Chover-Sierra, E.; Martínez-Sabater, A.; Lapeña-Moñux, Y.R. An instrument to measure nurse’s knowledge in palliative care: Validation of the Spanish version of Palliative Care Quiz for Nurses. PLoS ONE 2017, 18, 12. [Google Scholar]
- Pallás, J.A.; Villa, J.J. Métodos de Investigación Clínica y Metodológica; Elsevier: Amsterdam, The Netherlands, 2004. [Google Scholar]
- Hoyle, R.H. Structural Equation Modeling: Concept, Issues and Application; Sage: Sauzendoaks, CA, USA, 1995. [Google Scholar]
- Bentler, P.M. Comparative fit indexes in structural models. Psychological Bulletin. Psycholl Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Tucker, L.R.; Lewis, C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika 1973, 38, 1–10. [Google Scholar] [CrossRef]
- Steiger, J.H. Structural model evaluation and modification: An interval estimation approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef]
- Joreskog, K.G.; Sorbom, D. LISREL8: User’s Reference Guide; Scientific Software: Mooresville, NC, USA, 1996. [Google Scholar]
- Bentler, P.M. Alpha, dimension-free, and model-based internal consistency reliability. Psychometrika 2009, 74, 137–143. [Google Scholar] [CrossRef]
- Kaiser, H.F. Week’s Citation Classic. Educ Psychol Meas. 1960, 20, 141–151. Available online: https://awspntest.apa.org/record/1960-06772-001 (accessed on 23 September 2023). [CrossRef]
- Hair, J.F.; Anderson, R.E.; Tatham, R.L.; Black, W.C. Análisis Multivariante, 5th ed.; Hall, P., Ed.; Paper Knowledge. Toward a Media History of Documents; Pearson Prentice Hall: Madrid, Spain, 1999; Available online: https://dialnet.unirioja.es/servlet/libro?codigo=320227 (accessed on 25 September 2023).
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; Sage Publications: Thousand Oaks, CA, USA, 2003; pp. 232–233. [Google Scholar]
- Dolengevich-Segal, H.; Gonzalez-Baeza, A.; Valencia, J.; Valencia-Ortega, E.; Cabello, A.; Tellez-Molina, M.J.; Perez-Elias, M.J.; Serrano, R.; Perez-Latorre, L.; Martin-Carbonero, L.; et al. Drug-related and psychopathological symptoms in HIV-positive men who have sex with men who inject drugs during sex (slamsex): Data from the U-SEX GESIDA 9416 Study. PLoS ONE 2019, 14, 12. [Google Scholar] [CrossRef] [PubMed]
- Bohn, A.; Sander, D.; Köhler, T.; Hees, N.; Oswald, F.; Scherbaum, N.; Deimel, D.; Schecke, H. Chemsex and Mental Health of Men Who Have Sex with Men in Germany. Front. Psychiatry 2020, 4, 11. [Google Scholar] [CrossRef]
- Berg, R.C.; Amundsen, E.; Haugstvedt, Å. Links between chemsex and reduced mental health among Norwegian MSM and other men: Results from a cross-sectional clinic survey. BMC Public Health 2020, 10, 1785. [Google Scholar] [CrossRef]
- Moreno-Gámez, L.; Hernández-Huerta, D.; Lahera, G. Chemsex and Psychosis: A Systematic Review. Behav. Sci. 2022, 15, 516. [Google Scholar] [CrossRef] [PubMed]
- Gevonden, M.J.; Selten, J.P.; Myin-Germeys, I.; De Graaf, R.; Have, M.T.; Van Dorsselaer, S.; Van Os, J.; Veling, W. Sexual minority status and psychotic symptoms: Findings from the Netherlands Mental Health Survey and Incidence Studies (NEMESIS). Psychol. Med. 2014, 44, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Lafortune, D.; Blais, M.; Miller, G.; Dion, L.; Lalonde, F.; Dargis, L. Psychological and Interpersonal Factors Associated with Sexualized Drug Use Among Men Who Have Sex with Men: A Mixed-Methods Systematic Review. Arch. Sex. Behav. 2021, 50, 427–460. [Google Scholar] [CrossRef]
- Dolengevich-Segal, H.; Rodríguez-Salgado, B.; Gómez-Arnau, J.; Sánchez-Mateos, D. Severe Psychosis, Drug Dependence, and Hepatitis C Related to Slamming Mephedrone. Case Rep. Psychiatry 2016, 2016, 8379562. [Google Scholar] [PubMed]
- Kennedy, R.; Murira, J.; Foster, K.; Heinsbroek, E.; Keane, F.; Pal, N.; Chalmers, L.; Sinka, K. Sexualized drug use and specialist service experience among MSM attending urban and rural sexual health clinics in England and Scotland. Int. J. STD AIDS 2021, 32, 1338–1346. [Google Scholar] [CrossRef] [PubMed]
- Hegazi, A.; Lee, M.J.; Whittaker, W.; Green, S.; Simms, R.; Cutts, R.; Nagington, M.; Nathan, B.; Pakianathan, M.R. Chemsex and the city: Sexualized substance use in gay, bisexual and other men who have sex with men attending sexual health clinics. Int. J. STD AIDS 2017, 28, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Edmundson, C.; Heinsbroek, E.; Glass, R.; Hope, V.; Mohammed, H.; White, M.; Desai, M. Sexualised drug use in the United Kingdom (UK): A review of the literature. Int. J. Drug Pol. 2018, 55, 131–148. [Google Scholar] [CrossRef]
- Hibbert, M.P.; Brett, C.E.; Porcellato, L.A.; Hope, V. Psychosocial and sexual characteristics associated with sexualized drug use and chemsex among men who have sex with men (MSM) in the UK. Sex. Transm. Infect. 2019, 95, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Buller, A.M.; Devries, K.M.; Howard, L.M.; Bacchus, L.J. Associations between intimate partner violence and health among men who have sex with men: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001609. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, A. Sex, drugs and self-control: Why chemsex is fast becoming a public health concern. J. Fam. Plann Reprod. Health Care 2016, 42, 291–294. [Google Scholar] [CrossRef] [PubMed]


| Variables | n | % |
|---|---|---|
| Age (mean, SD) | 36.9 | SD 9.2 |
| Gender identity | ||
| Cisgender | 550 | 97.7 |
| Transgender | 2 | 0.3 |
| Queer (non-binary) | 11 | 2 |
| Sexual Identity | ||
| Gay/Homosexual | 372 | 66.1 |
| Heterosexual | 134 | 23.8 |
| Bisexual | 57 | 10.1 |
| Relationship Status | ||
| Single | 276 | 49 |
| Single with a domestic partner | 166 | 29.5 |
| Married | 100 | 17.8 |
| Divorced | 9 | 1.6 |
| Widower | 1 | 0.2 |
| Others | 11 | 2 |
| Employment status | ||
| Full-time employed | 458 | 81.3 |
| Part-time employed | 42 | 7.5 |
| Unemployed | 27 | 4.8 |
| Retired | 4 | 0.7 |
| Others | 32 | 5.7 |
| Monthly net income | ||
| <499 Euros | 14 | 2.5 |
| 500–999 Euros | 19 | 3.4 |
| 1000–1499 Euros | 99 | 17.6 |
| 1500–1999 Euros | 165 | 29.3 |
| 2000–2499 Euros | 127 | 22.6 |
| 2500–2999 Euros | 67 | 11.9 |
| 3000–4999 Euros | 61 | 10.8 |
| more than 5000 Euros | 11 | 2 |
| Educational level | ||
| Primary school | 14 | 2.5 |
| Baccalaureate | 39 | 6.9 |
| Diploma/Bachelor’s degree | 264 | 46.9 |
| Master’s degree | 213 | 37.8 |
| Doctor of Philosophy (PhD) | 33 | 5.9 |
| Substance use in 12 months in a sexual context | ||
| Amyl nitrite (Poppers) | 260 | 46.2 |
| Medication for erectile dysfunction | 111 | 19.7 |
| GHB/GBL | 151 | 26.8 |
| Alcohol | 264 | 46.9 |
| Tobacco | 161 | 28.6 |
| Ecstasy | 67 | 11.9 |
| Amphetamines | 49 | 8.7 |
| Ketamine | 48 | 8.5 |
| Methamphetamine | 58 | 10.3 |
| Mephedrone | 133 | 23.6 |
| THC | 66 | 11.7 |
| Cocaine | 114 | 20.2 |
| Opioid Analgesics | 11 | 2 |
| Heroin | 1 | 0.2 |
| Substance use in 12 months not in a sexual context | ||
| Amyl nitrite (Poppers) | 139 | 24.7 |
| Medication for erectile dysfunction | 7 | 1.2 |
| GHB/GBL | 52 | 9.2 |
| Alcohol | 395 | 70.2 |
| Tobacco | 198 | 35.2 |
| Ecstasy | 75 | 13.3 |
| Amphetamines | 40 | 7.1 |
| Ketamine | 39 | 6.9 |
| Methamphetamine | 27 | 4.8 |
| Mephedrone | 65 | 11.5 |
| THC | 92 | 16.3 |
| Cocaine | 120 | 21.3 |
| Opioid Analgesics | 44 | 7.8 |
| Heroin | 2 | 0.4 |
| Substances injected in a sexual context in 12 months | ||
| Ketamine | 8 | 1.4 |
| Methamphetamine | 21 | 3.7 |
| Mephedrone | 53 | 9.4 |
| Heroin | 1 | 0.2 |
| PrEP | yes 120 | % 21.3 |
| Have you acquired any STIs in the last six months? | yes | % |
| Gonorrhoea | 68 | 12.2 |
| Chlamydia | 53 | 9.4 |
| Genital herpes | 25 | 4.4 |
| Syphilis | 45 | 8 |
| HIV | 17 | 3 |
| MPOX | 10 | 1.8 |
| Hepatitis | 8 | 1.4 |
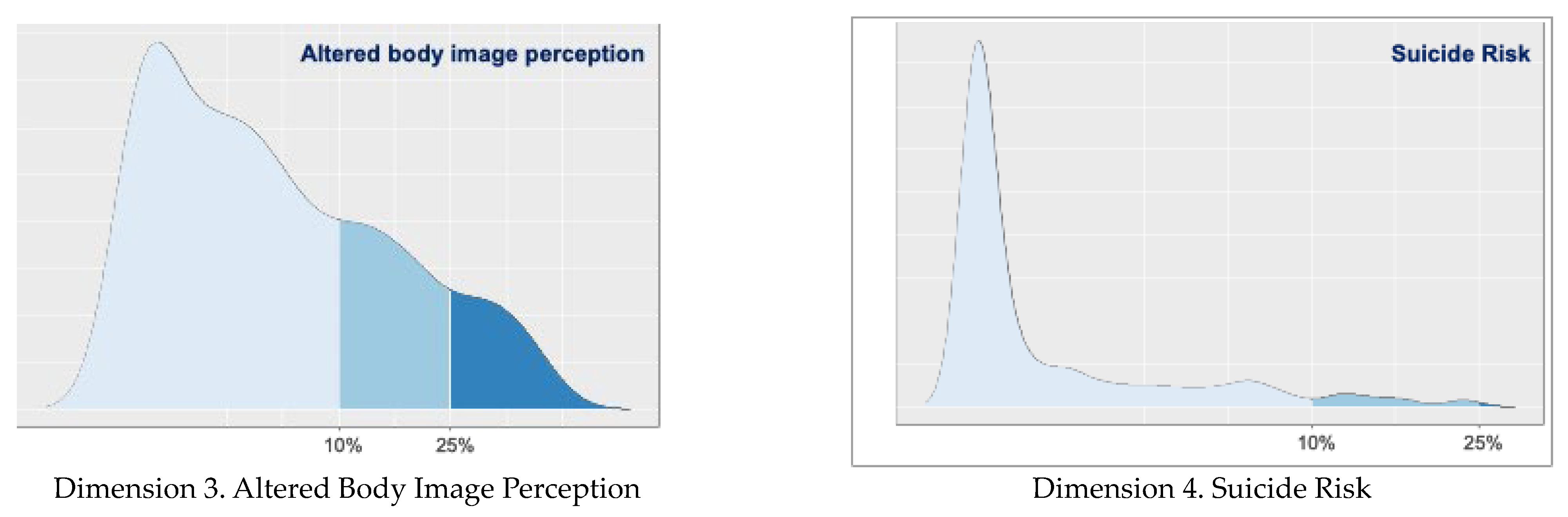
| Dimension 1 | Emotional Instability | |||||||||||||||||
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 17 | 30 | 40 | 43 | 42 | |||
| Load | 0.65 | 0.67 | 0.65 | 0.67 | 0.74 | 0.79 | 0.79 | 0.72 | 0.78 | 0.73 | 0.67 | 0.46 | 0.60 | 0.52 | 0.46 | |||
| Dimension 2 | Psychosis Risk | |||||||||||||||||
| Item | 12 | 13 | 14 | 15 | 16 | 18 | 19 | 20 | 21 | 22 | 23 | 45 | 46 | 47 | 48 | 49 | 50 | 51 |
| Load | 0.42 | 0.45 | 0.47 | 0.57 | 0.47 | 0.63 | 0.45 | 0.61 | 0.66 | 0.62 | 0.49 | 0.49 | 0.57 | 0.74 | 0.73 | 0.54 | 0.62 | 0.51 |
| Dimension 3 | Altered body image perception | |||||||||||||||||
| Item | 32 | 34 | 35 | 36 | 26 | |||||||||||||
| Load | 0.57 | 0.55 | 0.60 | 0.45 | 0.42 | |||||||||||||
| Dimension 4 | Suicide Risk | |||||||||||||||||
| Item | 39 | 11 | 37 | 38 | ||||||||||||||
| Load | 0.50 | 0.63 | 0.88 | 0.85 | ||||||||||||||
| Dimensions | Cronbach’s Alpha | McDonald’s Omega |
|---|---|---|
| Dimension 1: Emotional Instability | 0.95 | 0.95 |
| Dimension 2: Psychosis Risk | 0.94 | 0.94 |
| Dimension 3: Altered body image perception | 0.88 | 0.89 |
| Dimension 4: Suicide Risk | 0.88 | 0.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Pozo-Herce, P.; Baca-García, E.; Martínez-Sabater, A.; Pérez-Elvira, R.; Gea-Caballero, V.; Chover-Sierra, E.; Satústegui-Dordá, P.J.; Tovar-Reinoso, A.; Rodríguez-Velasco, F.J.; Sánchez-Barba, M.; et al. The Chem-Sex Inventory Scale (CSI): A Tool to Assess the Mental Health Risk of Chemsex Behaviors in Men Who Have Sex with Men. Nurs. Rep. 2024, 14, 2226-2245. https://doi.org/10.3390/nursrep14030166
Del Pozo-Herce P, Baca-García E, Martínez-Sabater A, Pérez-Elvira R, Gea-Caballero V, Chover-Sierra E, Satústegui-Dordá PJ, Tovar-Reinoso A, Rodríguez-Velasco FJ, Sánchez-Barba M, et al. The Chem-Sex Inventory Scale (CSI): A Tool to Assess the Mental Health Risk of Chemsex Behaviors in Men Who Have Sex with Men. Nursing Reports. 2024; 14(3):2226-2245. https://doi.org/10.3390/nursrep14030166
Chicago/Turabian StyleDel Pozo-Herce, Pablo, Enrique Baca-García, Antonio Martínez-Sabater, Rubén Pérez-Elvira, Vicente Gea-Caballero, Elena Chover-Sierra, Pedro José Satústegui-Dordá, Alberto Tovar-Reinoso, Francisco José Rodríguez-Velasco, Mercedes Sánchez-Barba, and et al. 2024. "The Chem-Sex Inventory Scale (CSI): A Tool to Assess the Mental Health Risk of Chemsex Behaviors in Men Who Have Sex with Men" Nursing Reports 14, no. 3: 2226-2245. https://doi.org/10.3390/nursrep14030166
APA StyleDel Pozo-Herce, P., Baca-García, E., Martínez-Sabater, A., Pérez-Elvira, R., Gea-Caballero, V., Chover-Sierra, E., Satústegui-Dordá, P. J., Tovar-Reinoso, A., Rodríguez-Velasco, F. J., Sánchez-Barba, M., Pérez, J., & Juárez-Vela, R. (2024). The Chem-Sex Inventory Scale (CSI): A Tool to Assess the Mental Health Risk of Chemsex Behaviors in Men Who Have Sex with Men. Nursing Reports, 14(3), 2226-2245. https://doi.org/10.3390/nursrep14030166













