Developing a Contextually Appropriate Integrated Hygiene Intervention to Achieve Sustained Reductions in Diarrheal Diseases
Abstract
:1. Introduction
2. Methods and Results
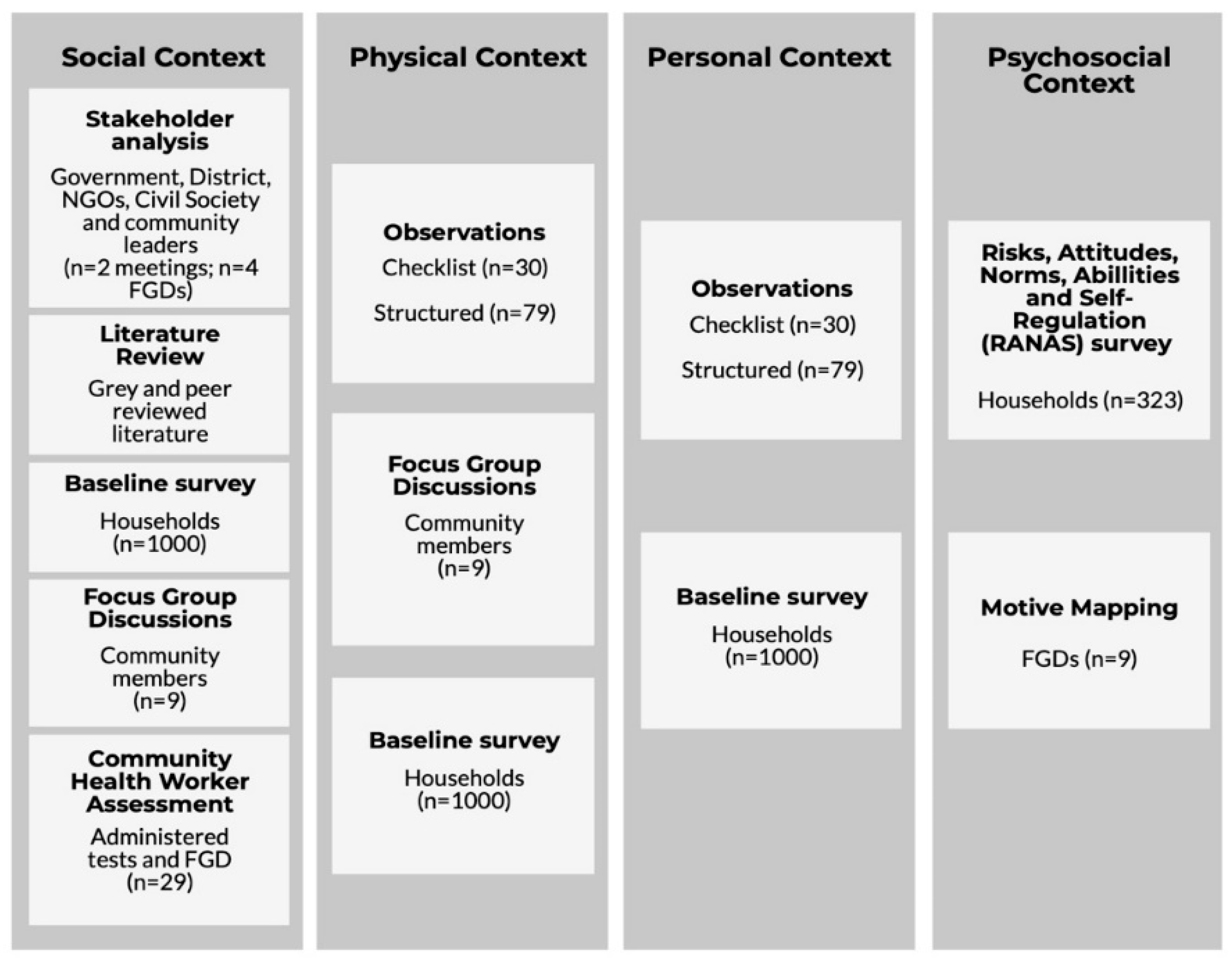
2.1. Formative Research
2.2. Setting and Population
2.3. Ethics and Consent to Participate
2.4. Recruitment and Participants
2.5. Literature Review and Key Informant Interviews
2.6. Observations
- HWWS at critical times (i.e., after latrine use, after cleaning child bottom, before food preparation and before child feeding/eating).
- Food hygiene: washing utensils with soap, keeping utensils and cooked food on an elevated place, reheating of left-over food until boiling and hygienic feeding.
- Feces management: safe and immediate removal of child and animal stools from the household compound into the latrine.
- Household water management: regular washing of water collection and storage containers with soap and covering of water during storage with tight fitting lids.
2.7. RANAS Questionnaire and Motive Mapping
2.8. Baseline Data Collection
- Although the mother was identified as the primary caregiver in this rural context, there is a need for strong male involvement in the intervention, as they are the primary managers and decision makers in terms of household finance.
- There was marked homogeneity across all households in terms of diet, cooking, food storage, feeding practices, and available utensils. This allows us to design an intervention to easily tackle food safety issues in a generic manner across the population.
- Comparison of data from baseline and observations demonstrated that knowledge of good hygiene practice is high. However, this does not translate into practice, and as such the intervention should have a behavior-centered approach to address this gap (Figure 4).
- Caregivers play a number of roles within their household and community, and any intervention needs to be cognizant of time commitments and availability.
- Although the results showed that health workers had a good level of understanding of water and sanitation issues (80% know to use water and soap for effective hand washing; 93% believe poor HWWS due to lack of soap/poverty; 69% understood animal feces could transmit disease), there was limited knowledge in relation to food hygiene practices (10% could describe critical behaviors around food hygiene). This needs to be addressed if they are to facilitate the intervention.
- The intervention must be cognizant of the low level of literacy and the level of poverty within the target population, and therefore behavior change techniques must be appropriate, and recommendations need to be realistic.
3. Intervention Design
- The impact of each intervention on the incidence of diarrheal disease.
- The impact of each intervention relative to the Control Group.
- The impact of the WASH intervention relative to the WASH + Food Hygiene Intervention.
3.1. Sample Size
3.2. Intervention Framework
3.3. Data Management and Analysis Plan
Data Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walker, C.L.F.; Rudan, I.; Liu, L.; Nair, H.; Theodoratou, E.; Bhutta, Z.A.; O’Brien, K.L.; Campbell, H.; Black, R.E. Global burden of childhood pneumonia and diarrhea. Lancet 2013, 381. [Google Scholar] [CrossRef]
- Bartram, J.; Cairncross, S. Hygiene, Sanitation, and Water: Forgotten Foundations of Health. PLoS Med. 2010, 7, e1000367. [Google Scholar] [CrossRef] [PubMed]
- UNICEF; WHO. Diarrhea: Why Children Are Still Dying and What Can Be Done; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Roche, R.; Bain, R.; Cumming, O. A long way to go—Estimates of combined water, sanitation and hygiene coverage for 25 sub-Saharan African countries. PLoS ONE 2017, 12, e0171783. [Google Scholar]
- Curtis, V.; Cairncross, S. Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infect. Dis. 2003, 3, 275–281. [Google Scholar] [CrossRef]
- Clasen, T.; Schmidt, W.-P.; Rabie, T.; Roberts, I.; Cairncross, S. Interventions to improve water quality for preventing diarrhoea: Systematic review and meta-analysis. BMJ 2007, 334, 782. [Google Scholar] [CrossRef] [PubMed]
- Waddington, H.; Snilstveit, B.; White, H.; Fewtrell, L. Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhea in Developing Countries. Syst. Rev. Repos. 2009, 119. [Google Scholar] [CrossRef]
- Mara, D. Shared sanitation: To include or to exclude? Trans. R. Soc. Trop. Med. Hyg. 2016, 110, 265–267. [Google Scholar] [CrossRef]
- Wolf, J.; Prüss-Ustün, A.; Cumming, O.; Bartram, J.; Bonjour, S.; Cairncross, S.; Clasen, T.; Colford, J.M.; Curtis, V.; De France, J.; et al. Systematic review: Assessing the impact of drinking water and sanitation on diarrhoeal disease in low- and middle-income settings: Systematic review and meta-regression. Trop. Med. Int. Health 2014, 19, 928–942. [Google Scholar] [CrossRef]
- Humphrey, J.H.; Jones, A.D.; Manges, A.; Mangwadu, G.; Maluccio, J.A.; Mbuya, M.N.N.; Moulton, L.H.; Ntozini, R.; Prendergast, A.J.; Stoltzfus, R.J.; et al. The Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial: Rationale, Design, and Methods. Clin. Infect. Dis. 2015, 61, S685–S702. [Google Scholar] [Green Version]
- Mbuya, M.N.N.; Tavengwa, N.V.; Stoltzfus, R.J.; Curtis, V.; Pelto, G.H.; Ntozini, R.; Kambarami, R.A.; Fundira, D.; Malaba, T.R.; Maunze, D.; et al. Design of an Intervention to Minimize Ingestion of Fecal Microbes by Young Children in Rural Zimbabwe. Clin. Infect. Dis. 2015, 61, S703–S709. [Google Scholar] [CrossRef]
- Null, C.; Stewart, C.P.; Pickering, A.J.; Dentz, H.N.; Arnold, B.F.; Arnold, C.D.; Benjamin-Chung, J.; Clasen, T.; Dewey, K.G.; Fernald, L.C.H.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: A cluster-randomised controlled trial. Lancet Glob. Health 2018, 6, e316–e329. [Google Scholar] [CrossRef]
- Luby, S.P.; Rahman, M.; Arnold, B.F.; Unicomb, L.; Ashraf, S.; Winch, P.J.; Stewart, C.P.; Begum, F.; Hussain, F.; Benjamin-Chung, J.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: A cluster randomised controlled trial. Lancet Glob. Health 2018, 6, e302–e315. [Google Scholar] [CrossRef]
- Berendes, D.; Leon, J.; Kirby, A.; Clennon, J.; Raj, S.; Yakubu, H.; Robb, K.; Kartikeyan, A.; Hemavathy, P.; Gunasekaran, A.; et al. Household sanitation is associated with lower risk of bacterial and protozoal enteric infections, but not viral infections and diarrhoea, in a cohort study in a low-income urban neighbourhood in Vellore, India. Trop. Med. Int. Health 2017, 22, 1119–1129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Moe, C.L.; Null, C.; Raj, S.J.; Baker, K.K.; Robb, K.A.; Yakubu, H.; Ampofo, J.A.; Wellington, N.; Freeman, M.C.; et al. Multipathway Quantitative Assessment of Exposure to Fecal Contamination for Young Children in Low-Income Urban Environments in Accra, Ghana: The SaniPath Analytical Approach. Am. J. Trop. Med. Hyg. 2017, 97, 1009–1019. [Google Scholar] [CrossRef] [PubMed]
- Hurd, J.; Hennink, M.; Robb, K.; Null, C.; Peprah, D.; Wellington, N.; Yakubu, H.; Moe, C.L. Behavioral influences on risk of exposure to fecal contamination in low-resource neighborhoods in Accra, Ghana. J. Water Sanit. Hyg. Dev. 2017, 7, 300–311. [Google Scholar] [CrossRef] [Green Version]
- Ercumen, A.; Pickering, A.J.; Kwong, L.H.; Arnold, B.F.; Parvez, S.M.; Alam, M.; Sen, D.; Islam, S.; Kullmann, C.; Chase, C.; et al. Animal Feces Contribute to Domestic Fecal Contamination: Evidence from E. coli Measured in Water, Hands, Food, Flies, and Soil in Bangladesh. Environ. Sci. Technol. 2017, 51, 8725–8734. [Google Scholar] [CrossRef]
- Barnes, A.N.; Mumma, J.; Cumming, O. Role, ownership and presence of domestic animals in peri-urban households of Kisumu, Kenya. Zoonoses Public Health 2017, 65, 202–214. [Google Scholar] [CrossRef] [Green Version]
- Ngure, F.M.; Majo, F.; Mbuya, M.N.N.; Humphrey, J.H.; Govha, M.; Chasekwa, B.; Mutasa, K.; Boor, K.J.; Mazarura, E.; Curtis, V.; et al. Formative Research on Hygiene Behaviors and Geophagy among Infants and Young Children and Implications of Exposure to Fecal Bacteria. Am. J. Trop. Med. Hyg. 2013, 89, 709–716. [Google Scholar] [CrossRef] [Green Version]
- Lanata, C. Studies of food hygiene and diarrhoeal disease. Int. J. Environ. Health Res. 2003, 13, S175–S183. [Google Scholar] [CrossRef]
- Kung’u, J.K.; Boor, K.J.; Ame, S.M.; Ali, N.S.; Jackson, A.E.; Stoltzfus, R.J. Bacterial Populations in Complementary Foods and Drinking-water in Households with Children Aged 10-15 Months in Zanzibar, Tanzania. J. Health Popul. Nutr. 2009, 27, 41–52. [Google Scholar] [CrossRef] [Green Version]
- Sheth, M.; Patel, J.; Sharma, S.; Seshadri, S. Hazard analysis and critical control points of weaning foods. Indian J. Pediatr. 2000, 67, 405–410. [Google Scholar] [CrossRef]
- Parvez, S.M.; Kwong, L.; Rahman, M.J.; Ercumen, A.; Pickering, A.J.; Ghosh, P.K.; Das, K.K.; Unicomb, L.; Luby, S.P. E. coli contamination of child complementary foods and association with domestic hygiene in rural Bangladesh. Trop. Med. Int. Health 2017, 22, 547–557. [Google Scholar] [CrossRef]
- Taulo, S.; Wetlesen, A.; Abrahamsen, R.; Kululanga, G.; Mkakosya, R.; Grimason, A. Microbiological hazard identification and exposure assessment of food prepared and served in rural households of Lungwena, Malawi. Int. J. Food Microbiol. 2008, 125, 111–116. [Google Scholar] [CrossRef]
- Toure, O.; Coulibaly, S.; Arby, A.; Maiga, F.; Cairncross, S. Improving microbiological food Safety in peri-urban Mali; an experimental study. Food Control 2011, 22, 1565–1572. [Google Scholar] [CrossRef]
- WHO. WHO Estimates of the Global Burden of Foodborne Diseases; WHO: Geneva, Switzerland, 2015; pp. 1–255. [Google Scholar]
- Cairncross, S.; Hunt, C.; Boisson, S.; Bostoen, K.; Curtis, V.; Fung, I.C.; Schmidt, W.-P. Water, sanitation and hygiene for the prevention of diarrhoea. Int. J. Epidemiol. 2010, 39, i193–i205. [Google Scholar] [CrossRef] [Green Version]
- Cairncross, S.; Bartram, J.; Cumming, O.; Brocklehurst, C. Hygiene, Sanitation, and Water: What Needs to Be Done? PLoS Med. 2010, 7, e1000365. [Google Scholar] [CrossRef]
- Mara, D.; Lane, J.; Scott, B.; Trouba, D. Sanitation and Health. PLoS Med. 2010, 7, e1000363. [Google Scholar] [CrossRef]
- Curtis, V.; Schmidt, W.; Luby, S.; Florez, R.; Toure, O.; Biran, A. Hygiene: New hopes, new horizons. Lancet Infect. Dis. 2011, 11, 312–321. [Google Scholar] [CrossRef]
- Mosler, H.-J. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: A conceptual model, a review, and a guideline. Int. J. Environ. Health Res. 2012, 22, 431–449. [Google Scholar] [CrossRef]
- Biran, A.; Schmidt, W.-P.; Varadharajan, K.S.; Rajaraman, D.; Kumar, R.; Greenland, K.; Gopalan, B.; Aunger, R.; Curtis, V. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. Lancet Glob. Health 2014, 2, e145–e154. [Google Scholar] [CrossRef]
- Aunger, R.; Curtis, V. A Guide to Behavior Centerd Design; London School of Hygiene and Tropical Medicine: London, UK, 2015. [Google Scholar]
- Devine, J. Introducing SaniFOAM: A Framework to Analyze Sanitation Behaviors to design Effective Sanitation Programs. 2009. Available online: http://www.wsp.org/sites/wsp.org/files/publications/GSP_sanifoam.pdf (accessed on 26 August 2019).
- Toure, O.; Coulibaly, S.; Arby, A.; Maiga, F.; Cairncross, S. Piloting an intervention to improve microbiological food safety in Peri-Urban Mali. Int. J. Hyg. Environ. Health 2013, 216, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Mahmud, Z.H.; Gope, P.S.; Zaman, R.U.; Hossain, Z.; Islam, M.S.; Mondal, D.; Sharker, M.A.; Islam, K.; Jahan, H.; et al. Hygiene intervention reduces contamination of weaning food in Bangladesh. Trop. Med. Int. Health 2013, 18, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Gautam, O.P.; Schmidt, W.-P.; Cairncross, S.; Cavill, S.; Curtis, V. Trial of a Novel Intervention to Improve Multiple Food Hygiene Behaviors in Nepal. Am. J. Trop. Med. Hyg. 2017, 96, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- Manjang, B.; Hemming, K.; Bradley, C.; Ensink, J.; Martin, J.T.; Sowe, J.; Jarju, A.; Cairncross, S.; Manaseki-Holland, S. Promoting hygienic weaning food handling practices through a community-based programme: Intervention implementation and baseline characteristics for a cluster randomised controlled trial in rural Gambia. BMJ Open 2018, 8, e017573. [Google Scholar] [CrossRef] [PubMed]
- National Statistical Office. Malawi Demographic and Health Survey 2015–16; National Statistical Office: Zomba, Malawi, 2017; pp. 1–658. [Google Scholar]
- National Statistical Office. Malawi MDG Endline Survey (MES) 2014 Report; National Statistical Office: Zomba, Malawi, 2014. [Google Scholar]
- Malawi National Statistical Office. Malawi Integrated Household Survey—Household Socio-Economic Characteristics Report; Malawi National Statistical Office: Zomba, Malawi, 2017. [Google Scholar]
- Gautam, O. Food Hygiene Intervention to Improve Food Hygiene Behaviours, and Reduce Food Contamination in Nepal: An Exploratory Trial. Ph.D. Thesis, London School of Hygiene & Tropical Medicine, London, UK, 2015. Available online: http://researchonline.lshtm.ac.uk/2531624/ (accessed on 26 August 2019). [CrossRef]
- Rippon, S.; Beattie, T.; Lungu, K.; Kumwenda, S.; Morse, T. Social capital insights from Healthy Settings needs assessment in Malawi. PLoS ONE 2018, 13, e0206156. [Google Scholar] [CrossRef] [PubMed]
- PATH. Charting the Course for Integrated Diarrhea Control in Malawi; PATH: Washington DC, USA, 2011; Available online: https://path.azureedge.net/media/documents/VAC_malawi_policy_fs.pdf (accessed on 26 August 2019).
- Contzen, N.; Meili, I.H.; Mosler, H.-J.; Molser, H.-J. Changing handwashing behaviour in southern Ethiopia: A longitudinal study on infrastructural and commitment interventions. Soc. Sci. Med. 2015, 124, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Lilje, J.; Kessely, H.; Mosler, H.-J. Factors Determining Water Treatment Behavior for the Prevention of Cholera in Chad. Am. J. Trop. Med. Hyg. 2015, 93, 57–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tumwebaze, I.K.; Orach, C.G.; Niwagaba, C.; Lüthi, C.; Mosler, H.-J. Sanitation facilities in Kampala slums, Uganda: users’ satisfaction and determinant factors. Int. J. Environ. Health Res. 2013, 23, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Huber, A.C.; Tobias, R.; Mosler, H.J. Evidence-based tailoring of behavior-change campaigns: Increasing fluoride-free water consumption in rural ethiopia with persuasion. Appl. Psychol. Health Well-Being 2014, 6. [Google Scholar] [CrossRef]
- Manda-Taylor, L.; Mwale, D.; Phiri, T.; Walsh, A.; Matthews, A.; Brugha, R.; Mwapasa, V.; Byrne, E. Changing times? Gender roles and relationships in maternal, newborn and child health in Malawi. BMC Pregnancy Childbirth 2017, 17, 321. [Google Scholar] [CrossRef] [PubMed]
- Zimba, E.; Kinney, M.V.; Kachale, F.; Waltensperger, K.Z.; Blencowe, H.; Colbourn, T.; George, J.; Mwansambo, C.; Joshua, M.; Chanza, H.; et al. Newborn survival in Malawi: A decade of change and future implications. Health Policy Plan. 2012, 27, 88–103. [Google Scholar] [CrossRef] [PubMed]
- Rutterford, C.; Copas, A.; Eldridge, S. Methods for sample size determination in cluster randomized trials. Int. J. Epidemiol. 2015, 44, 1051–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Targeted Behavior | Sub Item | Group Factor | Behavioral Factors | Motivational Drivers |
|---|---|---|---|---|
| Hand washing with soap at critical times: |
| Norm |
| Status and affiliation |
| Ability |
| |||
| Self-regulation |
| |||
| Attitude |
| |||
| Food hygiene |
| Ability |
| Affiliation, purity, nurture and attraction |
| Attitude |
| |||
| Norm |
| |||
| Risk |
| ||
| Norm |
| |||
| Ability |
| |||
| Attitude |
| ||
| Norms |
| |||
| Abilities |
| |||
| Attitude |
| ||
| Norms |
| |||
| Ability |
| |||
| Animal and child feces management |
| Risk |
| Disgust, diseases and status |
| Norm |
| |||
| Ability |
| |||
| Household water management |
| Risk |
| Affiliation, purity, diseases and disgust |
| Attitude |
| |||
| Risk |
| ||
| Norms |
| |||
| Ability |
|
| Treatment 1 | Treatment 2 | Control | |
|---|---|---|---|
| N (unless noted otherwise) | 400 | 400 | 200 |
| Female child | 0.49 | 0.52 | 0.55 |
| Child has a Health passport | 0.96 | 0.96 | 0.98 |
| Age distribution 1–5 months | 0.21 | 0.21 | 0.17 |
| 6–11 months | 0.28 | 0.31 | 0.31 |
| 12–17 months | 0.32 | 0.31 | 0.37 |
| 18+ months | 0.19 | 0.18 | 0.16 |
| Health status | |||
| Vaccinations | |||
| BCG (TB) vaccination at birth | 0.97 | 0.98 | 0.99 |
| Oral Polio Vaccine (OPV) at birth | 0.91 | 0.89 | 0.98 |
| % of eligible children at 6 weeks receiving OPV; Diphtheria, Pertussis, Tetanus, Hepatitis B, Influenza B | 0.96 | 0.97 | 0.98 |
| % of eligible children at 10 weeks receiving OPV; Diphtheria, Pertussis, Tetanus, Hepatitis B, Influenza B | 0.93 | 0.94 | 0.98 |
| % of eligible children at 14 weeks receiving OPV; Diphtheria, Pertussis, Tetanus, Hepatitis B, Influenza B | 0.87 | 0.84 | 0.89 |
| % of eligible children at 6 months receiving Vitamin A | 0.78 | 0.68 | 0.80 |
| % of eligible children at 9 months receiving Measles, Mumps and Rubella | 0.87 | 0.77 | 0.93 |
| % of eligible children at 12 months receiving Vitamin A | 0.68 | 0.55 | 0.61 |
| % of eligible children at 18 months receiving Vitamin A | 0.71 | 0.56 | 0.58 |
| Illness in last 2 weeks | |||
| Child had diarrhea in the last 2 weeks | 0.45 | 0.45 | 0.43 |
| Child was treated | 0.35 | 0.34 | 0.24 |
| Children <6 months | 0.21 | 0.21 | 0.17 |
| Who had diarrhea in the last 2 weeks | 0.13 | 0.16 | 0.18 |
| Children 6–11 months | 0.28 | 0.31 | 0.31 |
| Who had diarrhea in the last 2 weeks | 0.54 | 0.54 | 0.48 |
| Children 12–23 months | 0.51 | 0.49 | 0.52 |
| Who had diarrhea in the last 2 weeks | 0.53 | 0.51 | 0.47 |
| Child had respiratory infection in last 2 weeks | 0.56 | 0.62 | 0.57 |
| Child was treated | 0.43 | 0.48 | 0.34 |
| Child had skin infection in last 2 weeks | 0.18 | 0.18 | 0.20 |
| Child had eye infection in last 2 weeks | 0.05 | 0.04 | 0.04 |
| Child had ringworm in last 2 weeks | 0.02 | 0.01 | 0.00 |
| Child had schistosomiasis in last 2 weeks | 0.01 | 0.00 | 0.00 |
| Child Feeding | |||
| Child is breastfeeding | 0.98 | 0.99 | 1.00 |
| Among breastfeeding children, child drinks water | 0.86 | 0.89 | 0.86 |
| Child eats solid food | 0.82 | 0.85 | 0.85 |
| Number of meals child had yesterday (N = 799) * | 2.22 | 2.12 | 2.13 |
| Sanitation and Hygiene | |||
| Where nappies are disposed of | |||
| Household yard | 0.1 | 0.15 | 0.19 |
| Pit latrine | 0.82 | 0.77 | 0.65 |
| Various | 0.03 | 0.03 | 0.07 |
| Other | 0.05 | 0.06 | 0.10 |
| Flies are visible | 0.59 | 0.55 | 0.51 |
| Hand washing facility exists | 0.36 | 0.18 | 0.23 |
| Of those with facility, facility type | |||
| Basin + jug | 0.16 | 0.38 | 0.09 |
| Handmade from bottle | 0.79 | 0.56 | 0.91 |
| Other | 0.05 | 0.07 | 0.00 |
| Household has soap | 0.61 | 0.59 | 0.63 |
| Of households with soap | |||
| Used for bathing | 0.65 | 0.60 | 0.70 |
| Used for clothes washing | 0.82 | 0.81 | 0.82 |
| Used for washing hands | 0.62 | 0.56 | 0.47 |
| Used for washing kitchen utensils | 0.46 | 0.53 | 0.56 |
| Drinking water | |||
| Drinking water storage | |||
| Metal bucket | 0.00 | 0.00 | 0.00 |
| Plastic bucket | 0.24 | 0.37 | 0.38 |
| Jerrycan | 0.22 | 0.32 | 0.30 |
| Clay pot | 0.52 | 0.26 | 0.25 |
| Other | 0.02 | 0.06 | 0.09 |
| Average total volume of water storage (L) * | 98 | 117 | 101 |
| Water storage method | |||
| not covered | 0.14 | 0.13 | 0.25 |
| cover | 0.14 | 0.13 | 0.12 |
| total cover | 0.72 | 0.72 | 0.58 |
| not observed | 0.00 | 0.02 | 0.05 |
| Animal ownership | |||
| Number of animals that the household owns * | 1.43 | 1.44 | 1.20 |
| Outcome | Variable | Method of Measurement | Point of Measurement |
|---|---|---|---|
| Primary | Diarrheal disease | Self reporting Household/Cluster checks with community volunteer Community health worker reports | Continuous Baseline (illness 2 weeks prior) End line (illness 2 weeks prior) |
| Secondary | Health
| Self reporting | Continuous Baseline (illness 2 weeks prior) End line (illness 2 weeks prior) |
| Behavioral factors and changes | Risks, Attitudes, Norms, Abilities and Self Regulation questionnaire Observations | Baseline Midline End line | |
| Changes in household environment | Checklists Observations | Fortnightly checklists Baseline End line | |
Microbiological contamination of
| Microbiological testing for:
| End line 100 households per treatment arm and control | |
| Non-WASH benefits | Community networks analysis Social capital measurement | End line |
| Intervention Package | Event | Purpose | Key Content |
|---|---|---|---|
| Handwashing with soap (7 weeks) | First to fourth cluster meeting |
|
|
| First to third household visit |
|
| |
| Food hygiene (15 weeks) | First to eighth cluster meeting |
|
|
| First to seventh household visit |
|
| |
| Child and animal feces management (5 weeks) | First to third cluster meeting |
|
|
| First to second household visit |
|
| |
| Household water management (4 weeks) | First to second cluster meeting |
|
|
| First to second household visit |
|
|
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morse, T.; Chidziwisano, K.; Tilley, E.; Malolo, R.; Kumwenda, S.; Musaya, J.; Cairncross, S. Developing a Contextually Appropriate Integrated Hygiene Intervention to Achieve Sustained Reductions in Diarrheal Diseases. Sustainability 2019, 11, 4656. https://doi.org/10.3390/su11174656
Morse T, Chidziwisano K, Tilley E, Malolo R, Kumwenda S, Musaya J, Cairncross S. Developing a Contextually Appropriate Integrated Hygiene Intervention to Achieve Sustained Reductions in Diarrheal Diseases. Sustainability. 2019; 11(17):4656. https://doi.org/10.3390/su11174656
Chicago/Turabian StyleMorse, Tracy, Kondwani Chidziwisano, Elizabeth Tilley, Rossanie Malolo, Save Kumwenda, Janelisa Musaya, and Sandy Cairncross. 2019. "Developing a Contextually Appropriate Integrated Hygiene Intervention to Achieve Sustained Reductions in Diarrheal Diseases" Sustainability 11, no. 17: 4656. https://doi.org/10.3390/su11174656
APA StyleMorse, T., Chidziwisano, K., Tilley, E., Malolo, R., Kumwenda, S., Musaya, J., & Cairncross, S. (2019). Developing a Contextually Appropriate Integrated Hygiene Intervention to Achieve Sustained Reductions in Diarrheal Diseases. Sustainability, 11(17), 4656. https://doi.org/10.3390/su11174656





