Does Online Social Connectivity Promote Physical Activity in a Wearable Tracker-Based Intervention? A Pilot Randomized Controlled Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anthropometric and Blood Pressure
2.3. Intervention
2.4. Wearable Activity Tracker
2.5. Self-Efficacy, Exercise Motivation, and Social Support Questionnaire
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lee, J.M.; Kim, Y.; Welk, G.J. Validity of consumer-based physical activity monitors. Med. Sci. Sports Exerc. 2014, 46, 1840–1848. [Google Scholar] [CrossRef]
- Friedenreich, C.M.; Orenstein, M.R. Physical activity and cancer prevention: Etiologic evidence and biological mechanisms. J. Nutr. 2002, 132, 3456S–3464S. [Google Scholar] [CrossRef]
- Blackwell, D.L.; Clarke, T.C. State Variation in Meeting the 2008 Federal Guidelines for Both Aerobic and Muscle-strengthening Activities Through Leisure-time Physical Activity Among Adults Aged 18–64: United States, 2010-2015. Natl. Health Stat. Rep. 2018, 112, 1–22. [Google Scholar]
- Schmid, D.; Ricci, C.; Baumeister, S.E.; Leitzmann, M.F. Replacing Sedentary Time with Physical Activity in Relation to Mortality. Med. Sci. Sports Exerc. 2016, 48, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Leider, J.; Chriqui, J.F.; Thrun, E. Associations between active living-oriented zoning and no adult leisure-time physical activity in the US. Prev. Med. 2016, 95, S120–S125. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhu, X.; Welk, G.J.; Kim, Y.; Lee, J.; Meier, N.F. Using Sensewear armband and diet journal to promote adolescents’ energy balance knowledge and motivation. J. Sport Health Sci. 2014, 3, 326–332. [Google Scholar] [CrossRef]
- Brickwood, K.-J.; Watson, G.; O’Brien, J.; Williams, A.D. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e11819. [Google Scholar] [CrossRef]
- Böhm, B.; Karwiese, S.D.; Böhm, H.; Oberhoffer, R. Effects of Mobile Health Including Wearable Activity Trackers to Increase Physical Activity Outcomes Among Healthy Children and Adolescents: Systematic Review. JMIR mHealth uHealth 2019, 7, e8298. [Google Scholar] [CrossRef]
- Bravata, D.M.; Smith-Spangler, C.; Sundaram, V.; Gienger, A.L.; Lin, N.; Lewis, R.; Stave, C.D.; Olkin, I.; Sirard, J.R. Using pedometers to increase physical activity and improve health: A systematic review. J. Am. Med. Assoc. 2007, 298, 2296–2304. [Google Scholar] [CrossRef]
- Ridgers, N.D.; Timperio, A.; Brown, H.; Ball, K.; Macfarlane, S.; Lai, S.K.; Richards, K.; Mackintosh, K.A.; McNarry, M.A.; Foster, M. Wearable activity tracker use among Australian adolescents: Usability and acceptability study. JMIR mHealth uHealth 2018, 6, e86. [Google Scholar] [CrossRef]
- Lynch, B.M.; Nguyen, N.H.; Moore, M.M.; Reeves, M.M.; Rosenberg, D.; Boyle, T.; Vallance, J.K.; Milton, S.; Friedenreich, C.M.; English, D.R. A randomized controlled trial of a wearable technology-based intervention for increasing moderate to vigorous physical activity and reducing sedentary behavior in breast cancer survivors: The ACTIVATE Trial. Cancer 2019, 125, 2846–2855. [Google Scholar] [PubMed]
- Kononova, A.; Li, L.; Kamp, K.; Bowen, M.; Rikard, R.; Cotten, S.; Peng, W. The Use of Wearable Activity Trackers Among Older Adults: Focus Group Study of Tracker Perceptions, Motivators, and Barriers in the Maintenance Stage of Behavior Change. JMIR mHealth uHealth 2019, 7, e9832. [Google Scholar] [CrossRef] [PubMed]
- Franklin, N.C. Technology to promote and increase physical activity in heart failure. Heart Fail. Clin. 2015, 11, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.B.; Cadmus-Bertram, L.A.; Natarajan, L.; White, M.M.; Madanat, H.; Nichols, J.F.; Ayala, G.X.; Pierce, J.P. Wearable sensor/device (Fitbit One) and SMS text-messaging prompts to increase physical activity in overweight and obese adults: A randomized controlled trial. Telemed. e-Health 2015, 21, 782–792. [Google Scholar] [CrossRef]
- Cadmus-Bertram, L.; Marcus, B.H.; Patterson, R.E.; Parker, B.A.; Morey, B.L. Use of the Fitbit to Measure Adherence to a Physical Activity Intervention Among Overweight or Obese, Postmenopausal Women: Self-Monitoring Trajectory During 16 Weeks. JMIR mHealth uHealth 2015, 3, e96. [Google Scholar] [CrossRef]
- Jakicic, J.M.; Davis, K.K.; Rogers, R.J.; King, W.C.; Marcus, M.D.; Helsel, D.; Rickman, A.D.; Wahed, A.S.; Belle, S.H. Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: The IDEA randomized clinical trial. J. Am. Med. Assoc. 2016, 316, 1161–1171. [Google Scholar] [CrossRef]
- Culhane, K.M.; O’Connor, M.; Lyons, D.; Lyons, G.M. Accelerometers in rehabilitation medicine for older adults. Age Ageing 2005, 34, 556–560. [Google Scholar] [CrossRef]
- Kang, M.; Bassett, D.R.; Barreira, T.V.; Tudor-Locke, C.; Ainsworth, B.; Reis, J.P.; Strath, S.; Swartz, A. How many days are enough? A study of 365 days of pedometer monitoring. Res. Q. Exerc. Sport 2009, 80, 445–453. [Google Scholar] [CrossRef]
- An, H.-S.; Jones, G.C.; Kang, S.-K.; Welk, G.J.; Lee, J.-M. How valid are wearable physical activity trackers for measuring steps? Eur. J. Sport Sci. 2016, 17, 360–368. [Google Scholar] [CrossRef]
- Kooiman, T.J.; Dontje, M.L.; Sprenger, S.R.; Krijnen, W.P.; van der Schans, C.P.; de Groot, M. Reliability and validity of ten consumer activity trackers. BMC Sports Sci. Med. Rehabil. 2015, 7, 1–11. [Google Scholar] [CrossRef]
- Luszczynska, A.; Scholz, U.; Schwarzer, R. The general self-efficacy scale: Multicultural validation studies. J. Psychol. 2005, 139, 439–457. [Google Scholar] [CrossRef] [PubMed]
- Mullan, E.; Markland, D. Variations in self-determination across the stages of change for exercise in adults. Motiv. Emot. 1997, 21, 349–362. [Google Scholar] [CrossRef]
- Markland, D.; Tobin, V. A modification to the behavioural regulation in exercise questionnaire to include an assessment of amotivation. J. Sport Exerc. Psychol. 2004, 26, 191–196. [Google Scholar] [CrossRef]
- Sallis, J.F.; Grossman, R.M.; Pinski, R.B.; Patterson, T.L.; Nader, P.R. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987, 16, 825–836. [Google Scholar] [CrossRef]
- Liang, Y.; Lau, P.W.; Huang, W.Y.; Maddison, R.; Baranowski, T. Validity and reliability of questionnaires measuring physical activity self-efficacy, enjoyment, social support among Hong Kong Chinese children. Prev. Med. Rep. 2014, 1, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Fjeldsoe, B.S.; Miller, Y.D.; Marshall, A.L. MobileMums: A randomized controlled trial of an SMS-based physical activity intervention. Ann. Behav. Med. 2010, 39, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Gerber, B.S.; Stolley, M.R.; Thompson, A.L.; Sharp, L.K.; Fitzgibbon, M.L. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: A feasibility study. Health Inform. J. 2009, 15, 17–25. [Google Scholar] [CrossRef]
- Napolitano, M.A.; Hayes, S.; Bennett, G.G.; Ives, A.K.; Foster, G.D. Using Facebook and Text Messaging to Deliver a Weight Loss Program to College Students. Obesity 2013, 21, 25–31. [Google Scholar] [CrossRef]
- Patrick, K.; Raab, F.; Adams, M.A.; Dillon, L.; Zabinski, M.; Rock, C.L.; Griswold, W.G.; Norman, G.J. A text message-based intervention for weight loss: Randomized controlled trial. J. Med. Internet Res. 2009, 11, e1. [Google Scholar] [CrossRef]
- Shapiro, J.R.; Bauer, S.; Hamer, R.M.; Kordy, H.; Ward, D.; Bulik, C.M. Use of Text Messaging for Monitoring Sugar-sweetened Beverages, Physical Activity, and Screen Time in Children: A Pilot Study. J. Nutr. Educ. Behav. 2008, 40, 385–391. [Google Scholar] [CrossRef]
- Aittasalo, M.; Miilunpalo, S.; Kukkonen-Harjula, K.; Pasanen, M. A randomized intervention of physical activity promotion and patient self-monitoring in primary health care. Prev. Med. 2006, 42, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.J.; Vandelanotte, C.; Trost, S.G.; Rebar, A.L.; Rogers, N.; Burton, N.W.; Murawski, B.; Rayward, A.; Fenton, S.; Brown, W.J. Balanced: A randomised trial examining the efficacy of two self-monitoring methods for an app-based multi-behaviour intervention to improve physical activity, sitting and sleep in adults. BMC Public Health 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Conroy, M.B.; Yang, K.; Elci, O.U.; Gabriel, K.P.; Styn, M.A.; Wang, J.; Kriska, A.M.; Sereika, S.M.; Burke, L.E. Physical activity self-monitoring and weight loss: 6-month results of the SMART trial. Med. Sci. Sports Exerc. 2011, 43, 1568–1574. [Google Scholar] [CrossRef] [PubMed]
- Turner-McGrievy, G.M.; Beets, M.W.; Moore, J.B.; Kaczynski, A.T.; Barr-Anderson, D.J.; Tate, D.F. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J. Am. Med. Inform. Assoc. 2013, 20, 513–518. [Google Scholar] [CrossRef]
- Kouvonen, A.; De Vogli, R.; Stafford, M.; Shipley, M.J.; Marmot, M.G.; Cox, T.; Vahtera, J.; Väänänen, A.; Heponiemi, T.; Singh-Manoux, A.; et al. Social support and the likelihood of maintaining and improving levels of physical activity: The Whitehall II Study. Eur. J. Public Health 2011, 22, 514–518. [Google Scholar] [CrossRef]
- Morrissey, J.L.; Janz, K.F.; Letuchy, E.M.; Francis, S.L.; Levy, S.M. The effect of family and friend support on physical activity through adolescence: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 103. [Google Scholar] [CrossRef]
- Laird, Y.; Fawkner, S.; Kelly, P.; McNamee, L.; Niven, A. The role of social support on physical activity behaviour in adolescent girls: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 1–14. [Google Scholar] [CrossRef]
- Booth, M.L.; Owen, N.; Bauman, A.; Clavisi, O.; Leslie, E. Social–cognitive and perceived environment influences associated with physical activity in older Australians. Prev. Med. 2000, 31, 15–22. [Google Scholar] [CrossRef]
| Individual (n = 20) | Connected Group (n = 20) | G x T | η2p | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Post | ES | Baseline | Post | ES | |||
| Weight (kg) | 72.55 ± 15.09 (65.7 to 79.44) | 72.97 ± 15.39 (66.09 to 79.84) | 0.18 | 68.68 ± 15.32 (61.79 to75.56) | 68.87 ± 14.97 (62.00 to 75.75) | 0.11 | 0.17 | 0.01 |
| BMI (kg·m−2) | 23.58 ± 3.62 (22.01 to 25.15) | 23.70 ± 3.63 (22.14 to 25.25) | 0.17 | 24.52 ± 3.31 (22.95 to 26.09) | 24.61 ± 3.24 (23.05 to 26.17) | 0.82 | 0.02 | 0.00 |
| WC (cm) | 80.52 ± 8.17 (76.23 to 84.81) | 79.23 ± 7.79 (75.14 to 83.34) | 0.14 | 79.55 ± 10.63 (75.26 to 83.84) | 79.95 ± 10.17 (75.85 to 84.05) | 0.14 | 2.96 | 0.07 |
| Body fat (%) | 18.97 ± 8.28 (15.69 to 22.24) | 19.58 ± 8.19 (16.27 to 22.88) | 0.03 | 23.54 ± 6.03 (20.26 to 26.82) | 23.08 ± 6.29 (19.77 to 26.38) | 0.25 | 2.7 | 0.01 |
| SBP (mmHg) | 117.60 ± 11.82 (111.72 to 123.48) | 106.25 ± 21.78 (97.65 to 114.85) | 0.33 | 115.8 ± 14.07 (109.92 to 121.68) | 115.05 ± 15.75 (106.45 to 123.65) | 0.07 | 3.57 | 0.09 |
| DBP (mmHg) | 75.25 ± 6.47 (70.80 to 77.70) | 70.10 ± 5.74 (66.66 to 73.55) | 0.58 | 80.0 ± 8.62 (76.55 to 83.45) | 76.55 ± 9.10 (73.11 to 80.00) | 0.52 | 0.11 | 0.00 |
| EM | 68.21 ± 10.57 (63.06 to 73.37) | 69.00 ± 8.98 (64.53 to 73.47) | 0.11 | 70.21 ± 11.61 (64.21 to 76.22) | 72.29 ± 10.32 (67.07 to 77.50) | 0.17 | 0.17 | 0.01 |
| Self-efficient | 70.35 ± 25.79 (57.99 to 82.71) | 68.80 ± 20.13 (68.27 to 93.63) | 0.06 | 72.57 ± 22.54 (59.11 to 78.49) | 70.14 ± 22.86 (58.56 to 81.73) | 0.22 | 0.01 | 0.00 |
| Social support | N/A | 26.17 ± 9.78 (21.30 to 31.03) | 29.72 ± 10.80 *** (24.35 to 35.09) | 0.46 | ||||
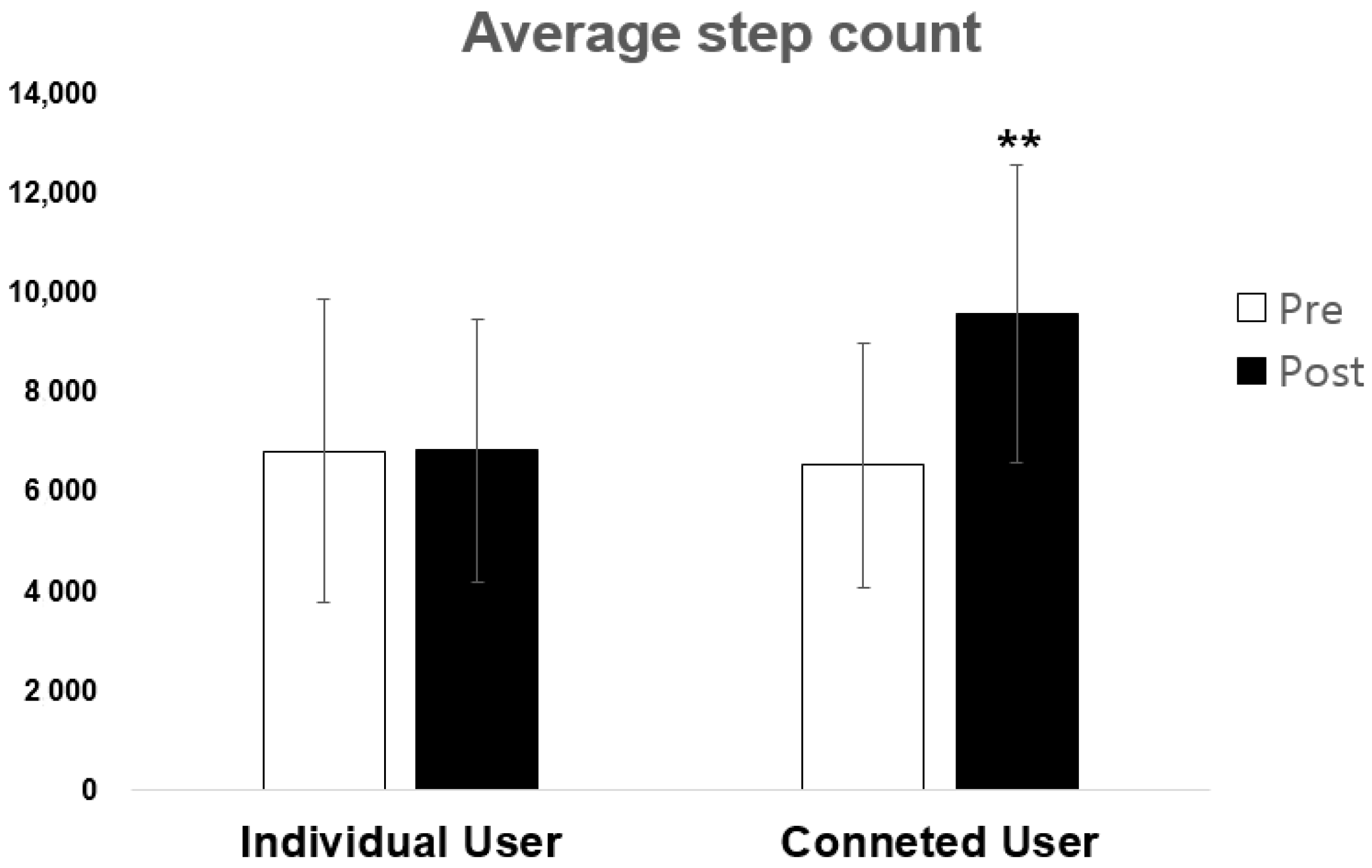
| Individual Users | Connected Users | Independent ES | |||
|---|---|---|---|---|---|
| Step Count | Dependent ES | Step Count | Dependent ES | ||
| Baseline | 6805.16 ± 3061.43 | 6516.11 ± 2465.88 | 0.14 | ||
| Vs. Week 1 | 7021.91 ± 3447.47 | 0.15 | 9565.03 ± 3379.29 | 1.53 *** | 0.75 |
| Vs. Week 2 | 6685.69± 2879.95 | 0.08 | 9749.37 ± 3914.10 | 1.47 *** | 0.90 |
| Vs. Week 3 | 6927.22 ± 3302.31 | 0.07 | 9694.43 ± 3384.53 | 1.52 *** | 0.82 |
| Vs. Week 4 | 6430.2 ± 2650.97 | 0.20 | 9717.04 ± 3334.59 | 1.19 *** | 1.10 |
| Vs. Week 5 | 6060.75 ± 2493.23 | 0.39 | 8649.07 ± 2762.55 | 1.40 *** | 0.98 |
| Vs. Week 6 | 6706.56 ± 3498.66 | 0.03 | 9007.20 ± 32214.88 | 1.44 ** | 0.69 |
| Vs. Week 7 | 7710.34 ± 2780.29 | 0.76 * | 10476.00 ± 4743.73 | 1.10 ** | 0.58 |
| Vs. Week 8 | 6747.19 ± 2806.32 | 0.09 | 9275.14 ± 3147.57 | 1.24 *** | 0.65 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, M.-W.; Kim, Y.; Jung, H.C.; Kim, J.-H.; Lee, J.-M. Does Online Social Connectivity Promote Physical Activity in a Wearable Tracker-Based Intervention? A Pilot Randomized Controlled Study. Sustainability 2020, 12, 8803. https://doi.org/10.3390/su12218803
Seo M-W, Kim Y, Jung HC, Kim J-H, Lee J-M. Does Online Social Connectivity Promote Physical Activity in a Wearable Tracker-Based Intervention? A Pilot Randomized Controlled Study. Sustainability. 2020; 12(21):8803. https://doi.org/10.3390/su12218803
Chicago/Turabian StyleSeo, Myong-Won, Youngdeok Kim, Hyun Chul Jung, Jung-Hyun Kim, and Jung-Min Lee. 2020. "Does Online Social Connectivity Promote Physical Activity in a Wearable Tracker-Based Intervention? A Pilot Randomized Controlled Study" Sustainability 12, no. 21: 8803. https://doi.org/10.3390/su12218803
APA StyleSeo, M.-W., Kim, Y., Jung, H. C., Kim, J.-H., & Lee, J.-M. (2020). Does Online Social Connectivity Promote Physical Activity in a Wearable Tracker-Based Intervention? A Pilot Randomized Controlled Study. Sustainability, 12(21), 8803. https://doi.org/10.3390/su12218803







