Effects of a Yoga Program in Reducing Cardiovascular Disease Risk Factors in Workers of Small Workplaces: A Pilot Test
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
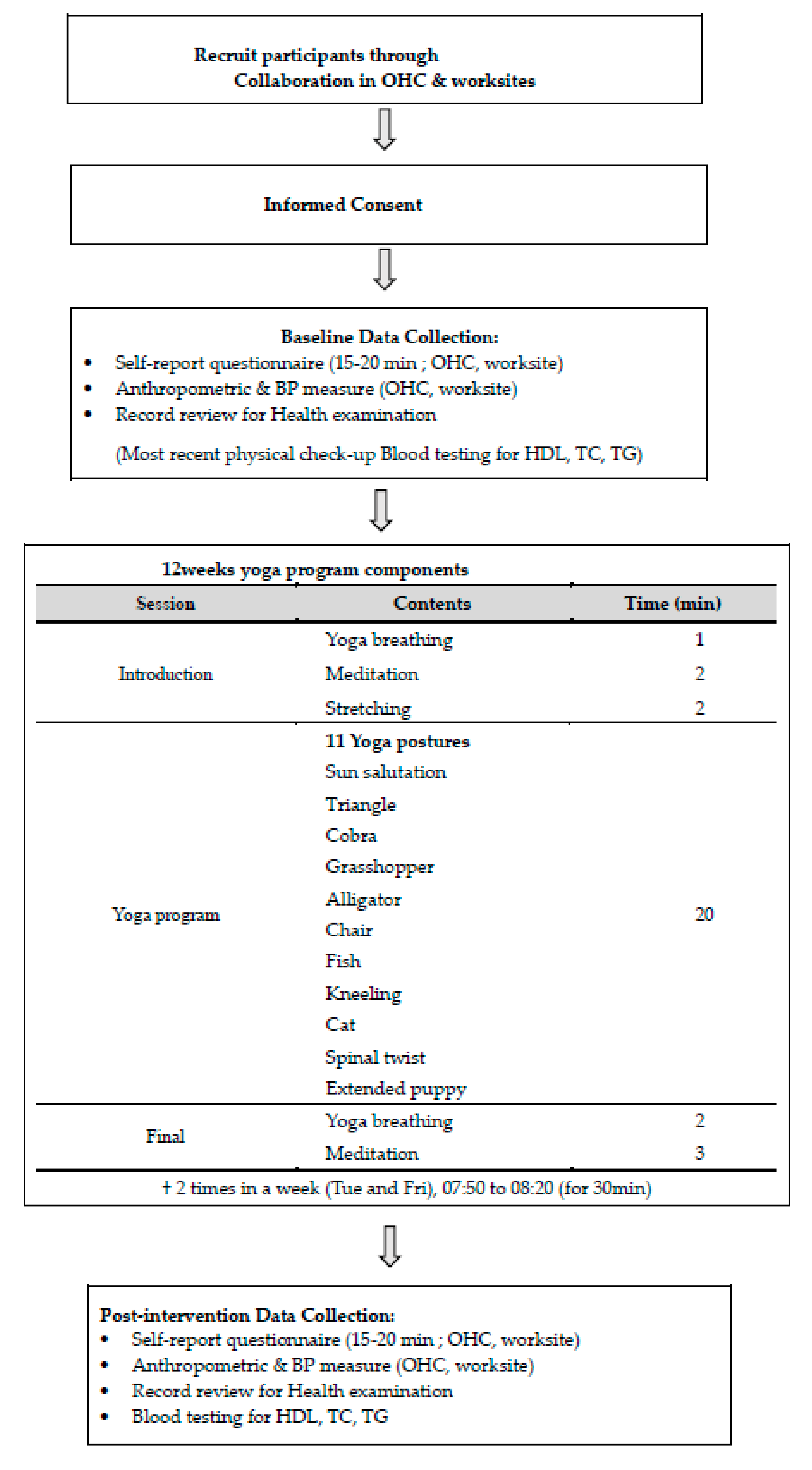
2.2. Experimental Design
2.2.1. Development of a Yoga Program
2.2.2. Baseline Measurement in Experimental and Control Groups
2.2.3. Experimental Treatment: Yoga Program
2.2.4. Post-Intervention Measurement in Experimental and Control Groups
2.3. Ethical Considerations
2.4. Measurements
2.4.1. Depressive Symptoms
2.4.2. Job Stress
2.4.3. Health-Promoting Behaviors
2.5. Data Analysis
3. Results
3.1. Homogeneity Testing
3.2. Psychosocial CVD Risk Factor
3.3. Physical CVD Risk Factor
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ministry of Employment and Labor. Analysis of Industrial Accident Outages; Ministry of Employment and Labor: Sejong, Korea, 2019. Available online: http://www.moel.go.kr/info/publict/publictDataView.do?bbs_seq=20191201074 (accessed on 20 November 2020).
- Hwang, W.J.; Kim, J.A. Developing a Health-Promotion Program Based on the Action Research Paradigm to Reduce Cardiovascular Disease Risk Factors among Blue Collar Workers. Int. J. Environ. Res. Public Health 2019, 16, 4958. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.A.; Hwang, W.J.; Jin, J. An Exploration of Contextual Aspects that Influence Cardiovascular Disease Risks Perceived by Workers in a Small–Medium-Sized Workplace. Int. J. Environ. Res. Public Health 2020, 17, 5155. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Park, Y. Ecological correlates of cardiovascular disease risk in Korean blue-collar workers: A multi-level study. J. Korean Acad. Nurs. 2015, 45, 857–867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.L.; Jung, H.S.; Lee, J.E.; Yi, U.J.; Kim, Y.G.; Lee, S.S.; Kim, E.-S. Cardiovascular disease management among workers in small-sized enterprise using community-based approach. Korean J. Occup. Health Nurs. 2010, 19, 70–77. [Google Scholar]
- Hwang, W.J.; Park, Y.; Kim, J.A. A systematic review of interventions for workers with cardiovascular disease risk factors: Using an ecological model. Korean J. Occup. Health Nurs. 2016, 25, 41–54. [Google Scholar] [CrossRef]
- Stress at Work. National Institute for Occupational Safety and Health. 30 December 1999. Available online: http://www.cdc.gov/niosh/docs/99-101/ (accessed on 11 September 2019).
- Catalina-Romero, C.; Calvo, E.; Sánchez-Chaparro, M.A.; Valdivielso, P.; Sainz, J.C.; Cabrera, M.; Gonzalez-Quintela, A.; Roman, J. The relationship between job stress and dyslipidemia. Scand. J. Public Health 2013, 41, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Kang, S.J. Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 2267. [Google Scholar] [CrossRef] [Green Version]
- Vitaliano, P.P.; Scanlan, J.M.; Zhang, J.; Savage, M.V.; Hirsch, I.B.; Siegler, I.C. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Am. Psychosomat. Med. 2002, 64, 418–435. [Google Scholar] [CrossRef]
- Kim, T.H.; Jung, M.H.; Lee, S.H. A study on correlation between job stress and metabolic syndrome of male employees of electronic goods manufacturer. Korean J. Occup. Health Nurs. 2016, 25, 55–64. [Google Scholar] [CrossRef] [Green Version]
- Hwang, C.K.; Koh, S.B.; Chang, S.J.; Park, C.Y.; Cha, B.S.; Hyun, S.J.; Park, J.H.; Lee, K.M.; Cha, K.T.; Park, W.J.; et al. Occupational stress in relation to cerebrovascular and cardiovascular disease: Longitudinal analysis from the NSDSOS Project. Korean J. Occup. Environ. Med. 2007, 19, 105–114. [Google Scholar] [CrossRef]
- Huh, J.Y.; An, H.J. The effects of yoga performance on mental health in menopause women. Korean J. Sports Sci. 2007, 16, 361–371. [Google Scholar]
- Kim, M.G.; Kim, K.S.; Ryoo, J.H.; Yoo, S.W. Relationship between Occupational Stress and Work-related Musculoskeletal Disorder in Korean Male Firefighters. Korean J. Occup. Environ. Med. 2013, 25, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, S.J.; Koh, S.B.; Kang, M.K.; Cha, B.S.; Park, J.K.; Hyun, S.J.; Park, J.H.; Kim, S.A.; Kang, D.M.; Chang, S.S.; et al. Epidemiology of psychosocial distress in Korean employees. Korean J. Prev. Med. 2005, 38, 25–37. [Google Scholar]
- Choi, E.S.; Ha, Y.M. Work-related stress and risk factors among Korean employees. J. Korean Acad. Nurs. 2009, 39, 549–561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riley, K.E.; Park, C.L. How does yoga reduce stress? A systematic review of mechanisms of change and guide to future injury. Health Psychol. Rev. 2015, 9, 379–396. [Google Scholar] [CrossRef]
- Michalsen, A.; Grossman, P.; Acil, A.; Langhorst, J.; Ludtke, R.; Esch, T. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three month intensive yoga program. Med. Sci. Monit. 2005, 11, 555–561. [Google Scholar]
- Park, J.G.; Lim, R.H. An effect of the 12 weeks the hatha yoga program for female physical fitness. Korean J. Phys. Ed. 2004, 43, 959–966. [Google Scholar]
- Parhad, O. Role of yoga in stress management. West Indian J. Med. 2004, 53, 191–194. [Google Scholar]
- Donesky-Cuenco, D.; Nguyen, H.Q.; Paul, S.; Carrieri-Kohlman, V. Yoga therapy decreases dyspnea-related distress and improves functional performance in people with chronic obstructive pulmonary disease: A pilot study. J. Altern. Complement. Med. 2009, 15, 225–234. [Google Scholar] [CrossRef]
- Lee, E.N.; An, H.J.; Song, Y.S.; Kim, J.H.; Cho, H.J.; Lee, M.H. The effects of a 4-weeks yoga program on mental Ⅲ inpatients’ anxiety and depression. J. Korean Acad. Psychiatric Ment. Health Nurs. 2008, 17, 161–170. [Google Scholar]
- Ko, J.E.; Kang, C.K.; Lee, M.G. Effects of a 10-week combined program of Hatha and Raja yoga on stress-related variables in middle-aged women. Korean J. Sports Sci. 2014, 23, 993–1006. [Google Scholar]
- Hasanpour-Dehkordi, A.; Jivad, N.; Solati, K. Effects of yoga on physiological indices, anxiety and social functioning in multiple sclerosis patients: A randomized trial. J. Clin. Diag. Res. 2016, 10, VC01–VC05. [Google Scholar] [CrossRef]
- Kligler, B.; Teets, R.; Quick, M. Complementary/integrative therapies that work: A review of the evidence. Am. Fam. Physician 2016, 94, 369–374. [Google Scholar] [PubMed]
- Yun, S.J.; Pack, S.H. The effect of yoga program on the changes in the daily stress the children’s. Off. J. Korean Soc. Dance Sci. 2014, 31, 185–195. [Google Scholar] [CrossRef]
- Park, H.S.; Kim, Y.J.; Kim, Y.H. The effect of yoga program on reduced blood pressure in elderly’s essential hypertension. J. Korean Acad. Nurs. 2002, 32, 633–642. [Google Scholar] [CrossRef]
- Park, Y.J. The effects of yoga program on stress and anxiety for worker. Korean Assoc. Mediat. Health 2013, 4, 13–24. [Google Scholar]
- Oh, H.S.; Lee, I.S. The effect of a yoga program on the stress levels of professionals. Perspect. Nurs. Sci. 2012, 9, 36–44. [Google Scholar]
- Tsai, S.Y. Effect of yoga exercise on premenstrual symptoms among female employees in Taiwan. Int. J. Environ. Res. Public Health 2016, 13, E721. [Google Scholar] [CrossRef] [Green Version]
- Thomley, B.S.; Ray, S.H.; Cha, S.S.; Bauer, B.A. Effects of a brief, comprehensive, yoga-based program on quality of life and biometric measures in an employee population: A pilot study. J. Sci. Health 2011, 7, 27–29. [Google Scholar] [CrossRef]
- Korea Occupational Safety & Health Agency. A Study on the Management Strategy of Workers’ Health for the Early Prevention of Cerebrocardio -Vascular Disease to Prepare for an Aging Society (2009-43-1084); Korea Occupational Safety & Health Research Institute: Incheon, Korea, 2009. [Google Scholar]
- Radloff, L.S. The CES-D scale, a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Cho, M.J.; Kim, K.H. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III-R major depression. J. Korean Neuropsychiatr. Assoc. 1993, 32, 381–399. [Google Scholar]
- Siegrist, J.; Starke, D.; Chandola, T.; Godin, I.; Marmot, M.; Niedhammer, I.; Peter, R. The measurement of effort–reward imbalance at work: European comparisons. Soc. Sci. Med. 2004, 58, 1483–1499. [Google Scholar] [CrossRef]
- Eum, K.D.; Li, J.; Lee, H.E.; Kim, S.S.; Paek, D.; Siegrist, J.; Cho, S.-I. Psychometric properties of the Korean version of the effort–reward imbalance questionnaire: A study in a petrochemical company. Int. Arch. Occup. Environ. Health 2007, 80, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Kim, J.A.; Rankin, S.H. Depressive Symptom and Related Factors: A Cross-Sectional Study of Korean Female Workers Working at Traditional Markets. Int. J. Environ. Res. Public Health 2017, 14, 1465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. The health promoting lifestyle profile: Development and psychometric characteristics. Nurs. Res. 1987, 36, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Hong, O.S.; Rankin, S.H. Predictors of health-promoting behavior associated with cardiovascular diseases among Korean blue-collar workers. Asia-Pac. J. Public Health 2015, 27, NP691–NP702. [Google Scholar] [CrossRef]
- Hilton, M.F.; Scuffham, P.A.; Vecchio, N.; Whiteford, H.A. Using the interaction of mental health symptoms and treatment status to estimate lost employee productivity. Aust. N. Z. J. Psychiatry 2010, 44, 151–161. [Google Scholar] [CrossRef]
- Burton, W.N.; Pransky, G.; Conti, D.J.; Chen, C.-Y.; Edington, D.W. The association of medical conditions and presenteeism. J. Occup. Environ. Med. 2004, 46, S38–S45. [Google Scholar] [CrossRef]
- Simard, A.-A.; Henry, M. Impact of a short yoga intervention on medical students’ health: A pilot study. Med. Teach. 2009, 31, 950–952. [Google Scholar] [CrossRef]
- Mitchell, K.S.; Dick, A.M.; DiMartino, D.M.; Smith, B.N.; Niles, B.; Koenen, K.C.; Street, A. A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. J. Traumatic. Stress 2014, 27, 121–128. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Haller, H.; Steckhan, N.; Michalsen, A.; Dobos, G. Effects of yoga on cardiovascular disease risk factors: A systematic review and meta-analysis. Int. J. Cardiol. 2014, 173, 170–183. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.S.; Shim, M.S. Affecting factors on depression among female labor workers. J. Korea Contents Assoc. 2011, 11, 822–831. [Google Scholar] [CrossRef]
- Tsutsumi, A.; Nagami, M.; Yoshikawa, T.; Kogi, K.; Kawakami, N. Participatory intervention for workplace improvements on mental health and job performance among blue-collar workers: A cluster randomized controlled trial. J. Occup. Environ. Med. 2009, 51, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Gu, M.O. Effects of community health promotion project for garlic cultivating farmers based on self-efficacy theory and community capacity building framework. J. Korean Acad. Nurs. 2011, 41, 80–91. [Google Scholar] [CrossRef] [PubMed]
- Kost, R.G.; Lee, L.M.; Yessis, J.; Coller, B.S.; Henderson, D.K.; Research Participant Perception Survey Focus Group Subcommittee. Assessing research participants’ perceptions of their clinical research experiences. Clin. Transl. Sci. 2011, 4, 403–413. [Google Scholar] [CrossRef]
- Kim, H.Y.; Kim, J.K.; Shin, G.G.; Han, J.A.; Kim, J.W. Association between abdominal obesity and cardiovascular risk factors in adults with normal body mass index: Based on the sixth Korea National Health and Nutrition Examination Survey. J. Obes. Metab. Syndr. 2019, 28, 262. [Google Scholar] [CrossRef] [Green Version]
- Westphal, S.A. Obesity, abdominal obesity, and insulin resistance. Clin. Cornerstone 2008, 9, 23–29. [Google Scholar] [CrossRef]
- Cramer, H.; Thoms, M.S.; Anheyer, D.; Lauche, R.; Dobos, G. Yoga in women with abdominal obesity—A randomized controlled trial. Dtsch. Arztebl. Int. 2016, 113, 645. [Google Scholar]
- Siu, P.M.; Angus, P.Y.; Benzie, I.F.; Woo, J. Effects of 1-year yoga on cardiovascular risk factors in middle-aged and older adults with metabolic syndrome: A randomized trial. Diabetol. Metab. Syndr. 2015, 7, 40. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | Categories | † Exp. (n = 31) | ‡ Cont. (n = 38) n (%)/Mean ± SD | χ2 or F | p | |||
|---|---|---|---|---|---|---|---|---|
| n (%)/Mean ± SD | Group 1 (n = 11) | Group 2 (n = 15) | Group 3 (n = 12) | Total (n = 38) | ||||
| Sex | Male | 14(45.2) | 6(54.5) | 6(40.0) | 8(66.7) | 20(52.6) | 0.38 | 0.354 |
| Female | 17(54.8) | 5(45.5) | 9(60.0) | 4(11.6) | 18(47.4) | |||
| Educational level | ≤Middle school | 3(9.7) | 0(0.0) | 1(6.7) | 2(16.7) | 3(7.9) | 2.89 | 0.235 |
| High school | 23(74.2) | 6(54.5) | 8(53.3) | 8(66.7) | 22(57.9) | |||
| ≥College | 5(16.1) | 5(45.5) | 6(40.0) | 2(16.7) | 13(34.1) | |||
| Marital status | Unmarried | 8(25.8) | 5(45.5) | 5(33.3) | 4(33.3) | 14(36.8) | 0.96 | 0.437 |
| Married | 23(74.2) | 6(54.5) | 10(66.7) | 8(66.7) | 24(63.2) | |||
| Monthly income (10.000 won) | ≤100 | 1(3.2) | 0(0.0) | 0(0.0) | 0(0.0) | 0(0.0) | 1.87 | 0.601 |
| 100~200 | 13(41.9) | 7(63.6) | 1(6.7) | 5(41.7) | 13(34.2) | |||
| 201~300 | 7(22.6) | 2(18.2) | 5(33.3) | 4(33.3) | 11(28.9) | |||
| ≥301 | 10(3203) | 2(18.2) | 9(60.0) | 3(25.0) | 14(36.8) | |||
| Working hours (/day) | 55.56 ± 4.71 | 55.45 ± 4.72 | 54.87 ± 5.23 | 55.00 ± 5.22) | 55.08 ± 4.96 | 0.38 | 0.707 | |
| Age (years) | 48.15 ± 8.26 | 49.46 ± 6.25 | 47.87 ± 8.98 | 45.92 ± 9.67 | 47.71 ± 8.41 | 0.21 | 0.845 | |
| Variables | Group | Pre-Test | Post-Test | Difference | p | Source | F | p |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||||||
| Depressive symptoms | † Exp. | 19.44 ± 8.08 | 19.81 ± 3.61 | −0.36 ± 7.97 | 0.798 | Group | 1.10 | 0.298 |
| Time | 0.56 | 0.457 | ||||||
| ‡ Cont. | 21.36 ± 6.89 | 20.18 ± 6.88 | 1.18 ± 10.83 | 0.504 | Group * Time | 7.52 | 0.008 | |
| Job stress | Exp. | 1.38 ± 1.80 | 1.02 ± 0.24 | 0.36 ± 1.81 | 0.280 | Group | 0.53 | 0.470 |
| Time | 1.43 | 0.236 | ||||||
| Cont. | 1.09 ± 0.32 | 1.09 ± 0.30 | 0.00 ± 0.37 | 0.980 | Group * Time | 1.40 | 0.240 | |
| Body weight (kg) | Exp. | 61.10 ± 12.65 | 62.07 ± 12.66 | −0.97 ± 5.88 | 0.364 | Group | 1.54 | 0.219 |
| Time | 1.18 | 0.282 | ||||||
| Cont. | 64.95 ± 11.15 | 65.08 ± 10.54 | −0.13 ± 2.00 | 0.688 | Group * Time | 0.68 | 0.411 | |
| Waist circumference (cm) | Exp. | 81.87 ± 8.01 | 79.21 ± 7.92 | 2.66 ± 2.47 | <0.001 | Group | 0.51 | 0.478 |
| Time | 29.21 | <0.001 | ||||||
| Cont. | 79.13 ± 8.27 | 79.16 ± 8.22 | −0.03 ± 1.55 | 0.917 | Group * Time | 30.39 | <0.001 | |
| Systolic blood pressure (mmHg) | Exp. | 128.48 ± 10.38 | 127.07 ± 10.64 | −1.41 ± 4.44 | 0.086 | Group | 0.01 | 0.961 |
| Time | 1.24 | 0.270 | ||||||
| Cont. | 127.47 ± 12.87 | 127.79 ± 13.14 | −0.32 ± 3.77 | 0.609 | Group * Time | 3.07 | 0.084 | |
| Diastolic blood pressure (mmHg) | Exp. | 81.04 ± 8.57 | 79.16 ± 8.11 | −1.88 ± 3.09 | 0.002 | Group | 1.40 | 0.242 |
| Time | 4.05 | 0.048 | ||||||
| Cont. | 82.29 ± 8.97 | 82.66 ± 8.09 | −0.37 ± 3.11 | 0.469 | Group * Time | 8.97 | 0.004 | |
| Total cholesterol (mg/dL) | Exp. | 201.19 ± 32.16 | 201.45 ± 33.81 | −0.27 ± 7.35 | 0.842 | Group | 2.12 | 0.150 |
| Time | 0.71 | 0.402 | ||||||
| Cont. | 192.76 ± 34.90 | 188.03 ± 30.46 | −4.73 ± 28.70 | 0.316 | Group * Time | 0.89 | 0.348 | |
| Health promotion behavior | Exp. | 109.13 ± 25.94 | 111.35 ± 15.56 | −2.23 ± 3.08 | 0.475 | Group | 6.01 | 0.017 |
| Time | 1.50 | 0.225 | ||||||
| Cont. | 97.26 ± 22.85 | 98.82 ± 20.41 | −1.55 ± 1.22 | 0.210 | Group * Time | 0.05 | 0.828 | |
| Health responsibility | Exp. | 16.39 ± 6.99 | 16.10 ± 4.69 | 0.29 ± 5.79 | 0.782 | Group | 1.89 | 0.173 |
| Time | 0.01 | 0.919 | ||||||
| Cont. | 14.55 ± 5.57 | 14.74 ± 4.67 | −0.18 ± 2.54 | 0.657 | Group * Time | 0.21 | 0.651 | |
| Physical activity | Exp. | 15.06 ± 6.18 | 17.13 ± 5.92 | −2.07 ± 6.99 | 0.111 | Group | 3.54 | 0.064 |
| Time | 3.46 | 0.067 | ||||||
| Cont. | 13.95 ± 4.71 | 14.16 ± 3.84 | −0.21 ± 5.27 | 0.617 | Group * Time | 2.29 | 0.134 | |
| Nutrition | Exp. | 19.77 ± 4.42 | 19.16 ± 4.28 | 0.61 ± 3.78 | 0.371 | Group | 12.38 | 0.001 |
| Time | 1.02 | 0.317 | ||||||
| Cont. | 16.42 ± 3.43 | 16.34 ± 3.54 | 0.08 ± 1.76 | 0.784 | Group * Time | 0.606 | 0.439 | |
| Spiritual growth | Exp. | 20.55 ± 5.22 | 21.16 ± 5.77 | −0.61 ± 4.75 | 0.478 | Group | 4.19 | 0.045 |
| Time | 0.05 | 0.823 | ||||||
| Cont. | 18.58 ± 4.35 | 18.18 ± 5.41 | 0.39 ± 3.30 | 0.466 | Group * Time | 1.08 | 0.304 | |
| Interpersonal relation | Exp. | 20.32 ± 5.22 | 20.74 ± 4.47 | −0.42 ± 2.77 | 0.405 | Group | 4.13 | 0.046 |
| Time | 0.65 | 0.422 | ||||||
| Cont. | 18.42 ± 3.78 | 18.53 ± 4.17 | −0.11 ± 2.62 | 0.806 | Group * Time | 0.23 | 0.630 | |
| Stress management | Exp. | 17.03 ± 5.04 | 17.06 ± 2.42 | −0.03 ± 4.57 | 0.969 | Group | 1.17 | 0.284 |
| Time | 1.14 | 0.290 | ||||||
| Cont. | 15.34 ± 4.18 | 16.87 ± 6.11 | −1.53 ± 7.01 | 0.188 | Group * Time | 1.05 | 0.310 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, W.J.; Kim, J.A.; Ha, J.S. Effects of a Yoga Program in Reducing Cardiovascular Disease Risk Factors in Workers of Small Workplaces: A Pilot Test. Sustainability 2020, 12, 10038. https://doi.org/10.3390/su122310038
Hwang WJ, Kim JA, Ha JS. Effects of a Yoga Program in Reducing Cardiovascular Disease Risk Factors in Workers of Small Workplaces: A Pilot Test. Sustainability. 2020; 12(23):10038. https://doi.org/10.3390/su122310038
Chicago/Turabian StyleHwang, Won Ju, Jin Ah Kim, and Ji Sun Ha. 2020. "Effects of a Yoga Program in Reducing Cardiovascular Disease Risk Factors in Workers of Small Workplaces: A Pilot Test" Sustainability 12, no. 23: 10038. https://doi.org/10.3390/su122310038
APA StyleHwang, W. J., Kim, J. A., & Ha, J. S. (2020). Effects of a Yoga Program in Reducing Cardiovascular Disease Risk Factors in Workers of Small Workplaces: A Pilot Test. Sustainability, 12(23), 10038. https://doi.org/10.3390/su122310038






