The Impact of the COVID-19 Pandemic on Social, Health, and Economy
Abstract
:1. Background
Methodology
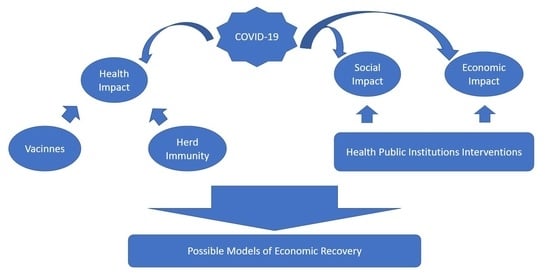
2. Impact of COVID-19 on Health
3. Herd Immunity or Vaccine as a Solution
4. Economic Impact of COVID-19
5. Social Impact of COVID-19
6. Public Health Institutions Interventions
- The adoption of a public health surveillance system for early detection and rapid response. Using an infectious disease model, the prevention of infection involves identifying the individual carrier of the virus to prevent others from getting infected, thus breaking the infection chain. In the case of coronavirus, since there is no treatment or vaccine available yet, the previous premise is crucial [26]. This strategy requires a strong surveillance capacity to be able to detect early cases and to be able to implement preventive measures. However, in most developing countries, epidemiological and laboratory capacity remain weak and need to be urgently strengthened. In Latin American countries, such as Colombia, there is a general shortage of trained human resources who can track the infection, and most of them depend on unstable job contracts or they are owed weeks and even months of wages [105]. This situation needs to change urgently, and the role of public health workers must be recognized [103].
- Risk communication and community participation. The role of the media is essential to ensure that public health measures are implemented effectively, and that people follow the advice provided by the government. This includes regular communication to the public of credible and evidence-based information through daily press conferences about the latest situation updates, associated risks, and actions taken. Risk communication is a key aspect for shaping the course of an pandemic and empowering people to make the right decisions. To encourage protective behavior, individuals need information that is appropriate, accurate, and easy to understand. This can help to limit the spread of misinformation causing panic or hysteria. It is essential to have a comprehensive risk communication strategy that is ethical and useful in the local context [106]. This strategy should be developed in collaboration with social scientists and experts in risk communication. The psychological impact of the pandemic has also been studied [107]. An effective strategy must also address this problem. Both local and national rulers should be responsible and be aware that their opinions outside scientific knowledge can lead to misinformation for the citizens [107,108].
- Protecting vulnerable groups in society. There is currently evidence that the disease affects all age groups but is disproportionately severe among older people and those with underlying conditions, such as hypertension, cardiovascular diseases, and diabetes. Therefore, there is a clear message that the elderly and people with underlying comorbidities must be protected in society and the family environment, so they are not exposed. Geriatric centers must be actively tracked for both the elderly and workers, and medical treatment must be guaranteed if needed.
- Implementation of incentives for research, technological innovation, and development of appropriate health technologies for COVID-19 (medical equipment, respirators, reagents, protective equipment, etc.), promoting cooperation between countries.
- Search information for the diagnosis, surveillance, and prevention of COVID-19. Identifying those that are based on scientific evidence, which can support and feed the processes of policymaking and decision making, and dismissing false information for the general population.
- Mobilization of public health institutions networks for the organization of shared research, human resources training, and technical assistance-cooperation appropriate for the situation.
- Professionalization of health professionals and epidemiologists under direct contracting schemes with official public health entities and not through outsourcing with hospitals and contact tracing centers.
- Strengthen laboratory testing capacity, biosafety protection awareness, and technical training, and carry out health education and publicity, as well as communication of risks to citizens [109].
7. Economic-Financial and Labor Outlook after COVID-19
- Adoption of a public health surveillance system for early detection and rapid response.
- Risk communication and community participation.
- Protecting the vulnerable in society.
- Strengthening of scientific and medical institutions
8. What Can History Teach Us?
9. Possible Models of Economic Recovery
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Worldometers. COVID-19 Coronavirus Pandemic. 2021. Available online: https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1?%20 (accessed on 18 May 2021).
- Feng, S.; Shen, C.; Xia, N.; Song, W.; Fan, M.; Cowling, B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020, 8, 434–436. [Google Scholar] [CrossRef]
- Marini, J.J.; Gattinoni, L. Management of COVID-19 respiratory distress. JAMA 2020, 323, 2329–2330. [Google Scholar] [CrossRef] [PubMed]
- Polak, S.B.; Van Gool, I.C.; Cohen, D.; von der Thüsen, J.H.; van Paassen, J. A systematic review of pathological findings in COVID-19: A pathophysiological timeline and possible mechanisms of disease progression. Mod. Pathol. 2020, 33, 2128–2138. [Google Scholar] [CrossRef]
- Información Científico-Técnica, Enfermedad por Coronavirus, COVID-19. Gob.es. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/ITCoronavirus/home.htm (accessed on 11 January 2021).
- McGonagle, D.; Sharif, K.; O’Regan, A.; Bridgewood, C. Interleukin-6 use in COVID-19 pneumonia related macrophage activation syndrome. Autoimmun. Rev. 2020, 19, 102537. [Google Scholar] [CrossRef]
- Lechowicz, K.; Drożdżal, S.; Machaj, F.; Rosik, J.; Szostak, B.; Zegan-Barańska, M.; Biernawska, J.; Dabrowski, W.; Rotter, I.; Kotfis, K. COVID-19: The Potential Treatment of Pulmonary Fibrosis Associated with SARS-CoV-2 Infection. J. Clin. Med. 2020, 9, 1917. [Google Scholar] [CrossRef]
- Who.int. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_4#:~:text=For%20COVID%2D19%2C,infections%2C%20requiring%20ventilation (accessed on 11 January 2021).
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020, 87, 49–50. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; Hans, S.; Barillari, M.R.; Jouffe, L.; Saussez, S. Loss of smell and taste in 2013 European patients with mild to moderate COVID-19. Ann. Intern. Med. 2020, 173, 672–675. [Google Scholar] [CrossRef]
- Tan, L.; Wang, Q.; Zhang, D.; Ding, J.; Huang, Q.; Tang, Y.-Q.; Wang, Q.; Miao, H. Correction: Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduct. Target. Ther. 2020, 5, 61. [Google Scholar] [CrossRef]
- Tan, W.; Aboulhosn, J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int. J. Cardiol. 2020, 309, 70–77. [Google Scholar] [CrossRef]
- Wise, J. Covid-19 and thrombosis: What do we know about the risks and treatment? BMJ 2020, 369, m2058. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the Coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese center for disease control and prevention: Summary of a report of 72,314 cases from the Chinese center for disease control and prevention. JAMA 2020, 323, 1239–1242. [Google Scholar]
- Dietz, W.; Santos-Burgoa, C. Obesity and its Implications for COVID-19 Mortality. Obesity 2020, 28, 1005. [Google Scholar] [CrossRef] [Green Version]
- Fang, L.; Karakiulakis, G.; Roth, M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020, 8, e21. [Google Scholar] [CrossRef]
- COVID-19 (Coronavirus): Long-Term Effects. Mayoclinic.org. 2020. Available online: https://www.mayoclinic.org/coronavirus-long-term-effects/art-20490351 (accessed on 11 January 2021).
- Zheng, Y.-Y.; Ma, Y.-T.; Zhang, J.-Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [Green Version]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Mao, L.; Wang, M.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; Li, Y.; Jin, H.; et al. Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: A retrospective case series study. bioRxiv 2020. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Dalamitros, A.A.; Beltran-Velasco, A.I.; Mielgo-Ayuso, J.; Tornero-Aguilera, J.F. Social and psychophysiological consequences of the COVID-19 pandemic: An extensive literature review. Front. Psychol. 2020, 11, 580225. [Google Scholar] [CrossRef]
- Thakur, V.; Jain, A. COVID 2019-suicides: A global psychological pandemic. Brain Behav. Immun. 2020, 88, 952–953. [Google Scholar] [CrossRef]
- Randolph, H.E.; Barreiro, L.B. Herd immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Hormeño-Holgado, A.; Jiménez, M.; Benitez-Agudelo, J.C.; Navarro-Jiménez, E.; Perez-Palencia, N.; Maestre-Serrano, R.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. Dynamics of population immunity due to the herd effect in the COVID-19 pandemic. Vaccines 2020, 8, 236. [Google Scholar] [CrossRef] [PubMed]
- Fine, P.; Eames, K.; Heymann, D.L. “Herd immunity”: A rough guide. Clin. Infect. Dis. 2011, 52, 911–916. [Google Scholar] [CrossRef] [PubMed]
- Read, J.M.; Bridgen, J.R.E.; Cummings, D.A.T.; Ho, A.; Jewell, C.P. Novel coronavirus 2019-nCoV: Early estimation of epidemiological parameters and epidemic predictions. bioRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Karin, O.; Bar-On, Y.M.; Milo, T.; Katzir, I.; Mayo, A.; Korem, Y. Adaptive cyclic exit strategies from lockdown to suppress COVID-19 and allow economic activity. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Walker, P.G.; Whittaker, C.; Watson, O.; Baguelin, M.; Ainslie, K.E.C.; Bhatia, S. The Global Impact of Covid-19 and Strategies for Mitigation and Suppression; Imperial College of London: London, UK, 2020. [Google Scholar]
- Kwok, K.O.; Lai, F.; Wei, W.I.; Wong, S.Y.S.; Tang, J.W. Herd immunity–estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. 2020, 80, 32–33. [Google Scholar] [CrossRef]
- Leung, K.; Wu, J.T.; Liu, D.; Leung, G.M. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: A modelling impact assessment. Lancet 2020, 395, 1382–1393. [Google Scholar] [CrossRef]
- Lee, D.; Heo, K.; Seo, Y. COVID-19 in South Korea: Lessons for developing countries. World Dev. 2020, 135, 105057. [Google Scholar] [CrossRef]
- BBC News. Wuhan Coronavirus: From Silent Streets to Packed Pools. BBC. 18 August 2020. Available online: https://www.bbc.com/news/world-asia-china-53816511 (accessed on 11 January 2021).
- Pfizer and BioNTech Announce Vaccine Candidate against COVID-19 Achieved Success in first Interim Analysis from Phase 3 Study. Pfizer.com. Available online: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-vaccine-candidate-against (accessed on 11 January 2021).
- Fair Allocation Mechanism for COVID-19 Vaccines through the COVAX Facility. Who.int. Available online: https://www.who.int/publications/m/item/fair-allocation-mechanism-for-covid-19-vaccines-through-the-covax-facility (accessed on 11 January 2021).
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- COVAX Facility. Gavi.org. Available online: https://www.gavi.org/covax-facilityfacility (accessed on 11 January 2021).
- Urreiztieta, E.; Polo, S. El Gobierno Compro los Test Chinos Falsos Para el Coronavirus por mas del Doble de su valor. El Mundo. 2020. Available online: https://www.elmundo.es/espana/2020/04/22/5ea08fad21efa03d058b4675.htmlfacility (accessed on 11 January 2021).
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Corey, L.; Mascola, J.R.; Fauci, A.S.; Collins, F.S. A strategic approach to COVID-19 vaccine R&D. Science 2020, 368, 948–950. [Google Scholar]
- Dean, N.E.; Gsell, P.-S.; Brookmeyer, R.; De Gruttola, V.; Donnelly, C.A.; Halloran, M.E.; Jasseh, M.; Nason, M.; Riveros, X.; Watson, C.H.; et al. Design of vaccine efficacy trials during public health emergencies. Sci. Transl. Med. 2019, 11, eaat0360. [Google Scholar] [CrossRef]
- Bowen, R.A.R. Ethical and organizational considerations for mandatory COVID-19 vaccination of health care workers: A clinical laboratorian’s perspective. Clin. Chim. Acta 2020, 510, 421–422. [Google Scholar] [CrossRef]
- Katz, R.D. Friendly fire: The mandatory military anthrax vaccination program. Duke Law J. 2001, 50, 1835–1863. [Google Scholar] [CrossRef] [Green Version]
- Kose, A.; Sugawara, N. Understanding the Depth of the 2020 Global Recession in 5 Charts. World Bank Data Blog 2020. Available online: https://blogs.worldbank.org/opendata/understanding-depth-2020-global-recession-5-charts (accessed on 15 May 2021).
- Lal, P.; Kumar, A.; Kumar, S.; Kumari, S.; Saikia, P.; Dayanandan, A.; Adhikari, D.; Khan, M.L. The dark cloud with a silver lining: Assessing the impact of the SARS COVID-19 pandemic on the global environment. Sci. Total Environ. 2020, 732, 139297. [Google Scholar] [CrossRef]
- Undp.org. Available online: http://hdr.undp.org/sites/default/files/covid-19_and_human_development_0.pdffacility (accessed on 11 January 2021).
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Tisdell, C.A. Economic, social and political issues raised by the COVID-19 pandemic. Econ. Anal. Policy 2020, 68, 17–28. [Google Scholar] [CrossRef]
- Fakhruddin, B.; Blanchard, K.; Ragupathy, D. Are we there yet? The transition from response to recovery for the COVID-19 pandemic. Prog. Disaster Sci. 2020, 7, 100102. [Google Scholar] [CrossRef]
- International Monetary Fund. World Economic Outlook Update, January 2021; Washington, DC, USA. 2021. Available online: https://www.imf.org/en/Publications/WEO/Issues/2021/01/26/2021-world-economic-outlook-update (accessed on 15 May 2021).
- World Economic Outlook. Imf.org. 2020. Available online: https://www.imf.org/en/Publications/WEO/Issues/2020/09/30/world-economic-outlook-october-2020facility (accessed on 11 January 2021).
- Zhang, D.; Hu, M.; Ji, Q. Financial markets under the global pandemic of COVID-19. Financ. Res. Lett. 2020, 36, 101528. [Google Scholar] [CrossRef]
- COVID-19 Leads to Massive Labour Income Losses Worldwide. 2020. Available online: https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_755875/lang--en/index.htm (accessed on 11 January 2021).
- Dam-broadcast.com. Available online: https://oecd.dam-broadcast.com/pm_7379_119_119686-962r78x4do.pdf (accessed on 11 January 2021).
- Donthu, N.; Gustafsson, A. Effects of COVID-19 on business and research. J. Bus. Res. 2020, 117, 284–289. [Google Scholar] [CrossRef]
- Lakner, C.; Mahler, D.G.; Negre, M.; Prydz, E.B. How Much Does Reducing Inequality Matter for Global Poverty? World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Sigala, M. Tourism and COVID-19: Impacts and implications for advancing and resetting industry and research. J. Bus. Res. 2020, 117, 312–321. [Google Scholar] [CrossRef]
- Why the World must Urgently Strengthen Learning and Protect Finance for Education. Unesco.org. 2020. Available online: https://en.unesco.org/news/why-world-must-urgently-strengthen-learning-and-protect-finance-education (accessed on 11 January 2021).
- Kanda, W.; Kivimaa, P. What opportunities could the COVID-19 outbreak offer for sustainability transitions research on electricity and mobility? Energy Res. Soc. Sci. 2020, 68, 101666. [Google Scholar] [CrossRef] [PubMed]
- Unwomen.org. Available online: https://data.unwomen.org/sites/default/files/documents/Publications/Spotlight-Gender-COVID-19-SDGs.pdf (accessed on 11 January 2021).
- Nightingale, E.; Brady, O.J.; Yakob, L.; CMMID Covid-19 Working Group. The importance of saturating density dependence for predicting SARS-CoV-2 resurgence. bioRxiv 2020. [Google Scholar] [CrossRef]
- Kraemer, M.U.G.; Yang, C.-H.; Gutierrez, B.; Wu, C.-H.; Klein, B.; Pigott, D.M.; Du Plessis, L.; Faria, N.R.; Li, R.; Hanage, W.P.; et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaiser, J.C.; Stathopoulos, G.T. Socioeconomic correlates of SARS-CoV-2 and influenza H1N1 outbreaks. Eur. Respir. J. 2020, 56, 2001400. [Google Scholar] [CrossRef] [PubMed]
- Cutler, D.M.; Summers, L.H. The COVID-19 pandemic and the $16 trillion virus. JAMA 2020, 324, 1495–1496. [Google Scholar] [CrossRef]
- Rhodes, T.; Lancaster, K.; Lees, S.; Parker, M. Modelling the pandemic: Attuning models to their contexts. BMJ Glob. Health 2020, 5, e002914. [Google Scholar] [CrossRef]
- Dingwall, R.; Hoffman, L.M.; Staniland, K. Introduction: Why a sociology of pandemics? Why aSociologyof pandemics? Sociol. Health Illn. 2013, 35, 167–173. [Google Scholar] [CrossRef]
- Chou, R.; Dana, T.; Jungbauer, R.; Weeks, C.; McDonagh, M.S. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings: A living rapid review: A living rapid review. Ann. Intern. Med. 2020, 173, 542–555. [Google Scholar] [CrossRef]
- Wang, X.; Ferro, E.G.; Zhou, G.; Hashimoto, D.; Bhatt, D.L. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers. JAMA 2020, 324, 703. [Google Scholar] [CrossRef]
- Baggett, T.P.; Keyes, H.; Sporn, N.; Gaeta, J.M. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA 2020, 323, 2191–2192. [Google Scholar] [CrossRef]
- Böhmer, M.M.; Buchholz, U.; Corman, V.M.; Hoch, M.; Katz, K.; Marosevic, D.V.; Böhm, S.; Woudenberg, T.; Ackermann, N.; Konrad, R.; et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: A case series. Lancet Infect. Dis. 2020, 20, 920–928. [Google Scholar] [CrossRef]
- Nishiura, H.; Oshitani, H.; Kobayashi, T.; Saito, T.; Sunagawa, T.; Matsui, T.; Wakita, T. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19). bioRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Kakimoto, K.; Kamiya, H.; Yamagishi, T.; Matsui, T.; Suzuki, M.; Wakita, T. Initial Investigation of Transmission of COVID-19 among Crew Members during Quarantine of a Cruise Ship, Yokohama, Japan, February 2020; CDC: Atlanta, GA, USA, 2020.
- Bolaño-Ortiz, T.R.; Camargo-Caicedo, Y.; Puliafito, S.E.; Ruggeri, M.F.; Bolaño-Diaz, S.; Pascual-Flores, R.; Saturno, J.; Ibarra-Espinosa, S.; Mayol-Bracero, O.L.; Torres-Delgado, E.; et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: A look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020, 191, 109938. [Google Scholar] [CrossRef]
- REACT Study Investigators; Riley, S.; Ainslie, K.E.C.; Eales, O.; Jeffrey, B.; Walters, C.E.; Atchison, C.J.; Diggle, P.J.; Ashby, D.; Donnelly, C.A.; et al. Community prevalence of SARS-CoV-2 virus in England during May 2020: REACT study. bioRxiv 2020. [Google Scholar] [CrossRef]
- Gagneux-Brunon, A.; Pelissier, C.; Gagnaire, J.; Pillet, S.; Pozzetto, B.; Botelho-Nevers, E.; Berthelot, P. SARS-CoV-2 infection: Advocacy for training and social distancing in healthcare settings. J. Hosp. Infect. 2020, 106, 610–612. [Google Scholar] [CrossRef] [PubMed]
- Ladhani, S.N.; Chow, J.Y.; Janarthanan, R.; Fok, J.; Crawley-Boevey, E.; Vusirikala, A.; Fernandez, E.; Perez, M.S.; Tang, S.; Dun-Campbell, K.; et al. Increased risk of SARS-CoV-2 infection in staff working across different care homes: Enhanced CoVID-19 outbreak investigations in London care Homes. J. Infect. 2020, 81, 621–624. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Steinman, L.E.; Casey, E.A. Combatting social isolation among older adults in a time of physical distancing: The COVID-19 social Connectivity Paradox. Front. Public Health 2020, 8, 403. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Bu, F.; Mak, H.W.; Steptoe, A. COVID-19 Social Study: Results Release; John Wiley & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Timmermann, R.; Von Graevenitz, A.; Kimmig, P.; Schiefer, H.G.; Schwarz, T.; Slenczka, W. Zoonoses: Infectious Diseases Transmissible from Animals to Humans; Zahner, H., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Horta, B.L.; Silveira, M.F.; Barros, A.J.D.; Barros, F.C.; Hartwig, F.P.; Dias, M.S.; Menezes, A.M.; Hallal, P.C.; Victora, C.G. Prevalence of antibodies against SARS-CoV-2 according to socioeconomic and ethnic status in a nationwide Brazilian survey. Rev. Panam. Salud Publica 2020, 44, e135. [Google Scholar] [CrossRef]
- Niedzwiedz, C.L.; O’Donnell, C.A.; Jani, B.D.; Demou, E.; Ho, F.K.; Celis-Morales, C.; Nicholl, B.I.; Mair, F.S.; Welsh, P.; Sattar, N.; et al. Ethnic and socioeconomic differences in SARS-CoV-2 infection: Prospective cohort study using UK Biobank. BMC Med. 2020, 18, 160. [Google Scholar] [CrossRef]
- Martin, A.; Markhvida, M.; Hallegatte, S.; Walsh, B. Socio-economic impacts of COVID-19 on household consumption and poverty. Econ. Disaster Clim. Chang. 2020, 4, 1–27. [Google Scholar]
- Patel, J.A.; Nielsen, F.B.H.; Badiani, A.A.; Assi, S.; Unadkat, V.A.; Patel, B.; Ravindrane, R.; Wardle, H. Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health 2020, 183, 110–111. [Google Scholar] [CrossRef]
- Eyre, D.W.; Lumley, S.F.; O’Donnell, D.; Campbell, M.; Sims, E.; Lawson, E.; Warren, F.; James, T.; Cox, S.; Howarth, A.; et al. Differential occupational risks to healthcare workers from SARS-CoV-2 observed during a prospective observational study. Elife 2020, 9. [Google Scholar] [CrossRef]
- Tso, R.V.; Cowling, B.J. Importance of face masks for COVID-19: A call for effective public education. Clin. Infect. Dis. 2020, 71, 2195–2198. [Google Scholar] [CrossRef]
- Batty, G.D.; Deary, I.J.; Luciano, M.; Altschul, D.M.; Kivimäki, M.; Gale, C.R. Psychosocial factors and hospitalisations for COVID-19: Prospective cohort study based on a community sample. Brain Behav. Immun. 2020, 89, 569–578. [Google Scholar] [CrossRef]
- Cromer, S.J.; Lakhani, C.M.; Wexler, D.J.; Burnett-Bowie, S.-A.M.; Udler, M.; Patel, C.J. Geospatial analysis of individual and community-level socioeconomic factors impacting SARS-CoV-2 prevalence and outcomes. medRxiv 2020. [Google Scholar] [CrossRef]
- Goyal, M.K.; Simpson, J.N.; Boyle, M.D.; Badolato, G.M.; Delaney, M.; McCarter, R.; Cora-Bramble, D. Racial and/or ethnic and socioeconomic disparities of SARS-CoV-2 infection among children. Pediatrics 2020, 146, e2020009951. [Google Scholar] [CrossRef]
- Wachtler, B.; Michalski, N.; Nowossadeck, E.; Diercke, M.; Wahrendorf, M.; Santos-Hövener, C.; Lampert, T.; Hoebel, J. Socioeconomic inequalities in the risk of SARS-CoV-2 infection–First results from an analysis of surveillance data from Germany. J. Health Monit. 2020. [Google Scholar] [CrossRef]
- Calderón, C.A.; de la Vega, G.; Herrero, D.B. Topic modeling and characterization of hate speech against immigrants on Twitter around the emergence of a far-right party in Spain. Soc. Sci. 2020, 9, 188. [Google Scholar] [CrossRef]
- Uyheng, J.; Carley, K.M. Bots and online hate during the COVID-19 pandemic: Case studies in the United States and the Philippines. J. Comput. Soc. Sci. 2020, 3, 1–24. [Google Scholar] [CrossRef]
- Laing, T. The economic impact of the Coronavirus 2019 (Covid-2019): Implications for the mining industry. Extr. Ind. Soc. 2020, 7, 580–582. [Google Scholar]
- Palermo, T.; Peterman, A. Undercounting, overcounting and the longevity of flawed estimates: Statistics on sexual violence in conflict. Bull. World Health Organ. 2011, 89, 924–925. [Google Scholar]
- Mittal, S.; Singh, T. Gender-based violence during COVID-19 pandemic: A mini-review. Front. Glob. Women’s Health 2020, 1. [Google Scholar] [CrossRef]
- Bhalotra, S.; Kambhampati, U.; Rawlings, S.; Siddique, Z. Intimate partner violence: The influence of job opportunities for men and women. World Bank Econ. Rev. 2019. [Google Scholar] [CrossRef] [Green Version]
- Lawson, M.; Piel, M.H.; Simon, M. Child maltreatment during the COVID-19 pandemic: Consequences of parental job loss on psychological and physical abuse towards children. Child Abus. Negl. 2020, 110 Pt 2, 104709. [Google Scholar] [CrossRef]
- Sidpra, J.; Abomeli, D.; Hameed, B.; Baker, J.; Mankad, K. Rise in the incidence of abusive head trauma during the COVID-19 pandemic. Arch. Dis. Child. 2020, 106, e14. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Bryant, D.J.; Oo, M.; Damian, A.J. The rise of adverse childhood experiences during the COVID-19 pandemic. Psychol. Trauma 2020, 12, S193–S194. [Google Scholar] [CrossRef]
- Comas-Herrera, A.; Fernandez, J.-L.; Hancock, R.; Hatton, C.; Knapp, M.; McDaid, D.; Malley, J.; Wistow, G.; Wittenberg, R. COVID-19: Implications for the support of people with social care needs in England. J. Aging Soc. Policy 2020, 32, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Abdulaal, A.; Ariyanayagam, D.; Killington, K.; Denny, S.J.; Mughal, N.; Hughes, S.; Goel, N.; Davies, G.W.; Moore, L.S.; et al. Investigating the association between ethnicity and health outcomes in SARS-CoV-2 in a London secondary care population. PLoS ONE 2020, 15, e0240960. [Google Scholar] [CrossRef] [PubMed]
- Narain, J.P.; Dawa, N.; Bhatia, R. Health system response to COVID-19 and future pandemics. J. Health Manag. 2020, 22, 138–145. [Google Scholar] [CrossRef]
- Transforming Our World: The 2030 Agenda for Sustainable Development. Sustainable Development Knowledge Platform. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld (accessed on 11 January 2021).
- Guerrero, J.; Pulido, G. Trabajo, salud y régimen contractual en personal de enfermería: Un enfoque psicosocial. Av. Enferm. 2010, 28, 111–122. [Google Scholar]
- Bhatia, R. Public engagement is key for containing COVID-19 pandemic. Indian J. Med. Res. 2020, 151, 118–120. [Google Scholar] [CrossRef]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef]
- Idrovo, A.J.; Manrique-Hernández, E.F.; Fernández Niño, J.A. Report from bolsonaro’s Brazil: The consequences of ignoring science. Int. J. Health Serv. 2021, 51, 31–36. [Google Scholar] [CrossRef]
- Deng, S.-Q.; Peng, H.-J. Characteristics of and public health responses to the Coronavirus disease 2019 outbreak in China. J. Clin. Med. 2020, 9, 575. [Google Scholar] [CrossRef] [Green Version]
- Ilo.org. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_emp/---emp_ent/documents/publication/wcms_741870.pdf (accessed on 11 January 2021).
- Fana, M.; Torrejón Pérez, S.; Fernández-Macías, E. Employment impact of Covid-19 crisis: From short term effects to long terms prospects. Econ. Polit. Ind. 2020, 47, 391–410. [Google Scholar] [CrossRef]
- Monitor ILO. COVID-19 and the World of Work. Updated Estimates and Analysis. 2020. Available online: https://www.ilo.org/wcmsp5/groups/public/@dgreports/@dcomm/documents/briefingnote/wcms_767028.pdf (accessed on 15 May 2021).
- Susskind, D.; Vines, D. The economics of the COVID-19 pandemic: An assessment. Oxf. Rev. Econ. Pol. 2020, 36 (Suppl. 1), S1–S13. [Google Scholar] [CrossRef]
- Fernandes, N. Economic effects of Coronavirus outbreak (COVID-19) on the world economy. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Betcherman, G.; Giannakopoulos, N.; Laliotis, I.; Pantelaiou, I.; Testaverde, M.; Tzimas, G. Reacting Quickly and Protecting Jobs: The Short-Term Impacts of the COVID-19 Lockdown on the Greek Labor Market. Policy Research Working Paper; No. 9356. World Bank: Washington, DC. © World Bank. 2020. Available online: https://openknowledge.worldbank.org/handle/10986/34353License:CCBY3.0IGO (accessed on 15 May 2021).
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109, 102433. [Google Scholar] [CrossRef]
- Global Economy. Credit-Suisse.com. Available online: https://www.credit-suisse.com/microsites/investment-outlook/en/global-economy.html (accessed on 11 January 2021).
- Hensher, M. Covid-19, Unemployment, and Health: Time for Deeper Solutions? BMJ 2020, 371. [Google Scholar] [CrossRef]
- La Enfermedad por D. en América Latina y el Caribe. Cepal.org. Available online: https://repositorio.cepal.org/bitstream/handle/11362/45602/1/S2000313_es.pdf (accessed on 11 January 2021).
- Europa.eu. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:52020DC0143&from=ES (accessed on 11 January 2021).
- Jobs and Economy during the Coronavirus Pandemic. Europa.eu. 2020. Available online: https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/jobs-and-economy-during-coronavirus-pandemic_en (accessed on 11 January 2021).
- Snowden, F.M. Epidemics and Society: From the Black Death to the Present; Yale University Press: New Haven, CT, USA, 2019. [Google Scholar]
- Manzoni, A. I Promessi Sposi; Newton Compton Editori: Rome, Italy, 2010; Volume 29. [Google Scholar]
- Ibrahim, S. The Pandemic Century: A History of Global Contagion from the Spanish Flu to COVID-19. Malays. Orthop. J. 2020, 14, 209. [Google Scholar]
- Cdc.gov. Available online: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2017-vol-29.pdf (accessed on 11 January 2021).
- Waltner-Toews, D. On Pandemics: Deadly Diseases from Bubonic Plague to Coronavirus; Greystone Books: Vancouver, BC, Canada, 2020. [Google Scholar]
- McMillen, C.W. Pandemics: A Very Short Introduction; Oxford University Press: New York, NY, USA, 2016. [Google Scholar]
- Cavallino, P.; De Fiore, F. Central Banks’ Response to Covid-19 in Advanced Economies; Bank for International Settlements. 2020. Available online: https://www.bis.org/publ/bisbull21.htm (accessed on 15 May 2021).
- Europa.eu. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=OJ:L:2020:091:FULL&from=EN (accessed on 11 January 2021).
- Gruszczynski, L. The COVID-19 pandemic and international trade: Temporary turbulence or paradigm shift? Eur. J. Risk Regul. 2020, 11, 337–342. [Google Scholar] [CrossRef] [Green Version]
- Altig, D.; Baker, S.; Barrero, J.M.; Bloom, N.; Bunn, P.; Chen, S.; Davis, S.J.; Leather, J.; Meyer, B.; Mihaylov, E.; et al. Economic uncertainty before and during the COVID-19 pandemic. J. Public Econ. 2020, 191, 104274. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Gustafsson, A. Investigating the emerging COVID-19 research trends in the field of business and management: A bibliometric analysis approach. J. Bus. Res. 2020, 118, 253–261. [Google Scholar] [CrossRef]
- Djalante, R.; Nurhidayah, L.; Van Minh, H.; Phuong, N.T.N.; Mahendradhata, Y.; Trias, A.; Lassa, J.; Miller, M.A. COVID-19 and ASEAN responses: Comparative policy analysis. Prog. Disaster Sci. 2020, 8, 100129. [Google Scholar] [CrossRef]
- Korhonen, J.; Honkasalo, A.; Seppälä, J. Circular Economy: The Concept and its Limitations. Ecol. Econ. 2018, 143, 37–46. [Google Scholar] [CrossRef]
- Lahcen, B.; Brusselaers, J.; Vrancken, K.; Dams, Y.; Da Silva Paes, C.; Eyckmans, J.; Rousseau, S. Green recovery policies for the COVID-19 crisis: Modelling the impact on the economy and greenhouse gas emissions. Environ. Resour. Econ. 2020, 76, 1–20. [Google Scholar] [CrossRef]
- Fiscal Monitor. Imf.org. 2020. Available online: https://www.imf.org/en/Publications/FM/Issues/2020/09/30/october-2020-fiscal-monitor (accessed on 11 January 2021).
- International Monetary Fund (2020). World Economic Outlook: A Long and Difficult Ascent; International Monetary Fund: Washington, DC, USA, 2020; Available online: https://www.imf.org/en/Publications/WEO/Issues/2020/09/30/world-economic-outlook-october2020#Chapter%202:%20The%20Great%20Lockdown,%20Dissecting%20The%20Economic%20Effects (accessed on 15 May 2021).
- European Central Bank. Decision (EU) 2020/440 of the European Central Bank of 24 March 2020 on a temporary pandemic emergency purchase programme (ECB/2020/17). Off. J. Eur. Union 2020, L91/1, 1–4. [Google Scholar]
- European Commission. Europe’s Moment: Repair and Prepare for the Next Generation, Communication From The Commission To The European Parliament, The European Council, The Council, The European Economic And Social Committee and The Committee Of The Regions. COM (2020) 456 Final. 2020. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52020DC0456&from=EN (accessed on 15 May 2021).
- Online Platform on Sustainable and Resilient Recovery from COVID-19. Policies, Measures and Actions on Climate Change and Environmental Protection in the Context of COVID-19 Recovery. Online Ministerial Meeting, Chaired by the Japanese Minister of the Environment, Koizumi Shinjiro, 3 September 2020. Available online: https://platform2020redesign.org/ (accessed on 15 May 2021).
- European Council. Special Meeting of the European Council (17, 18, 19, 20, 21 July 2020): Conclusions. 2020. Available online: https://data.consilium.europa.eu/doc/document/ST-10-2020-INIT/en/pdf (accessed on 15 May 2021).
- European Commission. The European Green Deal. Communication From The Commission To The European Parliament, The Council, The European Economic And Social Committee and The Committee Of The Regions. COM (2019) 640 Final. 2019. Available online: https://eur-lex.europa.eu/resource.html?uri=cellar:b828d165-1c22-11ea-8c1f-01aa75ed71a1.0002.02/DOC_1&format=PDF (accessed on 15 May 2021).
- Rodriguez-Besteiro, S.; Tornero-Aguilera, J.F.; Fernández-Lucas, J.; Clemente-Suárez, V.J. Gender Differences in the COVID-19 Pandemic Risk Perception, Psychology, and Behaviors of Spanish University Students. Int. J. Environ. Res. Public Health 2021, 18, 3908. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Navarro-Jiménez, E.; Jimenez, M.; Hormeño-Holgado, A.; Martinez-Gonzalez, M.B.; Benitez-Agudelo, J.C.; Perez-Palencia, N.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. Impact of COVID-19 Pandemic in Public Mental Health: An Extensive Narrative Review. Sustainability 2021, 13, 3221. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Navarro-Jiménez, E.; Ruisoto, P.; Dalamitros, A.A.; Beltran-Velasco, A.I.; Hormeño-Holgado, A.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. Performance of Fuzzy Multi-Criteria Decision Analysis of Emergency System in COVID-19 Pandemic. An Extensive Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 5208. [Google Scholar] [CrossRef]


| Country | Renegotiation of External Debt | Take International Loans with Multilateral Banks | Take Loans to Face Health Situation | Postponement of Social Security Payment by Employers | Financing Essential Sectors of the Economy | Working Capital Loans to SMEs | Refinancing of Mortgage and Consumer Debts to Individuals for Variable Terms | Tax Relief for the Hotel Sector | Approval of Disbursement to Banks by the Central Bank to Finance Personal and Business Loans | Temporary Unemployment Benefit |
|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | x | x | x | X | x | x | x | |||
| Colombia | x | x | x The social security system guarantees the payment of a work disability to the worker infected by COVID-19 and empowers the general population to telework | X | x | x | x | x | ||
| Costa Rica | x | x | x | x | x | |||||
| Dominican Republic | x | x | x | x | x | |||||
| Ecuador | x | x | x | x | x | |||||
| El Salvador | x Refinancing payments for up to 2 years in public services. | |||||||||
| Guatemala | x | x | x | x | ||||||
| Honduras | x | x | x | x | x | x | x | |||
| México | x | x at 0% interest | x | x | ||||||
| Panamá | x | x. | ||||||||
| Perú | x | x | x | x | ||||||
| Uruguay | x | x | x | x |
| Country | Confinement Measures | Reducing Worker Exposure to COVID-19 in the Workplace | Financial Aid to Sick Workers and Their Families | Income Support for Quarantined Workers Unable to Work from Home | Income Assistance for People Who Lose Their Jobs or Self-Employment Income | Helps Companies Adjust Working Time to Retain Jobs | Financial Support to Companies Affected by the Drop in Consumer Demand | Changes in the Regulation of Dismissals | Helps Economically Insecure Workers Stay Home |
|---|---|---|---|---|---|---|---|---|---|
| Austria | x | x | x | x | x | x | x | x | |
| Belgium | x | x | x | x | x | x | x | x | |
| Czech Republic | x | x | x | x | x | x | x | x | |
| Denmark | x | x | x | x | x | x | x | x | |
| Estonia | x | x | x | x | x | x | x | x | |
| Finland | x | x | x | x | x | x | x | x | |
| France | x | x | x | x | x | x | x | x | |
| Germany | x | x | x | x | x | x | x | x | |
| Greece | x | x | x | x | x | x | x | ||
| Hungary | x | x | x | x | x | x | x | ||
| Iceland | x | x | x | x | x | x | x | ||
| Ireland | x | x | x | x | x | x | x | x | |
| Italy | x | x | x | x | x | x | x | x | x |
| Japan | x | x | x | x | x | x | x | x | |
| South Korea | x | x | x | x | x | x | x | x | |
| Latvia | x | x | x | x | x | x | x | x | |
| Holland | x | x | x | x | x | x | x | ||
| Norway | x | x | x | x | x | x | x | ||
| Poland | x | x | x | x | x | x | x | x | |
| Portugal | x | x | x | x | x | x | x | ||
| Slovakia | x | x | x | x | x | x | x | x | |
| Spain | x | x | x | x | x | x | x | x | x |
| Sweden | x | x | x | x | x | x | x | x | |
| United Kingdom | x | x | x | x | x | x | x | x |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clemente-Suárez, V.J.; Navarro-Jiménez, E.; Moreno-Luna, L.; Saavedra-Serrano, M.C.; Jimenez, M.; Simón, J.A.; Tornero-Aguilera, J.F. The Impact of the COVID-19 Pandemic on Social, Health, and Economy. Sustainability 2021, 13, 6314. https://doi.org/10.3390/su13116314
Clemente-Suárez VJ, Navarro-Jiménez E, Moreno-Luna L, Saavedra-Serrano MC, Jimenez M, Simón JA, Tornero-Aguilera JF. The Impact of the COVID-19 Pandemic on Social, Health, and Economy. Sustainability. 2021; 13(11):6314. https://doi.org/10.3390/su13116314
Chicago/Turabian StyleClemente-Suárez, Vicente Javier, Eduardo Navarro-Jiménez, Libertad Moreno-Luna, María Concepción Saavedra-Serrano, Manuel Jimenez, Juan Antonio Simón, and Jose Francisco Tornero-Aguilera. 2021. "The Impact of the COVID-19 Pandemic on Social, Health, and Economy" Sustainability 13, no. 11: 6314. https://doi.org/10.3390/su13116314
APA StyleClemente-Suárez, V. J., Navarro-Jiménez, E., Moreno-Luna, L., Saavedra-Serrano, M. C., Jimenez, M., Simón, J. A., & Tornero-Aguilera, J. F. (2021). The Impact of the COVID-19 Pandemic on Social, Health, and Economy. Sustainability, 13(11), 6314. https://doi.org/10.3390/su13116314