1. Introduction
Dengue fever (DF) is a major communicable disease and it is a continual public health problem, with mosquitoes carrying the disease. Globally, about 500,000 severe dengue cases with 12,500 deaths are reported annually [
1]. The World Health Organization (WHO) estimates that about 100 million DF infections occur annually and that approximately 2.5 billion people live in countries where dengue is endemic [
1]. Dengue viruses are transmitted mainly by
Aedes aegypti and possibly by
Ae. albopictus in tropical and sub-tropical areas [
2]. Dengue has become endemic in nearly 100 countries in Africa, the Americas, the Eastern Mediterranean, Southeast Asia, and the Western Pacific [
3]. Thailand reported its first experience of dengue fever in 1949 [
4] and the first outbreak of dengue hemorrhagic fever (DHF) was reported in Bangkok in 1958 [
4].
In 2019, the number of dengue fever cases in all regions of Thailand was 131,157 with 197.27 cases per 100,000 population and 142 deaths (mortality rate of 0.21 per 100,000 population). In the southern region, 17,167 cases with 181.20 cases per 100,000 population and 31 deaths (mortality rate of 0.33 per 100,000 population) were reported [
5]. When considered in the southern region, the mortality rate was higher than the total rate for all regions of Thailand. In Pattani province, there were 1264 dengue cases with a morbidity rate of 175.17 per 100,000 population. In Yala province, 1440 dengue cases and a morbidity rate of 269.50 per 100,000 population were reported. There were 2088 dengue cases (morbidity rate of 259.30 per 100,000 population) in Narathiwat province [
5].
The southern region of Thailand is different from its other regions, for this peninsular part consists of seaside and mountainous areas. Thailand is classified as a tropical region with high temperatures and rainy weather all year round. The heaviest rainfalls on the west side of the southern region are caused by the southwest monsoon, from June to October, while the northeast monsoon prevailing during mid-October to mid-February, causes heavy rainfall on the eastern side of the peninsula. The average number of rainy days is 148.7 days per year and the average rainfall is 1781.7 mm per year [
6]. These weather conditions are very favorable to mosquito breeding [
7].
The factors related to the spread of these diseases have been documented by studies completed in Nakhon Si Thammarat and Patthalung provinces of Thailand [
8], as well as in Indonesia [
9] and Taiwan [
10]. Weather parameters have widely been studied as substantial factors that need to be considered for better understanding of dengue transmission worldwide [
8,
9,
11,
12]. In recent decades, weather variables such as temperature, rainfall, and relative humidity have been widely studied for their potential to provide an early warning of dengue transmission [
13] also in Thailand [
11,
14], Malaysia [
3], and Indonesia [
9]. Spatiotemporal modeling is important for predicting the risk of dengue fever in several localities, including Puerto Rico [
15], Venezuela [
12], and Thailand [
11].
In this study, we aim to show maps and analyses that display dengue cases and weather-related factors in the three southernmost provinces of Thailand, namely, Pattani, Yala, and Narathiwat provinces, as well as the effects of weather on dengue transmission using data from 2015–2019 with a predictive model, fit with time series Poisson regression approach. Finally, an early warning system with a weather-based predictive model is an essential tool for providing scientific information for effective dengue prevention and control programs.
2. Materials and Methods
2.1. Study Areas
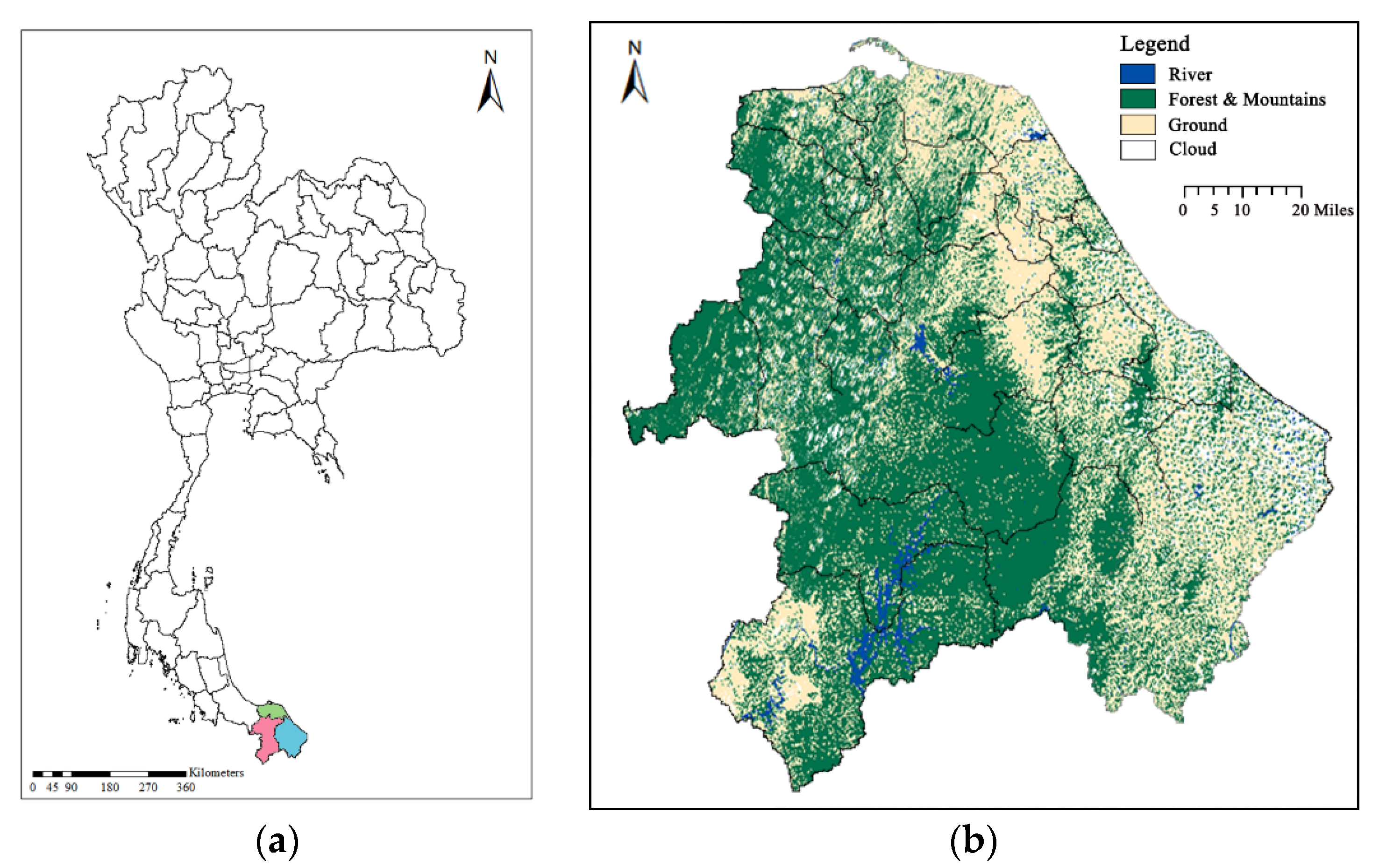
In this study, we selected the three southernmost provinces of Thailand (
Figure 1a,b) for the study areas, consisting of Pattani, Yala, and Narathiwat provinces. Southern Thailand is on the Malay Peninsula with an area of around 70,714 km
2, bounded to the north by Kra Isthmus, the narrowest part of the peninsula. Pattani coastline faces the Gulf of Thailand to the north. The south is dominated by the Sankalakhiri Mountain Range, which includes Budo-Su-ngai Padi National Park, on the border with Yala and Narathiwat. Yala is the southernmost province of Thailand and is one of two landlocked provinces in Southern Thailand. Its southern part borders on Kedah and Perak of Malaysia. Narathiwat is on the Gulf of Thailand. To the south, it borders on the Malaysian states of Kelantan and Perak. The study areas are located near the seaside and mountainous areas, with high temperatures and rainfall throughout the year. The weather is influenced by the northeast monsoon that occurs from mid-October to mid-February. Regarding the topographic characteristics of the central and southern study areas, the region has the Sankalakiri Mountain Range (Yala and Narathiwat) resting in the east–west direction and a border between Thailand and Malaysia. To the east is a river basin stretching to the coast of the Gulf of Thailand in Pattani and Narathiwat provinces.
2.2. Data Collection
The computerized data set on monthly dengue fever cases from January 2015 to December 2019 in the three southernmost provinces of Thailand (i.e., Pattani, Yala, and Narathiwat provinces) were obtained from the Bureau of Epidemiology, Ministry of Public Health. Weather data for the same period were collected from the Meteorological Department of Southern Thailand as regards rainfall, rainy day, mean temperature, minimum temperature, maximum temperature, relative humidity, and air pressure (
Figure 2).
The amount of rainfall, the number of rainy days, relative humidity, and air pressure were collected from 12 weather stations in Pattani, 8 stations in Yala, and 13 stations in Narathiwat, covering all the districts in the studied provinces (1 station/district). Mean temperature, minimum temperature, and maximum temperature were collected from a single weather station in each province. Then, the averages of the amount of rainfall, the number of rainy days, relative humidity, and air pressure in each province were used to represent the weather data for each province. The weather data used in data analysis match the number of data records and dimension of dengue fever data.
The monthly number of dengue cases by province were collected from the Bureau of Epidemiology, Ministry of Public Health, through the dengue cases report in Thailand via the website
https://apps.doe.moph.go.th/boe/org.php (accessed on 6 January 2020). The user can access the system and select the year for downloading the data. For requesting the weather data in the southern region of Thailand, the user can access the system via the website
http://www.songkhla.tmd.go.th/service_main.php (accessed on 8 November 2019). The system provided the service for requesting 5 years of weather data using the user provided identifier information (i.e., name, parameter, time period, and location: name of district and province).
2.3. Data Analysis
For data pre-processing, the raw data of dengue cases in rich text format (RFT) and the raw weather data in Microsoft Excel Open XML Spreadsheet (XLSX) file were converted to comma-separated values (CSV) format using Microsoft Excel software. The processed data were imported to RStudio software for data analysis.
The distribution of dengue cases was assessed using box-and-whisker plots for the analysis of the spread period in the three southernmost provinces of Thailand (i.e., Pattani, Yala, and Narathiwat). A box plot provides a visualization of a distribution. The box stretches from the lower hinge (defined as the 25th percentile) to the upper hinge (the 75th percentile). The median is shown as a line across the box [
16]. Spearman’s rank correlation test was used to evaluate the correlations of the monthly weather variables and cases of dengue fever for time lags from zero to two months. The time lag was defined as the period between one weather observation and the incidence of dengue [
17]. A basic multivariable Poisson regression model can be written as:
The model adjusted for the first-order autocorrelation was:
Here, the variables XTmean, XTmin, XTmax, XRainfall, XRainydays, XRH, and XAirpressure stand for mean temperature, minimum temperature, maximum temperature, amount of rainfall, number of rainy days, relative humidity, and air pressure, respectively. All the weather variables were tested for multicollinearity with Variance Inflation Factors (VIF).
In assessing the selected model of the study area, data were divided into two sets: training and test sets. Data from January 2015 to December 2018 (training data) were used to create time series models. Seasonal adjustment with differencing was used for training data. Afterwards, the model was evaluated for prediction accuracy by using the data from January 2019 to December 2019 (test data). The residual deviance was used for a goodness of fit test, which shows how well the response is predicted by the model when the predictors are included. A low residual deviance implies that the trained model is appropriate. If the model is correct, the residual deviance should be approximately Chi-squared (χ2) with the stated degrees of freedom. All statistical analyses were performed using the RStudio version 1.2.5001 with a package of time series analysis (Northern Ave, Boston, MA, USA).
The inverse distance weighted (IDW) interpolation approach was used to estimate the weather data in all districts in the studied province. The IDW method is a spatial interpolation method, which uses spatial distance for the correlation calculation that is the distance weight calculation. IDW is used to estimate the properties at each unknown point [
18]. The IDW technique computes an average value for unsampled locations using values from nearby measured locations, with weights. The weights are proportional to the proximity of the sampled points to the unsampled location and can be modified by the IDW power coefficient.
The number of dengue cases and the estimated weather data with IDW interpolation approach in each district were used for dengue prediction in the district using the province model. The predicted dengue cases in the district were identified using the classes of dengue incidence rate, namely, 0.00, 0.01–70.00, 70.01–140.00, 140.01–210.00, 210.01–280.00, 280.01–350.00, and >350.00 [
19]. The class of dengue incidence rate in all districts among the three southernmost provinces were mapped from low to high dengue transmission risk areas shown by shading. The predicted dengue cases were grouped according to attribute values using equal intervals dividing the range of attribute values into equal-sized subranges. The annual incidence was then represented on a spatial map, created using the geographical information system ArcGIS version 10.8 (ESRI, Redlands, CA, USA).
The diagram illustrating the course of the research procedure is summarized in
Figure 3.
3. Results
During the study period from 2015 to 2019, ranking all data points for monthly dengue cases by province showed the largest number of dengue cases from June to August in Pattani province (
Figure 4a). In Yala province, the largest number of dengue cases occurred from June to September during 2015–2019 (
Figure 4b). Furthermore, the largest number of dengue cases occurred from June to October in Narathiwat, in the same study period (
Figure 4c). When comparing the distributions of dengue cases among the three southernmost provinces, it was found that Narathiwat had a longer disease delay than Pattani and Yala provinces. Additionally, there was the longest period of dengue transmission in Narathiwat province (i.e., from June to October) based on five years of data as the study period.
Spearman’s rank correlation test was used to analyze the association between dengue cases during the study period and weather predictors at zero to two months lag times. In Pattani, the monthly amount of rainfall, the number of rainy days, relative humidity, and mean temperature showed positive correlations with the dengue cases at a lag of 1 month (
Table 1). A positive association was also shown for minimum and maximum temperatures at a lag of 2 months (
Table 1). Monthly air pressure showed a negative correlation with dengue cases at a lag of two months in Pattani province (
Table 1).
In Yala province, relative humidity in the current month was positively associated with the number of dengue cases (
Table 1). A positive association was also observed for the monthly amount of rainfall, the number of rainy days and the mean/min/max temperatures at lags of one and two months, respectively (
Table 1). The air pressure was negatively correlated with the number of dengue cases at a lag of two months in Yala (
Table 1).
In Narathiwat province, the number of rainy days and the monthly amount of rainfall showed positive correlations with dengue cases in the current month and two months, respectively (
Table 1). The mean/min/max temperatures at a lag of two months were positively associated with dengue cases in Narathiwat (
Table 1), whereas negative correlations were observed between dengue cases and air pressure or relative humidity at a lag of two months (
Table 1).
Poisson Regression Model and Spatial Mapping
The number of dengue cases, relative humidity and the amount of rainfall at a lag of one month, and maximum temperature at a lag of two months were positively associated with the number of dengue cases at the current month in Pattani province (Poisson regression model: The number of dengue cases with lag 1, relative humidity with lag 1, rainfall with lag 1, maximum temperature with lag 2,
Table 2). The average air pressure at a lag of two months had negative effects on the number of dengue cases in Pattani (Poisson regression model: air pressure with lag 2,
Table 2).
The Poisson regression model for Pattani province was
The maximum temperature and the number of rainy days at a lag of two months, and the number of dengue cases during the previous month were positively associated with the number of dengue cases in the current month in Yala province (Poisson regression model: The number of rainy days with lag 2, maximum temperature with lag 2,
Table 3). The air pressure had a negative effect on the number of dengue cases in Yala (Poisson regression model: air pressure with lag 2,
Table 3).
The Poisson regression model for Yala province was
The number of dengue cases in the current month was related to the number of dengue cases during the previous month for Narathiwat province (Poisson regression model: The number dengue cases with lag 1,
Table 4). The amount of rainfall and minimum temperature at a lag of two months positively affected the number of dengue cases in Narathiwat (Poisson regression model: rainfall with lag 2, minimum temperature with lag 2,
Table 4). The air pressure at a lag of two months had a negative effect on the number of dengue cases (Poisson regression model: air pressure with lag 2,
Table 4).
The Poisson regression model for Narathiwat province was
During the prediction for January–December 2019, the residual deviance of our model in Pattani province is 863.02, suggesting that air pressure, relative humidity, amount of rainfall, maximum temperature, and past dengue cases can be used to explain the monthly dengue counts (Pattani province: AIC: 1196.8, Residual Deviance: 863.02). In Yala province, air pressure, number of rainy days, maximum temperature, and number of dengue cases in the previous month were suitable parameters to explain the monthly number of dengue cases (Yala province: AIC: 398.57, residual deviance: 202.59). In Narathiwat province, air pressure, amount of rainfall, minimum temperature, and past dengue cases can be used to explain the monthly dengue occurrence (Narathiwat province: AIC: 711.77, residual deviance: 446.52). The goodness-of-fit analyses revealed that the model fits the data reasonably well with chi-squared test statistically significant (Pattani: residual deviance: 863.02, Chi-squared test: χ241 = 108.00, p > 0.001; Yala: residual deviance: 202.59, Chi-squared test: χ241 = 119.99, p > 0.001; Narathiwat: residual deviance: 446.52, Chi-squared test: χ241 = 110.99, p > 0.001).
The best fitted model in all provinces was the time-series Poisson regression model (Model I) with the lowest AIC and residual deviance and high correlation coefficient between actual and predicted dengue cases (
Table 5).
The time-series Poisson regression models were developed by fitting the observed monthly dengue incidences over 48 months for the period from January 2015 to December 2018 and were validated with monthly numbers of dengue cases for the period from January 2019 to December 2019. The time series predictions for the validation period and the actual reported cases are shown in
Figure 5 (Pattani,
Figure 5a; Yala,
Figure 5b; and Narathiwat,
Figure 5c).
The predicted dengue cases in each district were obtained from the province model using the actual number of dengue cases and estimated weather data with IDW interpolation in the district. The spatial mapping of dengue fever cases in all districts among the three southernmost provinces of Thailand during the study period from 2015–2018 is shown in
Figure 6 (2015,
Figure 6a; 2016,
Figure 6b; 2017,
Figure 6c; 2018,
Figure 6d). Additionally, the distribution of actual and predicted dengue fever cases for all districts in the year 2019 were mapped from low to high dengue transmission risk areas shown by shading (actual dengue fever cases,
Figure 6e; predicted dengue fever cases,
Figure 6f).
4. Discussion
This study is the first attempt to develop a predictive model for dengue cases based on weather and geospatial data in the three southernmost provinces of Thailand, and to provide a basis for assessing dengue trends. The results of this study on the Poisson regression model suggest that weather factors are associated with the dengue case counts. Our results support a previous study [
8] in the claim that air pressure, relative humidity, rainfall, and temperature are associated with dengue incidence; that prior study was carried out in Nakhon Si Thammarat, Thailand.
The transient trends of dengue disease suggest that the weather variables play an important role in the dengue incidence in southern Thailand [
11]. Our findings indicate that dengue transmission occurred from June to August during 2015–2019 in Pattani province, from June to September in Yala, and from June to October in Narathiwat. In addition, the longest dengue transmission duration in these three southernmost provinces of Thailand is from June to October over the study period from 2015–2019. These results agree with a previous study in southern Thailand [
11] in that the longest dengue transmission duration in the Gulf of Thailand was from June to September; this is also consistent with previous findings in Singapore [
20] that indicate a higher dengue incidence from June to October. This might be because the geography and climate in Thailand and Singapore are similar. Thailand and Singapore are both located in Southeast Asia, and are geographically south of China, east of the Indian subcontinent and north-west of Australia. Singapore’s climate is characterized by two monsoon seasons: northeast monsoon from December to early March and southwest monsoon from June to September [
21]. The dengue incidence in Delhi, India is highest in April and from June to October [
22]. This might be because the monsoon periods differ between Thailand and India. Additionally, the maximum temperature in India reaches up to 45 °C during the summer in April, May, and June [
22].
Our results show that the highest dengue case counts occurred in June in Pattani and Yala provinces. Narathiwat province had the most dengue cases in August. These results are consistent with the previous findings that the most dengue cases occurred during June in the provinces near the Andaman Sea, including Phang-Nga, Phuket, Ranong, and Trang provinces [
11].
This study found that the temperature contributes to dengue transmission in three southernmost provinces of Thailand. This result corresponds with the previous studies [
23,
24] that temperature is reported as a precipitating factor for dengue transmission. Temperature is the most important weather factor affecting the growth and dispersion of mosquito vector, and a potential predictor of dengue outbreak [
11,
25]. Temperature also plays a role in altering the entire mosquito’s incubation life cycle and behavior, including the density of the mosquito population [
26], biting rates, gonotrophic cycle lengths, and vector size [
27]. The results in this study confirm the previous studies [
8,
28,
29] indicating that extreme temperature affects the development of dengue vectors [
21,
30,
31]. Therefore, temperature affects vectorial efficiency [
32] and risk of an epidemic [
33]. Given the association between temperature and dengue cases, the projected change in temperature may exacerbate dengue transmission by the three southernmost provinces of Thailand.
Our results show that rainfall and the number of rainy days were positively associated with dengue transmission in the three southernmost provinces of Thailand. This finding is in general agreement with other studies [
9,
11,
34], in which rainfall is reported as a precipitating factor for dengue transmission. Mosquitoes complete their life cycles in water, then hatch to be adult mosquitoes. Increased rain may increase larval habitat and vector population size by creating a new habitat or increase adult survival [
29]. This study found that the number of rainy days was positively associated with the number of dengue cases in Yala province. The results match those of a previous study [
11] in which the number of rainy days was positively associated with the number of dengue cases in Phatthalung province, but were negatively associated with the number of dengue cases in Nakhon Si Thammarat [
11]. Our findings may be influenced by the topographical similarity of Yala and Phatthalung provinces as there is no seaside area in Yala or Phatthalung, and the previous studies also showed that
Ae. albopictus are found more in seaside areas than in mountainous areas [
34].
Additionally, this study found that the amount of rainfall was associated with the dengue cases in Pattani and Narathiwat. Our findings confirm that rainfall is a critical factor influencing dengue epidemics, as previously reported in Taiwan [
35] and Jakarta [
9]. Light rain can occur in some areas, which creates a habitat for the
Ae. aegypti, while heavy rains can cause the larvae to be washed away, as reported in Malaysia [
36].
Our results show that relative humidity was positively correlated over the current month and was negatively correlated for the previous two months. Similar results were also found in previous studies [
14,
29,
37]. This might be because the relative humidity affects the rainfall, as it indicates the saturation of moisture in the air, and a downward change in temperature of saturated air will cause condensation and rain [
38].
The Pattani and Narathiwat provinces are near the Gulf of Thailand and have many rivers, while the Yala province does not have any land adjacent to the sea or mountains [
39]. In addition to the weather variables that affect the occurrence of dengue, the population density may affect dengue case counts [
40] because population congestion supports the spread of an epidemic. The population growth rate in the southernmost provinces in 2019 (2626 populations) has increased slightly from 2017 and 2018 (2017: 1447 populations; 2018: 943 populations) [
41].
5. Conclusions
This study presents spatial and temporal modelling of dengue fever transmission and mapping of dengue predictions using Geographic Information System (GIS) technology. The Poisson regression model using dengue case data and weather data included rainfall, number of rainy days, mean temperature, minimum temperature, maximum temperature, relative humidity, and air pressure as candidate predictors, in the three southernmost provinces of Thailand. The weather variables are the main predictors for dengue transmission with a high correlation between the actual monthly dengue cases and the predicted monthly dengue cases in the three southernmost provinces. The identification of trends in dengue cases can be used to support local public health policies and actions. Pre-planning of emergency mosquito control measures can help reduce the risk of a dengue outbreak [
42,
43].
This study had some limitations that should be mentioned to ensure that the study findings are fairly interpreted. Monthly data for five years were used in this study. Increasing sample size or spatial resolution could potentially improve the efficiency of the machine learning approach. Weekly data could be used for a more accurate model, using weather factors to predict dengue fever transmission. In addition, other factors such as land use, land cover, mosquito larvae data, and population density are interesting factors for updating or improving the dengue predictive model. Adding more environmental factors may improve the model and reduce the prediction errors. Automatic dengue prediction could be applied with other algorithms in machine learning. The results from this study may be useful scientific information, demonstrating use of weather data in the study areas in a predictive model, eventually intended for an early warning system on dengue transmission. The spatial mapping of dengue cases could enable effective area-based dengue prevention and control programs and enable more efficient planning for dealing with dengue fever. The predictive model can support decision making by public health organizations and for management of high-risk areas.
 ), Yala (
), Yala ( ), and Narathiwat (
), and Narathiwat ( ), and (b) study area map with land cover data including rivers (
), and (b) study area map with land cover data including rivers ( ), forests and mountains (
), forests and mountains ( ), and ground (
), and ground ( ).
).
 ), Yala (
), Yala ( ), and Narathiwat (
), and Narathiwat ( ), and (b) study area map with land cover data including rivers (
), and (b) study area map with land cover data including rivers ( ), forests and mountains (
), forests and mountains ( ), and ground (
), and ground ( ).
).