Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria
Abstract
:1. Introduction
2. Medical Waste Challenges in Nigeria
3. Methodology
3.1. Multi-Criteria Decision Analysis
- Resource assignment
- Choice
- Market comparison
- Prioritization
- Quality control

3.2. Ethical Consideration
4. Results and Discussion
4.1. The Results of the Analytical Hierarchy Process (AHP)
4.2. The Results of the Fuzzy Analytical Hierarchy Process (F-AHP)
4.3. Comparative Validation of Results using Fuzzy TOPSIS and Sensitivity Analysis
4.4. Implication of Medical Waste Management on Health Workers and the Public Health in Nigeria
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Safe Management of Wastes from Healthcare Activities, 2nd ed.; Chartier, Y., Emmanuel, J., Pieper, U., Pruss, A., Rushbrook, P., Stringer, R., Townend, W., Wilbum, S., Zghondi, R., Eds.; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- WHO. Safe Management of Wastes from Healthcare Activities. 2017. Available online: https://apps.who.int/iris/handle/10665/259491 (accessed on 3 February 2021).
- Romero, I.; Carnero, M.C. Environmental assessment in health care organizations. Environ. Sci. Pollut. Res. 2019, 26, 3196–3207. [Google Scholar] [CrossRef]
- Aung, T.; Luan, S.; Xu, Q. Application of multi-criteria-decision approach for the analysis of medical waste management systems in Myanmar. J. Clean. Prod. 2019, 222, 733–745. [Google Scholar] [CrossRef]
- You, S.; Sonne, C.; Ok, Y.S. COVID-19’s unsustainable waste management. Science 2020, 368. [Google Scholar] [CrossRef]
- Manupati, V.K.; Ramkumar, M.; Baba, V.; Agarwal, A. Selection of the best healthcare waste disposal techniques during and post COVID-19 pandemic era. J. Clean. Prod. 2020, 281, 125175. [Google Scholar] [CrossRef]
- Emenike, P.C.; Tenebe, T.I.; Omeje, M.; Osinubi, D.S. Health risk assessment of heavy metal variability in sachet water sold in Ado-Odo Ota, South-Western Nigeria. Environ. Monit. Assess. 2017, 189, 480. [Google Scholar] [CrossRef]
- Federal Ministry of Health. Nigeria Health Facility Registry. 2021. Available online: https://hfr.health.gov.ng/ (accessed on 27 January 2021).
- Worldometer. Nigeria Population. 2021. Available online: https://www.worldometers.info/world-population/nigeria-population/ (accessed on 24 June 2021).
- United Nations. World Population Projected to Reach 9.8 Billion in 2050, and 11.2 Billion in 2100. 2017. Available online: https://www.un.org/en/development/desa/population/events/pdf/other/21/21June_FINALPRESSRELEASE_WPP17.pdf (accessed on 22 January 2021).
- Etim, M.-A.; Babaremu, K.; Lazarus, J.; Omole, D. Health Risk and Environmental Assessment of Cement Production in Nigeria. Atmosphere 2021, 12, 1111. [Google Scholar] [CrossRef]
- Omole, D.O.; Isiorho, S.A. Municipal Solid Wastes and Water Quality Issues in Nigeria. 2013. Available online: https://gsa.confex.com/gsa/2013AM/webprogram/Paper225375.html (accessed on 21 January 2021).
- Kaza, S.; Yao, L.; Bhada-Tata, P.; Van Woerden, F. What a Waste 2.0: A Global Snapshot of Solid Waste Management to 2050; World Bank: Washington, DC, USA, 2018. [Google Scholar] [CrossRef]
- Ike, C.C.; Ezeibe, C.C.; Anijiofor, S.C.; Daud, N.N.N. Solid Waste Management in Nigeria: Problems, Prospects, and Policies. J. Solid Waste Technol. Manag. 2018, 44, 163–172. [Google Scholar] [CrossRef]
- BioEnergy Consult. Solid Waste Management in Nigeria. 2021. Available online: https://www.bioenergyconsult.com/solid-waste-nigeria/ (accessed on 24 June 2021).
- Abah, S.O.; Ohimain, E.I. Healthcare waste management in Nigeria: A case study. J. Public Heal. Epidemiol. 2011, 3, 99–110. [Google Scholar]
- Longe, O.E. Healthcare waste management status in Lagos State, Nigeria: A case study from selected healthcare facilities in Ikorodu and Lagos metropolis. Waste Manag. Res. 2011, 30, 562–571. [Google Scholar] [CrossRef]
- Federal Ministry of Health. National Healthcare Waste Management Policy Federal Ministry of Environment in Collaboration with Federal Ministry of Health. 2013. Available online: https://www.technet-21.org/media/com_resources/trl/6133/multi_upload/NationalHealthcareWasteManagementPolicy(2013).pdf (accessed on 27 June 2021).
- Stanley, H.; Okpara, K. Health care waste management in Port Harcourt Metropolis. Am. J. Sci. Ind. Res. 2011, 2, 769–773. [Google Scholar] [CrossRef]
- National Environmental Standards and Regulations Enforcement Agency. National Environmental (Sanitation and Wastes Control) Regulations 2009. 2009. Available online: https://www.nesrea.gov.ng/wp-content/uploads/2020/02/Sanitation_and_Wastes_Control_Regulations 2009.pdf (accessed on 27 January 2021).
- Federal Ministry of Health. Health Care Waste Management Plan (HCWMP) for Nigerian polio Eradication Support Project Additional Financing 3 Draft Report. 2018. Available online: https://documents1.worldbank.org/curated/pt/448401525781824503/text/Health-care-waste-management-plan.txt (accessed on 27 June 2021).
- Adunlin, G.; Diaby, V.; Montero, A.J.; Xiao, H. Multicriteria decision analysis in oncology. Health Expect. 2014, 18, 1812–1826. [Google Scholar] [CrossRef]
- Gani, M.A.; Tayyeh, H.K.; Hamid, R.A. Intelligent system for graduation projects allocation based on MCDA methods. Mater. Today Proc. 2021. [Google Scholar] [CrossRef]
- Maghsoodi, A.I.; Riahi, D.; Herrera-Viedma, E.; Zavadskas, E.K. An integrated parallel big data decision support tool using the W-CLUS-MCDA: A multi-scenario personnel assessment. Knowl. Based Syst. 2020, 195, 105749. [Google Scholar]
- Karczmarczyk, A.; Wątróbski, J.; Jankowski, J.; Ziemba, E. Comparative study of ICT and SIS measurement in Polish households using a MCDA-based approach. Procedia Comput. Sci. 2019, 159, 2616–2628. [Google Scholar] [CrossRef]
- Deshpande, P.C.; Skaar, C.; Brattebø, H.; Fet, A.M. Multi-criteria decision analysis (MCDA) method for assessing the sustainability of end-of-life alternatives for waste plastics: A case study of Norway. Sci. Total Environ. 2020, 719, 137353. [Google Scholar] [CrossRef]
- Rolles, S.; Schlag, A.K.; Measham, F.; Phillips, L.; Nutt, D.; Bergsvik, D.; Rogeberg, O. A multi criteria decision analysis (MCDA) for evaluating and appraising government policy responses to non medical heroin use. Int. J. Drug Policy 2021, 91, 103180. [Google Scholar] [CrossRef] [PubMed]
- Teich, V.; Penha, M.; Sano, F.; Martin, G.S.; Farina, T.; Gondo, C.; Campolina, A.; Mattar, Z.; Salgado, J. PRS49 a multicriteria decision analysis (MCDA) to evaluate alternative treatments for severe asthma in adult patients under the brazilian private healthcare system perspective. Value Health 2019, 22, S358. [Google Scholar] [CrossRef]
- Mokarram, M.; Mokarram, M.J.; Gitizadeh, M.; Niknam, T.; Aghaei, J. A novel optimal placing of solar farms utilizing multi-criteria decision-making (MCDA) and feature selection. J. Clean. Prod. 2020, 261, 121098. [Google Scholar] [CrossRef]
- Pagone, E.; Salonitis, K.; Jolly, M. Automatically weighted high-resolution mapping of multi-criteria decision analysis for sustainable manufacturing systems. J. Clean. Prod. 2020, 257, 120272. [Google Scholar] [CrossRef]
- Cuoghi, K.G.; Leoneti, A.B. A group MCDA method for aiding decision-making of complex problems in public sector: The case of Belo Monte Dam. Socio Econ. Plan. Sci. 2018, 68, 100625. [Google Scholar] [CrossRef]
- Bogaart, E.H.V.D.; Kroese, M.E.; Spreeuwenberg, M.D.; Ruwaard, D.; Tsiachristas, A. Economic Evaluation of New Models of Care: Does the Decision Change Between Cost-Utility Analysis and Multi-Criteria Decision Analysis? Value Health 2021, 24, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Tseng, M.-L. Application of ANP and DEMATEL to evaluate the decision-making of municipal solid waste management in Metro Manila. Environ. Monit. Assess. 2008, 156, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Babalola, M.A. A Multi-Criteria Decision Analysis of Waste Treatment Options for Food and Biodegradable Waste Management in Japan. Environments 2015, 2, 471–488. [Google Scholar] [CrossRef] [Green Version]
- Aghapour, P.; Nabizadeh, R.; Nouri, J.; Monavari, M.; Yaghmaeian, K. Analysis of hospital waste using a healthcare waste management index. Toxicol. Environ. Chem. 2013, 95, 579–589. [Google Scholar] [CrossRef]
- Carnero, M.C. Assessment of Environmental Sustainability in Health Care Organizations. Sustainability 2015, 7, 8270–8291. [Google Scholar] [CrossRef] [Green Version]
- Zamparas, M.; Kapsalis, V.; Kyriakopoulos, G.; Aravossis, K.; Kanteraki, A.; Vantarakis, A.; Kalavrouziotis, I. Medical waste management and environmental assessment in the Rio University Hospital, Western Greece. Sustain. Chem. Pharm. 2019, 13. [Google Scholar] [CrossRef]
- Nguyen, D.L.; Nguyen, X.T.B.T.H. Estimation of Current and Future Generation of Medical Solid Wastes In Hanoi City, Vietnam. Int. J. Waste Resour. 2014, 4. [Google Scholar] [CrossRef] [Green Version]
- Farzadkia, M.; Emamjomeh, M.M.; Golbaz, S.; Sajadi, H.S. An investigation on hospital solid waste management in Iran. Glob. Nest J. 2015, 17, 771–783. [Google Scholar]
- Komilis, D.; Fouki, A.; Papadopoulos, D. Hazardous medical waste generation rates of different categories of health-care facilities. Waste Manag. 2012, 32, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Yong, Z.; Gang, X.; Guanxing, W.; Tao, Z.; Dawei, J. Medical waste management in China: A case study of Nanjing. Waste Manag. 2009, 29, 1376–1382. [Google Scholar] [CrossRef]
- Muthoni, M.S.; Nyerere, K.A.; Ngugi, C.W. Assessment of Level of Knowledge in Medical Waste Management in Selected Hospitals in Kenya. Appl. Microbiol. Open Access 2016, 2. [Google Scholar] [CrossRef]
- Saaty, T.L.; Vargas, L.G. The Analytic Hierarchy Process: Planning, Priority Setting, Resource Allocation; McGraw-Hill: New York, NY, USA, 1980. [Google Scholar]
- Mufazzal, S.; Muzakkir, S. A new multi-criterion decision making (MCDM) method based on proximity indexed value for minimizing rank reversals. Comput. Ind. Eng. 2018, 119, 427–438. [Google Scholar] [CrossRef]
- Liu, X.; Wan, S.-P. A method to calculate the ranges of criteria weights in ELECTRE I and II methods. Comput. Ind. Eng. 2019, 137, 106067. [Google Scholar] [CrossRef]
- Afrane, S.; Ampah, J.D.; Jin, C.; Liu, H.; Aboagye, E.M. Techno-economic feasibility of waste-to-energy technologies for investment in Ghana: A multicriteria assessment based on fuzzy TOPSIS approach. J. Clean. Prod. 2021, 318, 128515. [Google Scholar] [CrossRef]
- Bhushan, N.; Kanwal, R. Strategic Decision Making; Springer: London, UK, 2004. [Google Scholar]
- Gani, A.; Asjad, M.; Talib, F. Prioritization and Ranking of indicators of sustainable manufacturing in Indian MSMEs using fuzzy AHP approach. Mater. Today Proc. 2021, 46, 6631–6637. [Google Scholar] [CrossRef]
- Olabanji, O.M.; Mpofu, K. Appraisal of conceptual designs: Coalescing fuzzy analytic hierarchy process (F-AHP) and fuzzy grey relational analysis (F-GRA). Results Eng. 2020, 9, 100194. [Google Scholar] [CrossRef]










| Goal: Assessment of Medical Waste Management Systems in Ota | ||
|---|---|---|
| Serial Number | Criterion | Attributes |
| M1 | Waste Segregation | This measures the efficiency of waste segregation into their different categories during waste generation in a particular medical facility. Health workers can identify each waste based on its potential hazard, and disposal is into the recommended color-coded containers. |
| M2 | Budget/Operational Cost | This measures the total budget and operating cost involved per year in operating and maintaining a particular medical facility. |
| M3 | Waste Treatment | This analyses the type and amount of waste that can be treated by each medical facility in a particular cycle of operation and the different treatment methods available. Are sharps autoclaved, shredded, or captured in cement? |
| M4 | Waste Transportation | This analyzes the various approaches by which medical waste is transported from facilities to treatment and disposal sites. Is the transportation time for medical waste fixed? How compliant are waste handlers when transporting and managing medical waste? |
| M5 | Waste Disposal | This measures the various disposal methods of medical waste, their disposal sites, and the closeness of the disposal site to a medical facility. |
| M6 | Environmental Public Health/Occupational Safety Practices | This analyzes the environmental degrading toxic emissions associated with each medical facility and the dangerous health effects on health workers and the immediate surroundings. It further examines the requirement of various safety procedures and risks associated with operating a particular medical facility. Prevention against nosocomial infections. Documentation of incidents and accidents during medical operations and waste handling. Are health workers immunized against potentially infectious diseases? |
| M7 | Awareness/Capacity Building | This measures the occupational awareness of health workers and professionals to medical waste management and the aptitude of each facility to develop its workers. How often are health workers trained on managing emerging infections? |
| M8 | Organizational Policy/Management Plan | This analyzes the operational structure of medical waste management available in each facility. It measures the implementation of internal regulations and the national policy of medical waste management. Is there a health, safety, and environmental officer in charge of managing, monitoring, and enforcing the best waste management practices within each facility? |
| M9 | Waste Collection and Storage | This measure covers the different types of waste collection and storage methods available for various categories of medical waste, storage time, and collection procedures. Containers are correctly labelled. Medical waste bins are filled to no more than ¾ full. |
| Medical Facility (MF) | Hospital Type | Facility Level | |||
|---|---|---|---|---|---|
| Private | Public | Primary | Secondary | Tertiary | |
| MF–1: H5 | |||||
| MF–2: H6 | |||||
| MF–3: H7 | |||||
| MF–4: H4 | |||||
| MF–5: H2 | |||||
| MF–6: H1 | |||||
| MF–7: H3 | |||||
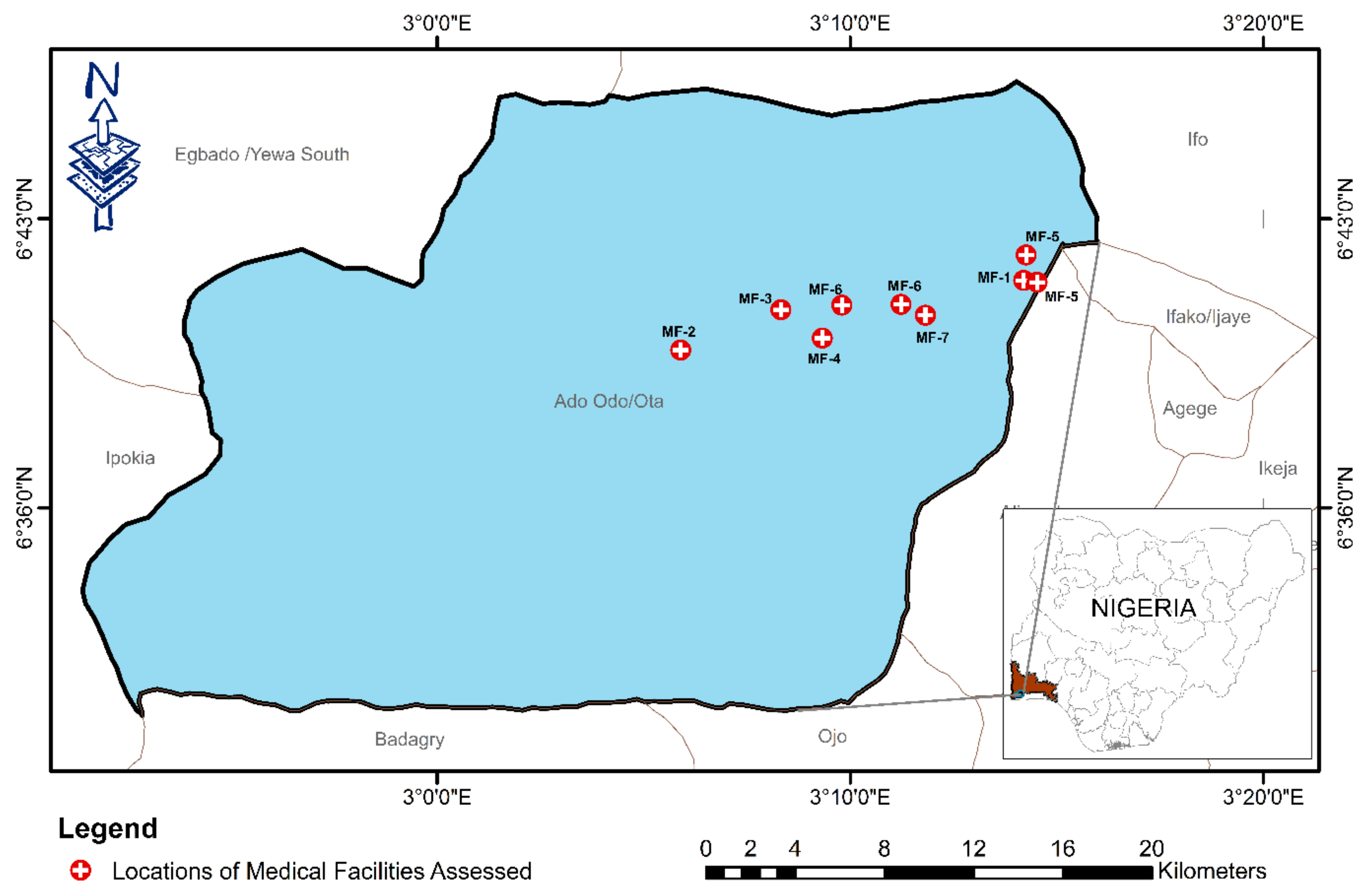
| S/N | Health Institution | Description | Services Rendered | No. of Beds | No. of Health Workers | Location |
|---|---|---|---|---|---|---|
| 1 | H5 | Largest public health center in Ota, publicly owned | Outpatient services, infant care and immunization services, family planning, ante-natal planning, post-natal planning, maternity, pharmaceutical services, XYZ session, eye clinic, laboratory services. | 7 | 29 | Ota |
| 2 | H2 | Privately owned | 24-h general outpatient clinic services and in-patient care, 24-h emergency and ambulance services, antenatal clinic, post-natal care, dental clinic, laboratory services, public health services such as family planning and immunization, pharmaceutical services, visual care services, general surgical services, diagnostic imaging and radiology, pediatrics, maternity services. | 26 | 55 | Ota |
| 3 | H6 | Largest primary health center in Atan, publicly owned | 24-h general outpatient clinic services and in-patient care, antenatal clinic, post-natal care, laboratory services, public health services such as family planning and immunization, pharmaceutical services, maternity services. | 4 | 8 | Atan |
| 4 | H7 | Largest primary health center in Iju, publicly owned | 24-h general outpatient clinic services and in-patient care, antenatal clinic, post-natal care, public health services such as family planning and immunization, pharmaceutical services, maternity services. | 4 | 7 | Iju |
| 5 | H3 | Privately owned | 24-h general outpatient clinic services and in-patient care, 24-h emergency and ambulance services, antenatal clinic, post-natal care, dental clinic, laboratory services, pharmaceutical services, general surgical services, physiotherapy, diagnostic imaging and radiology, maternity services, orthopedic services. | 29 | 24 | Ota |
| 6 | H1 | Largest privately-owned hospital in Ota | 24-h general outpatient clinic services and in-patient care, 24-h emergency and ambulance services, antenatal clinic, post-natal care, dental clinic, laboratory services, public health services such as family planning and immunization, pharmaceutical services, visual care services, general surgical services, physiotherapy, intensive care unit (ICU) or intensive treatment unit (ITU), diagnostic imaging and radiology, internal medicine (gastroenterology, cardiology, nephrology, pulmonology, etc.), pediatrics, maternity services. | 36 | 75 | Ota |
| 7 | H4 | Institutional and privately owned hospital | 24-h general outpatient clinic services and in-patient care, 24-h emergency and ambulance services, antenatal clinic, post-natal care, dental clinic, laboratory services, public health services such as family planning and immunization, pharmaceutical services, visual care services, general surgical services, physiotherapy, diagnostic imaging and radiology, pediatrics, maternity services. | 50 | 77 | Ota |
| Relative Intensity | Definition | Description |
|---|---|---|
| 1 | Equal value | Two criteria are of equal value |
| 3 | Slightly greater value | Slightly favors one criterion over another |
| 5 | Essential or strong value | Strongly favors one criterion over another |
| 7 | Very strong value | A criterion is strongly favored, and its dominance is demonstrated in practice |
| 9 | Extreme value | Highest possible order of affirmation and evidence favoring one over another |
| 2, 4, 6, 8 | Intermediate values between two adjacent judgements | When conciliation is required |
| Reciprocals | Reciprocals for inverse comparison | |
| Size of matrix | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| Random index (RI) | 0 | 0 | 0.58 | 0.9 | 1.12 | 1.24 | 1.32 | 1.41 | 1.45 | 1.49 | 1.51 | 1.58 |
| Linguistic Scale | Fuzzy Number | Triangular Fuzzy Numbers | Triangular Fuzzy Reciprocal Numbers |
|---|---|---|---|
| Equally important | (1, 1, 1) | (1, 1, 1) | |
| Judgement values between equally and moderately | (1, 2, 3) | (1/3, 1/2, 1) | |
| Moderately more important | (2, 3, 4) | (1/4, 1/3, 1/2) | |
| Judgement values between moderately and strongly | (3, 4, 5) | (1/5, 1/4, 1/3) | |
| Strongly more important | (4, 5, 6) | (1/6, 1/5, 1/4) | |
| Judgement values between strongly and very strongly | (5, 6, 7) | (1/7, 1/6, 1/5) | |
| Very strongly more important | (6, 7, 8) | (1/8, 1/7, 1/6) | |
| Judgement values between very strongly and extremely | (7, 8, 9) | (1/9, 1/8,/7) | |
| Extremely more important | (8, 9, 9) | (1/9, 1/9, 1/8) |
| Criteria | M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | M9 |
|---|---|---|---|---|---|---|---|---|---|
| M1 | 1.0000 | 2.0000 | 3.0000 | 3.0000 | 1.0000 | 2.0000 | 1.0000 | 3.0000 | 1.0000 |
| M2 | 0.5000 | 1.0000 | 3.0000 | 1.0000 | 1.0000 | 0.3333 | 1.0000 | 2.0000 | 2.0000 |
| M3 | 0.3333 | 0.3333 | 1.0000 | 2.0000 | 0.3333 | 1.0000 | 1.0000 | 1.0000 | 1.0000 |
| M4 | 0.3333 | 1.0000 | 0.5000 | 1.0000 | 1.0000 | 0.3333 | 0.3333 | 0.3333 | 2.0000 |
| M5 | 1.0000 | 1.0000 | 3.0000 | 1.0000 | 1.0000 | 3.0000 | 1.0000 | 1.0000 | 2.0000 |
| M6 | 0.5000 | 3.0000 | 1.0000 | 3.0000 | 0.3333 | 1.0000 | 3.0000 | 2.0000 | 2.0000 |
| M7 | 1.0000 | 1.0000 | 1.0000 | 3.0000 | 1.0000 | 0.3333 | 1.0000 | 2.0000 | 1.0000 |
| M8 | 0.3333 | 0.5000 | 1.0000 | 3.0000 | 1.0000 | 0.5000 | 0.5000 | 1.0000 | 2.0000 |
| M9 | 1.0000 | 0.5000 | 1.0000 | 0.5000 | 0.5000 | 0.5000 | 1.0000 | 0.5000 | 1.0000 |
| Criteria | Weighted Sum Value | Criteria Weight | Average |
|---|---|---|---|
| M1 | 1.7361 | 0.1674 | 10.3667 |
| M2 | 1.1278 | 0.1134 | 9.9400 |
| M3 | 0.7840 | 0.07552 | 10.3803 |
| M4 | 0.6861 | 0.0692 | 9.9072 |
| M5 | 1.5289 | 0.1469 | 10.4022 |
| M6 | 1.5703 | 0.1528 | 10.2751 |
| M7 | 1.1267 | 0.1121 | 10.0464 |
| M8 | 0.9099 | 0.0901 | 10.0964 |
| M9 | 0.7137 | 0.0722 | 9.8817 |
| 10.144 |
| M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | M9 | Criteria Weight | Weighted Sum | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 | 0.1667 | 0.1935 | 0.2069 | 0.1714 | 0.1395 | 0.2222 | 0.1017 | 0.2338 | 0.0714 | 0.1675 | 1.7361 |
| M2 | 0.0833 | 0.0968 | 0.2069 | 0.0571 | 0.1395 | 0.0370 | 0.1017 | 0.1558 | 0.1429 | 0.1135 | 1.1278 |
| M3 | 0.0556 | 0.0323 | 0.0690 | 0.1143 | 0.0465 | 0.1111 | 0.1017 | 0.0779 | 0.0714 | 0.0755 | 0.7840 |
| M4 | 0.0556 | 0.0968 | 0.0345 | 0.0571 | 0.1395 | 0.0370 | 0.0339 | 0.0260 | 0.1429 | 0.0693 | 0.6861 |
| M5 | 0.1667 | 0.0968 | 0.2069 | 0.0571 | 0.1395 | 0.3333 | 0.1017 | 0.0779 | 0.1429 | 0.1470 | 1.5289 |
| M6 | 0.0833 | 0.2903 | 0.0690 | 0.1714 | 0.0465 | 0.1111 | 0.3051 | 0.1558 | 0.1429 | 0.1528 | 1.5703 |
| M7 | 0.1667 | 0.0968 | 0.0690 | 0.1714 | 0.1395 | 0.0370 | 0.1017 | 0.1558 | 0.0714 | 0.1122 | 1.1267 |
| M8 | 0.0556 | 0.0484 | 0.0690 | 0.1714 | 0.1395 | 0.0556 | 0.0508 | 0.0779 | 0.1429 | 0.0901 | 0.9099 |
| M9 | 0.1667 | 0.0484 | 0.0690 | 0.0286 | 0.0698 | 0.0556 | 0.1017 | 0.0390 | 0.0714 | 0.0722 | 0.7137 |
| 1 | 9 |
| Inconsistency | IC = 0.1430 | RC = 0.0986 | |
|---|---|---|---|
| Criteria | Normalized | Idealized | Ranks |
| Waste Segregation, M1 | 0.1675 | 1 | 1 |
| Budget/Operational Cost, M2 | 0.1135 | 0.6776 | 4 |
| Waste Treatment, M3 | 0.0755 | 0.4507 | 7 |
| Waste Transportation, M4 | 0.0693 | 0.4137 | 9 |
| Waste Disposal, M5 | 0.147 | 0.8776 | 3 |
| Environmental Public Health/Occupational Safety Practices, M6 | 0.1528 | 0.9122 | 2 |
| Awareness/Capacity Building, M7 | 0.1122 | 0.6698 | 5 |
| Organizational Policy/Management Plan, M8 | 0.0901 | 0.5379 | 6 |
| Waste Collection and Storage, M9 | 0.0722 | 0.4310 | 8 |
| Criteria | Fuzzy Weights | Normalized | Idealized | Rank | ||
|---|---|---|---|---|---|---|
| Waste Segregation, M1 | 0.103 | 0.178 | 0.273 | 0.1703 | 1 | 1 |
| Budget/Operational Cost, M2 | 0.067 | 0.114 | 0.186 | 0.1128 | 0.6624 | 5 |
| Waste Treatment, M3 | 0.052 | 0.079 | 0.121 | 0.0773 | 0.4540 | 7 |
| Waste Transportation, M4 | 0.039 | 0.065 | 0.112 | 0.0663 | 0.3896 | 9 |
| Waste Disposal, M5 | 0.096 | 0.146 | 0.207 | 0.1379 | 0.8093 | 3 |
| Environmental Public Health/Occupational Safety Practices, M6 | 0.078 | 0.135 | 0.253 | 0.1433 | 0.8411 | 2 |
| Awareness/Capacity Building, M7 | 0.076 | 0.129 | 0.192 | 0.1219 | 0.7158 | 4 |
| Organizational Policy/Management Plan, M8 | 0.053 | 0.084 | 0.164 | 0.0925 | 0.5431 | 6 |
| Waste Collection and Storage, M9 | 0.045 | 0.072 | 0.135 | 0.0772 | 0.4533 | 8 |
| M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | M9 | Priorities | Rank | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| H1 | 0.0442 | 0.0289 | 0.0134 | 0.0120 | 0.0265 | 0.0253 | 0.0236 | 0.0195 | 0.0200 | 0.2134 | 1 |
| H2 | 0.0379 | 0.0205 | 0.0120 | 0.0123 | 0.0245 | 0.0268 | 0.0131 | 0.0173 | 0.0167 | 0.1811 | 2 |
| H3 | 0.0221 | 0.0174 | 0.0211 | 0.0192 | 0.0372 | 0.0299 | 0.0105 | 0.0133 | 0.0100 | 0.1805 | 3 |
| H4 | 0.0205 | 0.0186 | 0.0101 | 0.0096 | 0.0213 | 0.0172 | 0.0314 | 0.0170 | 0.0093 | 0.1549 | 4 |
| H5 | 0.0162 | 0.0113 | 0.0073 | 0.0047 | 0.0111 | 0.0167 | 0.0121 | 0.0108 | 0.0076 | 0.0978 | 5 |
| H6 | 0.0144 | 0.0081 | 0.0069 | 0.0043 | 0.0090 | 0.0123 | 0.0223 | 0.0075 | 0.0077 | 0.0926 | 6 |
| H7 | 0.0151 | 0.0081 | 0.0065 | 0.0043 | 0.0084 | 0.0152 | 0.0090 | 0.0071 | 0.0060 | 0.0796 | 7 |
| Rank | |||||
|---|---|---|---|---|---|
| H1 | 0.272531 | 0.937214 | 1.209745 | 0.774721 | 1 |
| H2 | 0.512023 | 0.699195 | 1.211218 | 0.577266 | 3 |
| H3 | 0.482834 | 0.725442 | 1.208276 | 0.600394 | 2 |
| H4 | 0.670391 | 0.538376 | 1.208767 | 0.445393 | 4 |
| H5 | 1.058571 | 0.152301 | 1.210872 | 0.125778 | 5 |
| H6 | 1.094628 | 0.118767 | 1.213394 | 0.09788 | 6 |
| H7 | 1.203205 | 0.023483 | 1.226688 | 0.019143 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Etim, M.-A.; Academe, S.; Emenike, P.; Omole, D. Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria. Sustainability 2021, 13, 10914. https://doi.org/10.3390/su131910914
Etim M-A, Academe S, Emenike P, Omole D. Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria. Sustainability. 2021; 13(19):10914. https://doi.org/10.3390/su131910914
Chicago/Turabian StyleEtim, Mmemek-Abasi, Sunday Academe, PraiseGod Emenike, and David Omole. 2021. "Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria" Sustainability 13, no. 19: 10914. https://doi.org/10.3390/su131910914
APA StyleEtim, M.-A., Academe, S., Emenike, P., & Omole, D. (2021). Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria. Sustainability, 13(19), 10914. https://doi.org/10.3390/su131910914






