Indoor Air Pollution with Fine Particles and Implications for Workers’ Health in Dental Offices: A Brief Review
Abstract
1. Introduction
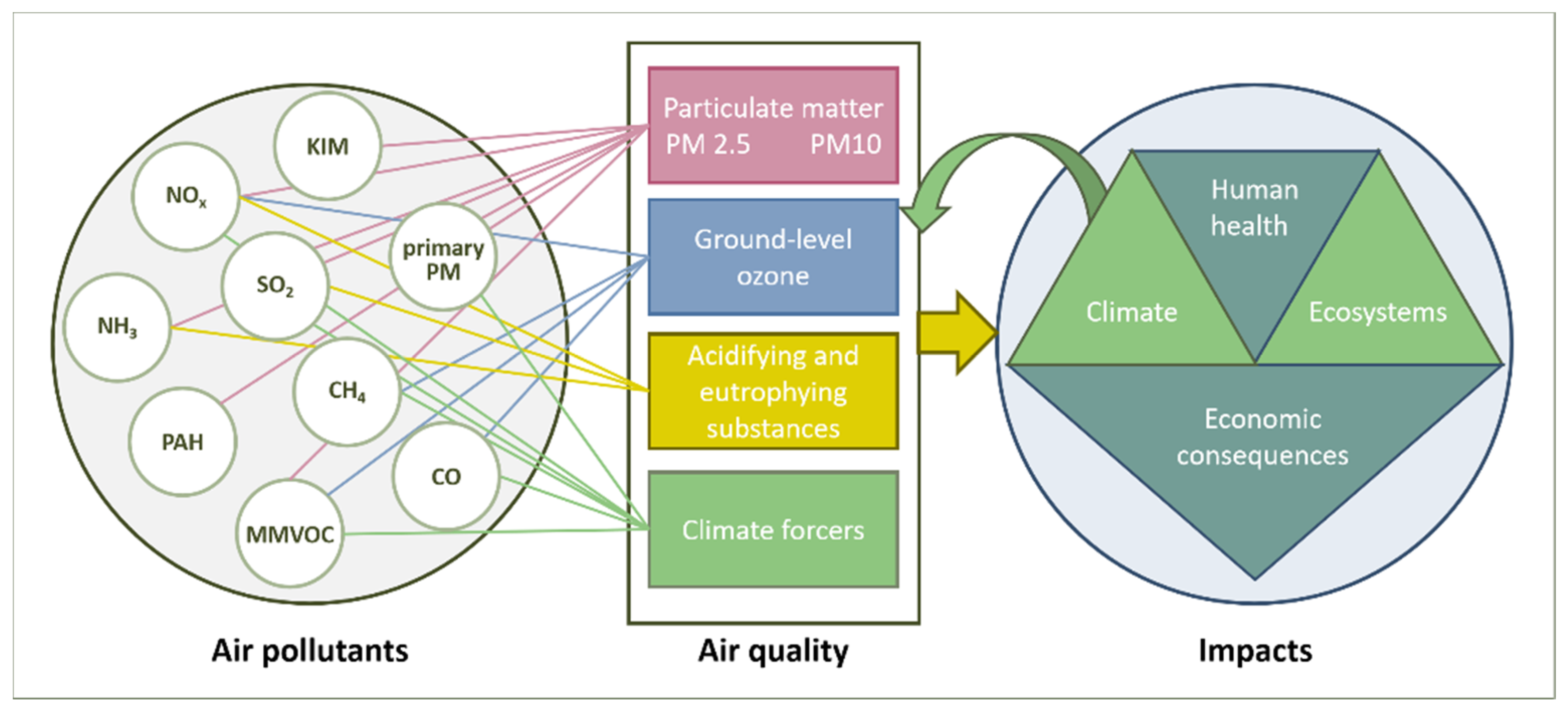
2. Factors Affecting the Indoor Air Quality
2.1. Outdoor Sources of PM10 and PM2.5 Pollution
2.2. Indoor Sources of PM10 and PM2.5
3. Results
3.1. Health Aspects of Air Pollution with PM
3.2. Indoor Air Pollution in Dentistry
3.2.1. Source of Occupational Exposure in Dental Offices and Potential Hazards
3.2.2. Pathogenic Potential of Aerosols
3.2.3. Chemical Hazards in Dental Workers
3.2.4. Dental Technicians and Their High Risk of Developing Occupational Illness
Respiratory Diseases
Skin Diseases
Neuropathies
Muscular Disorders
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Novel Coronavirus (2019-nCoV); Situation Report—12; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200201-sitrep-12-ncov.pdf?sfvrsn=273c5d35_2 (accessed on 30 May 2020).
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020, 7, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Singhal, T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Cirrincione, L.; Plescia, F.; Ledda, C.; Rapisarda, V.; Martorana, D.; Moldovan, R.E.; Theodoridou, K.; Cannizzaro, E. COVID-19 Pandemic: Prevention and Protection Measures to be Adopted at the Workplace. Sustainability 2020, 12, 3603. [Google Scholar] [CrossRef]
- Zhonghua, L.; Xing, B.; Xue, Z.Z. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin. J. Epidemiol. 2020, 41, 145–151. [Google Scholar] [CrossRef]
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 101–110. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.; Gamble, A.; Williamson, B.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.; et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N. Eng. J. Med. 2020, 1564–1567. [Google Scholar] [CrossRef]
- Pan, M.; Leah, C.; Lednicky, J.A.; Eiguren-Fernandez, A.; Hering, S.; Fan, Z.H.; Wu, C.-Y. Determination of the distribution of infectious viruses in aerosol particles using water-based condensational growth technology and a bacteriophage MS2 model. Aerosol. Sci. Technol. 2019, 53, 583–593. [Google Scholar] [CrossRef]
- Pan, M.; Lednicky, J.A. Collection, particle sizing and detection of airborne viruses. J. Appl. Microbiol. 2019, 127, 1596–1611. [Google Scholar] [CrossRef]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef]
- Gordon, C.J.; Tchesnokov, E.P.; Feng, J.Y.; Porter, D.P.; Gotte, M. The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus. J. Biol. Chem. 2020, 295, 4773–4779. [Google Scholar] [CrossRef]
- Ye, X.T.; Luo, Y.L.; Xia, S.C.; Sun, Q.F.; Ding, J.G.; Zhou, Y.; Chen, W.; Wang, X.F.; Zhang, W.W.; Du, W.J.; et al. Clinical efficacy of lopinavir/ritonavir in the treatment of Coronavirus disease 2019. Eur. Rev. Med. Pharm. Sci. 2020, 24, 3390–3396. [Google Scholar] [CrossRef]
- Setti, L.; Passarini, F.; De Gennaro, G.; Di Gilio, A.; Palmisani, J.; Buono, P.; Fornari, G.; Perrone, M.G.; Piazzalunga, A.; Barbieri, P.; et al. Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough. Int. J. Environ. Res. Public Health 2020, 17, 2932. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Milton, D.K. It is Time to Address Airborne Transmission of COVID-19. Clin. Infect. Dis. 2020, 71, 2311–2313. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study; Version 2. medRxiv 2020. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Causes of Death. Available online: https://ourworldindata.org/causes-of-death (accessed on 30 May 2020).
- Hendryx, M.; Islam, M.S.; Dong, G.-H.; Paul, G. Air Pollution Emissions 2008–2018 from Australian Coal Mining: Implications for Public and Occupational Health. Int. J. Environ. Res. Public Health 2020, 17, 1570. [Google Scholar] [CrossRef]
- Barthelemy, J.; Sanchez, K.; Miller, M.R.; Khreis, H. New Opportunities to Mitigate the Burden of Disease Caused by Traffic Related Air Pollution: Antioxidant-Rich Diets and Supplements. Int. J. Environ. Res. Public Health 2020, 17, 630. [Google Scholar] [CrossRef]
- Kumar, B.; Verma, K.; Kulshrestha, U. Deposition and Mineralogical Characteristics of Atmospheric Dust in relation to Land Use and Land Cover Change in Delhi (India). Geogr. J. 2014, 2014. [Google Scholar] [CrossRef]
- Kiselev, D.; Matsvay, A.; Abramov, I.; Dedkov, V.; Shipulin, G.; Khafizov, K. Current Trends in Diagnostics of Viral Infections of Unknown Etiology. Viruses 2020, 12, 211. [Google Scholar] [CrossRef]
- United States Department of Labor Occupational Safety and Health Administration. Dentistry Workers and Employers. 2020. Available online: https://www.osha.gov/SLTC/covid-19/dentistry.html (accessed on 14 December 2020).
- Harrel, S.K.; Molinari, J. Cover story, Aerosols and splatter in dentistry, A brief review of the literature and infection control implications. Clinical Practice. JADA 2004, 135, 429–437. [Google Scholar] [CrossRef]
- Abichandani, S.; Nadige, R. Cross contamination in dentistry: A comprehensive overview. J. Educ. Ethics Dent. 2012, 2, 3–9. [Google Scholar] [CrossRef]
- Merte, J.L.; Kroll, C.M.; Collins, A.S.; Melnick, A.L. An epidemiologic investigation of occupational transmission of Mycobacterium tuberculosis infection to dental health care personnel. Infection prevention and control implications. JADA 2014, 145, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Zemouri, C.; Awad, S.F.; Volgenant, C.M.C.; Crielaard, W.; Laheij, A.M.G.A.; De Soet, J.J. Modeling of the Transmission of Coronaviruses, Measles Virus, Influenza Virus, Mycobacterium tuberculosis, and Legionella Pneumophila in dental clinics. J. Dent. Res. 2020, 99, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Jimenez, J.L. Exhaled CO2 as COVID-19 infection risk proxy for different indoor environments and activities. MedRxiv 2020, 1–9. [Google Scholar] [CrossRef]
- Plog, J.; Wu, J.; Dias, Y.J.; Mashayek, F.; Cooper, L.F.; Yarin, A.L. Reopening dentistry after COVID-19: Complete suppression of aerosolization indental procedures by viscoelastic Medusa Gorgo. Phys. Fluids 2020, 32, 083111. [Google Scholar] [CrossRef]
- Wallace, L.A. The Total Exposure Assessment Methodology (TEAM) Study: Summary and Analysis; Environmental Protection Agency (EPA): Washington, DC, USA, 1987. Available online: https://nepis.epa.gov/Exe/ZyPDF.cgi/2000UC5T.PDF?Dockey=2000UC5T.PDF (accessed on 14 December 2020).
- Cincinelli, A.; Martellini, T. Editorial Indoor Air Quality and Health. Int. J. Environ. Res. Public Health 2017, 14, 1286. [Google Scholar] [CrossRef]
- Volgenant, C.M.C.; Persoon, I.F.; De Ruijter, R.A.G.; De Soet, J.J.H. Infection control in dental health care during and after the SARS-CoV-2 outbreak. Oral Dis. 2020, 1–10. [Google Scholar] [CrossRef]
- Shandilya, K.K.; Khare, M. Particulate Matter: Sources, Emission Rates and Health Effects. In Environmental and Agricultural Researcher Biographical Sketches and Research Summaries, Environmental Research Advances, 1st ed.; Cacioppo, L.T., Ed.; Nova Science Publishers: Hauppauge, NJ, USA, 2014; Volume 1, pp. 305–306. [Google Scholar]
- Massey, D.; Kulshrestha, A.; Masih, J.; Taneja, A.B.E.J. Seasonal trends of PM 10, PM 5.0, PM 2.5 & PM 1.0 in indoor and outdoor environments of residential homes located in North-Central India. Build. Environ. 2012, 47, 223–231. [Google Scholar] [CrossRef]
- Alberdi, E.; Alvarez, I.; Hernández, H.; Oyarbide-Zubillaga, A.; Goti, A. Analysis of the Air Quality of the Basque Autonomous Community Using Spatial Interpolation. Sustainability 2020, 12, 4164. [Google Scholar] [CrossRef]
- Urrutia, K.; Stendorf, S.; Molina, P.; Flores, I. Smart zero carbon city: Key factors towards smart urban decarbonization. DYNA 2019, 94, 676–683. [Google Scholar] [CrossRef]
- Muleski, G.E.; Cowherd, C., Jr.; Kinsey, J.S. Particulate Emissions from Construction Activities. J. Air Waste Manag. Assoc. 2005, 55, 772–783. [Google Scholar] [CrossRef]
- Chang, L.T.C.; Scorgie, Y.; Duc, H.N.; Monk, K.; Fuchs, D.; Trieu, T. Major Source Contributions to Ambient PM2.5 and Exposures within the New SouthWales Greater Metropolitan Region. Atmosphere 2019, 10, 138. [Google Scholar] [CrossRef]
- Xue, H.; Liu, G.; Zhang, H.; Hu, R.; Wang, X. Similarities and differences in PM10 and PM2.5 concentrations, chemical compositions and sources in Hefei City, China. Chemosphere 2019, 220, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Air Quality Standards, European Commission; Ambient Air Quality Standards (GB3095-2012), Ministry of Environmental Protection and General Administration of Quality Supervision, Inspection and Quarantine of China. 2012. Available online: http://english.mee.gov.cn/Resources/standards/Air_Environment/quality_standard1/201605/t20160511_337502.shtml (accessed on 5 August 2020).
- WHO. Household Air Pollution and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 5 August 2020).
- Sarafraz, M.; Sadani, M.; Teimouri, F. Indoor Aerosols: A Serious Threat for Human Health. J. Environ. Health Sustain. Dev. 2018, 3, 488–491. [Google Scholar]
- Schieweck, A.; Uhde, E.; Salthammer, T.; Salthammer, L.C.; Morawska, L.; Mazaheri, M.; Kumar, P. Smart homes and the control of indoor air quality. Renew. Sustain. Energ. Rev. 2018, 94, 705–718. [Google Scholar] [CrossRef]
- Destaillats, H.; Maddalena, R.L.; Singer, B.C.; Hodgson, A.T.; Mc Kone, T.E. Indoor pollutants emitted by office equipment: A review of reported data and information needs. Atmos. Environ. 2008, 42, 1371–1388. [Google Scholar] [CrossRef]
- De Gennaro, G.; Dambruoso, P.R.; Loiotile, A.D.; Di Gilio, A.; Giungato, P.; Tutino, M.; Marzocca, A.; Mazzone, A.; Palmisani, J.; Porcelli, F. Indoor air quality in schools. Environ. Chem. Lett. 2014, 12, 467–482. [Google Scholar] [CrossRef]
- European Committee for Standardization (CEN). UNE EN 12341:2015. Ambient Air. In Standard Gravimetric Measurement Method for the Determination of the PM10 and PM2.5 Mass Concentration of Suspended Particulate Matter; European Committee for Standardization: Brussel, Belgium, 2015; Available online: https://standards.iteh.ai/catalog/standards/cen/7ad508ad-33bd-4e41-942b-c52ddeb6d44d/en-12341-2014, (accessed on 5 August 2020).
- Environmental Protection Agency (EPA). Environmental Hazards in the Home; Environmental Protection Agency (EPA): Washington, DC, USA, 2016. Available online: http://library.hsh.com/articles/homeowners-repeat-buyers/environmental-hazards-in-the-home/ (accessed on 5 August 2020).
- Park, M.; Joo, H.S.; Lee, K.; Jang, M.; Kim, S.D.; Kim, I.; Borlaza, L.J.S.; Lim, H.; Shin, H.; Chung, K.H.; et al. Differential toxicities of fine particulate matters from various sources. Sci. Rep. 2018, 8, 17007–17018. [Google Scholar] [CrossRef]
- Brown, J.S.; Gordon, T.; Price, O.; Asgharian, B. Thoracic and respirable particle definitions for human health risk assessment. Part. Fibre Toxicol. 2013, 10, 12–24. [Google Scholar] [CrossRef]
- Hamra, G.B.; Guha, N.; Cohen, A.; Laden, F.; Raaschou-Nielsen, O.; Samet, J.M.; Vineis, P.; Forastiere, F.; Saldiva, P.; Yorifuji, T.; et al. Outdoor Particulate Matter Exposure and Lung Cancer: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2014, 122, 906–911. [Google Scholar] [CrossRef]
- Brauer, M.; Amann, M.; Burnett, R.T.; Cohen, A.; Dentener, F.; Ezzati, M.; Henderson, S.B.; Krzyzanowski, M.; Martin, R.V.; Van Dingenen, R.; et al. Exposure assessment for estimation of the global burden of disease attributable to outdoor air pollution. Environ. Sci Technol. 2012, 46, 652–660. [Google Scholar] [CrossRef]
- Jia, Y.Y.; Wang, Q.; Liu, T. Toxicity Research of PM2.5 Compositions in Vitro. Int. J. Environ. Res. Public Health 2017, 14, 232. [Google Scholar] [CrossRef] [PubMed]
- Burnett, R.T.; Pope III, C.A.; Ezzati, M.; Olives, C.; Lim, S.S.; Mehta, S.; Shin, H.H.; Singh, G.; Hubbell, B.; Brauer, M.; et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ. Health Perspect. 2014, 122, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, J.; Klingmueller, K.; Pozzer, A.; Pöschl, U.; Fnais, M.; Daiber, A.; Münzel, T. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur. Heart J. 2019, 40, 1590–1596. [Google Scholar] [CrossRef]
- Pozzer, A.; Dominici, F.; Haines, A.; Witt, C.; Münzel, T.; Lelieveld, J. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc. Res. 2020, 116, 2247–2253. [Google Scholar] [CrossRef]
- Contini, D.; Costabile, F. Does air pollution influence COVID-19 outbreaks? Atmosphere 2020, 11, 377. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.R.; Zhu, Y.; Li, B.; Huang, C.L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef]
- Lelieveld, J.; Pozzer, A.; Pöschl, U.; Fnais, M.; Haines, A.; Münzel, T. Comparison of mortality from ambient air pollution with other risk factors: A worldwide perspective. Cardiovasc. Res. 2020, 116, 1910–1917. [Google Scholar] [CrossRef]
- Miller, M.R. Oxidative stress and the cardiovascular effects of air pollution. Free Radic. Biol. Med. 2020, 151, 69–87. [Google Scholar] [CrossRef]
- Meng, Q.Y.; Turpin, B.J.; Korn, L.; Weisel, C.P.; Morandi, M.; Colome, S.; Zhang, J.; Stock, T.; Spektor, D.; Winer, A. Influence of ambient (outdoor) sources on residential indoor and personal PM2.5 concentrations: Analyses of RIOPA data. J. Expo. Sci. Environ. Epidemiol. 2005, 15, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Chatoutsidou, S.E.; Ondráček, J.; Tesar, O.; Tørseth, K.; Ždímal, V.; Lazaridis, M. Indoor/outdoor particulate matter number and mass concentration in modern offices. Build. Environ. 2015, 92, 462–474. [Google Scholar] [CrossRef]
- Jeričević, A.; Gašparac, G.; Mikulec, M.M.; Kumar, P.; Prtenjak, M.T. Identification of diverse air pollution sources in a complex urban area of Croatia. J. Environ. Manag. 2019, 243, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Moreno, T.; Trechera, P.; Querol, X.; Lah, R.; Johnson, D.; Wrana, A.; Williamson, B. Trace element fractionation between PM10 and PM2.5 in coal mine dust: Implications for occupational respiratory health. Int. J. Coal Geol. 2019, 203, 52–59. [Google Scholar] [CrossRef]
- Cullinan, P. Occupation and chronic obstructive pulmonary disease (COPD). Br. Med. Bull. 2012, 104, 143–161. [Google Scholar] [CrossRef] [PubMed]
- Khan, R.K.; Mark, A. Strand Road dust and its effect on human health: A literature review. Epidemiol. Health 2018, 40, e2018013. [Google Scholar] [CrossRef]
- Berger, U.; Karatzas, K.; Jaeger, S.; Voukantsis, D.; Sofiev, M.; Brandt, O.; Zuberbier, T.; Bergmann, K.C. Personalized pollen-related symptom-forecast information services for allergic rhinitis patients in Europe. Allergy 2013, 68, 963–965. [Google Scholar] [CrossRef]
- Weinhold, B. A Spreading Concern: Inhalational Health Effects of Mold. Environ. Health Perspect. 2007, 115, A300–A305. [Google Scholar] [CrossRef]
- Acevedo, N.; Zakzuk, J.; Caraballo, L. House Dust Mite Allergy Under Changing Environments Allergy Asthma. Immunol. Res. 2019, 11, 450–469. [Google Scholar] [CrossRef]
- Wang, H.; Wei, C.-X.; Min, L.; Zhu, L.-Y. Good or bad: Gut bacteria in human health and diseases. Biotechnol. Biotechnol. Equip. 2018, 32, 1075–1080. [Google Scholar] [CrossRef]
- Woolhouse, M.; Scott, F.; Hudson, Z.; Howey, R.; Chase, M. Topping Human viruses: Discovery and emergence. Philos. Trans. R. Soc. B Biol. Sci. 2012, 367, 2864–2871. [Google Scholar] [CrossRef] [PubMed]
- Hommi, Y.B.S.; Abdelaziz, M.S.; Ahmad, H.G. Effect of Occupational Cement Dust Pollution on The Respiratory Epithelium in Amran Cement Factory. J. Sci. Technol. 2013, 15, 25–32. [Google Scholar] [CrossRef]
- Kurda, R.; Silvestre, J.D.; De Brito, J. Toxicity and environmental and economic performance of fly ash and recycled concrete aggregates use in concrete: A review. Heliyon 2018, 4, 1–45. [Google Scholar] [CrossRef] [PubMed]
- Svedahl, S.; Svendsen, K.; Qvenild, T.; Sjaastad, A.K.; Hilt, B. Short term exposure to cooking fumes and pulmonary function. J. Occup. Med. Toxicol. 2009, 4, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.E.; Hoffmann, P.; Scheffran, J. Health impacts of smog pollution: The human dimensions of exposure. Lancet Planet. Health 2017, 1, E132–E133. [Google Scholar] [CrossRef]
- Bellisario, V.; Piccioni, P.; Bugiani, M.; Squillacioti, G.; Levra, S.; Gulotta, C.; Mengozzi, G.; Perboni, A.; Grignani, E.; Bono, R. Tobacco Smoke Exposure, Urban and Environmental Factors as Respiratory Disease Predictors in Italian Adolescents. Int. J. Environ. Res. Public Health 2019, 16, 4048. [Google Scholar] [CrossRef]
- Niranjan, R.; Thakur, A.K. The Toxicological Mechanisms of Environmental Soot (Black Carbon) and Carbon Black: Focus on Oxidative Stress and Inflammatory Pathways. Front. Immunol. 2017, 8, 1–20. [Google Scholar] [CrossRef]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef]
- Riediker, M.; Zink, D.; Kreyling, W.; Oberdörster, G.; Elder, A.; Graham, U.; Lynch, I.; Duschl, A.; Ichihara, G.; Ichihara, S.; et al. Particle toxicology and health—Where are we? Part. Fibre Toxicol. 2019, 16, 19–52. [Google Scholar] [CrossRef]
- Abelsohn, A.; Stieb, D.M. Health effects of outdoor air pollution: Approach to counselling patients using the Air Quality Health Index. Can. Fam. Physician 2011, 57, 881–887. [Google Scholar]
- Peraica, M.; Radic, B.; Lucic, A.; Pavlovic, M. Toxic effects of mycotoxins in humans. Bull. World Health Organ. 1999, 77, 754–766. [Google Scholar] [PubMed]
- Kim, H.S.; Kim, Y.J.; Seo, Y.R. An Overview of Carcinogenic Heavy Metal: Molecular Toxicity Mechanism and Prevention. J. Cancer Prev. 2015, 20, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Brocklehurst, P.; Ashley, J.; Tickle, M. Patient assessment in general dental practice—Risk assessment or clinical monitoring? Br. Dent. J. 2011, 210, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Moraru, R.I.; Babut, G.B.; Cioca, L.I. Rationale and criteria development for risk assessment tool selection in work environments. Environ. Eng. Manag. J. 2014, 13, 1371–1376. [Google Scholar] [CrossRef]
- Cioca, L.I.; Moraru, R.I.; Băbuţ, G.B. A framework for organisational characteristic assessment and their influences on safety and health at work. In Proceedings of the 15th International Scientific Conference the Knowledge Based Organization: Management, Land Forces Academy, Sibiu, Romania, 26–28 November 2009; Volume 2, pp. 43–48. [Google Scholar]
- Helmis, C.G.; Tzoutzas, J.; Flocas, H.A.; Halios, C.H.; Stathopoulou, O.I.; Assimakopoulos, V.D.; Panis, V.; Apostolatou, M.; Sgouros, G.; Adam, E. Indoor air quality in a dentistry clinic. Sci. Total Environ. 2007, 377, 349–365. [Google Scholar] [CrossRef]
- Demetrescu, I.; Luca, R.; Ionita, D.; Prodana, M. Evaluation of heavy metals of temporary teeth from areas with different pollution level. Mol. Cryst. Liq. Cryst. 2010, 523, 73–81. [Google Scholar] [CrossRef]
- Bo, M.; Salizzoni, P.; Clerico, M.; Buccolieri, R. Assessment of Indoor-Outdoor Particulate Matter Air Pollution: A Review. Atmosphere 2017, 8, 136. [Google Scholar] [CrossRef]
- Anjum, A.; Hosein, M.; Butt, S.A.; Fakhuruddin. Cross Infection in Dentistry and the Dental Aerosols—A Potential Health Hazard. Pak. J. Med. Dent. 2020, 9, 70–75. [Google Scholar]
- Azari, M.; Ghadjari, A.; Massoudinejad, M.; Nasiree, N.F. Airborne Microbial Contamination of Dental Units. Tanaffos 2008, 7, 4–57. [Google Scholar]
- Bhuvaneswari, P. Aerosols-A concern for dentists. Res. J. Pharm Technol. 2014, 7, 938–941. [Google Scholar]
- Raja, K.; Tilak, A.H. Occupational hazards in dentistry and its control measure—A review. World J. Pharm. Pharm. Sci. 2014, 3, 397–415. [Google Scholar]
- Soaita, C. Identifying occupational riscks in dentistry. Proc. Technol. 2014, 12, 558–565. [Google Scholar] [CrossRef][Green Version]
- Bruzell, R.E.M.; Jacobsen, N.; Hensten-Pettersen, A. Health hazards associated with curing light in the dental clinic. Clin. Oral Investig. 2004, 8, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Mojarad, F.; Massum, T.; Samavat, H. Noise Levels in Dental Offices and Laboratories in Hamedan, Iran. J. Dent. 2009, 6, 181–185. [Google Scholar]
- Pîrvu, C.; Pătraşcu, I.; Pîrvu, D.; Ionescu, C. The dentist’s operating posture—Ergonomic aspects. J. Med. Life 2014, 7, 177–182. [Google Scholar] [PubMed]
- Ayatollahi, J.; Ayatollahi, F.; Ardekani, A.M.; Bahrololoomi, R.; Ayatollahi, J.; Ayatollahi, A.; Owlia, M.B. Occupational hazards to dental staff. Dent. Res. J. 2012, 9, 2–7. [Google Scholar] [CrossRef]
- Yoo, Y.J.; Kwak, E.J.; Jeong, K.M.; Baek, S.H.; Baek, Y.S. Knowledge, attitudes and practices regarding methicillin-resistant Staphylococcus aureus (MRSA) infection control and nasal MRSA carriage rate among dental health-care professionals. Int. Dent. J. 2018, 68, 359–366. [Google Scholar] [CrossRef]
- Zemouri, C.; De Soet, H.; Crielaard, W.; Laheij, A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS ONE 2017, 12, e0178007. [Google Scholar] [CrossRef]
- Singh, A.; Manjunath, R.S.; Singla, D.; Bhattacharya, H.S.; Sarkar, A.; Chandra, N. Aerosol, a health hazard during ultrasonic scaling: A clinico-microbiological study. Indian J. Dent. Res. 2016, 27, 160–162. [Google Scholar] [CrossRef]
- Kobza, J.; Pastuszka, J.; Brągoszewska, E. Do exposures to aerosols pose a risk to dental professionals? Occup. Med. 2018, 68, 454–458. [Google Scholar] [CrossRef]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Sambri, V.; Prati, C. Risks of Aerosol Contamination in Dental Procedures during the Second Wave of COVID-19—Experience and Proposals of Innovative IPC in Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 8954. [Google Scholar] [CrossRef] [PubMed]
- Ge, Z.Y.; Yang, L.M.; Xia, J.J.; Fu, X.H.; Zhang, Y.Z. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J. Zhejiang Univ. 2020, 21, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Volgenant, C.; De Soet, J. Cross-transmission in the dental office: Does this make you ill? Curr. Oral Health Rep. 2018, 5, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Ramich, T.; Eickholz, P.; Wicker, S. Work-related infections in dentistry: Risk perception and preventive measures. Clin. Oral Investig. 2017, 21, 2473–2479. [Google Scholar] [CrossRef]
- Holloman, J.L.; Mauriello, S.M.; Pimenta, L.; Arnold, R.R. Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. J. Am. Dent. Assoc. 2015, 146, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, D.; Juluri, R.; Srihari, J.; Viswanathan, V. Comparing the efficacy of two mouth rinses in reducing bacterial aerosol contamination. J. Dent. Oral Health 2017, 4, 1–4. [Google Scholar]
- Sawhney, A.; Venugopal, S.; Babu, G.R.; Garg, A.; Mathew, M.; Yadav, M.; Gupta, B.; Tripathi, S. Aerosols how dangerous they are in clinical practice. J. Clin. Diagn. Res. 2015, 9, ZC52–ZC57. [Google Scholar] [CrossRef]
- Zadeh, A.N.; Dufresne, A. Chemical Hazards in Dental Laboratories. Indoor Built. Environ. 1998, 7, 146–155. [Google Scholar] [CrossRef]
- Fasunloro, A.; Owotade, F.J. Occupational hazards among clinical dental staff. J. Contemp. Dent. Pract. 2004, 5, 134–152. [Google Scholar] [CrossRef]
- Prashant, B.; Firoza, S.; Jaiswal, J.N.; Bansal, A. Occupational hazards among dentists: A review of literature. J. Int. Med. Dent. Res. 2011, 4, 87–93. [Google Scholar]
- Leggat, P.A.; Kedjarune, U.; Smith, D.R. Occupational Health Problems in Modern Dentistry: A Review. Ind. Health 2007, 45, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Rustemeyer, T.; Frosch, P.J. Occupational Contact Dermatitis in Dental Personnel. Kanerva’s Occup. Dermatol. 2020, 1879–1890. [Google Scholar] [CrossRef]
- Zhang, X.; Wei, L.C.; Wu, B.; Yu, L.Y.; Wang, X.P.; Liu, Y. A comparative analysis of metal allergens associated with dental alloy prostheses and the expression of HLA-DR in gingival tissue. Mol. Med. Rep. 2016, 13, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, B.W.; Jensen, E.P.H.; Örtengren, U.; Michelsen, V.B. Airborne exposure to gaseous and particle-associated organic substances in resin-based dental materials during restorative procedures. Eur. J. Oral Sci. 2019, 127, 1–10. [Google Scholar] [CrossRef]
- Polednik, B. Aerosol and bioaerosol particles in a dental office. Environ. Res. 2014, 134, 405–409. [Google Scholar] [CrossRef]
- Okamoto, M.; Tominaga, M.; Shimizu, S.; Yano, C.; Masuda, K.; Nakamura, M.; Zaizen, Y.; Nouno, T.; Sakamoto, S.; Yokoyama, M.; et al. Dental Technicians’ Pneumoconiosis. Intern. Med. 2017, 56, 3323–3326. [Google Scholar] [CrossRef]
- Inayati, E.; Salim, S.; Harwasih, S.; Indiani, S.R. Levels of crystalline silica dust in dental laboratorium of Dental Health Technology. Dent. J. 2015, 48, 183–187. [Google Scholar] [CrossRef][Green Version]
- Barnes, H.; Goh, N.S.L.; Leong, T.L.; Hoy, R. Silica-associated lung disease: An old-world exposure in modern industries. Respirology 2019, 24, 1165–1175. [Google Scholar] [CrossRef]
- Torres, P.P.T.S.; Marchiori, E.; Pinto, S.A.; Rabahi, M.F. Wood charcoal dust pneumoconiosis. Rev. Port. Pneumol. 2017, 23, 233–234. [Google Scholar] [CrossRef]
- Astudillo, L.; Sailler, L.; Ecoiffier, M.; Giron, J.; Couret, B.; Arlet-Suau, E. Exposure to silica and primary Sjögren’s syndrome in a dental technician. Rheumatology 2003, 42, 1268–1269. [Google Scholar] [CrossRef]
- WHO. IARC Monographs on the Identification of Carcinogenic Hazards to Humans. 2020. Available online: https://monographs.iarc.fr/ (accessed on 5 August 2020).
- Singh, T.; Bello, B.; Jeebhay, M. Risk factors associated with asthma phenotypes in dental healthcare workers. Am. J. Ind. Med. 2013, 56, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Tarlo, S.M. Occupational exposures and adult asthma. Immunol. Allergy Clin. 2008, 28, 563–576. [Google Scholar] [CrossRef] [PubMed]
- Lugović-Mihić, L.; Ferček, I.; Duvančić, T.; Bulat, V.; Ježovita, J.; Novak-Bilić, G.; Šitum, M. Occupational contact dermatitis amongst dentists and dental technicians. Acta Clin. Croat. 2016, 55, 293–300. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rai, R.; Dinakar, D.; Kurian, S.S.; Bndoo, Y.A. Investigation of contact allergy to dental materials by patch testing. Indian Derm. Online J. 2014, 5, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Aalto-Korte, K.; Alanko, K.; Kuuliala, O.; Jolanki, R. Methacrylate and acrylate allergy in dental personnel. Contact Dermat. 2007, 57, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Donaghy, M.; Rushworth, G.; Jacobs, J.M. Generalized peripheral neuropathy in a dental technician exposed to methyl methacrylate monomer. Neurology 1991, 41, 1112–1116. [Google Scholar] [CrossRef]
- Sakzewski, L.; Naser-ud-Din, S. Work-related musculoskeletal disorders in dentists and orthodontists: A review of the literature. Work 2014, 48, 37–45. [Google Scholar] [CrossRef]
- Jirau-Colón, H.; González-Parrilla, L.; Martinez-Jiménez, J.; Adam, W.; Jiménez-Velez, B. Rethinking the Dental Amalgam Dilemma: An Integrated Toxicological Approach. Int. J. Environ. Res. Public Health 2019, 16, 1036. [Google Scholar] [CrossRef]
- Hakovirta, M.; Denuwara, N. How COVID-19 Redefines the Concept of Sustainability. Sustainability 2020, 12, 3727. [Google Scholar] [CrossRef]
- Cioca, L.I.; Moraru, R.L.; Băbuţ, G.B.; Ungureanu, N.S. Integrating Risk Analysis with Safety Dyagnostic In Complex Industrial Systems: Modeling Hazard. Acta Univ. Cibiniensis 2015, 66. [Google Scholar] [CrossRef][Green Version]
| Indicator | Category | India Outdoor | India Indoor | Observations |
|---|---|---|---|---|
| PM2.5 μg m−3 | Annual average concentration 2012 | 160 | 161 | Health effects on occupants of the houses with a higher concentration level of both PM2.5 and PM10 were more aggressive |
| PM10 μg m−3 | Annual average concentration 2012 | 255 | 247 |
| Contaminants | Aerodynamic Diameter (μm) | Health Effects of Air Pollution from Particulate Matter | |
|---|---|---|---|
| Suspended atmospheric dust | 0.005–1 | Chronic obstructive pulmonary disease [63,64] |
| Setting dust | 1–100 | Respiratory and heart diseases depending on a.d. size [65] | |
| Pollen | 10–100 | Asthma, rhinitis, and allergic conjunctivitis [66] |
| Mold spores | 8–80 | Sneezing, watery eyes, and asthma [67] | |
| House dust | 0.1–10 | Asthma rhinitis and others [68] | |
| Bacteria | 0.05–10 | Various good and bad effects [69] | |
| Viruses | 0.05–0.5 | 219 species inducing various diseases [20,70] | |
| Cement dust | 0.5–100 | Respiratory diseases [71] |
| Fly ash | 1–100 | Respiratory effects [72] | |
| Oil smoke | 0.05–0.7 | Affect respiratory system; after long exposure, organs can be affected [73] | |
| Smog | 0.01–1.2 | Respiratory diseases [74] | |
| Tobacco smoke | 0.01–1 | Heart and lung disease, stroke, diabetes, and chronic pulmonary disease [75] | |
| Soot | 0.01–0.5 | Inflammatory pulmonary pathway [76] | |
| Potential Hazard Due to Indoor Air Pollution | Control Methods | |
|---|---|---|
| 1 | Exposure to respiratory disease through airborne transmission | Employee training to use respiratory protective equipment and apply appropriate cleaning routines |
| 2 | Exposure to environmental biological contaminants from ventilation systems | Periodic cleaning of ventilation systems in order to detect and remove the mold |
| 3 | Exposure to respiratory infectious disease through droplet transmission | Using appropriate medical protection equipment (gloves, glasses, and masks) |
| 4 | Exposure to disinfectants and cleaning agents in routine cleaning activities | Strict schedule for well-maintained ventilation |
| 5 | Exposure to metal or silica components in working materials | Disposal and replacement with an equivalent product Ensuring local exhaust ventilation |
| 6 | Exposure to freshener products | Replace the air fresheners and sprays with products that contain less harmful chemicals |
| 7 | Exposure to mercury from mercury-containing amalgams | Replacing mercury-containing products with some less harmful equivalents |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cocârţă, D.M.; Prodana, M.; Demetrescu, I.; Lungu, P.E.M.; Didilescu, A.C. Indoor Air Pollution with Fine Particles and Implications for Workers’ Health in Dental Offices: A Brief Review. Sustainability 2021, 13, 599. https://doi.org/10.3390/su13020599
Cocârţă DM, Prodana M, Demetrescu I, Lungu PEM, Didilescu AC. Indoor Air Pollution with Fine Particles and Implications for Workers’ Health in Dental Offices: A Brief Review. Sustainability. 2021; 13(2):599. https://doi.org/10.3390/su13020599
Chicago/Turabian StyleCocârţă, Diana Mariana, Mariana Prodana, Ioana Demetrescu, Patricia Elena Maria Lungu, and Andreea Cristiana Didilescu. 2021. "Indoor Air Pollution with Fine Particles and Implications for Workers’ Health in Dental Offices: A Brief Review" Sustainability 13, no. 2: 599. https://doi.org/10.3390/su13020599
APA StyleCocârţă, D. M., Prodana, M., Demetrescu, I., Lungu, P. E. M., & Didilescu, A. C. (2021). Indoor Air Pollution with Fine Particles and Implications for Workers’ Health in Dental Offices: A Brief Review. Sustainability, 13(2), 599. https://doi.org/10.3390/su13020599









