PARO as a Biofeedback Medical Device for Mental Health in the COVID-19 Era
Abstract
:1. Introduction
2. PARO as a Biofeedback Medical Device
2.1. What Is PARO
2.2. Clinical Evidence of the Benefits and Barriers of PARO
2.2.1. Benefit 1: Reducing Negative Emotion and Behavioral Symptoms
2.2.2. Benefit 2: Improving Social Engagement
2.2.3. Benefit 3: Promoting Positive Mood and Quality of Care Experience
2.2.4. Barrier 1: Cost and Workload
2.2.5. Barrier 2: Infection Control
2.2.6. Barrier 3: Stigma and Ethical Issues
2.3. Integration of PARO in the Medical and Welfare Systems in the World
2.3.1. Medical and Welfare Systems in Denmark
2.3.2. Medical and Welfare Systems in the U.S.
2.3.3. Medical and Welfare Systems in Hong Kong, France, Singapore, Australia and Japan
2.4. Cleaning Protocols for Infection Prevention and Control (IPC)
3. Practical Uses of PARO in the New Lifestyle under COVID-19
3.1. Continued Use of PARO in the U.S.
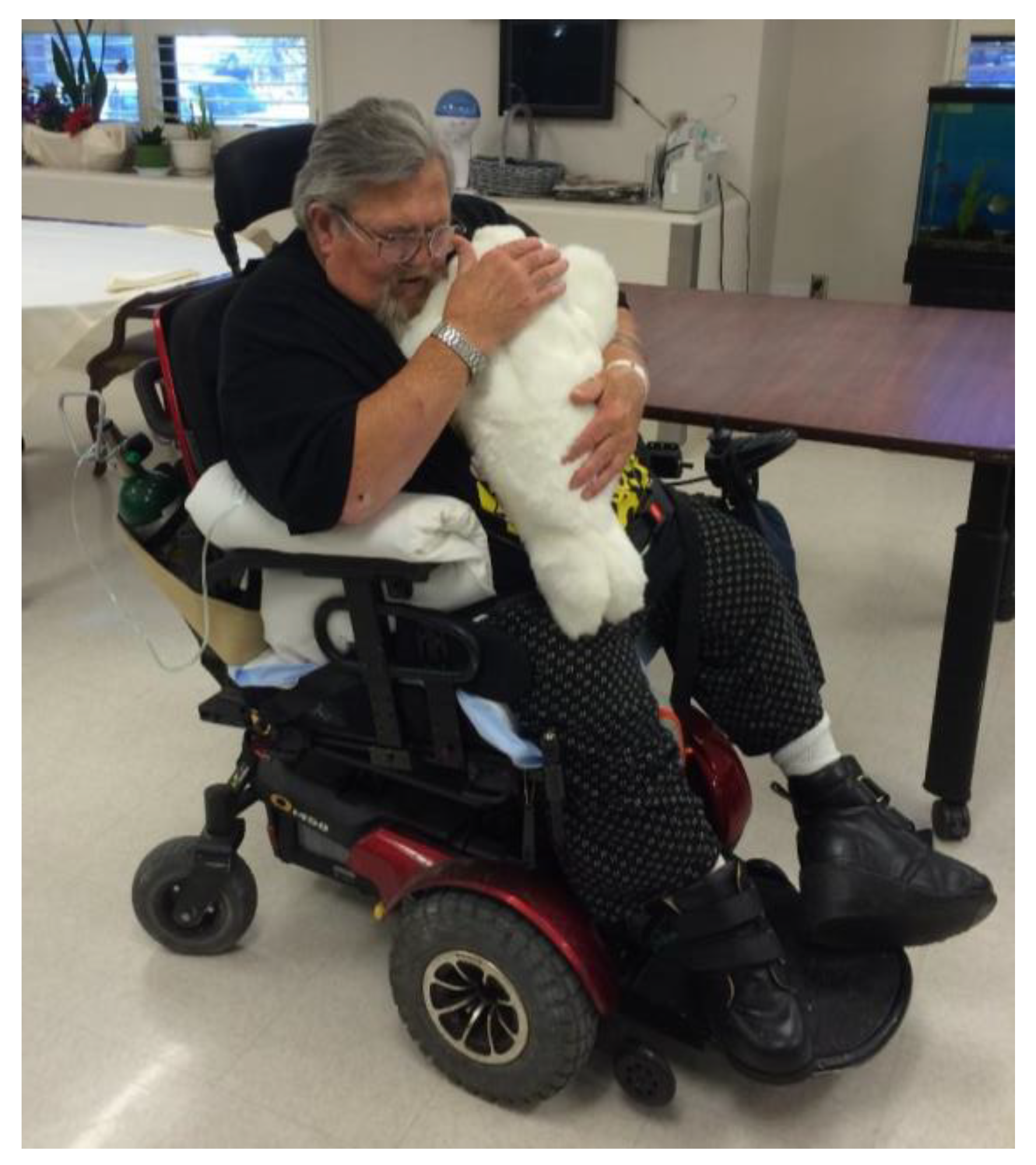
3.1.1. Continued Use of PARO in Home Health Services and Institutional Medical Services
3.1.2. Continued Use of PARO at Long-Term Care Facilities (Case 1)
3.1.3. Continued Use of PARO at Long-Term Care Facilities (Case 2)
3.2. Continued Use of PARO in Japan in At-Home Care of Parents with Dementia
3.3. New Installments of PARO in Australia for Home Care at “Community Living”
3.4. Using PARO for a Resident with Mild Dementia at a Nursing Home in Japan
3.5. PARO in the Acute Frailty Unit of the Chelsea and Westminster Hospital NHS Foundation Trust in the UK
3.6. Registered Nurse for ICU Uses PARO for Emotional Support
3.7. PARO for Mental Health Care for Telephone Counselors at Public Health Center, Toshima City, Tokyo in Japan
4. Discussion and Conclusions
4.1. PARO in the COVID-19 Pandemic
- Social distancing,
- Restriction of living areas (prohibition of outings and restriction of outside visits),
- Restriction of services (closed facilities, limited human contact),
- Rigorous infectious disease prevention and control,
- Dementia progression (effects of isolation, worsening of anxiety and depression, and behavioral issues caused by restrictions),
- Post-coronavirus pandemic disorders (PTSD, pain, anxiety, depression, etc.).
4.2. PARO in the Digital Era
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ranieri, J.; Guerra, F.; Angione, A.L.; Di Giacomo, D.; Passafiume, D. Cognitive Reserve and Digital Confidence among Older Adults as New Paradigm for Resilient Aging. Gerontol. Geriatr. Med. 2021, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.-Z.; Nelson, B.J.; Murphy, R.R.; Choset, H.; Christensen, H.; Collins, S.H.; Dario, P.; Goldberg, K.; Ikuta, K.; Jacobstein, N.; et al. Combating COVID-19—The role of robotics in managing public health and infectious diseases. Sci. Robot. 2020, 5, eabb5589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pu, L.; Moyle, W.; Jones, C.; Todorovic, M. The Effectiveness of Social Robots for Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Studies. Gerontologist 2019, 59, e37–e51. [Google Scholar] [CrossRef] [PubMed]
- Scoglio, A.A.; Reilly, E.D.; Gorman, J.A.; Drebing, C. Use of Social Robots in Mental Health and Well-Being Research: Systematic Review. J. Med. Internet Res. 2019, 21, e13322. [Google Scholar] [CrossRef] [PubMed]
- Shibata, T.; Coughlin, J.F. Trends of robot therapy with neurological therapeutic seal robot, PARO. J. Robot Mechatron. 2014, 26, 418–425. [Google Scholar] [CrossRef]
- Hung, L.; Liu, C.; Woldum, E.; Au-Yeung, A.; Berndt, A.; Wallsworth, C.; Horne, N.; Gregorio, M.; Mann, J.; Chaudhury, H. The benefits of and barriers to using a social robot PARO in care settings: A scoping review. BMC Geriatr. 2019, 19, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Shibata, T. Therapeutic Seal Robot as Biofeedback Medical Device: Qualitative and Quantitative Evaluations of Robot Therapy in Dementia Care. Proc. IEEE 2012, 100, 2527–2538. [Google Scholar] [CrossRef]
- Shibata, T.; Inoue, K.; Irie, R. Emotional robot for intelligent system-artificial emotional creature project. In Proceedings of the 5th IEEE International Workshop on Robot and Human Communication. RO-MAN’96 TSUKUBA, Ibaraki, Japan, 11–14 November 1996; pp. 466–471. [Google Scholar]
- Crossman, M.K.; Kazdin, A.E.; Kitt, E.R. The Influence of a Socially Assistive Robot on Mood, Anxiety, and Arousal in Children. Prof. Psychol. Res. Pract. 2018, 49, 48–56. [Google Scholar] [CrossRef]
- Karner, S.; Stenner, H.; Spate, M.; Behrens, J.; Krakow, K. Effects of a robot intervention on visuospatial hemineglect in post-acute stroke patients: A randomized controlled trial. Clin. Rehabil. 2019, 33, 1940–1948. [Google Scholar] [CrossRef]
- Lane, G.W.; Noronha, D.; Rivera, A.; Craig, K.; Yee, C.; Mills, B.; Villanueva, E. Effectiveness of a social robot, “Paro,” in a VA long-term care setting. Psychol Serv. 2016, 13, 292–299. [Google Scholar] [CrossRef]
- Jøranson, N.; Pedersen, I.; Rokstad, A.M.M.; Ihlebaek, C. Change in quality of life in older people with dementia participating in Paro-activity: A cluster-randomized controlled trial. J. Adv. Nurs. 2016, 72, 3020–3033. [Google Scholar] [CrossRef]
- Moyle, W.; Jones, C.; Murfield, J.; Thalib, L.; Beattie, E.R.; Shum, D.H.K.; O’Dwyer, S.; Mervin, M.C.; Draper, B.M. Use of a Robotic Seal as a Therapeutic Tool to Improve Dementia Symptoms: A Cluster-Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2017, 18, 766–773. [Google Scholar] [CrossRef] [Green Version]
- Mervin, M.C.; Moyle, W.; Jones, C.; Murfield, J.; Draper, B.; Beattie, E.; Shum, D.H.; O’Dwyer, S.; Thalib, L. The Cost-Effectiveness of Using PARO, a Therapeutic Robotic Seal, to Reduce Agitation and Medication Use in Dementia: Findings from a Cluster–Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2018, 19, 619–622.e1. [Google Scholar] [CrossRef]
- Moyle, W.; Bramble, M.; Jones, C.; Murfield, J. Care staff perceptions of a social robot called Paro and a look-alike Plush Toy: A descriptive qualitative approach. Aging Ment. Health 2018, 22, 330–335. [Google Scholar] [CrossRef]
- Petersen, S.; Houston, S.; Qin, H.; Tague, C.; Studley, J. The Utilization of Robotic Pets in Dementia Care. J. Alzheimer’s Dis. 2016, 55, 569–574. [Google Scholar] [CrossRef] [Green Version]
- Wada, K.; Shibata, T.; Saito, T.; Tanie, K. Effects of robot-assisted activity for elderly people and nurses at a day service center. Proc. IEEE 2004, 92, 1780–1788. [Google Scholar] [CrossRef]
- Liang, A.; Piroth, I.; Robinson, H.; MacDonald, B.; Fisher, M.; Nater, U.; Skoluda, N.; Broadbent, E. A Pilot Randomized Trial of a Companion Robot for People with Dementia Living in the Community. J. Am. Med. Dir. Assoc. 2017, 18, 871–878. [Google Scholar] [CrossRef]
- Bemelmans, R.; Gelderblom, G.J.; Jonker, P.; de Witte, L. Effectiveness of Robot Paro in Intramural Psychogeriatric Care: A Multicenter Quasi-Experimental Study. J. Am. Med. Dir. Assoc. 2015, 16, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Robinson, H.; MacDonald, B.; Kerse, N.; Broadbent, E. The Psychosocial Effects of a Companion Robot: A Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2013, 14, 661–667. [Google Scholar] [CrossRef] [PubMed]
- The 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention, Hand Hygiene Recommendations: Guidance for Healthcare Providers about Hand Hygiene and COVID-19. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html (accessed on 15 June 2020).
- NHS England, DHSC, PHW, PHA Northern Ireland, HPS, PHE, COVID-19: Guidance for Maintaining Services within Health and Care Settings Infection Prevention and Control Recommendations. 2020. Available online: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control (accessed on 14 July 2021).
- Ienca, M.; Jotterand, F.; Vică, C.; Elger, B. Social and Assistive Robotics in Dementia Care: Ethical Recommendations for Research and Practice. Int. J. Soc. Robot. 2016, 8, 565–573. [Google Scholar] [CrossRef]
- Epley, N.; Waytz, A.; Cacioppo, J.T. On seeing human: A three-factor theory of anthropomorphism. Psychol. Rev. 2007, 114, 864–886. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Nakamura, S.; Sato, M.; Sato, Y.; Ando, N.; Takayama, T.; Fujita, M.; Ishihara, M. Synthesis and Application of Silver Nanoparticles (Ag NPs) for the Prevention of Infection in Healthcare Workers. Int. J. Mol. Sci. 2019, 20, 3620. [Google Scholar] [CrossRef] [Green Version]
- Dodds, P.; Martyn, K.; Brown, M. Infection prevention and control challenges of using a therapeutic robot. Nurs. Older People 2018, 30, 34–40. [Google Scholar] [CrossRef]
- Petersen, S. PARO: An important solution for symptom control. In Proceedings of the 11th Int’l Symp. on Robot Therapy with PARO, Tokyo, Japan, 1 November 2018; pp. 10–14. [Google Scholar]
- Knibbs, K. There’s No Cure for COVID-19 Loneliness, but Robots Can Help. WIRED, 22 June 2020. [Google Scholar]
- Santos, J.; Yoon, J.; Park, D. PARO 6-month Analysis, Front Porch Center for Innovation and Wellbeing. 2016. Available online: http://fpciw.org/wp-content/uploads/sites/15/2016/06/PARO-6-month-analysis-report.pdf (accessed on 12 October 2021).
- Hori, Y.; Omura, F.; Iwahashi, M.; Kato, K.; Sugishita, A.; Shibata, T. Case study on introduction of Paro for family caregivers who take long-distance care and multiple care. In Proceedings of the 11th International Symposium on Robot Therapy with PARO, Tokyo, Japan, 16 December 2019; pp. 33–45. [Google Scholar]
- Cetinkaya, G.; Peumala, C.; Edginton, T.; Mizoguchi, R. Improving the well-being of in-patients within the National Health Service hospital wards using social-robot short interventions. In Proceedings of the 11th Int’l Symp. on Robot Therapy with PARO, Tokyo, Japan, 16 December 2019; pp. 71–72. [Google Scholar]









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shibata, T.; Hung, L.; Petersen, S.; Darling, K.; Inoue, K.; Martyn, K.; Hori, Y.; Lane, G.; Park, D.; Mizoguchi, R.; et al. PARO as a Biofeedback Medical Device for Mental Health in the COVID-19 Era. Sustainability 2021, 13, 11502. https://doi.org/10.3390/su132011502
Shibata T, Hung L, Petersen S, Darling K, Inoue K, Martyn K, Hori Y, Lane G, Park D, Mizoguchi R, et al. PARO as a Biofeedback Medical Device for Mental Health in the COVID-19 Era. Sustainability. 2021; 13(20):11502. https://doi.org/10.3390/su132011502
Chicago/Turabian StyleShibata, Takanori, Lillian Hung, Sandra Petersen, Kate Darling, Kaoru Inoue, Katharine Martyn, Yoko Hori, Geoffrey Lane, Davis Park, Ruth Mizoguchi, and et al. 2021. "PARO as a Biofeedback Medical Device for Mental Health in the COVID-19 Era" Sustainability 13, no. 20: 11502. https://doi.org/10.3390/su132011502
APA StyleShibata, T., Hung, L., Petersen, S., Darling, K., Inoue, K., Martyn, K., Hori, Y., Lane, G., Park, D., Mizoguchi, R., Takano, C., Harper, S., Leeson, G. W., & Coughlin, J. F. (2021). PARO as a Biofeedback Medical Device for Mental Health in the COVID-19 Era. Sustainability, 13(20), 11502. https://doi.org/10.3390/su132011502





