Developing Hospital Emergency and Disaster Management Index Using TOPSIS Method
Abstract
:1. Introduction
2. Hospital Disaster Preparedness Tools and Indices
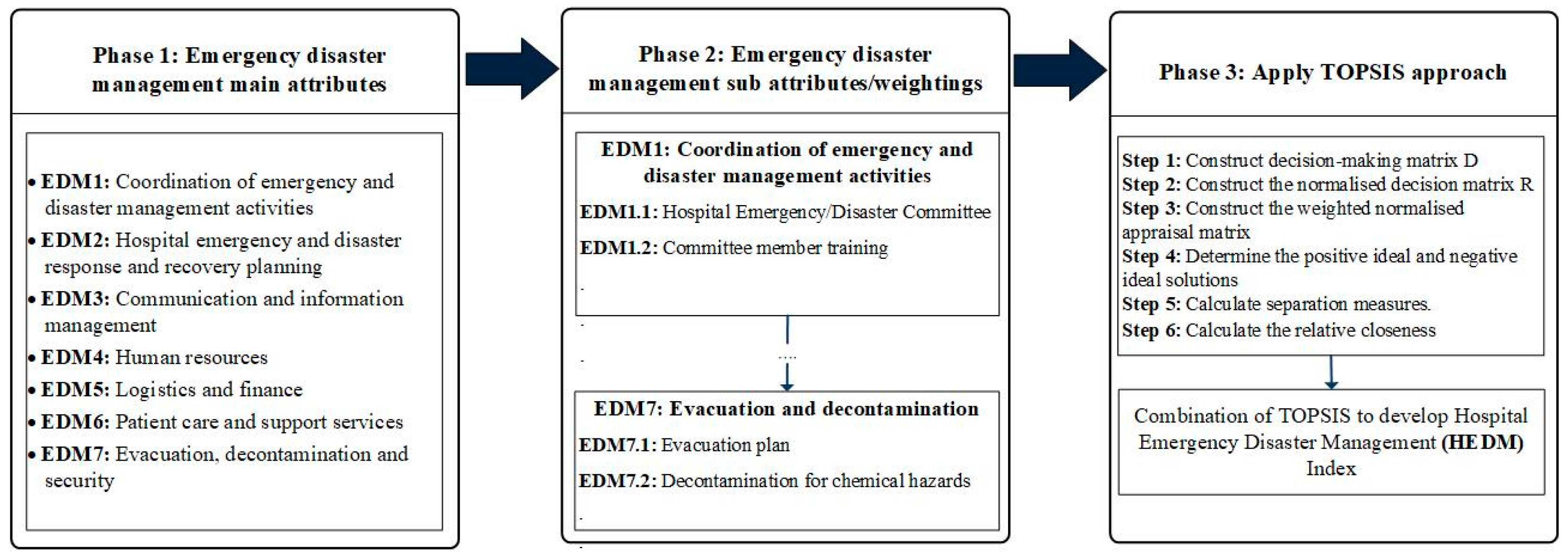
3. Conceptual Framework for Hospital Emergency and Disaster Management Index
- HSI 0–0.35, level C: Urgent intervention measures are needed. The current levels of disaster management measures are not sufficient to protect the lives of patients and hospital staff in disaster events.
- HSI 0.36–0.65, level B: Intervention measures are needed in the short term. Patients, hospital staff, and the hospital’s ability to function during and after emergencies and disasters are potentially at risk.
- HSI 0.66–1, Level A: The hospital situation is normal. However, it is recommended to improve emergency, disaster management capacity and safety level in case of emergencies and disasters.
4. Research Methods
5. Technique for Order of Preference by Similarity to Ideal Solution (TOPSIS)
6. Application of TOPSIS to Indonesian Hospital Emergency and Disaster Management
7. Discussion
- Identifying the most susceptible hospitals which are located in disaster-prone areas.
- Evaluating the disaster and emergency preparedness of hospitals in vulnerable areas. The results can be used to prioritize the allocation of resources and budgeting.
- Implementing disaster risk management proactive measures as needed. Prioritization is necessary for optimum budget allocation.
- Introducing the appropriate solutions for specific local governments to manage disaster risk that is more specific to the related hospitals and to improve the resilience of the hospitals.
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hurlimann, A.; Cobbinah, P.B.; Bush, J.; March, A. Is climate change in the curriculum? An analysis of Australian urban planning degrees. Environ. Educ. Res. 2020, 1–22. [Google Scholar] [CrossRef]
- Aghapour, A.H.; Yazdani, M.; Jolai, F.; Mojtahedi, M. Capacity planning and reconfiguration for disaster-resilient health infrastructure. J. Build. Eng. 2019, 26, 100853. [Google Scholar] [CrossRef]
- Lapčević, Z.; Mandić-Rajčević, S.; Lepić, M.; Jovanović, M. Evaluating a primary healthcare centre’s preparedness for disasters using the hospital safety index: Lessons learned from the 2014 floods in Obrenovac, Serbia. Int. J. Disaster Risk Reduct. 2019, 34, 436–442. [Google Scholar] [CrossRef]
- Chen, C.; Wang, J.; Qiu, F.; Zhao, D. Resilient distribution system by microgrids formation after natural disasters. IEEE Trans. Smart Grid 2015, 7, 958–966. [Google Scholar] [CrossRef]
- World Health Organization. Mass Casualty Management Systems: Strategies and Guidelines for Building Health Sector Capacity; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Nekoie-Moghadam, M.; Kurland, L.; Moosazadeh, M.; Ingrassia, P.L.; Corte, F.D.; Djalali, A. Tools and Checklists Used for the Evaluation of Hospital Disaster Preparedness: A Systematic Review. Disaster Med. Public Health Prep. 2016, 10, 781–788. [Google Scholar] [CrossRef] [PubMed]
- James, E. Getting Ahead of the Next Disaster: Recent Preparedness Efforts in Indonesia. Dev. Pr. 2008, 18, 424–429. [Google Scholar] [CrossRef]
- Zoraster, R.M. Barriers to Disaster Coordination: Health Sector Coordination in Banda Aceh Following the South Asia Tsunami. Prehosp. Disaster Med. 2006, 21, S13–S18. [Google Scholar] [CrossRef]
- Elnashai, A.S.; Kim, S.J.; Yun, G.J.; Sidarta, D. The Yogyakarta Earthquake of 27 May 2006. Available online: http://mae.cee.illinois.edu/publications/reports/Report07–02.pdf (accessed on 30 October 2018).
- United Nations Office for Disaster Risk Reduction. Indonesia Pledges Safety of Over 3000 Schools and 100-Plus Hospitals. Available online: https://www.unisdr.org/archive/14779 (accessed on 21 April 2017).
- Paulik, R.; Gusman, A.; Williams, J.H.; Pratama, G.M.; Lin, S.; Prawirabhakti, A.; Sulendra, K.; Zachari, M.Y.; Fortuna, Z.E.D.; Layuk, N.B.P.; et al. Tsunami Hazard and Built Environment Damage Observations from Palu City after the September 28, 2018 Sulawesi Earthquake and Tsunami. Pure Appl. Geophys. 2019, 176, 3305–3321. [Google Scholar] [CrossRef]
- World Health Organization. Hospital Safety Index: Guide for Evaluators, 2nd ed.; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Sunindijo, R.Y.; Lestari, F.; Wijaya, O. Hospital Safety Index: Assessing the Readiness and Resiliency of Hospitals in Indonesia. Facilities 2019, 38, 39–51. [Google Scholar] [CrossRef]
- Behzadian, M.; Otaghsara, S.K.; Yazdani, M.; Ignatius, J. A state-of-the-art survey of TOPSIS applications. Expert Syst. Appl. 2012, 39, 13051–13069. [Google Scholar] [CrossRef]
- Kaji, A.H.; Lewis, R.J. Assessment of the Reliability of the Johns Hopkins/Agency for Healthcare Research and Quality Hospital Disaster Drill Evaluation Tool. Ann. Emerg. Med. 2008, 52, 204–210. [Google Scholar] [CrossRef]
- Shabanikiya, H.; Jafari, M.; Gorgi, H.A.; Seyedin, H.; Rahimi, A. Developing a practical toolkit for evaluating hospital preparedness for surge capacity in disasters. Int. J. Disaster Risk Reduct. 2019, 34, 423–428. [Google Scholar] [CrossRef]
- American College of Emergency Physicians. Hospital Disaster Privileging (Policy #400326). Available online: https://www.acep.org/webportal/PracticeResources/PolicyStatements/hosp.htm (accessed on 9 February 2005).
- Tas, F.; Cakir, M.; Kadioglu, S. Identification of the preparedness level of nurses for disasters in Turkey: A university hospital example. Int. J. Disaster Risk Reduct. 2020, 44, 101441. [Google Scholar] [CrossRef]
- Munasinghe, N.L.; Matsui, K. Examining disaster preparedness at Matara district general hospital in Sri Lanka. Int. J. Disaster Risk Reduct. 2019, 40, 101154. [Google Scholar] [CrossRef]
- Phalkey, R.; Dash, S.; Mukhopadhyay, A.; Runge-Ranzinger, S.; Marx, M. Prepared to react? Assessing the functional capacity of the primary health care system in rural Orissa, India to respond to the devastating flood of September 2008. Glob. Health Action 2012, 5, 10964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Shareef, A.S.; Alsulimani, L.K.; Bojan, H.M.; Masri, T.M.; Grimes, J.O.; Molloy, M.S.; Ciottone, G.R. Evaluation of Hospitals’ Disaster Preparedness Plans in the Holy City of Makkah (Mecca): A Cross-Sectional Observation Study. Prehosp. Disaster Med. 2017, 32, 33. [Google Scholar] [CrossRef]
- Aladhrai, S.A.; Djalali, A.; Della Corte, F.; Alsabri, M.; El-Bakri, N.K.; Ingrassia, P.L. Impact of the 2011 Revolution on Hospital Disaster Preparedness in Yemen. Disaster Med. Public Health Prep. 2015, 9, 396–402. [Google Scholar] [CrossRef]
- Fung, O.W.; Loke, A.Y.; Lai, C.K. Disaster preparedness among Hong Kong nurses. J. Adv. Nurs. 2008, 62, 698–703. [Google Scholar] [CrossRef]
- O’Sullivan, T.L.; Dow, D.; Turner, M.C.; Lemyre, L.; Corneil, W.; Krewski, D.; Amaratunga, C.A. Disaster and emergency management: Canadian nurses’ perceptions of preparedness on hospital front lines. Prehosp. Disaster Med. 2008, 23, S11–S18. [Google Scholar] [CrossRef] [Green Version]
- Krajewski, M.J.; Sztajnkrycer, M.; Baez, A.A. Hospital Disaster Preparedness in the United States: New issues, New Challenges. IJDRR 2005, 4, 22–25. [Google Scholar]
- Fallah-Aliabadi, S.; Ostadtaghizadeh, A.; Ardalan, A.; Fatemi, F.; Khazai, B.; Mirjalili, M.R. Towards developing a model for the evaluation of hospital disaster resilience: A systematic review. BMC Health Serv. Res. 2020, 20, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Labrague, L.J.; Hammad, K.; Gloe, D.S.; McEnroe-Petitte, D.M.; Fronda, D.C.; Obeidat, A.A.; Leocadio, M.C.; Cayaban, A.R.; Mirafuentes, E.C. Disaster preparedness among nurses: A systematic review of literature. Int. Nurs. Rev. 2018, 65, 41–53. [Google Scholar] [CrossRef] [Green Version]
- Cole, G.; Rosenblum, A.J.; Boston, M.; Barnett, D.J. Applying the Haddon Matrix to Hospital Earthquake Preparedness and Response. Disaster Med. Public Health Prep. 2020, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Dell’Era, S.; Hugli, O.; Dami, F. Hospital Disaster Preparedness in Switzerland Over a Decade: A National Survey. Disaster Med. Public Health Prep. 2019, 13, 433–439. [Google Scholar] [CrossRef]
- Paganini, M.; Borrelli, F.; Cattani, J.; Ragazzoni, L.; Djalali, A.; Carenzo, L.; Corte, F.D.; Burkle, F.M.; Ingrassia, P.L. Assessment of disaster preparedness among emergency departments in Italian hospitals: A cautious warning for disaster risk reduction and management capacity. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 101. [Google Scholar] [CrossRef] [Green Version]
- El Sayed, M.; Chami, A.F.; Hitti, E. Developing a Hospital Disaster Preparedness Plan for Mass Casualty Incidents: Lessons Learned From the Downtown Beirut Bombing. Disaster Med. Public Health Prep. 2018, 12, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Naser, W.N.; Ingrassia, P.L.; Aladhrae, S.; Abdulraheem, W.A. A Study of Hospital Disaster Preparedness in South Yemen. Prehosp. Disaster Med. 2017, 33, 133–138. [Google Scholar] [CrossRef]
- Davidson, R.A.; Lambert, K.B. Comparing the Hurricane Disaster Risk of U.S. Coastal Counties. Nat. Hazards Rev. 2001, 2, 132–142. [Google Scholar] [CrossRef]
- Zyoud, S.H.; Fuchs-Hanusch, D. A bibliometric-based survey on AHP and TOPSIS techniques. Expert Syst. Appl. 2017, 78, 158–181. [Google Scholar] [CrossRef]
- Locurcio, M.; Tajani, F.; Morano, P.; Anelli, D. A Multi-Criteria Decision Analysis for the Assessment of the Real Estate Credit Risks; Springer: Cham, Switzerland, 2021; pp. 327–337. [Google Scholar]
- Liern, V.; Pérez-Gladish, B. Multiple criteria ranking method based on functional proximity index: Un-weighted TOPSIS. Ann. Oper. Res. 2020, 1–23. [Google Scholar] [CrossRef]
- Hwang, C.-L.; Yoon, K. Methods for Multiple Attribute Decision Making. In Lecture Notes in Economics and Mathematical Systems; Springer: Berlin/Heidelberg, Germany, 1981; pp. 58–191. [Google Scholar]
- Mojtahedi, M.; Mousavi, S.M.; Makui, A. Project risk identification and assessment simultaneously using multi-attribute group decision making technique. Saf. Sci. 2010, 48, 499–507. [Google Scholar] [CrossRef]
- Abdel-Basset, M.; Mohamed, R. A novel plithogenic TOPSIS-CRITIC model for sustainable supply chain risk management. J. Clean. Prod. 2020, 247, 119586. [Google Scholar] [CrossRef]
- Shukla, A.; Agarwal, P.; Rana, R.S.; Purohit, R. Applications of TOPSIS algorithm on various manufacturing processes: A review. Mater. Today Proc. 2017, 4, 5320–5329. [Google Scholar] [CrossRef]
- Ozkaya, G.; Erdin, C. Evaluation of smart and sustainable cities through a hybrid MCDM approach based on ANP and TOPSIS technique. Heliyon 2020, 6, e05052. [Google Scholar] [CrossRef] [PubMed]
- Rashid, T.; Beg, I.; Husnine, S.M. Robot selection by using generalized interval-valued fuzzy numbers with TOPSIS. Appl. Soft Comput. 2014, 21, 462–468. [Google Scholar] [CrossRef]
- Kusumawardani, R.P.; Agintiara, M. Application of Fuzzy AHP-TOPSIS Method for Decision Making in Human Resource Manager Selection Process. Procedia Comput. Sci. 2015, 72, 638–646. [Google Scholar] [CrossRef] [Green Version]
- Niu, D.; Wu, G.; Ji, Z.; Wang, D.; Li, Y.; Gao, T. Evaluation of Provincial Carbon Neutrality Capacity of China Based on Combined Weight and Improved TOPSIS Model. Sustainability 2021, 13, 2777. [Google Scholar] [CrossRef]
- Mohammed, A.; Yazdani, M.; Oukil, A.; Gonzalez, E.D. A Hybrid MCDM Approach towards Resilient Sourcing. Sustainability 2021, 13, 2695. [Google Scholar] [CrossRef]
- Luu, C.; von Meding, J.; Mojtahedi, M. Analyzing Vietnam’s national disaster loss database for flood risk assessment using multiple linear regression-TOPSIS. Int. J. Disaster Risk Reduct. 2019, 40, 101153. [Google Scholar] [CrossRef]
- Nyimbili, P.H.; Erden, T.; Karaman, H. Integration of GIS, AHP and TOPSIS for earthquake hazard analysis. Nat. Hazards 2018, 92, 1523–1546. [Google Scholar] [CrossRef]
- Kou, G.; Chao, X.; Peng, Y.; Xu, L.; Chen, Y. Intelligent Collaborative Support System for AHP-Group Decision Making. Stud. Inform. Control 2017, 26, 131–142. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, L.; Solangi, Y.A. Strategic renewable energy resources selection for Pakistan: Based on SWOT-Fuzzy AHP approach. Sustain. Cities Soc. 2020, 52, 101861. [Google Scholar] [CrossRef]
- Antoniou, F.; Aretoulis, G. A multi-criteria decision-making support system for choice of method of compensation for highway construction contractors in Greece. Int. J. Constr. Manag. 2019, 19, 492–508. [Google Scholar] [CrossRef]
- Marlyono, S.G.; Nandi, N. The Preparedness Level of Community in Facing Disaster in West Java Province. IOP Conf. Ser. Earth Environ. Sci. 2018, 145. [Google Scholar] [CrossRef]
- McRae, G.; Hodgkin, D. Half full or half empty? Shelter after the Jogjakarta earthquake. Disasters 2011, 35, 243–267. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. REKOMPAK: Rebuilding Indonesia’s Communities after Disasters, The Secretariat of the Multi Donor Fund for Aceh and Nias and the Java Reconstruction Fund; World Bank: Jakarta, Indonesia, 2012. [Google Scholar]

| Code | Attributes |
|---|---|
| EDM1 | Coordination of emergency and disaster management activities |
| EDM1.1 | Hospital Emergency/Disaster Committee |
| EDM1.2 | Committee member responsibilities and training |
| EDM1.3 | Designated emergency and disaster management coordinator |
| EDM1.4 | Preparedness programme for strengthening emergency and disaster response and recovery |
| EDM1.5 | Hospital incident management system |
| EDM1.6 | Emergency Operations Centre (EOC) |
| EDM1.7 | Coordination mechanisms and cooperative arrangements with local emergency management agencies |
| EDM1.8 | Coordination mechanisms and cooperative arrangements with the health-care network |
| EDM2 | Hospital emergency and disaster response and recovery planning |
| EDM2.1 | Hospital emergency or disaster response plan |
| EDM2.2 | Hospital hazard-specific subplans |
| EDM2.3 | Procedures to activate and deactivate plans |
| EDM2.4 | Hospital emergency and disaster response plan exercises, evaluation and corrective actions |
| EDM2.5 | Hospital recovery plan |
| EDM3 | Communication and information management |
| EDM3.1 | Emergency internal and external communication |
| EDM3.2 | External stakeholder directory |
| EDM3.3 | Procedures for communicating with the public and media |
| EDM3.4 | Management of patient information |
| EDM4 | Human resources |
| EDM4.1 | Staff contact list |
| EDM4.2 | Staff availability |
| EDM4.3 | Mobilization and recruitment of personnel during an emergency or disaster |
| EDM4.4 | Duties assigned to personnel for emergency or disaster response and recovery |
| EDM5 | Logistics and finance |
| EDM5.1 | Agreements with local suppliers and vendors for emergencies and disasters |
| EDM5.2 | Transportation during an emergency |
| EDM5.3 | Food and drinking-water during an emergency |
| EDM5.4 | Financial resources for emergencies and disasters |
| EDM6 | Patient care and support services |
| EDM6.1 | Continuity of emergency and critical care services |
| EDM6.2 | Continuity of essential clinical support services |
| EDM6.3 | Expansion of usable space for mass casualty incidents |
| EDM6.4 | Triage for major emergencies and disasters |
| EDM6.5 | Triage tags and other logistical supplies for mass casualty incidents |
| EDM6.6 | System for referral, transfer and reception of patients |
| EDM6.7 | Infection surveillance, prevention and control procedures |
| EDM6.8 | Psychosocial services |
| EDM6.9 | Post-mortem procedures in a mass fatality incident |
| EDM7 | Evacuation, decontamination and security |
| EDM7.1 | Evacuation plan |
| EDM7.2 | Decontamination for chemical and radiological hazards |
| EDM7.3 | Personal protection equipment and isolation for infectious diseases and epidemics |
| EDM7.4 | Emergency security procedures |
| EDM7.5 | Computer system network security |
| Dimension | Max Score | Hospital 1 Score | Ratio |
|---|---|---|---|
| Logistics and finance | 4 | 2 | 0.500 |
| WJ1 | WJ2 | WJ3 | WJ4 | WJ5 | WJ6 | WJ7 | WJ8 | WJ9 | WJ10 | Y1 | Y2 | Y3 | Y4 | Y5 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EDM1.1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 1 | 0.5 |
| EDM1.2 | 0 | 0.5 | 0.5 | 0 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
| EDM1.3 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | 0.5 | 1 | 1 | 1 |
| EDM1.4 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| EDM1.5 | 0 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 |
| EDM1.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0.5 | 1 | 0.5 | 0.5 | 0.5 |
| EDM1.7 | 0.5 | 0.5 | 0.5 | 0 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0.5 | 0 | 0.5 | 0 | 0 |
| EDM1.8 | 0.5 | 1 | 0.5 | 0 | 1 | 0.5 | 1 | 1 | 1 | 1 | 0.5 | 0 | 0.5 | 0 | 0.5 |
| EDM2.1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 1 | 0 | 0 | 0.5 | 0 | 0 |
| EDM2.2 | 0.5 | 0.5 | 0.5 | 0 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| EDM2.3 | 0.5 | 0.5 | 0.5 | 0 | 1 | 0 | 0 | 1 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 |
| EDM2.4 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
| EDM2.5 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 0 | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| EDM3.1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0 | 0.5 | 1 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0 |
| EDM3.2 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0 | 1 | 0 | 0 | 0.5 |
| EDM3.3 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 |
| EDM3.4 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0 |
| EDM4.1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0 | 1 |
| EDM4.2 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
| EDM4.3 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 |
| EDM4.4 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0 | 0 |
| EDM4.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 0 |
| EDM5.1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 |
| EDM5.2 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0 | 0.5 | 1 | 0.5 | 1 | 1 | 1 | 0.5 | 1 | 1 |
| EDM5.3 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| EDM5.4 | 0.5 | 0.5 | 0.5 | 0 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| EDM6.1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| EDM6.2 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| EDM6.3 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 |
| EDM6.4 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 1 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 1 |
| EDM6.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 |
| EDM6.6 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0 | 0.5 |
| EDM6.7 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| EDM6.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 |
| EDM6.9 | 0 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0 |
| EDM7.1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 |
| EDM7.2 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0 | 0 | 0.5 | 0 | 0 |
| EDM7.3 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
| EDM7.4 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 |
| EDM7.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 |
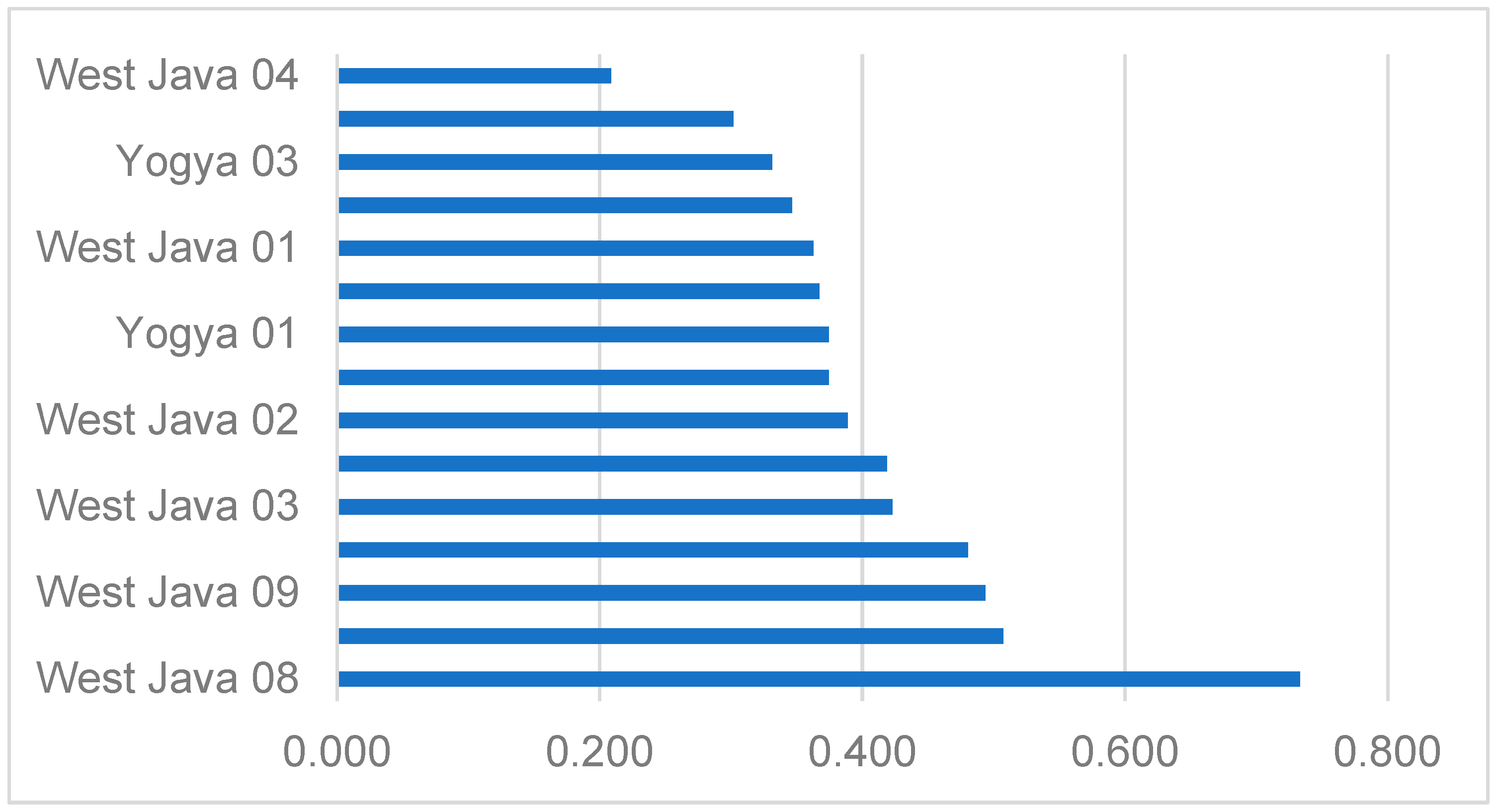
| Hospital | PIS | NIS | HEDM Index | Rank |
|---|---|---|---|---|
| West Java 1 | 0.0555 | 0.0316 | 0.363 | 11 |
| West Java 2 | 0.0534 | 0.0340 | 0.389 | 7 |
| West Java 3 | 0.0509 | 0.0373 | 0.423 | 5 |
| West Java 4 | 0.0698 | 0.0184 | 0.209 | 15 |
| West Java 5 | 0.0492 | 0.0455 | 0.480 | 4 |
| West Java 6 | 0.0557 | 0.0323 | 0.367 | 10 |
| West Java 7 | 0.0517 | 0.0373 | 0.419 | 6 |
| West Java 8 | 0.0257 | 0.0707 | 0.734 | 1 |
| West Java 9 | 0.0461 | 0.0449 | 0.494 | 3 |
| West Java 10 | 0.0454 | 0.0468 | 0.507 | 2 |
| Yogya 1 | 0.0567 | 0.0339 | 0.374 | 9 |
| Yogya 2 | 0.0632 | 0.0335 | 0.347 | 12 |
| Yogya 3 | 0.0603 | 0.0299 | 0.331 | 13 |
| Yogya 4 | 0.0644 | 0.0279 | 0.302 | 14 |
| Yogya 5 | 0.0605 | 0.0362 | 0.375 | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mojtahedi, M.; Sunindijo, R.Y.; Lestari, F.; Suparni; Wijaya, O. Developing Hospital Emergency and Disaster Management Index Using TOPSIS Method. Sustainability 2021, 13, 5213. https://doi.org/10.3390/su13095213
Mojtahedi M, Sunindijo RY, Lestari F, Suparni, Wijaya O. Developing Hospital Emergency and Disaster Management Index Using TOPSIS Method. Sustainability. 2021; 13(9):5213. https://doi.org/10.3390/su13095213
Chicago/Turabian StyleMojtahedi, Mohammad, Riza Yosia Sunindijo, Fatma Lestari, Suparni, and Oktomi Wijaya. 2021. "Developing Hospital Emergency and Disaster Management Index Using TOPSIS Method" Sustainability 13, no. 9: 5213. https://doi.org/10.3390/su13095213
APA StyleMojtahedi, M., Sunindijo, R. Y., Lestari, F., Suparni, & Wijaya, O. (2021). Developing Hospital Emergency and Disaster Management Index Using TOPSIS Method. Sustainability, 13(9), 5213. https://doi.org/10.3390/su13095213








