Adolescents’ School Travel and Unhealthy Snacking: Associations with School Transport Modes, Neighbourhood Deprivation, and Body Weight
Abstract
:1. Introduction
2. Materials and Methods
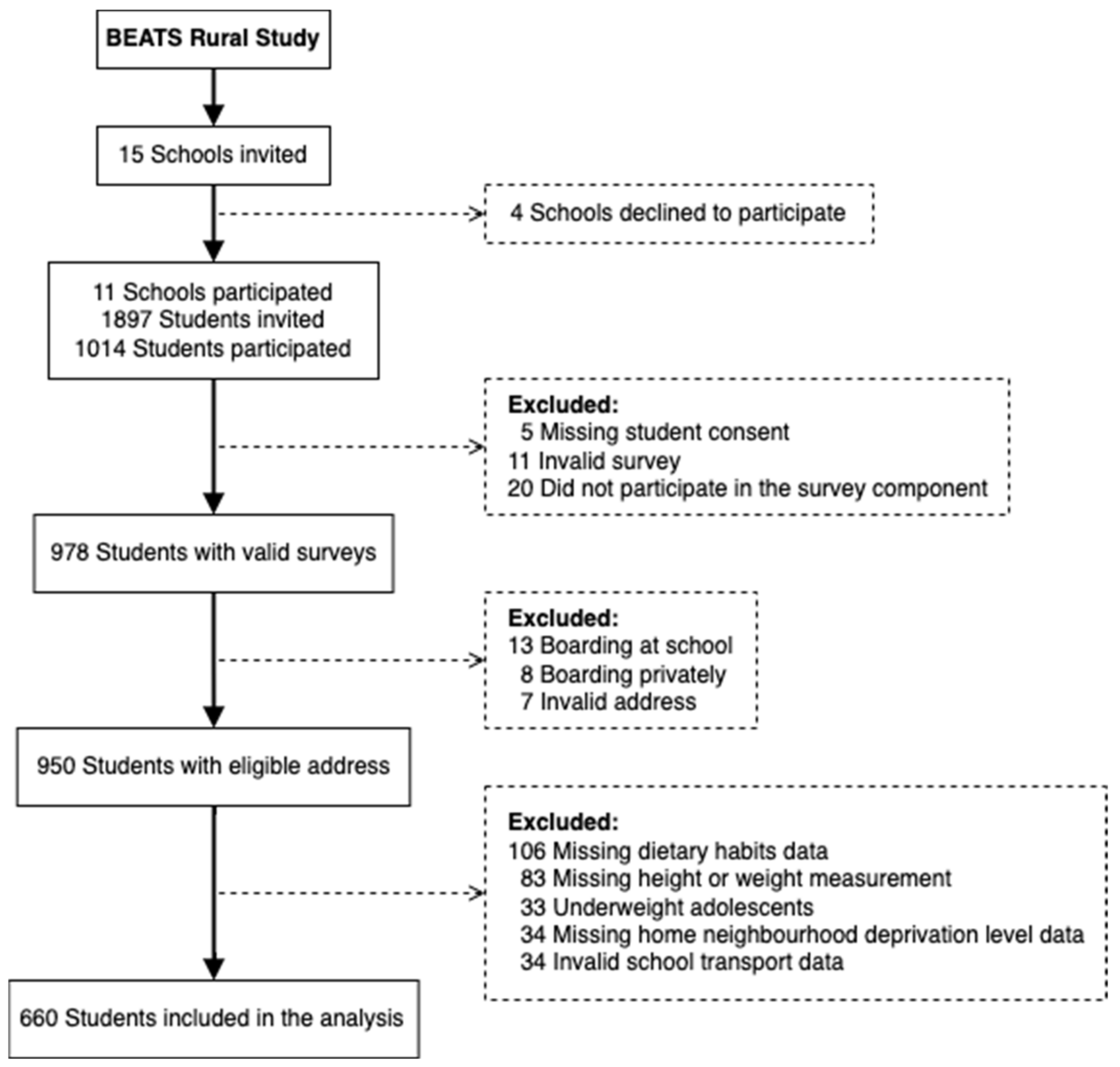
2.1. Study Setting and Participants
2.2. Measures
2.2.1. Student Survey
2.2.2. Anthropometric Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Implications
4.2. Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kek, C.C.; García Bengoechea, E.; Spence, J.C.; Mandic, S. The relationship between transport-to-school habits and physical activity in a sample of New Zealand adolescents. J. Sport Health Sci. 2019, 8, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Boreham, C.A.; Kelly, P.; Foster, C.E. The relationship between active travel to school and health-related fitness in children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez-Gomez, D.; Ruiz, J.R.; Gomez-Martinez, S.; Chillon, P.; Rey-Lopez, J.P.; Diaz, L.E.; Castillo, R.; Veiga, O.L.; Marcos, A.; Group, A.S. Active commuting to school and cognitive performance in adolescents: The AVENA study. Arch Pediatr. Adolesc. Med. 2011, 165, 300–305. [Google Scholar] [CrossRef] [Green Version]
- Chertok, M.; Voukelatos, A.; Sheppeard, V.; Rissel, C. Comparison of air pollution exposure for five commuting modes in Sydney—Car, train, bus, bicycle and walking. Health Promot. J. Aust. 2004, 15, 63–67. [Google Scholar] [CrossRef] [Green Version]
- Mizdrak, A.; Blakely, T.; Cleghorn, C.L.; Cobiac, L.J. Potential of active transport to improve health, reduce healthcare costs, and reduce greenhouse gas emissions: A modelling study. PLoS ONE 2019, 14, e0219316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stok, F.M.; De Vet, E.; Wardle, J.; Chu, M.T.; De Wit, J.; De Ridder, D.T. Navigating the obesogenic environment: How psychological sensitivity to the food environment and self-regulatory competence are associated with adolescent unhealthy snacking. Eat. Behav. 2015, 17, 19–22. [Google Scholar] [CrossRef]
- Townshend, T.; Lake, A. Obesogenic environments: Current evidence of the built and food environments. Perspect. Public Health 2016, 137, 38–44. [Google Scholar] [CrossRef] [Green Version]
- Rummo, P.E.; Wu, E.; McDermott, Z.T.; Wagner, R.F.; Schwartz, A.E.; Elbel, B. Relationship between retail food outlets near public schools and adolescent obesity in New York City. Health Place 2020, 65, 102408. [Google Scholar] [CrossRef]
- OECD. Obesity Update. 2017. Available online: https://www.oecd.org/health/obesity-update.htm (accessed on 12 January 2022).
- Ministry of Health. New Zealand Health Survey. Available online: https://minhealthnz.shinyapps.io/nz-health-survey-2020-21-annual-data-explorer/_w_95113a1c/#!/explore-indicators (accessed on 12 January 2022).
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A foundation for future health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Royal Society for Public Health. Routing Out Childhood Obesity. 2019. Available online: https://www.rsph.org.uk/our-work/policy/obesity/routing-out-childhood-obesity.html (accessed on 12 January 2022).
- Swinburn, B.; Egger, G.; Raza, F. Dissecting Obesogenic Environments: The Development and Application of a Framework for Identifying and Prioritizing Environmental Interventions for Obesity. Prev. Med. 1999, 29, 563–570. [Google Scholar] [CrossRef]
- Vandevijvere, S.; Molloy, J.; Hassen de Medeiros, N.; Swinburn, B. Unhealthy food marketing around New Zealand schools: A national study. Int. J. Public Health 2018, 63, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Vandevijvere, S.; Sushil, Z.; Exeter, D.J.; Swinburn, B. Obesogenic Retail Food Environments Around New Zealand Schools: A National Study. Am. J. Prev. Med. 2016, 51, e57–e66. [Google Scholar] [CrossRef]
- Yang, M.; Wang, H.; Qiu, F. The built environment of schools: Access to unhealthy food outlets and outdoor recreational facilities. Cities 2019, 87, 229–237. [Google Scholar] [CrossRef]
- Kelly, C.; Callaghan, M.; Gabhainn, S.N. ‘It’s Hard to Make Good Choices and It Costs More’: Adolescents’ Perception of the External School Food Environment. Nutrients 2021, 13, 1043. [Google Scholar] [CrossRef] [PubMed]
- Scully, M.; Morley, B.; Niven, P.; Crawford, D.; Pratt, I.S.; Wakefield, M. Factors associated with high consumption of soft drinks among Australian secondary-school students. Public Health Nutr. 2017, 20, 2340–2348. [Google Scholar] [CrossRef] [Green Version]
- Tripicchio, G.L.; Kachurak, A.; Davey, A.; Bailey, R.L.; Dabritz, L.J.; Fisher, J.O. Associations between snacking and weight status among adolescents 12–19 years in the United States. Nutrients 2019, 11, 1486. [Google Scholar] [CrossRef] [Green Version]
- Larson, N.; Story, M. A review of snacking patterns among children and adolescents: What are the implications of snacking for weight status? Child. Obes. 2013, 9, 104–115. [Google Scholar] [CrossRef]
- Marangoni, F.; Martini, D.; Scaglioni, S.; Sculati, M.; Donini, L.M.; Leonardi, F.; Agostoni, C.; Castelnuovo, G.; Ferrara, N.; Ghiselli, A.; et al. Snacking in nutrition and health. Int. J. Food Sci. Nutr. 2019, 70, 909–923. [Google Scholar] [CrossRef]
- Jensen, M.L.; Corvalán, C.; Reyes, M.; Popkin, B.M.; Taillie, L.S. Snacking patterns among Chilean children and adolescents: Is there potential for improvement? Public Health Nutr. 2019, 22, 2803–2812. [Google Scholar] [CrossRef]
- Williamson, V.G.; Dilip, A.; Dillard, J.R.; Morgan-Daniel, J.; Lee, A.M.; Cardel, M.I. The influence of socioeconomic status on snacking and weight among adolescents: A scoping review. Nutrients 2020, 12, 167. [Google Scholar] [CrossRef] [Green Version]
- Cowburn, G.; Matthews, A.; Doherty, A.; Hamilton, A.; Kelly, P.; Williams, J.; Foster, C.; Nelson, M. Exploring the opportunities for food and drink purchasing and consumption by teenagers during their journeys between home and school: A feasibility study using a novel method. Public Health Nutr. 2016, 19, 93–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadler, R.C.; Clark, A.F.; Wilk, P.; O’Connor, C.; Gilliland, J.A. Using GPS and activity tracking to reveal the influence of adolescents’ food environment exposure on junk food purchasing. Can. J. Public Health 2016, 107, eS14–eS20. [Google Scholar] [CrossRef] [PubMed]
- White, B.; Bengoechea, E.G.; Spence, J.C.; Coppell, K.J.; Mandic, S. Comparison of physical activity patterns across large, medium and small urban areas and rural settings in the Otago Region, New Zealand. N. Z. Med. J. 2021, 134, 51–65. [Google Scholar] [PubMed]
- Statistic New Zealand. ANZLIC Metadata Urban Rural. Available online: https://datafinder.stats.govt.nz/document/21473-anzlic-metadata-2018-urban-rural/ (accessed on 12 January 2022).
- Mandic, S.; Williams, J.; Moore, A.; Hopkins, D.; Flaherty, C.; Wilson, G.; Bengoechea, E.G.; Spence, J.C. Built Environment and Active Transport to School (BEATS) Study: Protocol for a cross-sectional study. BMJ Open 2016, 6, e011196. [Google Scholar] [CrossRef] [Green Version]
- Salmond, C.; Crampton, P.; King, P.; Waldegrave, C. NZiDep: A New Zealand index of socioeconomic deprivation for individuals. Soc. Sci. Med. 2006, 62, 1474–1485. [Google Scholar] [CrossRef]
- Mandic, S.; Hopkins, D.; García Bengoechea, E.; Flaherty, C.; Williams, J.; Sloane, L.; Moore, A.; Spence, J.C. Adolescents’ perceptions of cycling versus walking to school: Understanding the New Zealand context. J. Transport. Health 2017, 4, 294–304. [Google Scholar] [CrossRef]
- Mandic, S.; Bengoechea, E.G.; Coppell, K.J.; Spence, J.C. Clustering of (Un)Healthy Behaviors in Adolescents from Dunedin, New Zealand. Am. J. Health Behav. 2017, 41, 266–276. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [Green Version]
- Caspi, C.E.; Wang, Q.; Shanafelt, A.; Larson, N.; Wei, S.; Hearst, M.O.; Nanney, M.S. School Breakfast Program Participation and Rural Adolescents’ Purchasing Behaviors in Food Stores and Restaurants. J. Sch. Health 2017, 87, 723–731. [Google Scholar] [CrossRef]
- Mohammadi, S.; Jalaludin, M.Y.; Su, T.T.; Dahlui, M.; Azmi Mohamed, M.N.; Abdul Majid, H. Determinants of Diet and Physical Activity in Malaysian Adolescents: A Systematic Review. Int J. Environ. Res. Public Health 2019, 16, 603. [Google Scholar] [CrossRef] [Green Version]
- Savige, G.; MacFarlane, A.; Ball, K.; Worsley, A.; Crawford, D. Snacking behaviours of adolescents and their association with skipping meals. Int. J. Behav. Nutr. Phys. Act. 2007, 4, 61–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egli, V.; Hobbs, M.; Carlson, J.; Donnellan, N.; Mackay, L.; Exeter, D.; Villanueva, K.; Zinn, C.; Smith, M. Deprivation matters: Understanding associations between neighbourhood deprivation, unhealthy food outlets, unhealthy dietary behaviours and child body size using structural equation modelling. J. Epidemiol. Community Health 2020, 74, 460–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darling, H.; Reeder, A.I.; McGee, R.; Williams, S. Brief report: Disposable income, and spending on fast food, alcohol, cigarettes, and gambling by New Zealand secondary school students. J. Adolesc. 2006, 29, 837–843. [Google Scholar] [CrossRef] [PubMed]
- McKeown, A.; Nelson, R. Independent decision making of adolescents regarding food choice. Int. J. Consum. Stud. 2018, 42, 469–477. [Google Scholar] [CrossRef]
- Beal, T.; Morris, S.S.; Tumilowicz, A. Global Patterns of Adolescent Fruit, Vegetable, Carbonated Soft Drink, and Fast-Food Consumption: A Meta-Analysis of Global School-Based Student Health Surveys. Food Nutr. Bull. 2019, 40, 444–459. [Google Scholar] [CrossRef]
- Arango-Angarita, A.; Mendez-Gomez-Humaran, I.; Guerrero-Lopez, C.M.; Shamah-Levy, T. Is store density associated with sugar-sweetened beverages consumption and overweight or obesity in Mexican adolescents? Pediatr. Obes. 2021, 17, e12838. [Google Scholar] [CrossRef]
- Hess, J.M.; Slavin, J.L. The benefits of defining “snacks”. Physiol. Behav. 2018, 193, 284–287. [Google Scholar] [CrossRef]
- Wild, C.E.K.; Grant, C.C.; Cave, T.L.; Wynter, L.E.; Derraik, J.G.B.; Willing, E.J.; Hofman, P.L.; Anderson, Y.C. The importance of rurality data in understanding access to healthcare services for childhood obesity. N. Z. Med. J. 2019, 132, 60–63. [Google Scholar]
- Marshall, J.D.; Wilson, R.D.; Meyer, K.L.; Rajangam, S.K.; McDonald, N.C.; Wilson, E.J. Vehicle Emissions during Children’s School Commuting: Impacts of Education Policy. Environ. Sci. Technol. 2010, 44, 1537–1543. [Google Scholar] [CrossRef]
- Hopkins, D.; García Bengoechea, E.; Mandic, S. Adolescents and their aspirations for private car-based transport. Transportation 2019, 48, 67–93. [Google Scholar] [CrossRef] [Green Version]
- Trapp, G.; Hooper, P.; Thornton, L.E.; Kennington, K.; Sartori, A.; Wickens, N.; Billingham, W. Exposure to unhealthy food and beverage advertising during the school commute in Australia. J. Epidemiol. Community Health 2021, 75, 1232–1235. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, E.; Vandevijvere, S.; Swinburn, B. The healthiness of New Zealand school food environments: A national survey. Aust. N. Z. J. Public Health 2022, 46, 325–331. [Google Scholar] [CrossRef] [PubMed]

| Variables | Overall (n = 660) |
|---|---|
| Age (years) | 15.3 ± 1.3 |
| Gender | |
| Boys | 319 (48.3%) |
| Girls | 341 (51.7%) |
| Ethnicity (n = 659) | |
| New Zealand European | 493 (74.8%) |
| Māori | 84 (12.7%) |
| Pacific Islands | 25 (3.8%) |
| Asian | 14 (2.1%) |
| Other | 43 (6.5%) |
| Body mass index category | |
| Healthy weight | 505 (76.5%) |
| Overweight | 113 (17.1%) |
| Obese | 42 (6.4%) |
| Home neighbourhood deprivation level | |
| Low | 307 (46.5%) |
| Mid | 245 (37.1%) |
| High | 108 (16.4%) |
| School settlement type | |
| Medium urban area | 80 (12.1%) |
| Small urban area | 444 (67.3%) |
| Rural settlement | 136 (20.6%) |
| Transport modes TO school | |
| Active transport only | 190 (28.8%) |
| Motorised transport only | 336 (50.9%) |
| Mixed transport modes | 134 (20.3%) |
| Transport modes FROM school | |
| Active transport only | 204 (30.9%) |
| Motorised transport only | 342 (51.8%) |
| Mixed transport modes | 114 (17.3%) |
| School Transport Modes | |||||
|---|---|---|---|---|---|
| Total Sample | Motorised Transport | Active Transport | Mixed Transport | p-Value * | |
| On the Way TO School | |||||
| Frequency of Purchasing and Consuming Unhealthy Snack Food (days/week) | |||||
| Total Sample: | (n = 660) | (n = 336) | (n = 190) | (n = 134) | |
| Never | 547 (82.9%) | 291 (86.6%) | 146 (76.8%) | 110 (82.1%) | |
| 1 to 2 days | 78 (11.8%) | 32 (9.5%) | 27 (14.2%) | 19 (14.2%) | 0.025 |
| 3 to 5 days | 35 (5.3%) | 13 (3.9%) | 17 (8.9%) | 5 (3.7%) | |
| Boys: | (n = 319) | (n = 160) | (n = 102) | (n = 57) | |
| Never | 247 (77.4%) | 134 (83.8%) | 71 (69.6%) | 42 (73.7%) | |
| 1 to 2 days | 48 (15.0%) | 17 (10.6%) | 20 (19.6%) | 11 (19.3%) | 0.087 |
| 3 to 5 days | 24 (7.5%) | 9 (5.6%) | 11 (10.8%) | 4 (7.0%) | |
| Girls: | (n = 341) | (n = 176) | (n = 88) | (n = 77) | |
| Never | 300 (88.0%) | 157 (89.2%) | 75 (85.2%) | 68 (88.3%) | |
| 1 to 2 days | 30 (8.8%) | 15 (8.5%) | 7 (8.0%) | 8 (10.4%) | 0.256 |
| 3 to 5 days | 11 (3.2%) | 4 (2.3%) | 6 (6.8%) | 1 (1.3%) | |
| Frequency of Purchasing and Consuming Soft Drinks (days/week) | |||||
| Total Sample: | (n = 660) | (n = 336) | (n = 190) | (n = 134) | |
| Never | 578 (87.6%) | 308 (91.7%) | 157 (82.6%) | 113 (84.3%) | |
| 1 to 2 days | 61 (9.2%) | 24 (7.1%) | 21 (11.1%) | 16 (11.9%) | 0.005 |
| 3 to 5 days | 21 (3.2%) | 4 (1.2%) | 12 (6.3%) | 5 (3.7%) | |
| Boys: | (n = 319) | (n = 160) | (n = 102) | (n = 57) | |
| Never | 259 (81.2%) | 141 (88.1%) | 76 (74.5%) | 42 (73.7%) | |
| 1 to 2 days | 44 (13.8%) | 17 (10.6%) | 17 (16.7%) | 10 (17.5%) | 0.010 |
| 3 to 5 days | 16 (5.0%) | 2 (1.3%) | 9 (8.8%) | 5 (8.8%) | |
| Girls: | (n = 341) | (n = 176) | (n = 88) | (n = 77) | |
| Never | 319 (93.5%) | 167 (94.9%) | 81 (92.0%) | 71 (92.2%) | |
| 1 to 2 days | 17 (5.0%) | 7 (4.0%) | 4 (4.5%) | 6 (7.8%) | 0.267 |
| 3 to 5 days | 5 (1.5%) | 2 (1.1%) | 3 (3.4%) | 0 (0.0%) | |
| On the Way FROM School | |||||
| Frequency of Purchasing and Consuming Unhealthy Snack Food (days/week) | |||||
| Total Sample: | (n = 660) | (n = 342) | (n = 204) | (n = 114) | |
| Never | 447 (67.7%) | 233 (68.1%) | 148 (72.5%) | 66 (57.9%) | |
| 1 to 2 days | 182 (27.6%) | 96 (28.1%) | 48 (23.5%) | 38 (33.3%) | 0.044 |
| 3 to 5 days | 31 (4.7%) | 13 (3.8%) | 8 (3.9%) | 10 (8.8%) | |
| Boys: | (n = 319) | (n = 160) | (n = 106) | (n = 53) | |
| Never | 198 (62.1%) | 104 (65.0%) | 68 (64.2%) | 26 (49.1%) | |
| 1 to 2 days | 102 (32.0%) | 49 (30.6%) | 31 (29.2%) | 22 (41.5%) | 0.248 |
| 3 to 5 days | 19 (6.0%) | 7 (4.4%) | 7 (6.6%) | 5 (9.4%) | |
| Girls: | (n = 341) | (n = 182) | (n = 98) | (n = 61) | |
| Never | 249 (73.0%) | 129 (70.9%) | 80 (81.6%) | 40 (65.6%) | |
| 1 to 2 days | 80 (23.5%) | 47 (25.8%) | 17 (17.3%) | 16 (26.2%) | 0.053 |
| 3 to 5 days | 12 (3.5%) | 6 (3.3%) | 1 (1.0%) | 5 (8.2%) | |
| Frequency of Purchasing and Consuming Soft Drinks (days/week) | |||||
| Total Sample: | (n = 660) | (n = 342) | (n = 204) | (n = 114) | |
| Never | 502 (76.1%) | 270 (78.9%) | 158 (77.5%) | 74 (64.9%) | |
| 1 to 2 days | 135 (20.5%) | 64 (18.7%) | 35 (17.2%) | 36 (31.6%) | 0.007 |
| 3 to 5 days | 23 (3.5%) | 8 (2.3%) | 11 (5.4%) | 4 (3.5%) | |
| Boys: | (n = 319) | (n = 160) | (n = 106) | (n = 53) | |
| Never | 211 (66.1%) | 115 (71.9%) | 69 (65.1%) | 27 (50.9%) | |
| 1 to 2 days | 90 (28.2%) | 40 (25.0%) | 28 (26.4%) | 22 (41.5%) | 0.035 |
| 3 to 5 days | 18 (5.6%) | 5 (3.1%) | 9 (8.5%) | 4 (7.5%) | |
| Girls: | (n = 341) | (n = 182) | (n = 98) | (n = 61) | |
| Never | 291 (85.3%) | 155 (85.2%) | 89 (90.8%) | 47 (77.0%) | |
| 1 to 2 days | 45 (13.2%) | 24 (13.2%) | 7 (7.1%) | 14 (23.0%) | 0.058 |
| 3 to 5 days | 5 (1.5%) | 3 (1.6%) | 2 (2.0%) | 0 (0.0%) | |
| Neighbourhood Deprivation Level | Body Mass Index Category | ||||||
|---|---|---|---|---|---|---|---|
| Low | Mid | High | p-Value * | Healthy Weight | Overweight/Obese | p-Value * | |
| On the Way TO School | |||||||
| Frequency of Purchasing/Consuming Unhealthy Snack Food (days/week) | |||||||
| Total Sample: | (n = 307) | (n = 245) | (n = 108) | (n = 505) | (n = 155) | ||
| Never | 267 (87.0%) | 201 (82.0%) | 79 (73.1%) | 424 (84.0%) | 123 (79.4%) | ||
| 1 to 2 days | 31 (10.1%) | 31 (12.7%) | 16 (14.8%) | 0.003 | 57 (11.3%) | 21 (13.5%) | 0.360 |
| 3 to 5 days | 9 (2.9%) | 13 (5.3%) | 13 (12.0%) | 24 (4.8%) | 11 (7.1%) | ||
| Boys: | (n = 152) | (n = 119) | (n = 48) | (n = 249) | (n = 70) | ||
| Never | 126 (82.9%) | 94 (79.0%) | 27 (56.3%) | 193 (77.5%) | 54 (77.1%) | ||
| 1 to 2 days | 20 (13.2%) | 17 (14.3%) | 11 (22.9%) | <0.001 | 40 (16.1%) | 8 (11.4%) | 0.273 |
| 3 to 5 days | 6 (3.9%) | 8 (6.7%) | 10 (20.8%) | 16 (6.4%) | 8 (11.4%) | ||
| Girls: | (n = 155) | (n = 126) | (n = 60) | (n = 256) | (n = 85) | ||
| Never | 141 (91.0%) | 107 (84.9%) | 52 (86.7%) | 231 (90.2%) | 69 (81.2%) | ||
| 1 to 2 days | 11 (7.1%) | 14 (11.1%) | 5 (8.3%) | 0.526 | 17 (6.6%) | 13 (15.3%) | 0.048 |
| 3 to 5 days | 3 (1.9%) | 5 (4.0%) | 3 (5.0%) | 8 (3.1%) | 3 (3.5%) | ||
| Frequency of Purchasing/Consuming Soft Drinks (days/week) | |||||||
| Total Sample: | (n = 307) | (n = 245) | (n = 108) | (n = 505) | (n = 155) | ||
| Never | 287 (93.5%) | 209 (85.3%) | 82 (75.9%) | 452 (89.5%) | 126 (81.3%) | ||
| 1 to 2 days | 16 (5.2%) | 27 (11.0%) | 18 (16.7%) | <0.001 | 38 (7.5%) | 23 (14.8%) | 0.018 |
| 3 to 5 days | 4 (1.3%) | 9 (3.7%) | 8 (7.4%) | 15 (3.0%) | 6 (3.9%) | ||
| Boys: | (n = 152) | (n = 119) | (n = 48) | (n = 249) | (n = 70) | ||
| Never | 134 (88.2%) | 93 (78.2%) | 32 (66.7%) | 205 (82.3%) | 54 (77.1%) | ||
| 1 to 2 days | 14 (9.2%) | 19 (16.0%) | 11 (22.9%) | 0.013 | 31 (12.4%) | 13 (18.6%) | 0.415 |
| 3 to 5 days | 4 (2.6%) | 7 (5.9%) | 5 (10.4%) | 13 (5.2%) | 3 (4.3%) | ||
| Girls: | (n = 155) | (n = 126) | (n = 60) | (n = 256) | (n = 85) | ||
| Never | 153 (98.7%) | 116 (92.1%) | 50 (83.3%) | 247 (96.5%) | 72 (84.7%) | ||
| 1 to 2 days | 2 (1.3%) | 8 (6.3%) | 7 (11.7%) | <0.001 | 7 (2.7%) | 10 (11.8%) | <0.001 |
| 3 to 5 days | 0 (0.0%) | 2 (1.6%) | 3 (5.0%) | 2 (0.8%) | 3 (3.5%) | ||
| On the Way FROM School | |||||||
| Frequency of Purchasing/Consuming Unhealthy Snack Food (days/week) | |||||||
| Total Sample: | (n = 307) | (n = 245) | (n = 108) | (n = 505) | (n = 155) | ||
| Never | 215 (70.0%) | 163 (66.5%) | 69 (63.9%) | 347 (68.7%) | 100 (64.5%) | ||
| 1 to 2 days | 78 (25.4%) | 74 (30.2%) | 30 (27.8%) | 0.216 | 137 (27.1%) | 45 (29.0%) | 0.408 |
| 3 to 5 days | 14 (4.6%) | 8 (3.3%) | 9 (8.3%) | 21 (4.2%) | 10 (6.5%) | ||
| Boys: | (n = 152) | (n = 119) | (n = 48) | (n = 249) | (n = 70) | ||
| Never | 98 (64.5%) | 74 (62.2%) | 26 (54.2%) | 153 (61.4%) | 45 (64.3%) | ||
| 1 to 2 days | 44 (28.9%) | 41 (34.5%) | 17 (35.4%) | 0.341 | 83 (33.3%) | 19 (27.1%) | 0.416 |
| 3 to 5 days | 10 (6.6%) | 4 (3.4%) | 5 (10.4%) | 13 (5.2%) | 6 (8.6%) | ||
| Girls: | (n = 155) | (n = 126) | (n = 60) | (n = 256) | (n = 85) | ||
| Never | 117 (75.5%) | 89 (70.6%) | 43 (71.7%) | 194 (75.8%) | 55 (64.7%) | ||
| 1 to 2 days | 34 (21.9%) | 33 (26.2%) | 13 (21.7%) | 0.558 | 54 (21.1%) | 26 (30.6%) | 0.137 |
| 3 to 5 days | 4 (2.6%) | 4 (3.2%) | 4 (6.7%) | 8 (3.1%) | 4 (4.7%) | ||
| Frequency of Purchasing/Consuming Soft Drinks (days/week) | |||||||
| Total Sample: | (n = 307) | (n = 245) | (n = 108) | (n = 505) | (n = 155) | ||
| Never | 248 (80.8%) | 185 (75.5%) | 69 (63.9%) | 390 (77.2%) | 112 (72.3%) | ||
| 1 to 2 days | 52 (16.9%) | 53 (21.6%) | 30 (27.8%) | 0.002 | 100 (19.8%) | 35 (22.6%) | 0.291 |
| 3 to 5 days | 7 (2.3%) | 7 (2.9%) | 9 (8.3%) | 15 (3.0%) | 8 (5.2%) | ||
| Boys: | (n = 152) | (n = 119) | (n = 48) | (n = 249) | (n = 70) | ||
| Never | 107 (70.4%) | 77 (64.7%) | 27 (56.3%) | 167 (67.1%) | 44 (62.9%) | ||
| 1 to 2 days | 39 (25.7%) | 36 (30.3%) | 15 (31.3%) | 0.153 | 69 (27.7%) | 21 (30.0%) | 0.739 |
| 3 to 5 days | 6 (3.9%) | 6 (5.0%) | 6 (12.5%) | 13 (5.2%) | 5 (7.1%) | ||
| Girls: | (n = 155) | (n = 126) | (n = 60) | (n = 256) | (n = 85) | ||
| Never | 141 (91.0%) | 108 (85.7%) | 42 (70.0%) | 223 (87.1%) | 68 (80.0%) | ||
| 1 to 2 days | 13 (8.4%) | 17 (13.5%) | 15 (25.0%) | 0.002 | 31 (12.1%) | 14 (16.5%) | 0.101 |
| 3 to 5 days | 1 (0.6%) | 1 (0.8%) | 3 (5.0%) | 2 (0.8%) | 3 (3.5%) | ||
| Unadjusted Model | Adjusted Model 1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Buy and Consume Unhealthy Snack Food or Soft Drinks on the Way TO School | Buy and Consume Unhealthy Snack Food or Soft Drinks on the way FROM School | Buy and Consume Unhealthy Snack Food or Soft Drinks on the Way TO School | Buy and Consume Unhealthy Snack Food or Soft Drinks on the Say FROM School | |||||||||
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| School Transport Mode | ||||||||||||
| Motorised Transport Only (Ref) | ||||||||||||
| Active Transport Only | 1.91 | 1.23–2.95 | 0.004 | 0.82 | 0.57–1.19 | 0.305 | 1.42 | 0.88–2.29 | 0.154 | 0.68 | 0.46–1.03 | 0.068 |
| Mixed Transport Modes | 1.35 | 0.81–2.25 | 0.256 | 1.74 | 1.13–2.67 | 0.011 | 1.27 | 0.74–2.16 | 0.384 | 1.65 | 1.06–2.57 | 0.027 |
| Neighbourhood Deprivation | ||||||||||||
| Low (Ref) | ||||||||||||
| Mid | 1.70 | 1.09–2.64 | 0.020 | 1.21 | 0.85–1.72 | 0.290 | 1.65 | 1.02–2.66 | 0.041 | 1.40 | 0.96–2.06 | 0.081 |
| High | 2.82 | 1.68–4.74 | <0.001 | 1.61 | 1.03–2.52 | 0.038 | 2.85 | 1.62–4.98 | <0.001 | 1.87 | 1.15–3.05 | 0.012 |
| Body Mass Index Category | ||||||||||||
| Healthy Weight (Ref) | ||||||||||||
| Overweight/Obese | 1.46 | 0.95–2.24 | 0.086 | 1.25 | 0.86–1.80 | 0.240 | 1.51 | 0.96–2.37 | 0.072 | 1.24 | 0.85–1.82 | 0.271 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Situmorang, M.L.; Coppell, K.J.; Smith, M.; Keall, M.; Mandic, S. Adolescents’ School Travel and Unhealthy Snacking: Associations with School Transport Modes, Neighbourhood Deprivation, and Body Weight. Sustainability 2022, 14, 7038. https://doi.org/10.3390/su14127038
Situmorang ML, Coppell KJ, Smith M, Keall M, Mandic S. Adolescents’ School Travel and Unhealthy Snacking: Associations with School Transport Modes, Neighbourhood Deprivation, and Body Weight. Sustainability. 2022; 14(12):7038. https://doi.org/10.3390/su14127038
Chicago/Turabian StyleSitumorang, Margaretha L., Kirsten J. Coppell, Melody Smith, Michael Keall, and Sandra Mandic. 2022. "Adolescents’ School Travel and Unhealthy Snacking: Associations with School Transport Modes, Neighbourhood Deprivation, and Body Weight" Sustainability 14, no. 12: 7038. https://doi.org/10.3390/su14127038
APA StyleSitumorang, M. L., Coppell, K. J., Smith, M., Keall, M., & Mandic, S. (2022). Adolescents’ School Travel and Unhealthy Snacking: Associations with School Transport Modes, Neighbourhood Deprivation, and Body Weight. Sustainability, 14(12), 7038. https://doi.org/10.3390/su14127038







