Abstract
The aim of our research was to establish a reproducible curriculum that offers the possibility to gain basic surgical skills (knot tying, suturing, laparoscopy basics) through distance education in emergency situations by using tools available in the household. Forty-six volunteering third- and fourth-year medical students were involved in the study. The distance education system was set up using homemade or easily obtainable tools (an empty can, shoe box, sponge, etc.) to teach surgical knotting, suturing, and basic laparoscopic skills. The reachable learning objectives were contrasted with the original course plan. Feedback from the students has been collected. The students’ results were compared to the regular course of the previous years. Seventy-nine percent of the original learning objectives could be reached completely, and 15% partially. The necessary tools were available for 82% of the students. The students evaluated the course for 4.26 in general and 4.86 considering the circumstances (on a 5-level-scale). The homemade trainers were assessed over four as an acceptable substitution. Students’ exam results decreased only by 7% compared to the previous two years. Basic surgical skills can be educated with acceptable efficiency and student satisfaction using distance teaching and homemade tools. This is the first study where not only the simulators but the surgical instruments were replaced with household tools and evaluated by a reproducible curriculum.
1. Introduction
“For a hard knot, a hard tool must be sought.” Erasmus.
In medical education, the teaching of basic surgical skills has a fundamental role in all levels of the curriculum, including undergraduate, postgraduate, and specialized training programs. Knot tying, suturing and basic laparoscopic skills are essential for those who are willing to or still work on an invasive medical discipline, which is traditionally acquired by the Halstedian apprenticeship model.
Simulation-based learning (SBL) in surgical education has been found as an effective way of education [1,2]. With the rapid development of IT (info-communication technologies) and other engineering disciplines, innovative tools and methods are introduced in surgical education, including virtual and augmented reality [3], 3D printing [4], and artificial intelligence (AI) [5]. Despite their proven advantages and effectiveness, it must be mentioned that some high-end simulators are not widely available in low- or middle-income countries due to their high costs [6]. Another pitfall of advanced education tools and regular teaching sessions is that in emergency situations, the accessibility of simulation centers or clinical training sites can be difficult or even impossible, as could be seen in the era of the COVID-19 pandemic [7,8].
The pandemic has forced most universities around the world to—all of a sudden—switch to distance education, with extremely limited preparation possibilities and resources. The sudden change made it impossible to hold contact hours or to send the necessary equipment for the students to practice at home [9,10,11,12]. Although the pandemic catalyzed this process, we believe the lessons learned and the newly developed methodologies could be applied for further emergency situations, resource-limited settings, or even in the regular curriculum. Higher education institutes, teachers, and students have tirelessly worked on widely available, innovative, and intuitive teaching methods to overcome the challenges that the COVID-19 pandemic caused in surgical education. However, recent studies have highlighted that the critical evaluation of home-based and do-it-yourself (DIY) surgical education solutions is strongly recommended [13,14], along with education programs supported by distance and e-learning platforms [15,16].
The widespread use of mobile phones, tablets, and multimedia platforms has allowed e-learning materials to improve gradually in recent years. There are now numerous teaching aids available as instructional videos, podcasts, microblogs, etc., using a variety of education tools (from online lectures and tutorials to virtual patient scenarios). Although the utility and cost-effectivity of e-learning have already been demonstrated, many authors also draw attention to its disadvantages, as their (especially the free contents) quality and content are mostly uncontrolled [17,18,19,20,21].
The application of distance education poses a serious challenge in the teaching of practical topics such as basic surgical skills: knotting, suturing, and laparoscopy. Although e-learning-based educational materials and teaching programs can be found, they assume that the student has basic surgical instruments and simulators at their disposal, which is not necessarily true, especially in developing countries and remote locations.
However, numerous low-cost laparoscopic trainers have been published in the literature [22,23,24,25], and homemade knotting and suture trainers are not that popular. Although some do-it-yourself methods have already been constructed for developing countries (resource-limited settings) [26,27,28,29,30], we did not find any publication about low-cost or DIY replacement for surgical instruments in the reviewed literature.
The aim of the study was to design and develop a set of homemade tools and a complex methodology, along with a curriculum, in order to make basic surgical education widely available in case of emergency situations and to provide an affordable, widely available surgical teaching solution for those, who has no or limited access to high-end simulation centers and devices.
2. Materials and Methods
After the outbreak of the COVID-19 pandemic, our research group started to develop a curriculum to switch to distance education as fast as possible. The criteria for the methods and tools were the following:
- at least 2/3 of the original curriculum of the course can be completed,
- results of the students do not deteriorate drastically,
- the tools should be available or easily obtainable in the household,
- the alternative solutions should be acceptable and available to the students.
According to the indicators above, approximately 12 h long course plan was created (detailed description in Supplementary Material S1):
- Online consultation—7 times, a total of 420 min.
- Independent practice—5 stages, according to students’ feedback, approx. 40–60 min/stage.
- Online exam—average 22.4 min/student.
The course plan and the description of the necessary tools were shared with the students before the first session and discussed during the first online consultation.
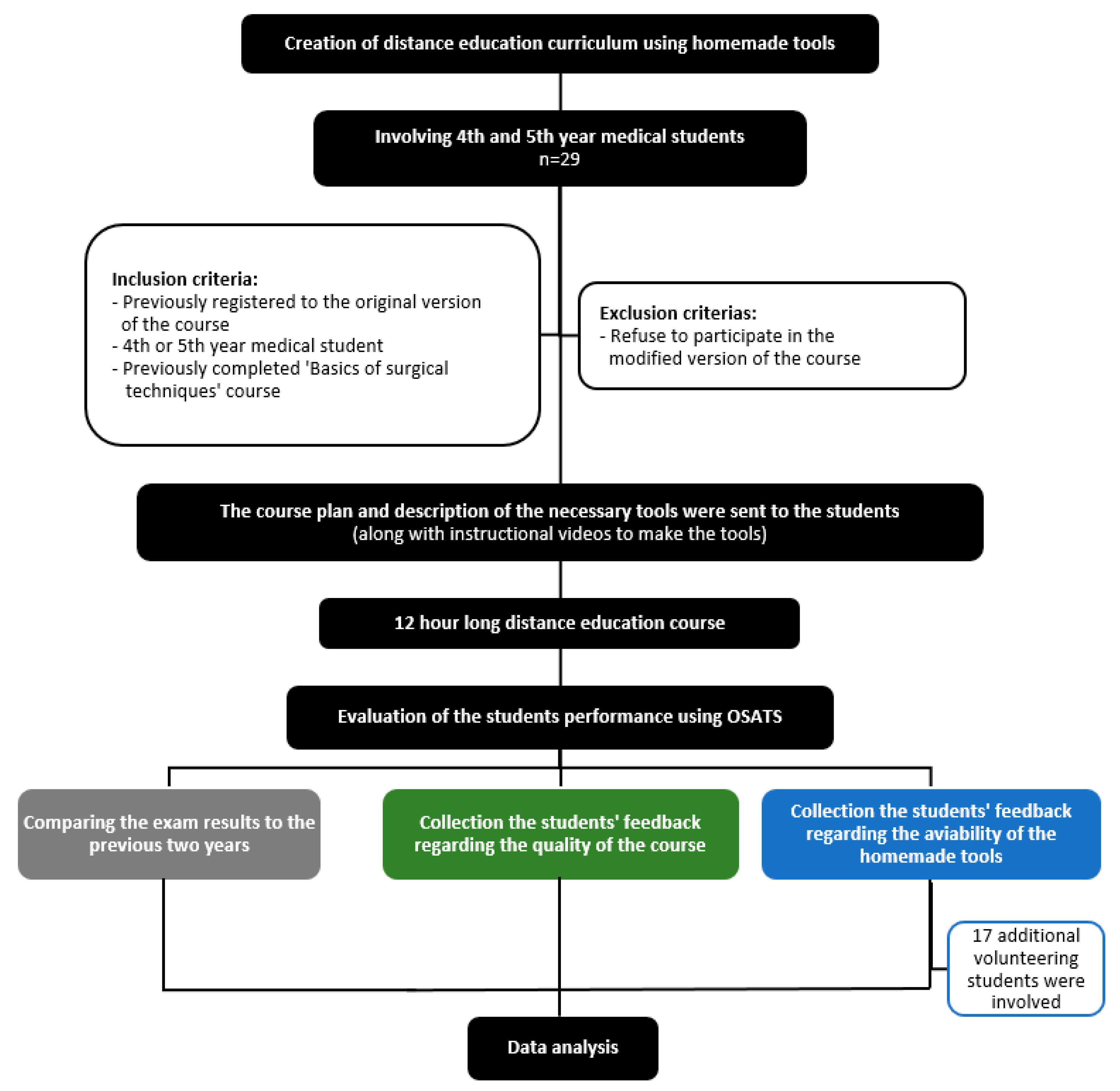
The study protocol is summarized in Figure 1.
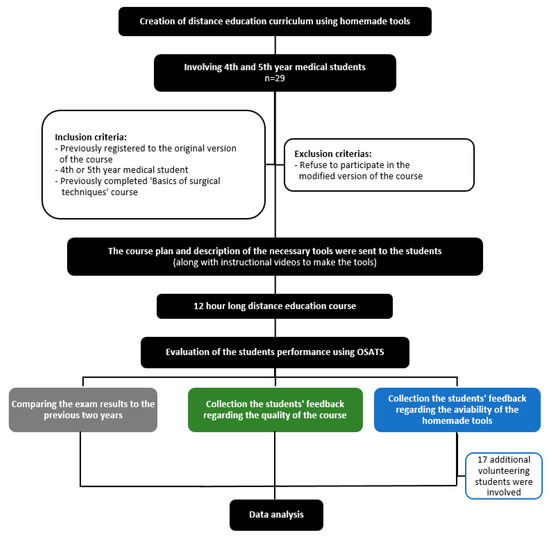
Figure 1.
Modified CONSORT diagram of the study protocol.
2.1. Study Setting
Study type: Prospective Observational Study.
Place and time: University of Pécs, Medical School, Hungary, 5 March 2020–15 April 2020.
2.2. Population of the Study
Thirty students were included in the study. They were 4th- and 5th-year medical students who originally applied for the elective course of the simulation education center of the university to improve their basic surgical skills. All students had previously completed the compulsory basic surgery course, so they had experience in surgical simulation and in the use of trainers.
Students who did not undertake the course in the below-demonstrated form were given the opportunity to cancel their registration subsequently. One student took this opportunity, decreasing the final study population to 29 students.
Additionally, 17 students from the Surgical Society of the university volunteered to test the homemade trainers and give feedback.
Microsoft Teams (version 1.3.00.4461, Microsoft Corp., Redmond, Washington, DC, USA) software was used for online consultation and examination.
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional and Regional Ethical Review Board of University (7719—PTE 2020). Informed Consent Statement: Written informed consent was obtained from study participants. All participants agreed to take part in the study and approved the use of their data for research purposes.
2.3. Knot Tying
The feasibility of the curriculum is summarized in Table 1.

Table 1.
The learning objectives of the original course plan related to knot tying, and its feasibility with homemade tools.
Required tools (Figure 2).

Figure 2.
Required tools for practicing knotting—shoelace, shoe, string, sock (any cloth), paper sheet, a can, thread, rubber ring.
- Suture materials—shoelace or string, for later—thread, yarn, or fishing line.
- Tissue under tension model—shoe (stuffed with socks, if necessary) or rubber band stretched between two objects.
- Easily tearing tissue model—empty can with a simple paper underneath. A circle was drawn around the bottom of the can.
Tasks.
- Acquire the correct movements of knot tying with a shoelace or a string, using a stable base such as a knob or a door handle.
- Obtain the correct movements of knot tying by using surgical suture-like threads, such as a fishing line or a longer piece of yarn attached to a stable base (e.g., knob or door handle).
- Mastering knot tying on tissues under tension by practicing on a shoe or a rubber band. The goal is to pull the eyebrows together with the shoelace as close as possible and keep this tightness when tying the knot without lifting the shoe from the table. Alternatively, tie the stretched rubber band with the least deflection of the band.
- Mastering knot tying on easily tearing tissue by using a can. The level of difficulty could be elevated by reducing the liquid volume inside the can. The goal is to keep the can within the circle drawn onto the paper without lifting it.
A video shows the preparation of the tools and tasks included in Video S1.
2.4. Suturing
The feasibility of the curriculum is summarized in Table 2.

Table 2.
The learning objectives of the original course plan regarding suturing, and its feasibility with homemade tools. 1 Although the students could practice with forceps such as instruments (e.g., eyebrow tweezer), what makes possible to learn the basic holding and movements, but it could not be considered as an unexceptionable replacement.
Required tools (Figure 3).

Figure 3.
Required tools for practicing suturing—any round object as template, forceps, plier, paper clip, traditional sewing needle, banana, sponge, mandarin, orange.
- Needle replacement.
- -
- bending a traditional sewing needle (if possible after heating) along a rolling pin, glass neck, or cardboard curl.
- -
- Straighten a paper clip, cut it over the loop, and then bend it as above.
- -
- Straighten a safety pin, cut it over the loop, and then bend it as above.
- Needle holder replacement.
- -
- Short nose, flat, knurled precision pliers (110–180 mm) or similar.
- -
- Any pliers with a flat jaw and a width of 2–5 mm.
- -
- Nail clipper (does not keep the needle stable due to its edge).
- In order to replace forceps—forceps found in most supermarkets and drugstores.
- -
- Eyebrow tweezers.
- To replace a sewing pad.
- -
- Banana—lies stable on the surface, it has a nearly circular cross-section, a long “wound” can be cut on it, the thickness of the peel is similar to the thickness of the human cutis, and it does not leak juice (the fresher, the better).
- -
- Orange/tangerine—sits stable on the surface; the thickness of the peel is close to the thickness of the human cutis, but only a short “wound” can be cut on it, and juice may leak during exercise (the fresher, the better).
- -
- Dishwashing sponge—sits stable on the surface; the side with a rub is suitable for modeling the cutis on some level, and it wears out slowly.
- -
- Animal skin—pig or chicken, difficult to handle, risk of contamination, and pigskin may be difficult to sew.
Tasks.
- Practicing piercing the needle through the model with the right rolling motion.
- Exercising needle control using dots painted on the model.
- Practicing instrument tie and aligning the edges of the skin through simple knot suturing.
- Practice different types of sutures.
A video showing the preparation of the tools included in Video S2.
2.5. Basics of Laparoscopic Surgery
The feasibility of the curriculum is summarized in Table 3.

Table 3.
The learning objectives of the original course plan regarding laparoscopic skills, and its feasibility with homemade tools. 1 First, with fixed mobile phone, it was impossible to learn camera manipulation, but those students who possess a webcam could fix it to a stick to practice camera handling. 2 Second, although the homemade pelvitrainer can simulate the limited, closed environment, the fixed view does not facilitate in-line visualization, rotation and horizon maintenance. 3 Three, using stick-like tools makes it possible to get used to elongated instruments, although the miss of the special tool-heads and handles restricts its simulation value.
Required tools (Figure 4).
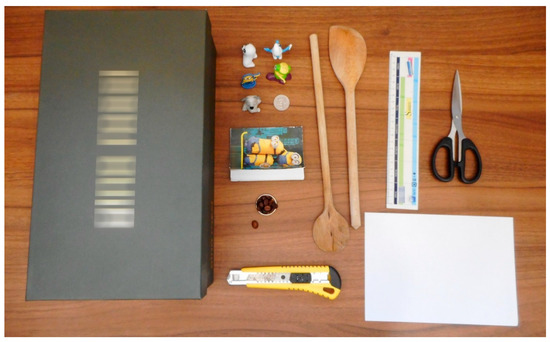
Figure 4.
Required tools for practicing laparoscopy—shoebox, toys and a coin, booklet, beans and a keyring, wooden spoons, a sheet of paper, some tools to prepare.
- Replacement of a pelvitrainer.
- -
- Shoe box or any smaller cardboard box.
- -
- Plastic box with lid.
- Replacement of camera.
- -
- Mobile phone and software/app that allows it to be used as a webcam (e.g., DroidCam, IP Webcam, EpocCam, etc.).
- -
- Webcam or conventional camera.
- -
- Suitable light source (e.g., phone cam light, bicycle light).
- -
- Monitor (notebook, computer, cellphone, television).
- To replace laparoscopic devices.
- -
- Wooden Spoon.
- -
- Any elongated device or stick that is sufficiently rigid, at least 30 cm long but not more than 2 cm in diameter.
Tasks.
- Development of orientation and deep perception in 2D environment—touching targets drawn on a sheet of paper, touching different objects
- Development of hand-eye coordination, triangulation—transferring different objects from point A to point B (the smaller, the rounder the surface, the harder the task will be)
- Development of hand-eye coordination, triangulation—turning the pages of a booklet or notepad
A video showing the preparation of the tools and the tasks is included in Video S3.
2.6. Evaluation of the Tasks and the Feedback of the Students
We assessed students’ efficacy in knot tying and suturing by online method, using OSATS scores correspondent for the past years [16,31], then evaluated them in comparison with results from the previous two years.
The students of the course and the volunteers from the surgical society filled out an online feedback form anonymously following the second online consultation. The students of the course filled out another anonymous feedback after the course as well. Questions concerned the difficulty of purchasing and preparing instruments in form of multiple-choice questions, as well as the Likert-scale and open questions.
Upon statistical analysis, Mann–Whitney U-test was applied (IBM SPSS v23, IBM Corp., Armonk, NY, USA), p < 0.05 was considered a significant deviation.
3. Results
Twenty-six learning objectives were completed out of the 33 that we set for the original course (knot tying 9/9, suturing 14/16, basics of laparoscopy 3/8); a further five objectives were partially executed (suturing 2/16, laparoscopy 3/8). Instruments could only be introduced in a previously recorded video. The given condition was not an eligible process for the comparison study in the case of basic laparoscopic skills due to the usage of the laparoscopic simulator system during the original scenario teaching laparoscopic suturing and laparoscopic knot tying.
Students reached an average of 37.56 ± 6.8 points related to knot tying, whilst it was 39.78 ± 4.56 and 41.21 ± 5.09 points (p = 0.09) in the previous two years. Regarding the suturing, it was 81.26 ± 6.2 points, although, in the last two years, it reached 88.22 ± 5.3 and 87.19 ± 6.1 points (p = 0.03).
Based on the first feedback of the students and volunteers, 91.3% of the students already had all the necessary things at home or could obtain them easily for practicing knotting, 89.1% of them for suturing, and 82.6% for laparoscopy. Only 6.5% of the students could not obtain everything for suturing and 4.3% for laparoscopy (Table 4).

Table 4.
The answers to the first feedback after the second online consultation (filled out by the students of the course and the volunteers as well, the results are presented in a number of answers and percentage).
The students of the course evaluated the course for 4.26 ± 0.89 (on a five-level scale) and 4.86 ± 0.25 when we asked them to take the circumstances also into account. They also assessed all the homemade simulators and tools over 4.00 (on a five-level scale) for a situation such as this (Table 5.). This section may be divided into subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.

Table 5.
The answers of the feedback after the course (filled out only by the students of the course, results are presented in average ± S.D).
4. Discussion
The COVID-19 outbreak fundamentally changed surgical training, which had traditionally been based on attendance education, and hands-on courses shifted to digital platforms [14]. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) created an at-home surgical training for ventral hernia repair with telementoring and porcine tissue models, delivered to the participant’s home 2 days before the course [32]. Although DIY solutions are quite popular today, these methods are not validated, and their feasibility is not supported by reliable data. The present study has focused on the teaching of basic surgical skills utilizing homemade tools through online scenarios. Furthermore, students’ satisfaction was also measured.
Seventy-nine percent of the original learning objectives could be performed completely, and 15% were possible partially. The demonstration of instruments was introduced only in a previously recorded video. There was no opportunity to teach laparoscopic suturing and knot tying. Any paper that was found in the literature where learning objectives of a regular course were compared with an emergency situation (or alternative homemade) solution.
In case students have been provided with a needle holder, surgical needles, and forceps, the total of learning objectives would reach 84% (making it possible to fulfill “Knowledge of the tools needed for wound closure, mastering their utilization/application” and “Proper use of forceps” objectives). With the supply of laparoscopic forceps and needle holders, it would be 97% (making it possible to fulfill “To adapt to the elongated laparoscopic instruments”, “Familiarize with the equipment and instruments”, and “To be able to suture and tie knots with laparoscopic instruments” objectives). However, the main aim of our study was to explore alternative uses of household tools with some modifications to develop surgical skills and competencies.
Students produced milder results in both suturing and knot tying tasks. Although the most significant deviation was in suturing, the scores only decreased by 7%. This is possibly due to the complex educational environment, as well as the simple fact that symmetrical sutures are difficult to make with needles bent by hand. In addition, the lack of real-time feedback during practice can also contribute to reduced effectiveness, as good skills are not reinforced, and incorrect movements are not corrected. Immediate feedback is crucial for patient safety [33]. Bonrath et al. found that residents who have received continuous coaching during surgery have achieved better results on a procedure-specific skill scale and made fewer surgical errors compared to those who did not receive feedback [34].
The necessary tools for the homemade simulators were available or easily obtainable for 82% of the students, and only 6.5% of them could not purchase anything. The mechanic plier and the needle proved to be the most problematic item to obtain. Some students reported the breaking of the traditional sewing needle through bending, which could be prevented by heating the metal, although it makes the procedure more dangerous.
There are more examples in the literature about using DIY, homemade or simple organic models to train suturing or other basic surgical skills [27,28,29,35]. Malaysian authors published a DIY surgical simulation kit. Tools from a hardware store (foam mat, plywood cut, wall cable organizer, nails, plastic water bottles, etc.) were used for knotting, simulating skin- (interrupted- and running suture lines), vascular and intestinal sutures costing USD 10 [36]. In the residency preparation course of the Royal College of Surgeons in Ireland (RCSI), flexor tendon repair was trained using pig’s trotter or sausage, skin sutures using orange and lemon, and end-to-end vascular anastomosis with the help of 2 min parboiled penne pasta. Necessary instruments and self-retaining retractors were provided for the participants [37]. Hoopes et al. reported simple household tools to simulate hysterectomy, colporrhaphy, and vaginal wall dissection using plastic flower pots, rubber rings, zip ties, gauze, foam balls, pool noodles, etc. The cost of each kit ranges from USD 20 to USD 50 [13]. Similar to our findings, these studies found the presented low-cost simulators as an acceptable replacement for the commercially available options, although these articles also presumed that the students are equipped with all the required tools. We did not find any paper in the reviewed literature where also the surgical instruments were replaced with homemade tools.
DIY laparoscopic training boxes are widely available in the literature prepared by cardboard boxes or wood with commercially used web cameras and any light sources [22,23,24,25]. For facilitating training, matches, matchbox, small objects, surgical needles, rubber rings, and gauze are inserted into the box. For proper usage, a screen (laptop, monitor, TV) and laparoscopic instruments are also needed. The disadvantages of these simulation boxes are that they are difficult to obtain, as they are commercially not available, and mainly could be purchased in sets and not separately [38]. Our version of the DIY pelvitrainer does not differ significantly from the previously published training boxes, although we had to replace the laparoscopic instruments and develop tasks using homemade tools as well.
We believe this way of teaching was acceptable for the students. Only one student asked for the cancellation of her registration subsequently. She judged the risk of obtaining the missing tools too high. The accomplishing students evaluated the course for 4.26 in general and 4.86 considering the circumstances. Our results harmonize with data available in the literature. The students usually evaluate these kinds of DIY methods highly [13,36,37]. All the homemade task trainers and tools were assessed over 4 on a 5-level scale as an acceptable substitution for a situation such as this; however, the needle holder and needle were evaluated for 3.23 and 3.15 in general.
Overall, the proposed complex methodology and the developed set of tools are found effective in the distance education of basic surgical skills. It can be a complementary element of the continuously developing field of medical simulation education [39]. Furthermore, it can effectively reflect emergency situations such as a global pandemic or the ongoing Ukrainian war situation, which has a major impact on the local healthcare system [40,41].
Limitations
The most important limitation of this paper is the narrow study population. Twenty-nine students were involved in the study group (supported by 17 other volunteers regarding the tools’ evaluation), and retrospectively 60 students to the control group. The limited opportunities at the time of study did not make us possible to increase the number of the involved students, and the changes in the circumstances did not allow for extending the study group.
Studying the test results from the previous years only provides an approximate comparison with the recent results. Neither the training nor the structure of the testing was similar. It might be eligible to demonstrate that there was only minor deterioration in results. When the crisis is over, a retest may be needed in person to compare the effectiveness of our training system to the general surgical techniques curriculum, which we plan to be the basis of our next study.
Students likely had experience with different training tools before, which might have influenced their answers given to the assessment of substitutional tools.
5. Conclusions
An innovative and simple way of training basic surgical skills through distance education with homemade tools has been demonstrated successfully with this study. To our knowledge, this is the first study where not only the simulators but the surgical instruments were replaced with household tools. We could apply this way of training in the teaching of basic knotting, suturing, and laparoscopic skills—except for special instrument handling or laparoscopic suturing—with acceptable efficiency and student satisfaction. At least the presented curriculum and way of evaluation are reproducible for further investigations on distance education.
New findings of the study:
- By using household tools, most of the basic surgical skills course’s original learning objectives could be performed (79% completely, 15% partially).
- The necessary tools for practicing basic surgical skills at home were available for almost all students (93.5% could obtain them).
- Students’ exam results did not deteriorate greatly (with only 7%).
- The students were generally satisfied with this way of teaching, especially when the circumstances were considered (they evaluated the course for 4.86 on a 5-level scale).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/su14148639/s1, Video S1: DIY tools for knotting. Video S2: DIY tools for suturing, Video S3: DIY tools for laparoscopy, Supplementary Material S1: detailed description of the course plan.
Author Contributions
Conceptualization, all author; methodology, Á.T.S., Z.B.P., K.B.-J., P.M. and Z.F.; investigation, Á.T.S., Z.B.P., A.K., E.K., P.V. and D.K.; resources, Á.T.S., P.M. and Z.F.; data curation, Á.T.S. and Z.B.P.; writing—original draft preparation, Á.T.S.; writing—review and editing, all author; visualization, Á.T.S.; supervision, Z.F.; funding acquisition, Á.T.S. and P.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by grants from National Research, Development, and Innovation Fund of Hungary tenders [EFOP-3.6.1-16-2016-00004 and GINOP-2.3.2.-15-2016-00022]. The work was also supported by the [NTP-NFTÖ-20-B-0137] for A.S. and [NTP-NFTÖ-20-0071]—for P.M, granted by the Hungarian Government. Project no. TKP2021-NVA-06 has been implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the TKP2021-NVA funding scheme.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional and Regional Ethical Review Board of University (8443—PTE 2020).
Informed Consent Statement
Written informed consent was obtained from study participants. All participant agreed to take part in the study and approved to use their data for research purposes.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to data protection of the participants but are available from the corresponding author on reasonable request.
Acknowledgments
We are grateful to Gábor Markó, who made his work-room available for us to experiment with the most adequate instruments and methods. Furthermore, we thank Surgical Society of University of Pécs for their advice and ideas. Some parts of this paper were previously published in Academic Medicine as a 343 word-long invited Letter to Editor [42]. In spite of this fact, we believe this paper contains a large quantity of unpublished data, as the details of the course setting and assessment, the availability of the tools, exams result, feedback of the students, elaborated conclusions, etc., to make it capable as an original manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Theodoulou, I.; Nicolaides, M.; Athanasiou, T.; Papalois, A.; Sideris, M. Simulation-Based Learning Strategies to Teach Undergraduate Students Basic Surgical Skills: A Systematic Review. J. Surg. Educ. 2018, 75, 1374–1388. [Google Scholar] [CrossRef] [PubMed]
- Karmali, R.J.; Siu, J.M.; You, D.Z.; Spano, S.; Winthrop, A.L.; Rudan, J.F.; Reznick, R.K.; Sanfilippo, A.T.; Belliveau, P. The Surgical Skills and Technology Elective Program (SSTEP): A comprehensive simulation-based surgical skills initiative for preclerkship medical students. Am. J. Surg. 2018, 216, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Sacks, D.; Baxter, B.; Campbell, B.C.V.; Carpenter, J.S.; Cognard, C.; Dippel, D.; Eesa, M.; Fischer, U.; Hausegger, K.; Hirsch, J.A.; et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weidert, S.; Andress, S.; Suero, E.; Becker, C.; Hartel, M.; Behle, M.; Willy, C. 3D printing in orthopedic and trauma surgery education and training: Possibilities and fields of application. Unfallchirurg 2019, 122, 444–451. [Google Scholar] [CrossRef]
- Yanik, E.; Intes, X.; Kruger, U.; Yan, P.; Diller, D.; Van Voorst, B.; Makled, B.; Norfleet, J.; De, S. Deep neural networks for the assessment of surgical skills: A systematic review. J. Def. Model. Simul. 2022, 19, 159–171. [Google Scholar] [CrossRef]
- Lu, J.; Cuff, R.F.; Mansour, M.A. Simulation in surgical education. Am. J. Surg. 2021, 221, 509–514. [Google Scholar] [CrossRef]
- Dedeilia, A.; Sotiropoulos, M.G.; Hanrahan, J.G.; Janga, D.; Dedeilias, P.; Sideris, M. Medical and Surgical Education Challenges and Innovations in the COVID-19 Era: A Systematic Review. In Vivo 2020, 34, 1603–1611. [Google Scholar] [CrossRef]
- Khan, K.S.; Keay, R.; McLellan, M.; Mahmud, S. Impact of the COVID-19 pandemic on core surgical training. Scott. Med. J. 2020, 65, 133–137. [Google Scholar] [CrossRef]
- Stojan, J.; Haas, M.; Thammasitboon, S.; Lander, L.; Evans, S.; Pawlik, C.; Pawilkowska, T.; Lew, M.; Khamees, D.; Peterson, W.; et al. Online learning developments in undergraduate medical education in response to the COVID-19 pandemic: A BEME systematic review: BEME Guide No. 69. Med. Teach. 2022, 44, 109–129. [Google Scholar] [CrossRef]
- Sinha, M.K.; Barman, A. Letter to the Editor: Undergraduate Surgical Training during COVID 19 Pandemic—The Lessons Learned. World J. Surg. 2021, 45, 3240–3241. [Google Scholar] [CrossRef]
- Calhoun, K.E.; Yale, L.A.; Whipple, M.E.; Allen, S.M.; Wood, D.E.; Tatum, R.P. The impact of COVID-19 on medical student surgical education: Implementing extreme pandemic response measures in a widely distributed surgical clerkship experience. Am. J. Surg. 2020, 220, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.A.; Pizanis, A.; Fischer, G.; Langer, F.; Scherber, P.; Stutz, J.; Orth, M.; Pohlemann, T.; Fritz, T. COVID-19: A catalyst for the digitization of surgical teaching at a German University Hospital. BMC Med. Educ. 2022, 22, 308. [Google Scholar] [CrossRef]
- Hoopes, S.; Pham, T.; Lindo, F.M.; Antosh, D.D. Home Surgical Skill Training Resources for Obstetrics and Gynecology Trainees during a Pandemic. Obstet. Gynecol. 2020, 136, 56–64. [Google Scholar] [CrossRef]
- Tuma, F.; Kamel, M.K.; Shebrain, S.; Ghanem, M.; Blebea, J. Alternatives surgical training approaches during COVID-19 pandemic. Ann. Med. Surg. 2021, 62, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Laloo, R.; Santhosh Karri, R.; Wanigasooriya, K.; Beedham, W.; Darr, A.; Layton, G.R.; Logan, P.; Tan, Y.; Mittapalli, D.; Patel, T.; et al. The perceived global impact of the COVID-19 pandemic on doctors’ medical and surgical training: An international survey. Int. J. Clin. Pract. 2021, 75, e14314. [Google Scholar] [CrossRef] [PubMed]
- Pintér, Z.B.; Maróti, P.; Kopjár, E.; Gasz, B.; Duga, Z.; Rendeki, S.; Nagy, B.; Füzesi, Z.; Schlégl, Á.T. Effectivity of Distance Learning in the Training of Basic Surgical Skills—A Randomized Controlled Trial. Sustainability 2022, 14, 4727. [Google Scholar] [CrossRef]
- Fritz, T.; Stachel, N.; Braun, B.J. Evidence in surgical training—A review. Innov. Surg. Sci. 2019, 4, 7–13. [Google Scholar] [CrossRef]
- Jayakumar, N.; Brunckhorst, O.; Dasgupta, P.; Khan, M.S.; Ahmed, K. e-Learning in Surgical Education: A Systematic Review. J. Surg. Educ. 2015, 72, 1145–1157. [Google Scholar] [CrossRef]
- Tarpada, S.P.; Morris, M.T.; Burton, D.A. E-learning in orthopedic surgery training: A systematic review. J. Orthop. 2016, 13, 425–430. [Google Scholar] [CrossRef]
- Maertens, H.; Madani, A.; Landry, T.; Vermassen, F.; Van Herzeele, I.; Aggarwal, R. Systematic review of e-learning for surgical training. Br. J. Surg. 2016, 103, 1428–1437. [Google Scholar] [CrossRef] [Green Version]
- Ovaere, S.; Zimmerman, D.D.E.; Brady, R.R. Social Media in Surgical Training: Opportunities and Risks. J. Surg. Educ. 2018, 75, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Li, M.M.; George, J. A systematic review of low-cost laparoscopic simulators. Surg. Endosc. 2017, 31, 38–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gravante, G.; Venditti, D. A systematic review on low-cost box models to achieve basic and advanced laparoscopic skills during modern surgical training. Surg. Laparosc. Endosc. Percutan. Tech. 2013, 23, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Montanari, E.; Schwameis, R.; Louridas, M.; Göbl, C.; Kuessel, L.; Polterauer, S.; Husslein, H. Training on an inexpensive tablet-based device is equally effective as on a standard laparoscopic box trainer: A randomized controlled trial. Medicine 2016, 95, e4826. [Google Scholar] [CrossRef]
- Soriero, D.; Atzori, G.; Barra, F.; Pertile, D.; Massobrio, A.; Conti, L.; Gusmini, D.; Epis, L.; Gallo, M.; Banchini, F.; et al. Development and Validation of a Homemade, Low-Cost Laparoscopic Simulator for Resident Surgeons (LABOT). Int. J. Environ. Res. Public Health 2020, 17, 323. [Google Scholar] [CrossRef] [Green Version]
- Dastur, N. DIY surgical knot-tying tool. Ann. R. Coll. Surg. Engl. 2009, 91, 268. [Google Scholar] [CrossRef]
- Wong, K.; Bhama, P.K.; d’Amour Mazimpaka, J.; Dusabimana, R.; Lee, L.N.; Shaye, D.A. Banana fruit: An “appealing” alternative for practicing suture techniques in resource-limited settings. Am. J. Otolaryngol. 2018, 39, 582–584. [Google Scholar] [CrossRef]
- Kumaresan, R.; Pendayala, S.; Srinivasan, B.; Kondreddy, K. A simplified suturing model for preclinical training. Indian. J. Dent. Res. 2014, 25, 541–543. [Google Scholar] [CrossRef]
- Kumaresan, R.; Karthikeyan, P. An Inexpensive Suturing Training Model. J. Maxillofac. Oral. Surg. 2014, 13, 609–611. [Google Scholar] [CrossRef] [Green Version]
- Uppal, N.; Saldanha, S. Low-cost suturing training model for use in developing nations. Br. J. Oral. Maxillofac. Surg. 2012, 50, e13–e14. [Google Scholar] [CrossRef]
- Pintér, Z.; Kardos, D.; Varga, P.; Kopjár, E.; Kovács, A.; Than, P.; Rendeki, S.; Czopf, L.; Füzesi, Z.; Schlégl, Á.T. Effectivity of near-peer teaching in training of basic surgical skills––A randomized controlled trial. BMC Med. Educ. 2021, 21, 156. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, J.A.; Schwarz, E.; Paige, J.; Dort, J.; Bachman, S. At-home hands-on surgical training during COVID-19: Proof of concept using a virtual telementoring platform. Surg. Endosc. 2021, 35, 1963–1969. [Google Scholar] [CrossRef]
- Hoffman, R.L.; Petrosky, J.A.; Eskander, M.F.; Selby, L.V.; Kulaylat, A.N. Feedback fundamentals in surgical education: Tips for success. Bull. Am. Coll. Surg. 2015, 100, 35–39. [Google Scholar] [PubMed]
- Bonrath, E.M.; Dedy, N.J.; Gordon, L.E.; Grantcharov, T.P. Comprehensive Surgical Coaching Enhances Surgical Skill in the Operating Room: A Randomized Controlled Trial. Ann. Surg. 2015, 262, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Triveni, K.; Shruti, S.L.; Varsha, R.; Govind, B.; Anuja, H.; Pranav, L. Comparative evaluation of two suturing models for preclinical training. J. Oral. Res. 2019, 11, 20–24. [Google Scholar] [CrossRef]
- Nah, S.A.; Singaravel, S.; Sanmugam, A. Do-It-Yourself Surgical Simulation Kits: One Academic Medical Center’s Response to the COVID-19 Pandemic in Malaysia. Acad. Med. 2021, 96, e3. [Google Scholar] [CrossRef]
- Heskin, L.; Morris, M.; Traynor, O. Surgical skills training and practice at home: When your grocery store becomes your simulator supplier. Am. J. Surg. 2021, 222, 292–293. [Google Scholar] [CrossRef]
- Parente, G.; De Marziani, L.; Cordola, C.; Gargano, T.; Libri, M.; Lima, M. Training minimally invasive surgery’s basic skills: Is expensive always better? Pediatr. Surg. Int. 2021, 37, 1287–1293. [Google Scholar] [CrossRef]
- Bogár, P.Z.; Tóth, L.; Rendeki, S.; Mátyus, L.; Németh, N.; Boros, M.; Nagy, B.; Nyitrai, M.; Maróti, P. The present and the future of medical simulation education in Hungary. Orv. Hetil. 2020, 161, 1078–1087. [Google Scholar] [CrossRef]
- Unukovych, D. Surgical services during the war in Ukraine: Challenges and call for help. Br. J. Surg. 2022. [Google Scholar] [CrossRef]
- Kazatchkine, M. Ukrainian war: An economic crisis in Eastern Europe and Central Asia will lead to a health crisis. BMJ 2022, 376, o793. [Google Scholar] [CrossRef] [PubMed]
- Schlégl, Á.T.; Pintér, Z.; Kovács, A.; Kopjár, E.; Varga, P.; Kardos, D.; Gasz, B.; Füzesi, Z. Teaching Basic Surgical Skills Using Homemade Tools in Response to COVID-19. Acad. Med. 2020, 95, e7. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).