Indonesia’s Climate-Related Disasters and Health Adaptation Policy in the Build-Up to COP26 and Beyond
Abstract
:1. Introduction
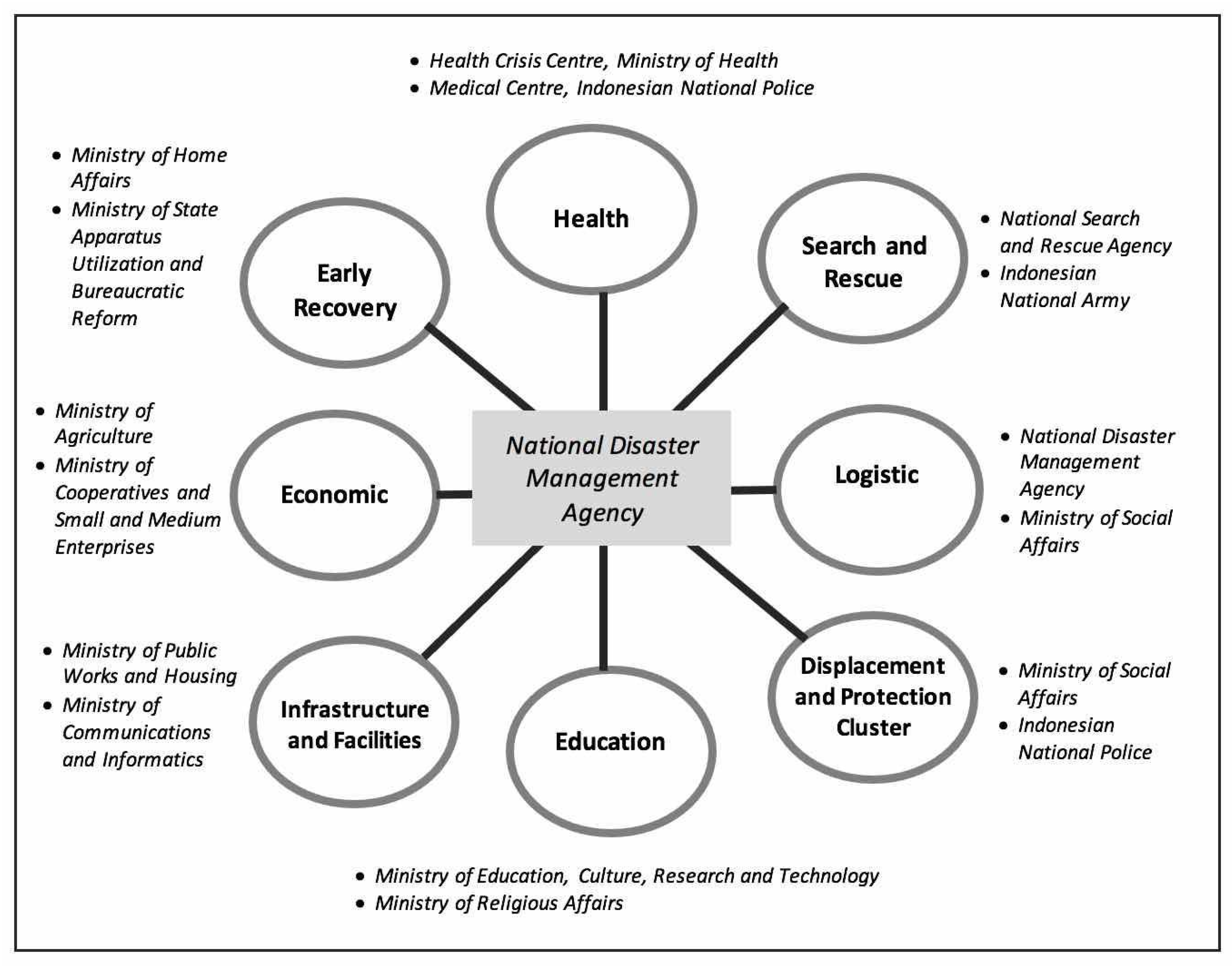
2. Disaster Management Governance, Policy and Strategy in Indonesia
3. Method
3.1. Desktop Review on Climate-Related Disaster Policy Addressing Health Impacts
3.1.1. Search Strategy and Document Selection
3.1.2. Data Extraction
3.2. Stakeholder Consultation
3.3. Data Analysis
4. Results and Discussions
4.1. Overview of Reviewed Documents
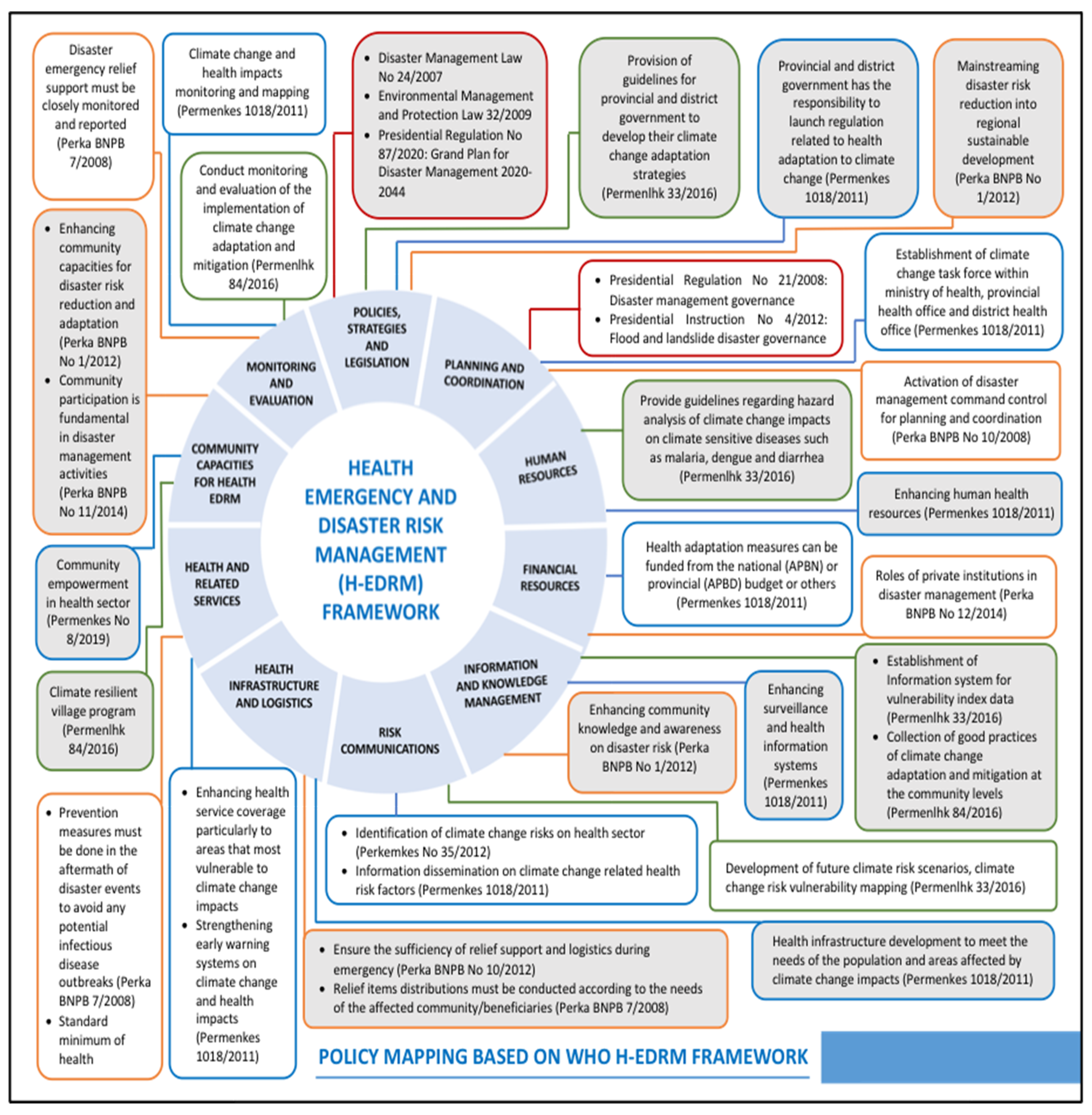
4.2. Analyzing Using WHO Health-EDRM Framework
4.2.1. Policies, Strategies and Legislation
4.2.2. Planning and Coordination
4.2.3. Human Resources
4.2.4. Financial Resources
4.2.5. Information and Knowledge Management
4.2.6. Risk Communications
4.2.7. Health Infrastructure and Logistics
4.2.8. Health and Related Services
4.2.9. Community Capacities for Health EDRM
4.2.10. Monitoring and Evaluation
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sendai Framework for Disaster Risk Reduction 2015–2030, United Nations International Strategy for Disaster Reduction (UNISDR). Available online: https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030 (accessed on 14 March 2021).
- World Health Organization. Health Emergency and Disaster Risk Management Framework. 2019. Available online: https://www.who.int/hac/techguidance/preparedness/health-emergency-and-disaster-risk-management-framework-eng.pdf (accessed on 14 March 2021).
- Field, C.B.; Barros, V.; Stocker, T.F.; Dahe, Q. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation: Special Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar]
- Annex, I. Managing the risks of extreme events and disasters to advance climate change adaptation. Sciences 2012, 10, 97–104. [Google Scholar]
- Malilay, J.; Heumann, M.; Perrotta, D.; Wolkin, A.F.; Schnall, A.H.; Podgornik, M.N.; Simms, E.F. The role of applied epidemiology methods in the disaster management cycle. Am. J. Public Health 2014, 104, 2092–2102. [Google Scholar] [CrossRef] [PubMed]
- Botchey, I.M.; Paruk, F.; Hung, Y.W.; Mehmood, A.; Bachani, A.; Hassan, S.; Hyder, A.A. Establishing mHealth Injury Surveillance Systems in Kenya. Prehospital Disaster Med. 2017, 32, S61. [Google Scholar] [CrossRef] [Green Version]
- Karo, B.; Haskew, C.; Khan, A.S.; Polonsky, J.A.; Mazhar, M.K.A.; Buddha, N. World Health Organization early warning, alert and response system in the Rohingya crisis, Bangladesh, 2017–2018. Emerg. Infect. Dis. 2018, 24, 2074. [Google Scholar] [CrossRef] [PubMed]
- Sumaryana, A.U.; Utami, S.B.; Pancasilawan, R. Creating Sustainable Disaster Management Collaboration in Indonesia. Int. J. Civ. Eng. Technol. 2019, 10, 2435–2440. [Google Scholar]
- Fahlevi, H.; Indriani, M.; Oktari, R.S. Is the Indonesian disaster response budget correlated with disaster risk? Jàmbá: J. Disaster Risk Stud. 2019, 11, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nurdin, N.; Rafliana, I.; Hidayati, S.; Oktari, R.S.; Djalante, R. Integrating Disaster Risk Reduction and Climate Change Adaptation into School Curricula: From National Policy to Local Implementation. In Disaster Risk Reduction in Indonesia; Djalante, R., Garschagen, M., Thomalla, F., Shaw, R., Eds.; Disaster Risk Reduction (Methods, Approaches and Practices); Springer: Cham, Switzerland, 2017; pp. 213–234. [Google Scholar]
- Simarmata, H.A.; Suryandaru, R.W. Institutions and planning: A reflection from disaster management planning in Indonesia. In Global Sustainability; Werlen, B., Ed.; Springer: Cham, Switzerland, 2015; pp. 239–265. [Google Scholar]
- Indonesian Disaster Information Data (DIBI-BNPB). Available online: https://www.dibi.bnpb.go.id (accessed on 14 March 2021).
- Centre for Research on the Epidemiology of Disasters—CRED. Disaster Year in Review 2020: Global Trends and Perspectives; Cred Crunch; Université Catholique de Louvain: Brussels, Belgium, 2021; Volume 62, p. 2. [Google Scholar]
- Keim, M.E. Climate-Related Disasters: The Role of Prevention for Managing Health Risk. In Global Climate Change and Human Health: From Science to Practice; Lemery, J., Knowlton, K., Sorensen, C., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2021; p. 25. [Google Scholar]
- Benevolenza, M.A.; DeRigne, L. The impact of climate change and natural disasters on vulnerable populations: A systematic review of literature. J. Hum. Behav. Soc. Environ. 2019, 29, 266–281. [Google Scholar] [CrossRef]
- Banwell, N.; Rutherford, S.; Mackey, B.; Chu, C. Towards improved linkage of disaster risk reduction and climate change adaptation in health: A review. Int. J. Environ. Res. Public Health 2018, 15, 793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. COP26 Health Programme. 2021. Available online: https://www.who.int/initiatives/cop26-health-programme (accessed on 14 March 2021).
- World Health Organization. Countries Commit to Develop Climate-Smart Health Care at COP26 UN Climate Conference. 2021. Available online: https://www.who.int/news/item/09-11-2021-countries-commit-to-develop-climate-smart-health-care-at-cop26-un-climate-conference (accessed on 14 March 2021).
- Indonesian Law No. 24 of 2007 Concerning Disaster Management. Available online: https://www.ifrc.org/docs/IDRL/956EN.pdf (accessed on 14 March 2021).
- Indonesian Law No. 32 of 2009 Concerning Environmental Protection and Management. Available online: https://www.fao.org/faolex/results/details/en/c/LEX-FAOC097643/ (accessed on 14 March 2021).
- Indonesian Law No. 36 of 2009 Concerning Health. Available online: https://www.ilo.org/dyn/natlex/natlex4.detail?p_lang=en&p_isn=91185 (accessed on 14 March 2021).
- Indonesian Law No. 1 of 2014 Concerning the Amendment to Law No. 27 of 2007 on Management of Coastal Areas and Small Islands. Available online: https://peraturan.bpk.go.id/Home/Details/38521/uu-no-1-tahun-2014 (accessed on 14 March 2021).
- Decree of the Head of BNPB No. 173 of 2014 Concerning National Clusters for Disaster Management. Available online: https://bnpb.go.id/uploads/regulation/1085/Perka%20No%2014%20Tahun%202014.pdf (accessed on 14 March 2021).
- Presidential Regulation, No. 16 of 2015 concerning the Ministry of Environment and Forestry. Available online: https://peraturan.bpk.go.id/Home/Details/41738/perpres-no-16-tahun-2015 (accessed on 14 March 2021).
- Ministry of Environment and Forestry Regulation No: P.33/Menlhk/Setjen/Kum.1/3/2016 Concerning the Guideline to Develop Climate Change Adaptation Plan. Available online: http://ditjenppi.menlhk.go.id/reddplus/images/resources/permen/permen33.pdf (accessed on 14 March 2021).
- Ministry of Environment and Forestry Regulation Number P.84/Menlhk/Setjen/Kum.1/11/2016 Concerning Climate-Resilient Village Program. Available online: http://jdih.menlhk.co.id/uploads/files/P.84.pdf (accessed on 14 March 2021).
- Ministry of Health Regulation No. 1018 of 2011 Concerning Health Sector Adaptation Strategy to the Climate Change Impact. Available online: https://peraturan.go.id/common/dokumen/bn/2011/bn344-2011.pdf (accessed on 14 March 2021).
- Ministry of Health Regulation No. 8 of 2019 on Community Empowerment in Health Sector. Available online: https://peraturan.bpk.go.id/Home/Details/111722/permenkes-no-8-tahun-2019 (accessed on 14 March 2021).
- World Health Organization. Framework for Action in Building Health Systems Resilience to Climate Change in South-East Asia Region, 2017–2022; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Head of National Agency for Disaster Management No. 11 of 2014 Concerning Community Participation in Disaster Management. Available online: https://bnpb.go.id/berita/perka-bnpb-no-11-2014-tentang-peran-serta-masyarakat-dalam-penanggulangan-bencana (accessed on 14 March 2021).
- Head of National Agency for Disaster Management No. 14 of 2014 Concerning Handling, Protection and Participation of Persons with Disabilities in Disaster Management. Available online: https://bnpb.go.id/berita/perka-bnpb-no-14-2014-tentang-penanganan-perlindungan-dan-partisipasi-penyandang-disabilitas-dalam-pb (accessed on 14 March 2021).
- Head of National Agency for Disaster Management No. 10 of 2014 concerning Guidelines for Verification of Financial Accountability Documents within BNPB. Available online: https://bnpb.go.id/produk-hukum/peraturan-kepala-bnpb/peraturan-kepala-bnpb-no-10-tahun-2014 (accessed on 14 March 2021).
- Head of National Agency for Disaster Management No. 13 of 2014 concerning Gender Mainstreaming in Disaster Management. Available online: https://bnpb.go.id/berita/perka-bnpb-no-13-2014-tentang-pengarusutamaan-gender-di-bidang-pb (accessed on 14 March 2021).
- Head of National Agency for Disaster Management No. 10 of 2012 Concerning Management of Logistics Assistance during Emergencies. Available online: https://bnpb.go.id/produk-hukum/peraturan-kepala-bnpb/peraturan-kepala-bnpb-no-10-tahun-2012 (accessed on 14 March 2021).
- Head of National Agency for Disaster Management No. 10 of 2008 Concerning Disaster Emergency Response Command. Available online: https://www.bnpb.go.id/index.php/produk-hukum/peraturan-kepala-bnpb/peraturan-kepala-bnpb-no-10-tahun-2008 (accessed on 14 March 2021).
- Head of National Agency for Disaster Management No. 15 of 2011 Concerning Guidelines for Post-Disaster Needs Assessment. Available online: https://www.bnpb.go.id/index.php/produk-hukum/peraturan-kepala-bnpb/peraturan-kepala-bnpb-no-15-tahun-2011 (accessed on 14 March 2021).
- Presidential Regulation No. 87 of 2020 on the Indonesian Grand Plan for Disaster Management 2022–2044. Available online: https://peraturan.bpk.go.id/Home/Details/146481/perpres-no-87-tahun-2020 (accessed on 14 March 2021).
- World Health Organization. Climate Change and Human Health: An Assessment (No. WHO/EHG/96.7). Available online: https://apps.who.int/iris/handle/10665/62989 (accessed on 14 March 2021).
- McMichael, A.J.; Kovats, R.S. Climate change and climate variability: Adaptations to reduce adverse health impacts. Environ. Monit. Assess. 2000, 61, 49–64. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Climate Change and Human Health: Impact and Adaptation. Available online: https://apps.who.int/iris/handle/10665/66776 (accessed on 14 March 2021).
- Grambsch, A.; Menne, B. Adaptation and adaptive capacity in the public health context. In Climate Change and Health: Risks and Responses; McMichael, A.J., Campbell-Lendrum, D.H., Corvalan, C.F., Ebi, K.L., Githeko, A., Scheraga, J.D., Woodward, A., Eds.; World Health Organization: Geneva, Switzerland, 2003; pp. 220–236. [Google Scholar]
- EM-DAT. The International Disaster Database. Centre for Research on the Epidemiology of Disaster (CRED). EM-DAT Glossary. Available online: https://www.emdat.be/Glossary (accessed on 14 March 2021).
- UN Office for Disaster Risk Reduction (UNDRR). Terminology. Available online: www.undrr.org/terminology (accessed on 14 March 2021).
- Lo, S.T.T.; Chan, E.Y.Y.; Chan, G.K.W.; Murray, V.; Abrahams, J.; Ardalan, A.; Kayano, R.; Yau, J.C.W. Health emergency and disaster risk management (Health-EDRM): Developing the research field within the Sendai framework paradigm. Int. J. Disaster Risk Sci. 2017, 8, 145–149. [Google Scholar] [CrossRef]
- Kayano, R.; Chan, E.Y.; Murray, V.; Abrahams, J.; Barber, S.L. WHO thematic platform for health emergency and disaster risk management research network (TPRN): Report of the Kobe expert meeting. Int. J. Environ. Res. Public Health 2019, 16, 1232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kayano, R.; Nomura, S.; Abrahams, J.; Huda, Q.; Chan, E.Y.; Murray, V. Progress towards the development of research agenda and the launch of knowledge hub: The who thematic platform for health emergency and disaster risk management research network (health edrm rn). Int. J. Environ. Res. Public Health 2021, 18, 4959. [Google Scholar] [CrossRef] [PubMed]
- Wright, N.; Fagan, L.; Lapitan, J.M.; Kayano, R.; Abrahams, J.; Huda, Q.; Murray, V. Health emergency and disaster risk management: Five years into implementation of the Sendai framework. Int. J. Disaster Risk Sci. 2020, 11, 206–217. [Google Scholar] [CrossRef]
- World Health Organization. International Health Regulations. Available online: https://www.who.int/publications/i/item/9789241580496 (accessed on 14 March 2021).
- Hung, K.K.; Mashino, S.; Chan, E.Y.; MacDermot, M.K.; Balsari, S.; Ciottone, G.R.; Della Corte, F.; Dell’Aringa, M.F.; Egawa, S.; Evio, B.D.; et al. Health Workforce Development in Health Emergency and Disaster Risk Management: The Need for Evidence-Based Recommendations. Int. J. Environ. Res. Public Health 2021, 18, 3382. [Google Scholar] [CrossRef]
- Nomura, S.; Kayano, R.; Egawa, S.; Harada, N.; Koido, Y. Expected Scopes of Health Emergency and Disaster Risk Management (Health EDRM): Report on the Expert Workshop at the Annual Conference for the Japanese Association for Disaster Medicine 2020. Int. J. Environ. Res. Public Health 2021, 18, 4447. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Sham, T.S.; Shahzada, T.S.; Dubois, C.; Huang, Z.; Liu, S.; Hung, K.K.; Tse, S.L.; Kwok, K.O.; Chung, P.H.; et al. Narrative Review on Health-EDRM Primary Prevention Measures for Vector-Borne Diseases. Int. J. Environ. Res. Public Health 2020, 17, 5981. [Google Scholar] [CrossRef] [PubMed]
- Updated Nationally Determined Contribution Republic of Indonesia. Available online: https://www4.unfccc.int/sites/ndcstaging/PublishedDocuments/Indonesia%20First/Updated%20NDC%20Indonesia%202021%20-%20corrected%20version.pdf (accessed on 14 March 2021).
- Dwirahmadi, F.; Rutherford, S.; Phung, D.; Chu, C. Understanding the operational concept of a flood-resilient urban community in Jakarta, Indonesia, from the perspectives of disaster risk reduction, climate change adaptation and development agencies. Int. J. Environ. Res. Public Health 2019, 16, 3993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Disaster Management Plan 2020–2024. Available online: https://ss.bnpb.go.id/ss/pages/renas-2020 (accessed on 20 October 2021). (In Indonesian).
- Rose, D.A.; Murthy, S.; Brooks, J.; Bryant, J. The evolution of public health emergency management as a field of practice. Am. J. Public Health 2017, 107, S126–S133. [Google Scholar] [CrossRef]
- Review Book in Health Crisis Management Year 2017. Available online: https://www.who.int/docs/default-source/searo/indonesia/non-who-publications/2017-health-emergency-op-centre-information-product---disaster-review-bahasa.pdf?sfvrsn=7e5563ed_2 (accessed on 20 October 2021). (In Indonesian).
- Oktari, R.S.; Munadi, K.; Idroes, R.; Sofyan, H. Knowledge management practices in disaster management: Systematic review. Int. J. Disaster Risk Reduct. 2020, 51, 101881. [Google Scholar] [CrossRef]
- Zhong, M.; Xiao, L.; Zhang, Q.; Jiang, T. Risk Perception, Risk Communication, and Mitigation Actions of Flash Floods: Results from a Survey in Three Types of Communities. Sustainability 2021, 13, 12389. [Google Scholar] [CrossRef]
- Adu-Gyamfi, B.; Shaw, R. Characterizing Risk Communication and Awareness for Sustainable Society: The Case of Foreign Residents in the Tokyo Metropolitan Area of Japan. Sustainability 2021, 13, 5786. [Google Scholar] [CrossRef]
- Ministry of Health. Risk Communication Guideline for Health Crisis Management; Ministry of Health: Jakarta, Indonesia, 2021. [Google Scholar]
- Gan, C.C.; Oktari, R.S.; Nguyen, H.X.; Yuan, L.; Yu, X.; Alisha, K.C.; Hanh, T.T.; Phung, D.T.; Dwirahmadi, F.; Liu, T.; et al. A scoping review of climate-related disasters in China, Indonesia and Vietnam: Disasters, health impacts, vulnerable populations and adaptation measures. Int. J. Disaster Risk Reduct. 2021, 66, 102608. [Google Scholar] [CrossRef]
- Head of National Agency for Disaster Management No. 1/2012 Concerning General Guidelines for Disaster Resilient Villages. Available online: https://bnpb.go.id/berita/perka-bnpb-no-1-2012-tentang-pedoman-umum-desa-kelurahan-tangguh-bencana (accessed on 14 March 2021).
- Ministry of Health. Technical Guideline for Healthy Climate Village; Ministry of Health: Jakarta, Indonesia, 2021; Unpublished Work. [Google Scholar]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| H-EDRM Component | Progress | Challenges | Ways Forward |
|---|---|---|---|
| Policies, Strategies and Legislation |
| Yet, health issues are not well represented in non-health sectors [DR] | Advocacy efforts to ensure that health takes a more central position in multisectoral legislations, approaches, and actions |
| Planning and Coordination | Initiation of a joint secretariat, monitoring dashboard and Non-Government Collaboration Forum [FD] |
| Inter-sectoral cooperation |
| Human Resources | Increasing the capacity of human resources governed by regulation by the Minister of Health [DR] |
|
|
| Financial Resources |
| Disaster risk reduction has not been prioritized by many district/city governments [FD] | Allocate adequate funding by the government and other related institutions |
| Information and Knowledge Management | Several information systems have been developed [DR] |
| Establishment of effective knowledge management mechanism |
| Risk Communications | Identification of risks, information dissemination and development of future risk scenarios and mapping have been regulated [DR] | Dissemination of conflicting information [CM] |
|
| Health Infrastructure and Logistics | Regulation exists to ensure the sufficiency of logistics and relief items distribution [DR] |
| Ensure a safe and secure condition of health infrastructure and logistics |
| Health and Related Services | Focus on increasing health service coverage and strengthening early warning systems on climate change and health impacts [DR] | Lack of attention to vulnerable groups who require special attention/treatment, particularly for health-related needs [CM] |
|
| Community Capacities for Health EDRM | Various initiatives to build resilience at the village level (i.e., Disaster Resilient Village, Healthy Climate Village, Climate Village Program) [DR] | How to build community capacity [CM] | The need for synergy between programs carried out at the village level |
| Monitoring and Evaluation | Monitoring and evaluation with the existing authorities and mechanisms within the institution, both at national and local levels [DR] | No standard indicators to monitor program risk, capacity and implementation [FD] | Integration into existing health sector monitoring systems |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oktari, R.S.; Dwirahmadi, F.; Gan, C.C.R.; Darundiyah, K.; Nugroho, P.C.; Wibowo, A.; Chu, C. Indonesia’s Climate-Related Disasters and Health Adaptation Policy in the Build-Up to COP26 and Beyond. Sustainability 2022, 14, 1006. https://doi.org/10.3390/su14021006
Oktari RS, Dwirahmadi F, Gan CCR, Darundiyah K, Nugroho PC, Wibowo A, Chu C. Indonesia’s Climate-Related Disasters and Health Adaptation Policy in the Build-Up to COP26 and Beyond. Sustainability. 2022; 14(2):1006. https://doi.org/10.3390/su14021006
Chicago/Turabian StyleOktari, Rina Suryani, Febi Dwirahmadi, Connie Cai Ru Gan, Kristin Darundiyah, Pratomo Cahyo Nugroho, Arif Wibowo, and Cordia Chu. 2022. "Indonesia’s Climate-Related Disasters and Health Adaptation Policy in the Build-Up to COP26 and Beyond" Sustainability 14, no. 2: 1006. https://doi.org/10.3390/su14021006








