The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States
Abstract
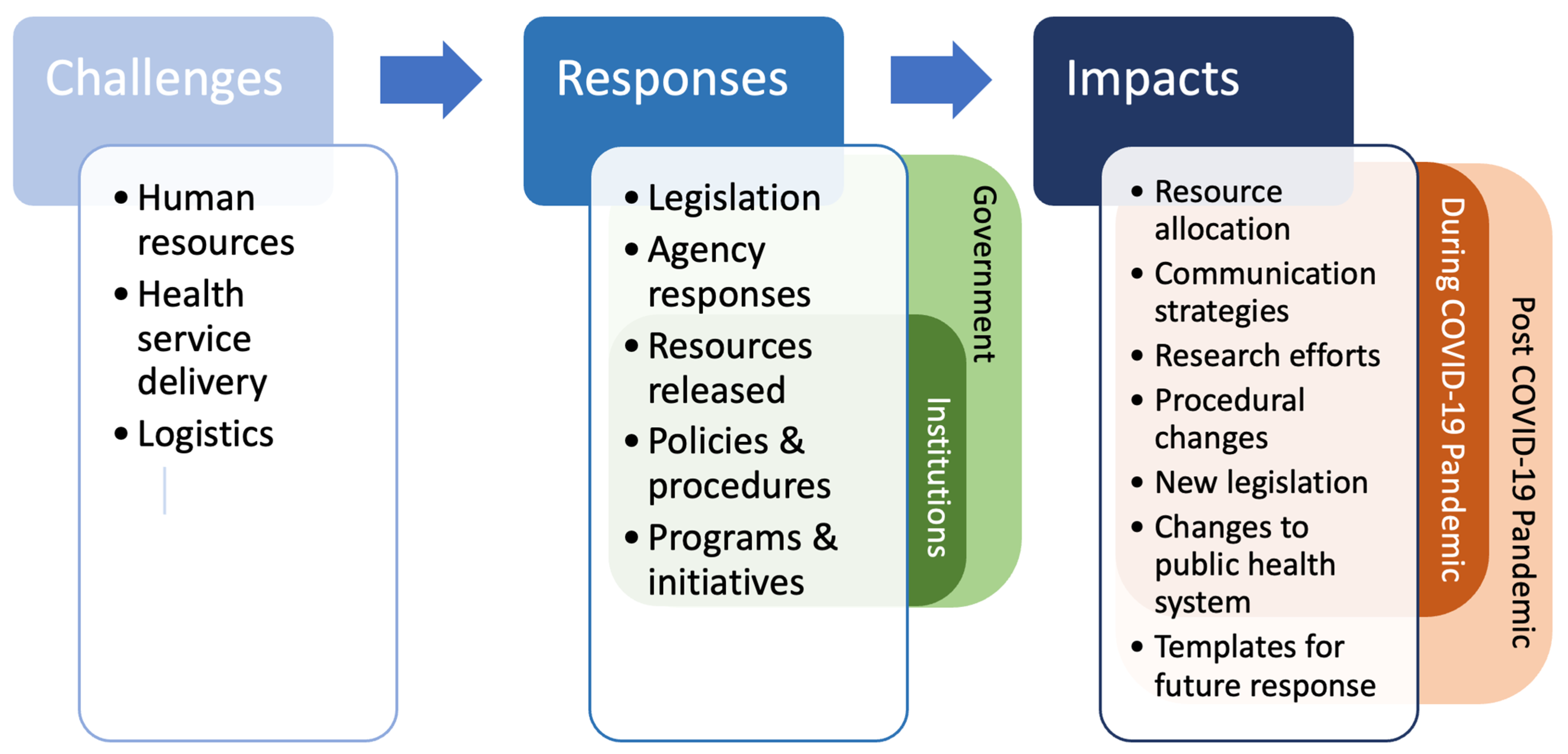
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Data Abstraction
3. Results
3.1. Human Resources
3.1.1. Personnel Shortage
3.1.2. Support of Healthcare Workers
3.2. Health Service Delivery
3.2.1. Testing and Surveillance
3.2.2. Healthcare Disparities
3.2.3. Medical Countermeasures and Vaccines
3.2.4. Clinical Practices
3.2.5. Return to Work and School
3.3. Logistics
3.3.1. Surge Response
3.3.2. International Efforts
4. Discussion
4.1. Human Resources
4.2. Health Service Delivery
4.3. Logistics Systems
4.4. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID Data Tracker. Centers for Disease Control and Prevention. 28 July 2022. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 2 August 2022).
- Laboratory-Confirmed COVID-19-Associated Hospitalizations. COVID-NET, Centers for Disease Control and Prevention. 23 July 2022. Available online: https://gis.cdc.gov/grasp/covidnet/covid19_5.html (accessed on 2 August 2022).
- World Health Organization. Health Emergency and Disaster Risk Management Framework. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/326106/9789241516181-eng.pdf (accessed on 2 August 2022).
- Aitsi-Selmi, A.; Murray, V.; Heymann, D.; McCloskey, B.; Azhar, E.I.; Petersen, E.; Zumla, A.; Dar, O. Reducing risks to health and wellbeing at mass gatherings: The role of the Sendai Framework for Disaster Risk Reduction. Int. J. Infect. Dis. 2016, 47, 101–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Hughes, S.; American Hospital Association. AHA Letter Re: Challenges Facing America’s Health Care Workforce as the U.S. Enters Third Year of COVID-19 Pandemic. 1 March 2022. Available online: https://www.aha.org/lettercomment/2022-03-01-aha-provides-information-congress-re-challenges-facing-americas-health (accessed on 6 April 2022).
- Office of the Assistant Secretary for Planning and Evaluation. Impact of the COVID-19 Pandemic on the Hospital and Outpatient Clinician Workforce: Challenges and Policy Responses. (Issue Brief No. HP-2022-13). U.S. Department of Health and Human Services. 3 March 2022. Available online: https://aspe.hhs.gov/sites/default/files/documents/9cc72124abd9ea25d58a22c7692dccb6/aspe-covid-workforce-report.pdf (accessed on 2 August 2022).
- Fadel, L.; Stone, W.; Anderson, M.; Benincasa, R. As Hospitals Lose Revenue, More Than a Million Health Care Workers Lose Jobs. NPR. 8 May 2020. Available online: https://www.npr.org/2020/05/08/852435761/as-hospitals-lose-revenue-thousands-of-health-care-workers-face-furloughs-layoff (accessed on 2 August 2022).
- Staff Shortages. Centers for Disease Control and Prevention. 21 January 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staff-shortages.html (accessed on 2 August 2022).
- Begun, J.W.; Jiang, H.J. Health Care Management During COVID-19: Insights from Complexity Science. NEJM Catal. Innov. Care Deliv. 2020, 1, 1–12. [Google Scholar] [CrossRef]
- McAfee, M.; Pedersen, C.; Kim, D.; Hawkins, S.; Redman, M. Doctors, Nurses from Across the US Step Up to Help NYC on the Coronavirus Front Lines. ABC News. 10 April 2020. Available online: https://abcnews.go.com/US/doctors-nurses-us-step-nyc-coronavirus-front-lines/story?id=70049109 (accessed on 2 August 2022).
- NYC Health + Hospitals/Coney Island Welcomes, U.S. Department of Defense Medical Team. NYC Health + Hospitals. 24 January 2022. Available online: https://www.nychealthandhospitals.org/pressrelease/coney-island-hospital-welcomes-military-medical-team/ (accessed on 2 August 2022).
- U.S. Army North Public Affairs. Military Hospital Support to Fema Begins in Five States, Navajo Nation, Expands Elsewhere. U.S. Northern Command. 21 January 2022. Available online: https://www.northcom.mil/Newsroom/News/Article/Article/2907587/military-hospital-support-to-fema-begins-in-five-states-navajo-nation-expands-e/ (accessed on 2 August 2022).
- Pollack, R.; American Hospital Association. Hospital Workforce Shortage Crisis Demands Immediate Action. American Hospital Association. Available online: https://www.aha.org/lettercomment/2022-01-27-hospital-workforce-shortage-crisis-demands-immediate-action (accessed on 2 August 2022).
- COVID-19 Contact Tracing. Coursera. Available online: https://www.coursera.org/learn/covid-19-contact-tracing (accessed on 2 August 2022).
- Connley, C. States Are Hiring Thousands of Coronavirus Contact Tracers—Here’s What to Know about the Job. CNBC. 21 May 2020. Available online: https://www.cnbc.com/2020/05/21/what-is-a-coronavirus-contact-tracer-and-how-to-get-hired-as-one.html (accessed on 2 August 2022).
- Connecticut COVID-19 Response. Volunteer to Support Your Community. 2022. Available online: https://portal.ct.gov/Coronavirus/Information-For/Volunteers (accessed on 2 August 2022).
- Opportunities for Medical and Non-Medical Volunteers. City of Chicago. 2022. Available online: https://www.chicago.gov/city/en/sites/covid19-vaccine/home/for-volunteers.html (accessed on 2 August 2022).
- Hancock, S.C. Perspective: An Inside Look at a Rural Hospital Preparing for the Wave. The Kansas Leadership Center Journal. 6 April 2020. Available online: https://klcjournal.com/inside-rural-hospital-covid-19/ (accessed on 2 August 2022).
- Davis, J. Episode 2—The Silver Lining: COVID-19 Care Teams and Cross-Training. American Association of Critical-Care Nurses. 4 June 2020. Available online: https://www.aacn.org/clinical-resources/covid-19/podcast-series/the-silver-lining (accessed on 2 August 2022).
- U.S. Department of Health and Human Services. Health Misinformation. Available online: https://www.hhs.gov/surgeongeneral/priorities/health-misinformation/index.html (accessed on 2 August 2022).
- Prasad, K.; McLoughlin, C.; Stillman, M.; Poplau, S.; Goelz, E.; Taylor, S.; Nankivil, N.; Brown, R.; Linzer, M.; Cappelucci, K.; et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. eClinicalMedicine 2021, 35, 100879. [Google Scholar] [CrossRef] [PubMed]
- Byhoff, E.; Paulus, J.K.; Guardado, R.; Zubiago, J.; Wurcel, A.G. Healthcare workers’ perspectives on coronavirus testing availability: A cross sectional survey. BMC Health Serv. Res. 2021, 21, 719. [Google Scholar] [CrossRef] [PubMed]
- Additional Background: Sweeping Regulatory Changes to Help U.S. Healthcare System Address COVID-19 Patient Surge. 30 March 2020. Available online: https://www.cms.gov/newsroom/fact-sheets/additional-backgroundsweeping-regulatory-changes-help-us-healthcare-system-address-covid-19-patient (accessed on 2 August 2022).
- U.S. Department of Health and Human Services. Biden-Harris Administration Awards $103 Million in American Rescue Plan Funds to Reduce Burnout and Promote Mental Health and Wellness Among Health Care Workforce. 20 January 2022. Available online: https://www.hhs.gov/about/news/2022/01/20/biden-harris-administration-awards-103-million-american-rescue-plan-funds-reduce-burnout-promote-mental-health-wellness-among-health-care-workforce.html (accessed on 2 August 2022).
- Harry, E.M.; Carlasare, L.E.; Sinsky, C.A.; Brown, R.L.; Goelz, E.; Nankivil, N.; Linzer, M. Childcare Stress, Burnout, and Intent to Reduce Hours or Leave the Job During the COVID-19 Pandemic Among US Health Care Workers. JAMA Netw. Open 2022, 5, e2221776. [Google Scholar] [CrossRef] [PubMed]
- Berg, S. Half of Health Workers Report Burnout Amid COVID-19. American Medical Association. 20 July 2021. Available online: https://www.ama-assn.org/practice-management/physician-health/half-health-workers-report-burnout-amid-covid-19 (accessed on 2 August 2022).
- Yong, E. Why Health-care Workers are Quitting in Droves. The Atlantic. 16 November 2021. Available online: https://www.theatlantic.com/health/archive/2021/11/the-mass-exodus-of-americas-health-care-workers/620713/ (accessed on 2 August 2022).
- Kelly, J. New Survey Shows That Up To 47% Of U.S. Healthcare Workers Plan to Leave Their Positions By 2025. Forbes. 19 April 2022. Available online: https://www.forbes.com/sites/jackkelly/2022/04/19/new-survey-shows-that-up-to-47-of-us-healthcare-workers-plan-to-leave-their-positions-by-2025/?sh=4acd8d9e395b (accessed on 2 August 2022).
- Berlin, G.; Lapointe, M.; Murphy, M. Surveyed Nurses Consider Leaving Direct Patient Care at Elevated Rates. McKinsey. 17 February 2022. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/surveyed-nurses-consider-leaving-direct-patient-care-at-elevated-rates (accessed on 2 August 2022).
- Sinsky, C.A.; Brown, R.L.; Stillman, M.J.; Linzer, M. COVID-Related Stress and Work Intentions in a Sample of US Health Care Workers. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- The White House. National COVID-19 Preparedness Plan. March 2022. Available online: https://www.whitehouse.gov/covidplan/ (accessed on 6 April 2022).
- Centers for Disease Control and Prevention. CDC’s COVID-19 Data Improvement. 29 October 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/data-improvements.html (accessed on 2 August 2022).
- U.S. Department of Health and Human Services. Community-Based Testing Sites for COVID-19. 24 January 2022. Available online: https://www.hhs.gov/coronavirus/community-based-testing-sites/index.html (accessed on 2 August 2022).
- Centers for Disease Control and Prevention. Waterborne Disease & Outbreak Surveillance Reporting. 21 March 2022. Available online: https://www.cdc.gov/healthywater/surveillance/wastewater-surveillance/wastewater-surveillance.html (accessed on 2 August 2022).
- Centers for Disease Control and Prevention. COVID-19: Specific Groups of People. 25 March 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html (accessed on 2 August 2022).
- US Department of Health and Human Services. CDC Found Ways to Use Data to Understand and Address COVID-19 Health Disparities, Despite Challenges with Existing Data. July 2022. Available online: https://oig.hhs.gov/oei/reports/OEI-05-20-00540.pdf (accessed on 24 November 2022).
- Cohen, J. Unveiling ‘Warp Speed’, the White House’s America-First Push for a Coronavirus Vaccine. ScienceInsider. 12 May 2020. Available online: https://www.science.org/content/article/unveiling-warp-speed-white-house-s-america-first-push-coronavirus-vaccine (accessed on 2 August 2022).
- National Institutes of Health. Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV). Available online: https://www.nih.gov/research-training/medical-research-initiatives/activ (accessed on 2 August 2022).
- CDC. COVID-19 Vaccinations in the United States. 16 November 2022. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-additional-dose-totalpop (accessed on 24 November 2022).
- MN Department of Health. COVID-19 Vaccine Phases and Planning. 9 May 2022. Available online: https://www.health.state.mn.us/diseases/coronavirus/vaccine/plan.html (accessed on 2 August 2022).
- Centers for Disease Control and Prevention. A Guide for Community Partners: Increasing COVID-19 Vaccine Uptake among Members of Racial and Ethnic Minority Communities. 6 April 2021. Available online: https://www.cdc.gov/vaccines/covid-19/downloads/guide-community-partners.pdf (accessed on 2 August 2022).
- Perez-Stable, E. Overcoming Racial Disparities in Vaccine Hesitancy and Access. Briefings—Foreign Press Centers, U.S. Department of State. 2021. Available online: https://www.state.gov/briefings-foreign-press-centers/overcoming-racial-disparities-in-vaccine-hesitancy-and-access/ (accessed on 2 August 2022).
- Jones, M.; Khader, K.; Branch-Elliman, W. Estimated Impact of the US COVID-19 Vaccination Campaign—Getting to 94% of Deaths Prevented. JAMA Netw. Open 2022, 5, e2220391. [Google Scholar] [CrossRef] [PubMed]
- Schneider, E.C.; Shah, A.; Sah, P.; Moghadas, S.M.; Vilches, T.; Galvania, A. The U.S. COVID-19 Vaccination Program at One Year: How Many Deaths and Hospitalizations Were Averted? The Commonwealth Fund. 14 December 2021. Available online: https://www.commonwealthfund.org/publications/issue-briefs/2021/dec/us-covid-19-vaccination-program-one-year-how-many-deaths-and (accessed on 2 August 2022).
- Holder, J. Tracking Coronavirus Vaccinations around the World. The New York Times. 21 November 2022. Available online: https://www.nytimes.com/interactive/2021/world/covid-vaccinations-tracker.html (accessed on 24 November 2022).
- Kriss, J.L.; Hung, M.-C.; Srivastav, A.; Black, C.L.; Lindley, M.C.; Lee, J.T.; Koppaka, R.; Tsai, Y.; Lu, P.-J.; Yankey, D.; et al. COVID-19 Vaccination Coverage, by Race and Ethnicity—National Immunization Survey Adult COVID Module, United States, December 2020–November 2021. MMWR. Morb. Mortal. Wkly. Rep. 2022, 71, 757–763. [Google Scholar] [CrossRef]
- King, W.C.; Rubinstein, M.; Reinhart, A.; Mejia, R. Time trends, factors associated with, and reasons for COVID-19 vaccine hesitancy: A massive online survey of US adults from January–May 2021. PLoS ONE 2021, 16, e0260731. [Google Scholar] [CrossRef]
- AAFP. Four Reasons for COVID-19 Vaccine Hesitancy among Health care Workers, and Ways to Counter Them. 27 April 2021. Available online: https://www.aafp.org/pubs/fpm/blogs/inpractice/entry/countering_vaccine_hesitancy.html (accessed on 2 August 2022).
- Newport, P. Vaccine Hesitancy and U.S. Public Opinion. Gallup. 30 July 2021. Available online: https://news.gallup.com/opinion/polling-matters/352976/vaccine-hesitancy-public-opinion.aspx (accessed on 2 August 2022).
- World Health Organization. Infodemic. Available online: https://www.who.int/health-topics/infodemic#tab=tab_1 (accessed on 2 August 2022).
- U.S. Department of Health and Human Services. COVID-19 Concerns and Opportunities for Healthcare Leadership. September 2022. Available online: https://files.asprtracie.hhs.gov/documents/covid-19-concerns-and-opportunities-for-healthcare-leadership.pdf (accessed on 6 April 2022).
- Biodefense in Crisis: Immediate Action Needed to Address National Vulnerabilities. Bipartisan Commission on Biodefense. March 2021. Available online: https://biodefensecommission.org/wp-content/uploads/2021/03/Indicators-Report_final7_070221_web.pdf (accessed on 6 April 2022).
- Berlin, G.; Singhal, S.; Lapointe, M.; Schulz, J. Challenges Emerge for the US Healthcare System as COVID-19 Cases Rise. McKinsey & Company. 25 November 2020. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/challenges-emerge-for-the-us-healthcare-system-as-covid-19-cases-rise (accessed on 6 April 2022).
- Centers for Medicare & Medicaid Services. CMS Adult Elective Surgery and Procedures Recommendations. 7 April 2020. Available online: https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf (accessed on 2 August 2022).
- Centers for Medicare & Medicaid Services. Non-Emergent, Elective Medical Services, and Treatment Recommendations. 7 April 2020. Available online: https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf (accessed on 2 August 2022).
- Goldman, B. Stanford Medicine to Enroll 900 in NIH-Funded long-COVID Study. Stanford Medicine News Center. 22 November 2021. Available online: https://med.stanford.edu/news/all-news/2021/11/long-covid-research-initiative.html (accessed on 2 August 2022).
- Weiner, S. What Happens to Telemedicine after COVID-19? AAMC News. 21 October 2021. Available online: https://www.aamc.org/news-insights/what-happens-telemedicine-after-covid-19 (accessed on 2 August 2022).
- U.S. Department of Health and Human Services. Telehealth Policy Changes after the COVID-19 Public Health Emergency. 29 June 2022. Available online: https://telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/policy-changes-after-the-covid-19-public-health-emergency/ (accessed on 2 August 2022).
- Bestsennyy, O.; Gilbert, G.; Harris, A.; Rost, J. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company. 9 July 2021. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality (accessed on 2 August 2022).
- Administration for Strategic Preparedness & Response, U.S. Department of Health and Human Services. Regional Disaster Health Response System. Available online: https://aspr.hhs.gov/RDHRS/Pages/default.aspx (accessed on 2 August 2022).
- Mehta, A.; Lowe, J.; Mukherjee, V. To Prepare For The Next Pandemic, Build A National Care Delivery Network By Leveraging Existing Systems. Health Affairs. 15 October 2021. Available online: https://www.healthaffairs.org/do/10.1377/forefront.20211014.312600 (accessed on 2 December 2022).
- Administration for Strategic Preparedness & Response, U.S. Department of Health and Human Services. National Emerging Special Pathogens Training and Education Center: Mission, Vision & Goals. Available online: https://netec.org/nsps/mission-goals/ (accessed on 2 August 2022).
- Administration for Strategic Preparedness & Response, U.S. Department of Health and Human Services. National Special Pathogen System of Care (NSPS) Strategy Summary. 18 June 2021. Available online: https://netec.org/wp-content/uploads/2021/12/NETEC_NSPS-Strategy-Summary-1.pdf (accessed on 2 August 2022).
- U.S. Department of Education. U.S. Department of Education Approves Maryland’s Plan for Use of American Rescue Plan Funds to Support K-12 Schools and Students, Distributes Remaining More Than $651 Million to State. 14 October 2021. Available online: https://www.ed.gov/news/press-releases/us-department-education-approves-marylands-plan-use-american-rescue-plan-funds-support-k-12-schools-and-students-distributes-remaining-more-651-million-state (accessed on 2 August 2022).
- Miller, C.C. A Key to Returning to Normal Is Paid Sick Leave, Democrats Say. The New York Times. 20 February 2022. Available online: https://www.nytimes.com/2022/02/21/upshot/paid-leave-covid-democrats.html (accessed on 2 August 2022).
- The White House. Biden Administration Launches Effort to Improve Ventilation and Reduce the Spread of COVID-19 in Buildings. 17 March 2022. Available online: https://www.whitehouse.gov/briefing-room/statements-releases/2022/03/17/fact-sheet-biden-administration-launches-effort-to-improve-ventilation-and-reduce-the-spread-of-covid-19-in-buildings/ (accessed on 2 August 2022).
- World Bank Group. COVID-19 and the Global Supply Chains for Medical Supplies. Available online: https://www.globalfinancingfacility.org/sites/gff_new/files/documents/COVID-19-Supply-Chain-ENGLISH.pdf (accessed on 2 August 2022).
- Aboulenein, A. Overwhelmed by Omicron Surge, U.S. Hospitals Delay Surgeries. Reuters. 7 January 2022. Available online: https://www.reuters.com/world/us/overwhelmed-by-omicron-surge-us-hospitals-delay-surgeries-2022-01-07/ (accessed on 2 August 2022).
- Dwyer, C. ‘This Is A Big Deal’: New York Hails Ventilator Deliveries from China and Oregon. NPR. 4 April 2020. Available online: https://www.npr.org/sections/coronavirus-live-updates/2020/04/04/827314791/this-is-a-big-deal-new-york-hails-ventilator-deliveries-from-china-and-oregon (accessed on 2 August 2022).
- Donnelly, C. Field Hospitals Return to Some States As COVID-19 Pushes Hospitals to Breaking Point. NPR. 31 January 2021. Available online: https://www.npr.org/2021/01/31/962528974/field-hospitals-return-to-some-states-as-covid-19-pushes-hospitals-to-breaking-p (accessed on 2 August 2022).
- The Arizona Surgeline. Available online: https://www.azdhs.gov/covid19/documents/healthcare-providers-surge-line/faqs-for-healthcare-facilities-providers.pdf (accessed on 2 August 2022).
- Robinson, D. The Companies Repurposing Manufacturing to Make Key Medical Kit during COVID-19 Pandemic. NS Medical Devices. 1 April 2020. Available online: https://www.nsmedicaldevices.com/analysis/companies-ventilators-shortage-coronavirus/ (accessed on 2 August 2022).
- Centers for Disease Control and Prevention. Decontamination & Reuse of N95 Respirators. 19 October 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html (accessed on 2 August 2022).
- Administration for Strategic Preparedness & Response, U.S. Department of Health and Human Services. H-CORE: HHS Coordination Operations and Response Element. Available online: https://aspr.hhs.gov/h-core/Pages/Default.aspx (accessed on 2 August 2022).
- Office of the Assistant Secretary for Preparedness and Response; U.S. Department of Health and Human Services. The Last Mile: A Pilot Project. 3 April 2019. Available online: https://www.phe.gov/Preparedness/planning/last-mile/Pages/default.aspx (accessed on 2 August 2022).
- U.S. Department of State. Foreign Assistance for Coronavirus (COVID-19). Available online: https://www.state.gov/foreign-assistance-for-coronavirus-covid-19/ (accessed on 2 August 2022).
- Power, S. Marking Delivery of Half a Billion U.S.-Donated COVID-19 Vaccines. Office of Press Relations, USAID. 17 March 2022. Available online: https://www.usaid.gov/news-information/press-releases/mar-17-2022-marking-delivery-half-billion-us-donated-covid-19-vaccines (accessed on 2 August 2022).
- KFF. Tracking U.S. COVID-19 Vaccine Donations. 22 September 2021. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/tracking-u-s-covid-19-vaccine-donations/ (accessed on 24 November 2022).
- Office of Press Relations, USAID. USAID Announces Initiative for Global Vaccine Access (Global VAX) to Accelerate Vaccine Access and Delivery Assistance Around the World. 6 December 2021. Available online: https://www.usaid.gov/news-information/press-releases/dec-6-2021-usaid-announces-initiative-global-vaccine-access-global-vax (accessed on 2 August 2022).
- Rouw, A.; Kates, J.; Michaud, J.; Wexler, A. COVAX and the United States. KFF. 18 February 2021. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/covax-and-the-united-states/ (accessed on 2 August 2022).
- Office of Inspector General. USAID Had Limited Control Over COVID-19 Ventilator Donations, Differing from Its Customary Response to Public Health Emergencies. U.S. Agency for International Development. 24 February 2021. Available online: https://oig.usaid.gov/sites/default/files/2021-02/4-936-21-002-P_0.pdf (accessed on 2 August 2022).
- USAID. COVID-19—Sub-Saharan Africa: Fact Sheet #4. 31 March 2022. Available online: https://www.usaid.gov/sites/default/files/documents/Regional_Fact_Sheet_4_-_SSA.pdf (accessed on 2 August 2022).
- Overton, D.; Ramkeesoon, S.A.; Kirkpatrick, K.; Byron, A.; Pak, E.S. Lessons from the COVID-19 Crisis on Executing Communications and Engagement at the Community Level During a Health Crisis. National Academies. 7 December 2021. Available online: https://www.nationalacademies.org/news/2021/12/lessons-from-covid-19-on-executing-communications-and-engagement-at-the-community-level-during-a-health-crisis (accessed on 24 November 2022).
- NIH. Autoimmune Response Found in Many with COVID-19. 28 September 2021. Available online: https://www.nih.gov/news-events/nih-research-matters/autoimmune-response-found-many-covid-19 (accessed on 24 November 2022).
- Poon, Y.-S.R.; Lin, Y.P.; Griffiths, P.; Yong, K.K.; Seah, B.; Liaw, S.Y. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: A systematic review with future directions. Hum. Resour. Health 2022, 20, 70. [Google Scholar] [CrossRef] [PubMed]
- Nebehay, S. Global Shortage of Nurses Set to Grow as Pandemic Enters Third Year-Group. Reuters. 10 December 2021. Available online: https://www.reuters.com/business/healthcare-pharmaceuticals/global-shortage-nurses-set-grow-pandemic-enters-third-year-group-2021-12-10/ (accessed on 24 November 2022).
- Tessema, G.A.; Kinfu, Y.; Dachew, B.A.; Tesema, A.G.; Assefa, Y.; Alene, K.A.; Aregay, A.F.; Ayalew, M.B.; Bezabhe, W.M.; Bali, A.G.; et al. The COVID-19 pandemic and healthcare systems in Africa: A scoping review of preparedness, impact and response. BMJ Glob. Health 2021, 6, e007179. [Google Scholar] [CrossRef]
- Siwakoti, S.; Yadav, K.; Thange, I.; Bariletto, N.; Zanotti, L.; Ghoneim, A.; Shapiro, J.N. Localized Misinformation in a Global Pandemic: Report on COVID-19 Narratives around the World. Empirical Studies of Conflict. 2021. Available online: https://esoc.princeton.edu/publications/localized-misinformation-global-pandemic-report-covid-19-narratives-around-world (accessed on 24 November 2022).
| Domain | Key Takeaway Impacts |
|---|---|
| Human Resources |
|
| Health Service Delivery |
|
| Logistics |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, A.P.; Hansoti, B.; Hsu, E.B. The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States. Sustainability 2022, 14, 16301. https://doi.org/10.3390/su142316301
Chen AP, Hansoti B, Hsu EB. The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States. Sustainability. 2022; 14(23):16301. https://doi.org/10.3390/su142316301
Chicago/Turabian StyleChen, Allison P., Bhakti Hansoti, and Edbert B. Hsu. 2022. "The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States" Sustainability 14, no. 23: 16301. https://doi.org/10.3390/su142316301





