Abstract
Urban and rural areas are situated in contrasting physical and social settings, which influence their levels of exposure as well as their preventive behaviors in response to the COVID-19 outbreak. The study investigated whether there were differences between the areas regarding the levels of difficulty and anxiety felt by the general public during the first wave of COVID-19 in April and May 2020. We conducted an online questionnaire in Fukuoka and Kumamoto Prefecture in southern Japan via a private research company and collected a total of 913 valid responses from individuals whose conditions of employment were affected by the coronavirus outbreak. Although urban areas experienced higher case rates compared to rural areas, ordinal logistic regression analysis revealed no significant differences between urban and rural respondents concerning the level of difficulty in routine life. The daily-life contents which made them feel difficult during the first wave also did not differ largely between the contrasting areas. Urban respondents appeared to have experienced a higher level of difficulty in finding an alternative job, but how respondents found one, if successful, did not differ between urban and rural areas. The area of residence played a role in explaining the level of anxiety toward being infected, especially when the anxiety-related questions involved relationships with neighbors. Rural respondents showed a significantly higher level of anxiety toward causing neighbors trouble and being criticized if infected. Respondents who were better embedded in their communities generally felt more anxious about being infected, regardless of whether they lived in urban or rural areas. Women and respondents with children were more likely affected by abnormal situations caused by the COVID-19 outbreak. Our study highlights the prevailing impact of the COVID-19 pandemic on the general public regardless of whether in urban or rural settings, as well as the potential contribution of social ties among people to protecting communities from infectious pathogens.
1. Introduction
On 11 March 2020, the World Health Organization declared the coronavirus 2019 (COVID-19) outbreak as a global pandemic. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is primarily transmitted from person-to-person through respiratory droplets and contaminated surfaces in the immediate environment around an infected person [1]. Airborne infection is also a possible transmission mechanism, particularly in indoor settings with poor ventilation [2]. As close proximity over a prolonged time is key to viral transmission, physical distancing has been regarded as one of the effective means to reduce the risk of infection [3]. Population density has a significant influence on how infectious pathogens spread [4,5], as it constrains how far people can be spatially separated from each other. Human behavior is another factor that determines the transmission of the virus [6,7].
Urban and rural areas are situated in contrasting physical and social settings, which influence people’s level of exposures as well as their preventive behaviors in response to the infectious disease outbreak. Urban inhabitants are presumably more exposed to COVID-19, as the effective reproduction number of the virus (i.e., the average number of secondary cases caused by an infected person) is likely higher in large urban areas due to greater reproductive opportunities afforded by denser populations and built-up environments [8,9]. Being the center of social activities may be another reason for the high risk of viral transmission in urban areas. Rural areas are, in contrast, sparsely populated. However, rural areas are considered more susceptible to coronavirus because they have large shares of senior/elder populations who are particularly at high risk for severe illness [10]. Their susceptibility also stems from the limited health care workforce and resources such as personnel, equipment, and services, especially during times of widespread disasters such as pandemics [11]. Rural areas are known to have developed strong social ties within a community [12]. Social norms inherent in rural areas may have functioned as a way to make their people take collective actions in order to protect communities from the unknown, quick-spreading virus, as reported by previous studies [13,14]. They contribute to preventive behaviors [15], but networks with high levels of bonding can sometimes lead to social exclusion if one fails to meet the norm [16]. Urban inhabitants are, in this regard, less prone to such social pressure. Furthermore, a substantial number of people had to experience dismissal or temporary leave from work due to an extensive reduction in social and economic activities caused by the coronavirus outbreak. It could be that people had a higher chance of finding alternative jobs to strive through the period of lower income if they belonged to a society with established social ties (e.g., jobs introduced by neighbors and friends) and if jobs were available that do not involve much interaction with others (e.g., primary sector such as agriculture and forestry). In other words, we considered that community-level systems may have functioned as a safety net for affected people when their primary works were no longer possible. Due to the differences in these physical and social settings, the general public in urban and rural areas may have felt different levels of difficulty and anxiety or worries pursuing day-to-day activities from different aspects during the COVID-19 pandemic. A meta-analysis from Wang et al. [17] pointed out the scarcity of studies especially from rural areas and called for studies to better understand the urban-rural gradient of COVID-19 impacts.
The global health crisis has immensely impacted the three pillars of sustainability in human lives [18]. In times of great instability brought on by COVID-19, the social dimension has been identified as the main priority for organizations to achieve sustainability [19], while it pushed back the environmental and economic dimensions of sustainability based on the priority of needs [20]. In accordance with the classification of research on the sustainability pillars and COVID-19 [18], our study is centered around social sustainability (i.e., social norms and public health efforts against the pandemic) and its intersections with environmental (i.e., healthcare resources) and economic sustainability (i.e., alternative jobs offered via information channels established in communities). Comparing how urban and rural people perceived life during the pandemic, and the underlying reasons for their perceptions may help identify key elements that have contributed to sustaining one’s living under the strict public health interventions and to protecting their communities from the rapidly spreading virus.
The study took a cross-sectional approach to investigate whether there were differences between urban and rural areas with regard to the levels of difficulty and anxiety felt by the general public during the first wave of COVID-19 in Japan. COVID-19 arrived in Japan in January 2020 [21]. The Japanese government declared the first state of emergency on 7 April 2020 to seven prefectures with high case rates and expanded the target areas to all 47 prefectures in the following week [22]. Emergency measures continued until the middle or end of May depending on the situation of prefectures [22]. Although COVID-19 was pronounced in large cities (for example, the Tokyo Metropolis alone accounted for 28% of the total confirmed cases in Japan as of 6 April 2020 [21]), measures were uniformly implemented across the nation or a prefecture, including rural areas where there were no or only a few confirmed cases [13]. These include stay-at-home requests, restricted movement between prefectures, and basic infection control measures such as social distancing, wearing masks, and washing hands, and avoidance of the “3Cs (closed spaces, crowded places, and close-contact settings)” [22]. Temporary school closure was implemented nationwide in March 2020 and repeatedly thereafter [23]. Many public facilities and non-essential businesses were requested to close temporarily as well, and restaurants were requested to shorten business hours according to the national and prefectural guidelines [22]. Influenced by these measures, the number of workers who were on temporary leave increased substantially during the first state of emergency, followed by a gradual increase in the unemployment rate later in 2020 [24]. All citizens were informed of, or at least had access to, updates related to the pandemic through the media and the government’s press conference, where the news coverage was based on urban situations most of the time [13].
We expected the following outcomes: (H1) urban inhabitants felt a higher level of difficulty in pursuing their daily life as compared to rural inhabitants due to a higher exposure to the infectious pathogens in urban settings, and that (H2) the contents of difficulty felt by people differ between urban and rural areas due to their contrasts in socio-economic situations. Related to the research question on difficulty contents, we investigated whether (H3) there is any difference in how urban and rural inhabitants found an alternative job to compensate for income loss caused by dismissal or temporary leave during this time. In addition, we hypothesized that (H4) urban inhabitants felt higher levels of anxiety toward themselves and their family members being infected owing to higher exposure, but that (H5) rural inhabitants felt higher levels of anxiety toward causing their neighbors trouble if they are infected due to the norms and social cognition inherent in rural areas. For the same reason, we expected (H6) rural inhabitants to show higher levels of anxiety toward being criticized for being infected in comparison to urban inhabitants.
2. Methods
2.1. Study Area
The study was conducted in urban and rural areas of Fukuoka and Kumamoto Prefecture located in the southern part of Japan (Figure 1). Fukuoka Prefecture lies in the north facing the main island across the sea and consists of the fourth largest metropolitan area of the country. Kumamoto Prefecture is historically and locationally the center of Kyushu Island, and its largest city is designated as a metropolitan area.
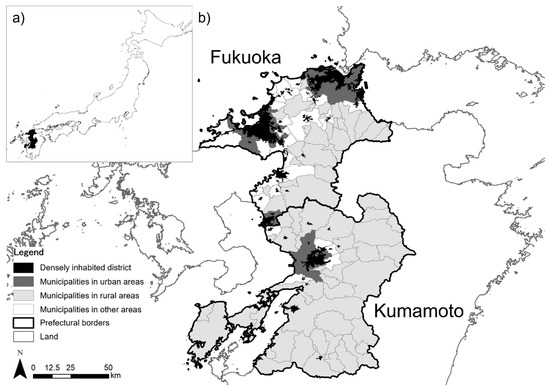
Figure 1.
Maps showing (a) the location of the study area, and (b) urban and rural areas studied.
In order to define urban and rural areas of the two prefectures, we employed a dataset on the area of densely inhabited district (DID) available from the Ministry of Land, Infrastructure, Transportation, and Tourism [25]. It has been invented to identify urban areas based on population density (>4000 people per km2) and total population (>5000 people). As the following sampling was conducted at the municipal level, we set arbitrary criteria for defining urban and rural areas; municipalities whose proportion of DID in total land area was greater than 20% were defined as urban areas, while those with 3% and less were classified as rural areas. Those that fell in other areas were excluded from our study. As a result, Fukuoka Prefecture included 14 municipalities as urban areas and 27 as rural areas, and Kumamoto Prefecture included 1 and 39, respectively (Figure 1).
2.2. Data Collection
We collected municipal-level variables related to COVID-19 case rates, population, and medical care situations in our study area (urban N = 15, rural N = 66). These include the cumulative number of confirmed cases per 100,000 inhabitants, population density, aging rate, and the numbers of hospital beds and hospital physicians per 100,000 inhabitants. Information related to the number of infections were collated for April and May 2020, which covers the period of the first state of emergency. Prefectural and municipal portal sites were used. As some of the municipal information were publicized based on regional-level public health centers, case rates (i.e., the cumulative number of confirmed cases per 100,000 inhabitants) were calculated at the regional level. An equal value was assigned to municipalities that belong to the same region, assuming that the density is uniform within the region. Population data were based on 2020 [26], and the aging rate was defined as the proportion of the population aged 65 and above. The number of hospital beds (i.e., the sum of general and infectious disease beds) was taken from the Survey of Medical Institutions 2019 [27]. The number of hospital physicians, including those working for hospitals affiliated with medical educational institutions, was obtained from the Survey of Physicians, Dentists and Pharmacists 2018 [28].
An online questionnaire was carried out covering a wide range of individuals who experienced dismissal or temporary leave from work in April and May 2020 due to the coronavirus outbreak. The survey was outsourced to a research company, which conducts questionnaires to pre-registered individuals in their web-based portal system. The questionnaire was distributed randomly to individuals living in the urban and rural areas defined in Section 2.1 until the target sample size was reached. The sampling was designed in a way that samples were collected evenly across gender, age groups, and regions (i.e., Fukuoka-urban, Fukuoka-rural, Kumamoto-urban, and Kumamoto-rural). Students were excluded from sampling. We took a gradient of the degree of reduction in working hours to make sure that the respondent had time to work for alternative jobs during the time. We first focused on collecting samples from respondents whose working hours had been reduced severely—by more than 25%. As three regions (Fukuoka-rural, Kumamoto-urban, and Kumamoto-rural) did not reach the target sample size after the first round, the sampling population was expanded to include individuals who had their working hours reduced at least by 5%. The second round was closed after 85% of the target sample size was collected for the three regions, as the number of samples did not increase anymore. The remaining 15% of the samples from the three regions were complemented by the Fukuoka-urban region instead. Data collection was done for three weeks in September 2020. A total of 913 samples were collected, and the resulting distribution is summarized in the Supplementary Material (Table S1). The distribution depicting the levels of working hour reduction is shown in Figure 2.
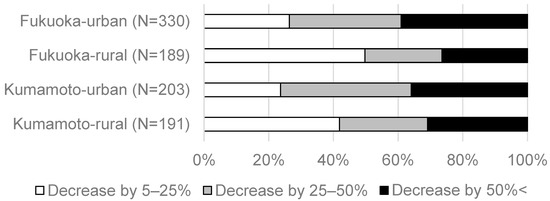
Figure 2.
The proportion of respondents with different levels of reduced working hours (N = 913).
The questionnaire was structured in six sections. The first section was associated with changes in the respondent’s average household income in April and May 2020 relative to January 2020, i.e., before COVID-19 became a major issue in Japan. We asked a four-scale question of whether their monthly income had undergone 5–25%/25–50%/50% < decrease or ‘no change or increase,’ including any other kind of payments made to compensate for their income loss. The second section was regarding rating difficulty in a scale of 1–10 with 10 being the highest difficulty felt by the respondent. The respondent was also asked to answer a multiple-choice question on 18 items to indicate which matter made them feel especially difficult in the time of the first wave. The third section involved the respondent’s job-hunting history during the first state of emergency. We asked whether the respondent looked for job opportunities, including short-term, temporary ones such as paid tasks spontaneously available at a neighbor’s place, and whether they actually found one. As we were interested in the success of finding a job through a network of personal contacts, we asked respondents who did short-term, temporary jobs how they found those in a multiple-choice question (with nine items). The fourth section was related to the respondent’s anxiety or concerns toward contracting the virus, which was measured on a 6-point Likert scale where “1 = did not feel anxious at all” and “6 = felt very anxious.” The level of anxiety was identified for three different aspects: (1) the respondent themself and their family get infected; (2) the respondent will cause their neighbors trouble if infected; (3) the respondent will be criticized if infected. Note that anxiety here is different from psychological anxiety, which involves mental and physical symptoms, and that it has rather a closer meaning to fear, concerns, or worries in this study. The fifth section was about the respondent’s relationship with their neighbors to measure how well they were connected in their community. We adopted an indicator frequently used to measure social ties in Japan [29]. The respondent was asked if they have neighbors whom they (1) greet, (2) chat to outside, (3) cooperate with for daily stuff and consult with, or if they have (4) no one to interact with. The last section dealt with the socio-demographic characteristics of the respondent (i.e., gender, age, annual household income in 2019, and whether or not the respondent has a child under 12 years old).
2.3. Statistical Analysis
In order to compare case rates, population, and medical situations between urban and rural areas, we first conducted the Mann–Whitney U test on variables collected at the municipal level. A conditional independence test was carried out to determine whether the level of relationship with neighbors was independent of the urban or rural setting. Prefectures were treated as a control variable. We used ordinal logistic regression to explain the level of difficulty (ten ordinal classes) and anxiety (six ordinal classes) felt by the respondent in April and May 2020. To detect which population groups felt more affected, the respondent’s attributes such as areas (urban/rural), prefectures (Fukuoka/Kumamoto), gender, age group, the level of change in their monthly household income, annual household income in 2019, and whether or not they have a child under 12 years old were employed as explanatory variables. Regression analysis on anxiety additionally accounted for the level of relationship with neighbors, as the questions involved anxiety arising from interaction with others. For regression analysis, we used 836 samples out of 913 who responded to the question regarding annual household income. Backward stepwise model selection was applied, and the best-fit model was selected based on the Akaike’s Information Criterion. Best-fit models were assessed by Nagelkerke pseudo-R2, which indicates the degree of improvement from the null model in a range from 0 to 1. In order to analyze whether the contents that made the respondent experience difficulty during the first state of emergency differ between urban and rural areas, we performed a conditional independence test on each of the 18 items by treating prefectures as a control variable. We also employed the same statistical test on the respondent’s job-hunting history (i.e., whether or not they looked for a job and actually found one) as well as on the nine items related to the methods of how the respondent found an alternative job during the time. All statistical analyses were conducted with R version 3.6.1 [30], and R-package MASS [31] was used for the conditional independence test and ordinal logistic regression. We used R-package DescTools [32] to calculate Nagelkerke pseudo-R2.
2.4. Ethical Consideration
Our study falls outside the scope of the Japanese government’s Ethical Guidelines for Medical and Health Research Involving Human Subjects. There are no national ethical guidelines for humanities and social science research in Japan. Our research follows the basic ethical principles. It is a non-interventional study, where we conducted questionnaire toward the general public under stratified random sampling.
All survey participants gave their consent to participate in the anonymous online survey by the research company. The authors did not obtain any personal information about the participants. After being informed about the purposes of the study, participants agreed to participate. They had the right to quit the survey any time. Completion of the entire questionnaire was considered to indicate participant consent.
3. Results
3.1. Situations in Urban and Rural Areas
The summary for case rates, population density, and medical care situations in the study area is provided in Table 1. The spread of the coronavirus disease was severer in urban areas, as the number of confirmed cases per 100,000 inhabitants was significantly higher in these densely populated areas than in rural areas. Rural areas were, in contrast, represented by a higher aging rate and a smaller capacity of medical care systems such as smaller numbers of hospital beds and hospital physicians per 100,000 inhabitants. The level of relationship with neighbors was significantly associated with areas of residence (urban/rural; X2 = 26.0, d.f. = 6, p < 0.001), where rural respondents showed a stronger level of association with their communities (Figure S1).

Table 1.
Summary of situations in urban and rural areas. Values refer to mean and standard deviation (in parentheses). Significant differences are denoted with asterisk(s) based on the Mann–Whitney U test.
3.2. Difficulty
The results of ordinal logistic regression on the level of difficulty felt by the respondent during the first wave are shown in Table 2. Nagelkerke pseudo-R2 was 0.247, meaning that the best-fit model improved from the null model by a small degree. Log-likelihood ratio test revealed that the improvement was significant (p < 0.001). According to the results, the area of residence (urban/rural) was not selected in the model selection, indicating that there is no significant difference between urban and rural areas with regard to the level of difficulty. Higher level of difficulty was felt by respondents who had experienced a greater decrease in their monthly household income. The odds ratio suggests that respondents whose income decreased by 50%< were, for example, 14.8 times more likely to undergo difficult times than those whose income did not decrease. The level of difficulty significantly decreased with increasing income with the exception of the highest income group. Although the effects were only marginal (p = 0.07), respondents with a child under 12 years old were 1.36 times more likely to experience difficulty compared to those without.

Table 2.
Results of ordinal logistic regression explaining the level of difficulty felt by the respondent in April and May 2020 (on a scale from 1 to 10 with 10 being the highest difficulty). Coefficients are shown as mean and standard errors (in parentheses). Significance is indicated with ***, **, *, and . for p < 0.001, p < 0.01, p < 0.05, and p < 0.1, respectively.
The contents which made the respondent experience difficulty during the first wave also did not differ largely between urban and rural areas (Figure 3). Controlled for prefectures, there were only two contents that showed significant differences between the two contrasting areas. They were namely visiting a hospital/clinic (X2 = 6.68, d.f. = 2, p < 0.05) and corresponding to school closure (X2 = 9.97, d.f. = 2, p < 0.01), both of which gave rural respondents more difficulties. As opposed to our expectation, two-thirds of the surveyed people did not search for job opportunities to compensate for their reduced working hours during this time. Approximately 70% of the respondents who went on job hunting were not able to find a job, with a higher probability among urban respondents (X2 = 6.79, d.f. = 2, p < 0.05). This result is in line with the one from the difficulty content related to job hunting, where urban respondents found it more difficult to find a job than rural respondents (X2 = 4.85, d.f. = 2, p = 0.09; Figure 3). Among the respondents who found a short-term job (N = 53), including paid tasks that are spontaneously available at a neighbor’s place, there were no significant differences between urban and rural areas in how they found one (Figure 4).
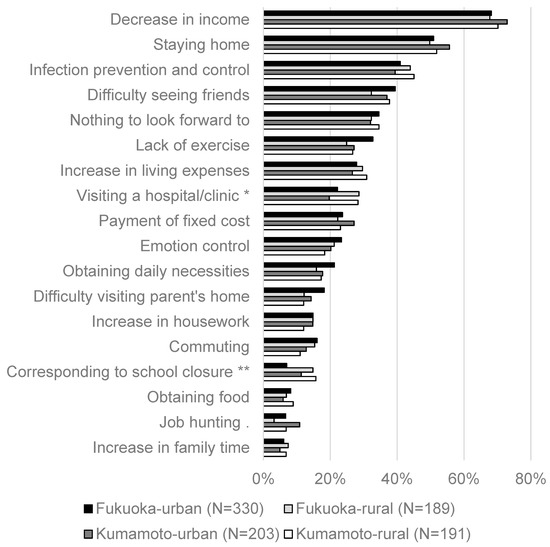
Figure 3.
Contents of difficulty (N = 913). Significance is indicated with **, *, and . for p < 0.01, p < 0.05, and p < 0.1, respectively.
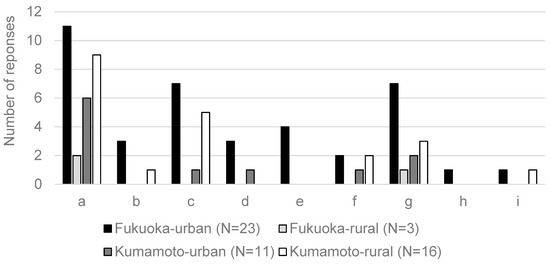
Figure 4.
Methods of how the respondent found a temporary job answered in a multiple-choice question: (a) internet and magazines, (b) the government’s Employment Service Center, (c) a private employment agency, (d) a previous or current workplace, (e) a workplace where they have worked from time to time, (f) family members and relatives, (g) friends and acquaintances, (h) neighbors, and (i) others. Conditional independence test was performed, but no significant difference was observed between urban and rural areas.
3.3. Anxiety
The results of ordinal logistic regression on three different aspects of anxiety are provided in Table 3. The best-fit models improved slightly from the respective null models (Nagelkerke pseudo R2 ranging from 0.06 to 0.09), but the improvements were all determined to be significant (log-likelihood ratio test p < 0.001). The area of residence (urban/rural) was not selected for the first question (i.e., the respondent and their family getting infected), but was relevant for the second (i.e., the respondent causing trouble if infected; p < 0.01) and third (i.e., the respondent being criticized if infected; p = 0.05). According to the odds ratios of the latter two questions, rural respondents were 1.40 and 1.29 times more likely to feel anxious than urban respondents, respectively. The respondent’s economic situations appeared to be less relevant for anxiety when compared to difficulty, as the odds ratios of income change showed relatively smaller values. Annual household income was not selected in any of the models. For all of the three questions, women exhibited a significantly higher level of anxiety as well as respondents with a child under 12 years old. The level of anxiety also increased with an increasing level of relationship with neighbors. Respondents who were better embedded in their communities felt significantly more anxious about being infected when compared to those who had no interactions. The only exceptions were respondents who had neighbors to greet in the first question and those who had neighbors to cooperate with for daily stuff and consult with in the third question.

Table 3.
Results of ordinal regression models explaining the level of anxiety in April and May 2020 described from three aspects (six ordinal classes where “1 = do not feel anxious at all” and “6 = feel very anxious”). Coefficients are shown as mean and standard errors (in parentheses). Significance is indicated with ***, **, *, and . for p < 0.001, p < 0.01, p < 0.05, and p < 0.1, respectively.
4. Discussion
Our study investigated whether there were differences between urban and rural areas in the levels of difficulty and anxiety felt by the general public during the first wave of COVID-19 in the southern part of Japan. The results revealed that there were no significant differences between urban and rural respondents in the level of difficulty in pursuing their daily life (rejecting H1), although the level of exposure to the virus and the social-economic situations to deal with the outbreak are presumably different in these areas. The contents of difficulty as well as how respondents found an alternative job during the period of unemployment or temporary leave also did not differ between the contrasting areas (rejecting H2 and H3, respectively). Additionally, no significant difference was found between urban and rural respondents in the level of anxiety toward themselves and their family members being infected (rejecting H4). The area of residence, however, played a role in explaining the level of anxiety toward being infected when the questions involved relationship with neighbors; rural respondents showed significantly higher level of anxiety toward causing neighbors trouble and being criticized if infected, in comparison to urban respondents (confirming H5 and H6, respectively).
Regression analysis showed that the degree of income changes was the main variable explaining the level of difficulty experienced during the first state of emergency. The daily life content ranked on top was also related to their economic situations (i.e., decrease in income), and those in the second and third were to COVID-19 safety measures (i.e., staying home and infection prevention and control, respectively). Non-significant differences between urban and rural areas in response to these difficulty-related questions may indicate that measures to combat COVID-19 have induced similar changes in social and economic situations of people’s livelihoods in different parts of Japan, as they were implemented uniformly across the nation or a prefecture. Media coverage may also be responsible for the non-significant differences between the contrasting areas observed for the contents related to COVID-19 safety measures. Previous studies reported that broadcasts can influence people’s preventive behaviors, even in areas where the virus spread is relatively limited [33,34]. Ohta et al. [13] confirmed that rural Japanese communities were largely influenced by COVID-19-related news from urban Japan and around the world and acted according to the standard precautionary measures. Although their study was focused on older people, it is likely that our samples from rural areas have likewise taken preventive behaviors because they were informed of the outbreak as much as urban respondents were. While the literature citing urban and rural situations in the adherence to the behavioral recommendations appears to report mixed results around the world (e.g., a higher level of compliance found in urban people [17,35,36,37,38,39,40,41] or no differences [42,43,44]), preventive behaviors in Japan seem to be fairly similar between urban and rural areas [13,14,34]. Our work provides a more holistic view on people’s preventive behaviors in urban and rural Japan by covering a broader range of people in our cross-sectional survey (vs. small group interviews [13,14]) and by explicitly defining urban and rural areas at the municipal level (vs. comparison at the prefectural level [34]). Stress brought on by the COVID-19 outbreak also did not differ between urban and rural areas in Japan [45].
Interestingly, we have also observed no significant differences between urban and rural respondents in the level of anxiety about themselves being infected, although case rates were significantly higher in urban areas. The non-significant differences observed for this question may come from different concerns regarding COVID-19 infection; urban people were anxious about the outbreak being pronounced in their living environments, while rural people were concerned about introducing the virus to their communities and affecting their neighbors. The different views of urban and rural people can be supported by the significant difference found in the second question, where rural people felt higher level of anxiety toward causing their neighbors trouble if infected. Although only marginal, rural people also showed a higher level of anxiety toward being criticized if infected, in comparison to people living in urban areas. These concerns related to others have probably increased rural people’s anxiety toward themselves being infected, even though the virus was not as widespread as in urban areas. These may also be responsible for the non-significant differences observed for the difficulty contents related to COVID-19 safety measures such as staying home and infection prevention and control, as rural people were also careful not to be infected in consideration of others.
High bonding social capital developed in rural communities may explain the significantly higher level of anxiety rural people showed when the questions involved concerns for others. Social capital is a concept in social science which is related to the social norms, networks, and trust that facilitate cooperation within or between groups [46]. It is known to generate benefits to society, as communities with strong social ties are equipped to undertake collective actions, enforce and maintain social norms, promote reciprocity exchanges between members of a network, and diffuse innovations via information channels that exist within network structures [15]. There is a growing body of evidence that social capital has played a key role in curbing the spread of infectious disease [47,48,49]. Of the three types of social capital, bonding (i.e., within-group social ties that build trust and mutual reliance [50]) and linking (i.e., vertical ties between groups and those with power or authority that help communities petition for public goods and responsive governance [51]) types have been identified as a key to positive COVID-19 outcomes of communities [49]. Rural communities are associated with high bonding social capital [12], where within-group solidarity has facilitated the uptake of new social norms among their members that were formed during the pandemic [14]. Collective actions to prevent the virus spread may have complemented rural vulnerabilities related to high aging rate and scarce medical resources, as case rates were shown to be significantly lower in rural areas than in urban areas. Our study shed light on rural areas and is one of the few case studies from Japan to discuss the potential contributions of social capital to controlling the pandemic, besides the work from Fraser and Aldrich [52] and Kokubun and Yamakawa [53].
Failure to comply with rules can, however, lead to social discrimination [16], and previous studies have reported that rural inhabitants felt anxious about other people’s perception of their behaviors and rumors that might spread in their community [13,14]. Higher proportions of rural respondents expressing difficulty related to hospital/clinic visits may be related to both aspects of collective actions and the fear for social discrimination. Visiting hospitals and clinics can increase the potential risk of introducing the virus to medical facilities and thus putting a burden on the limited healthcare resources. People were probably afraid of social discrimination from using the facilities as well because they were initially deemed as the source of the virus spread, as reported by previous studies related to ostracism felt by health care workers [54]. In total, our findings are in support for the association between high bonding social capital and anxiety related to community compliance, as rural respondents were found to have stronger associations with neighbors than urban respondents, and people with stronger social ties were associated with a higher level of anxiety. Here, anxiety concerning others may include perception of others when they are infected, in addition to putting their community at risk of virus spread. Contracting coronavirus with respect to others is probably less of a concern in urban areas because the virus is already widespread and urban inhabitants generally have less interactions with neighbors.
Urban respondents appeared to have felt a higher level of difficulty finding a job than rural respondents. This is understandable because coronavirus was more widespread in urban areas, and many economic activities there involve face-to-face interactions such as wholesaling, large retail business, and foodservice [55]. We expected that people who were affected in work would have looked for job opportunities to compensate for their income loss, but this was not the case in our study. Two-thirds of our respondents did not look for a job at all, and only 30% of those who went on job hunting were successful. This resulted in a smaller sample size to test the third hypothesis. As opposed to our expectation, of those who were successful in getting short-term, temporary jobs, there were no significant differences in how urban and rural respondents found one. We anticipated that rural respondents would be able to find small jobs because there was presumably a huge demand for people who could help farmers with rice-planting during the first state of emergency. As their children in cities were not able to come home and help them with the heavy labor, we considered that rural inhabitants could take these spontaneously available jobs via information channels established in communities and were able to strive through the period of lower income. Even though our study could not disentangle whether community-level systems functioned as a safety net or backup when primary economic activities were no longer possible, there might be cases where small jobs available in local communities could support people’s living in times of a crisis like the COVID-19 pandemic. Site-level studies would help evaluate the contributions of community-level systems to building resilience in the society.
Our study also observed consistent association between female respondents and higher levels of measurements such as difficulty pursuing their daily life and anxiety toward coronavirus contraction. The results could be related to the severity of psychological impact on women that has been reported in many previous studies [45,56,57,58], as well as to a pronounced increase in the female suicide rate in Japan during the second wave of the pandemic [59,60]. In addition, respondents who had a child under 12 years old were shown to be associated with higher levels of difficulty and anxiety. This result is evident, as school closure for months can increase childcare needs massively [61], and possibly because kids were deemed to play a major role in spreading the virus during the first wave of COVID-19 according to what we have learnt from influenza [62]. Our results also indicated a significant difference between urban and rural respondents regarding the difficulty content related to school closure. We do not have a clear explanation of the reason why rural people found school closures more difficult, as it was implemented nationwide, and urban and rural respondents equally found it difficult to see (and depend on) their parents. In any case, outreach programs for a crisis like the COVID-19 pandemic should target women and people with small children proactively.
The study has some limitations. First, our samples were collected using an online survey. While it provides a good alternative for data collection, particularly when face-to-face surveys are difficult, there is also a pitfall that individuals who are not registered as an Internet Panel remain unexamined. Site-level studies would help improve the generality of results found in large-scale studies like ours. Second, we focused on people whose working conditions were affected by the outbreak. We consider that our conclusion would not change, even if unaffected people were included, because the study showed consistent results with previous studies from other parts of Japan reporting non-significant differences in preventive behaviors [34]. Our results could also be well explained by the social cognitive theory [47,48,49]. Therefore, we would expect that whether people were personally affected in work or not is not decisive enough to override the general patterns (i.e., significant or non-significant difference between urban and rural areas) found in the study. Third, because we employed stratified random sampling to get an equal representation of people across gender and age groups from each region, our data may contain a wider range of noise compared to data taken from people who know well about their communities. This may limit the cognitive value of our research. On the other hand, the significant difference in the anxiety level observed in our data may also indicate the generality of protective behaviors that rural people have taken collectively in the face of the invisible coronavirus outbreak.
5. Conclusions
In this paper, we provide evidence from urban and rural areas in southern Japan that the spread of the coronavirus disease had prevailing influences on the general public regardless of their infection situations. The two contrasting areas found it equally difficult to adopt the new life brought on by the pandemic, and people in rural areas were especially concerned about affecting others and the criticisms of them in case of infection. By comparing the perceptions of urban and rural people, the study also identified social capital to be the key element that might have contributed to protecting oneself and communities from infectious pathogens and consequently to preventing the collapse of local and regional systems. It is desirable to accumulate knowledge from urban and rural areas on how the general public responded to COVID-19, especially from the latter communities where the amount of information is generally limited. We believe that further research on how people strived through the difficult times would contribute to formulating policy actions based on the urban-rural character of a place so that society can be better prepared for future epidemics and pandemics, both in terms of assuring one’s sustainable living and maintaining the functioning of communities.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/su14042277/s1, Table S1: The sampling distribution of the study; Figure S1: The proportion of respondents with different levels of relationship with neighbors.
Author Contributions
Conceptualization, K.S. and T.I.; Data Curation, K.S.; Formal Analysis, K.S.; Funding Acquisition, T.I.; Investigation, K.S.; Methodology, K.S. and T.I.; Project Administration, T.I.; Resources, T.I.; Software, T.I.; Supervision, T.I.; Validation, T.I.; Visualization, K.S.; Writing—Original Draft, K.S.; Writing—Review and Editing, K.S. and T.I. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the Environmental Restoration and Conservation Agency of Japan (project ID JPMEERF19S20507).
Institutional Review Board Statement
Ethical review and approval were waived for this study because our study falls outside the scope of the Japanese government’s Ethical Guidelines for Medical and Health Research Involving Human Subjects.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We would like to thank our online survey participants for providing us valuable data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions; Scientific Brief: Geneva, Switzerland, 2020. [Google Scholar]
- Somsen, G.A.; van Rijn, C.; Kooij, S.; Bem, R.A.; Bonn, D. Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission. Lancet Respir. Med. 2020, 8, 658–659. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Wang, Q. Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet 2020, 395, 1950–1951. [Google Scholar] [CrossRef]
- Hu, H.; Nigmatulina, K.; Eckhoff, P. The scaling of contact rates with population density for the infectious disease models. Math. Biosci. 2013, 244, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.S.; Li, Y. Spreading of COVID-19: Density matters. PLoS ONE 2020, 15, e0242398. [Google Scholar] [CrossRef] [PubMed]
- Lunn, P.D.; Belton, C.A.; Lavin, C.; McGowan, F.P.; Timmons, S.; Robertson, D.A. Using Behavioral Science to help fight the Coronavirus. J. Behav. Public Adm. 2020, 3. [Google Scholar] [CrossRef] [Green Version]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Delamater, P.L.; Street, E.J.; Leslie, T.F.; Yang, Y.T.; Jacobsen, K.H. Complexity of the Basic Reproduction Number (R0). Emerg. Infect. Dis. 2019, 25, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Huang, Q.; Jackson, S.; Derakhshan, S.; Lee, L.; Pham, E.; Jackson, A.; Cutter, S.L. Urban-rural differences in COVID-19 exposures and outcomes in the South: A preliminary analysis of South Carolina. PLoS ONE 2021, 16, e0246548. [Google Scholar] [CrossRef]
- Peters, D.J. Community Susceptibility and Resiliency to COVID-19 Across the Rural-Urban Continuum in the United States. J. Rural Health 2020, 36, 446–456. [Google Scholar] [CrossRef]
- Patel, L.; Elliott, A.; Storlie, E.; Kethireddy, R.; Goodman, K.; Dickey, W. Ethical and Legal Challenges During the COVID-19 Pandemic: Are We Thinking About Rural Hospitals? J. Rural Health 2021, 37, 175–178. [Google Scholar] [CrossRef] [Green Version]
- Sørensen, J.F.L. Rural–Urban Differences in Bonding and Bridging Social Capital. Reg. Stud. 2016, 50, 391–410. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Sano, C. Fears Related to COVID-19 among Rural Older People in Japan. Healthcare 2021, 9, 524. [Google Scholar] [CrossRef] [PubMed]
- Takashima, R.; Onishi, R.; Saeki, K.; Hirano, M. Perception of COVID-19 Restrictions on Daily Life among Japanese Older Adults: A Qualitative Focus Group Study. Healthcare 2020, 8, 450. [Google Scholar] [CrossRef]
- Kawachi, I. Social capital and health. In Handbook of Medical Sociology, 6th ed.; Bird, C.E., Conrad, P., Fremont, A.M., Timmermans, S., Eds.; Springer: New York, NY, USA, 2008; pp. 18–32. [Google Scholar]
- Claridge, T. Functions of social capital–bonding, bridging, linking. Soc. Cap. Res. 2018, 20, 1–7. [Google Scholar]
- Wang, X.; Lin, L.; Xuan, Z.; Xu, J.; Wan, Y.; Zhou, X. Risk communication on behavioral responses during COVID-19 among general population in China: A rapid national study. J. Infect. 2020, 81, 911–922. [Google Scholar] [CrossRef] [PubMed]
- Ranjbari, M.; Shams Esfandabadi, Z.; Zanetti, M.C.; Scagnelli, S.D.; Siebers, P.O.; Aghbashlo, M.; Peng, W.; Quatraro, F.; Tabatabaei, M. Three pillars of sustainability in the wake of COVID-19: A systematic review and future research agenda for sustainable development. J. Clean Prod. 2021, 297, 126660. [Google Scholar] [CrossRef] [PubMed]
- Barreiro-Gen, M.; Lozano, R.; Zafar, A. Changes in Sustainability Priorities in Organisations due to the COVID-19 Outbreak: Averting Environmental Rebound Effects on Society. Sustainability 2020, 12, 5031. [Google Scholar] [CrossRef]
- Rydzewski, P. Between Economy and Security. Dilemmas of Sustainable Development in the Covid-19 Era–an Example of Great Britain. Probl. Ekorozw. 2020, 15, 15–21. [Google Scholar] [CrossRef]
- NHK. COVID-19 Cases in Japan. Available online: https://www3.nhk.or.jp/news/special/coronavirus/data-all/ (accessed on 5 January 2022). (In Japanese).
- MHLW. Basic Policies for Novel Coronavirus Disease Control by the Government of Japan (Summary); Ministry of Health, Labor and Welfare: Tokyo, Japan, 2020.
- MEXT. Information on MEXT’s Measures against COVID-19. Available online: https://www.mext.go.jp/en/mext_00006.html (accessed on 5 January 2022).
- MHLW. White Paper—The Novel Coronavirus and Social Security; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2021. (In Japanese)
- MLIT. Densely Inhabited District. Available online: https://nlftp.mlit.go.jp/ksj/gml/datalist/KsjTmplt-A16-v2_3.html (accessed on 20 February 2020). (In Japanese)
- Statistics Bureau. Population and Households 2020. Available online: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00200241&tstat=000001039591&cycle=7&year=20200&month=0&tclass1=000001039601&stat_infid=000031971230&result_back=1&tclass2val=0 (accessed on 27 January 2021). (In Japanese)
- Statistics Bureau. Survey of Medical Institutions 2019 (N1). Available online: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450021&tstat=000001030908&cycle=7&tclass1=000001144570&tclass2=000001144573&stat_infid=000031982297&tclass3val=0 (accessed on 27 January 2021). (In Japanese)
- Statistics Bureau. Survey of Physicians, Dentists and Pharmacists 2018 (8). Available online: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450026&tstat=000001135683&cycle=7&tclass1=000001135684&tclass2=000001135687&stat_infid=000031889158&tclass3val=0 (accessed on 27 January 2021). (In Japanese)
- CAO. Social Capital: Toward a Better Feedback Cycle in Society. Available online: https://www.npo-homepage.go.jp/toukei/2009izen-chousa/2009izen-sonota/2002social-capital (accessed on 5 January 2022). (In Japanese)
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Venables, W.; Ripley, B. Modern Applied Statistics with S, 4th ed.; Springer: New York, NY, USA, 2002. [Google Scholar]
- Signorell, A.; Aho, K.; Alfons, A.; Anderegg, N.; Aragon, T.; Arachchige, C.; Arppe, A.; Baddeley, A.; Barton, K.; Bolker, B. DescTools: Tools for Descriptive Statistics. 2021. Available online: https://cran.R-project.Org/package=DescTools (accessed on 26 January 2021).
- Kim, E.; Shepherd, M.E.; Clinton, J.D. The effect of big-city news on rural America during the COVID-19 pandemic. Proc. Natl. Acad. Sci. USA 2020, 117, 22009–22014. [Google Scholar] [CrossRef]
- Shiina, A.; Niitsu, T.; Kobori, O.; Idemoto, K.; Hashimoto, T.; Sasaki, T.; Igarashi, Y.; Shimizu, E.; Nakazato, M.; Hashimoto, K.; et al. Relationship between perception and anxiety about COVID-19 infection and risk behaviors for spreading infection: A national survey in Japan. Brain Behav. Immun. Health 2020, 6, 100101. [Google Scholar] [CrossRef]
- Banu, B.; Haque Chowdhury, S.; Akter, N.; Rakibul Islam, K.; Mahmud Hossain, S.; Ruhul Amin, M. Preventive Behaviors to Mitigate COVID-19: Urban-Rural Disparities of Densely Populated Country like Bangladesh. J. Environ. Sci. Public Health 2021, 5, 433–450. [Google Scholar] [CrossRef]
- Shahnazi, H.; Ahmadi-Livani, M.; Pahlavanzadeh, B.; Rajabi, A.; Hamrah, M.S.; Charkazi, A. Assessing preventive health behaviors from COVID-19: A cross sectional study with health belief model in Golestan Province, Northern of Iran. Infect Dis. Poverty 2020, 9, 157. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chen, H. Differences in Preventive Behaviors of COVID-19 between Urban and Rural Residents: Lessons Learned from A Cross-Sectional Study in China. Int. J. Environ. Res. Public Health 2020, 17, 4437. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Yao, L.; Hu, L.; Zhou, L.; Yuan, F.; Zhong, X. Urban and Rural Disparities of Personal Health Behaviors and the Influencing Factors During the COVID-19 Outbreak in China: Based on an Extended IMB Model. Disaster Med. Public Health Prep. 2020, 1–5. [Google Scholar] [CrossRef]
- Probst, J.C.; Crouch, E.L.; Eberth, J.M. COVID-19 risk mitigation behaviors among rural and urban community-dwelling older adults in summer, 2020. J. Rural Health 2021, 37, 473–478. [Google Scholar] [CrossRef]
- Callaghan, T.; Lueck, J.A.; Trujillo, K.L.; Ferdinand, A.O. Rural and Urban Differences in COVID-19 Prevention Behaviors. J. Rural Health 2021, 37, 287–295. [Google Scholar] [CrossRef]
- Chauhan, R.S.; Capasso da Silva, D.; Salon, D.; Shamshiripour, A.; Rahimi, E.; Sutradhar, U.; Khoeini, S.; Mohammadian, A.; Derrible, S.; Pendyala, R. COVID-19 related Attitudes and Risk Perceptions across Urban, Rural, and Suburban Areas in the United States. Findings 2021, 23714. [Google Scholar] [CrossRef]
- Min, C.; Shen, F.; Yu, W.; Chu, Y. The relationship between government trust and preventive behaviors during the COVID-19 pandemic in China: Exploring the roles of knowledge and negative emotion. Prev. Med 2020, 141, 106288. [Google Scholar] [CrossRef]
- Geana, M.V. Kansans in the middle of the pandemic: Risk perception, knowledge, compliance with preventive measures, and primary sources of information about COVID-19. Kans. J. Med. 2020, 13, 160. [Google Scholar] [CrossRef]
- Vicerra, P.M.M. Knowledge-Behavior Gap on COVID-19 among Older People in Rural Thailand. Gerontol. Geriatr. Med. 2021, 7, 2333721421997207. [Google Scholar] [CrossRef]
- Uehara, M.; Fujii, M.; Kobayashi, K. A Model of Stress Change under the First COVID-19 Pandemic among the General Public in Japanese Major Cities and Rural Areas. Sustainability 2021, 13, 1207. [Google Scholar] [CrossRef]
- Productivity Commission. Social Capital: Reviewing the Concept and Its Policy Implications; University Library of Munich: Munich, Germany, 2003. [Google Scholar]
- Bartscher, A.K.; Seitz, S.; Siegloch, S.; Slotwinski, M.; Wehrhöfer, N. Social capital and the spread of Covid-19: Insights from European countries. J. Health Econ. 2021, 80, 102531. [Google Scholar] [CrossRef] [PubMed]
- Raude, J.; Lecrique, J.M.; Lasbeur, L.; Leon, C.; Guignard, R.; du Roscoat, E.; Arwidson, P. Determinants of Preventive Behaviors in Response to the COVID-19 Pandemic in France: Comparing the Sociocultural, Psychosocial, and Social Cognitive Explanations. Front. Psychol. 2020, 11, 584500. [Google Scholar] [CrossRef] [PubMed]
- Fraser, T.; Aldrich, D.P.; Page-Tan, C. Bowling alone or distancing together? The role of social capital in excess death rates from COVID19. Soc. Sci. Med. 2021, 284, 114241. [Google Scholar] [CrossRef]
- Lee, J. Bonding and bridging social capital and their associations with self-evaluated community resilience: A comparative study of East Asia. J. Community Appl. Soc. Psychol. 2019, 30, 31–44. [Google Scholar] [CrossRef]
- Aldrich, D.P. Building Resilience: Social Capital in Post-Disaster Recovery; University of Chicago Press: Chicago, IL, USA, 2012. [Google Scholar]
- Fraser, T.; Aldrich, D.P. The dual effect of social ties on COVID-19 spread in Japan. Sci. Rep. 2021, 11, 1596. [Google Scholar] [CrossRef]
- Kokubun, K.; Yamakawa, Y. Social Capital Mediates the Relationship between Social Distancing and COVID-19 Prevalence in Japan. Inquiry 2021, 58, 469580211005189. [Google Scholar] [CrossRef] [PubMed]
- The Japan Nursing Ethics Association. Honor Medical Professionals Fighting COVID-19. Available online: http://jnea.net/9.html#200403 (accessed on 5 January 2022). (In Japanese).
- The Small and Medium Enterprise Agency. 4 Structural Difference in Job Types between Urban and Rural Areas. Available online: https://www.chusho.meti.go.jp/amphlet/hakusyo/H28/h28/shoukibodeta/html/b1_4_1_4.html (accessed on 5 January 2022). (In Japanese)
- Losada-Baltar, A.; Jimenez-Gonzalo, L.; Gallego-Alberto, L.; Pedroso-Chaparro, M.D.S.; Fernandes-Pires, J.; Marquez-Gonzalez, M. “We Are Staying at Home.” Association of Self-perceptions of Aging, Personal and Family Resources, and Loneliness with Psychological Distress During the Lock-Down Period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e10–e16. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Kala, M.P.; Jafar, T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0244630. [Google Scholar] [CrossRef]
- Yamamoto, T.; Uchiumi, C.; Suzuki, N.; Yoshimoto, J.; Murillo-Rodriguez, E. The Psychological Impact of ‘Mild Lockdown’ in Japan during the COVID-19 Pandemic: A Nationwide Survey under a Declared State of Emergency. Int. J. Environ. Res. Public Health 2020, 17, 9382. [Google Scholar] [CrossRef]
- Nomura, S.; Kawashima, T.; Yoneoka, D.; Tanoue, Y.; Eguchi, A.; Gilmour, S.; Kawamura, Y.; Harada, N.; Hashizume, M. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res. 2021, 295, 113622. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021, 5, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Alon, T.; Doepke, M.; Olmstead-Rumsey, J.; Tertilt, M. The Impact of COVID-19 on Gender Equality; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Imamura, T.; Saito, M.; Ko, Y.K.; Imamura, T.; Otani, K.; Akaba, H.; Ninomiya, K.; Furuse, Y.; Miyahara, R.; Sando, E.; et al. Roles of Children and Adolescents in COVID-19 Transmission in the Community: A Retrospective Analysis of Nationwide Data in Japan. Front. Pediatr. 2021, 9, 705882. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).