Effects of Hospital Decentralization Processes on Patients’ Satisfaction: Evidence from Two Public Romanian Hospitals across Two Decades
Abstract
:1. Introduction
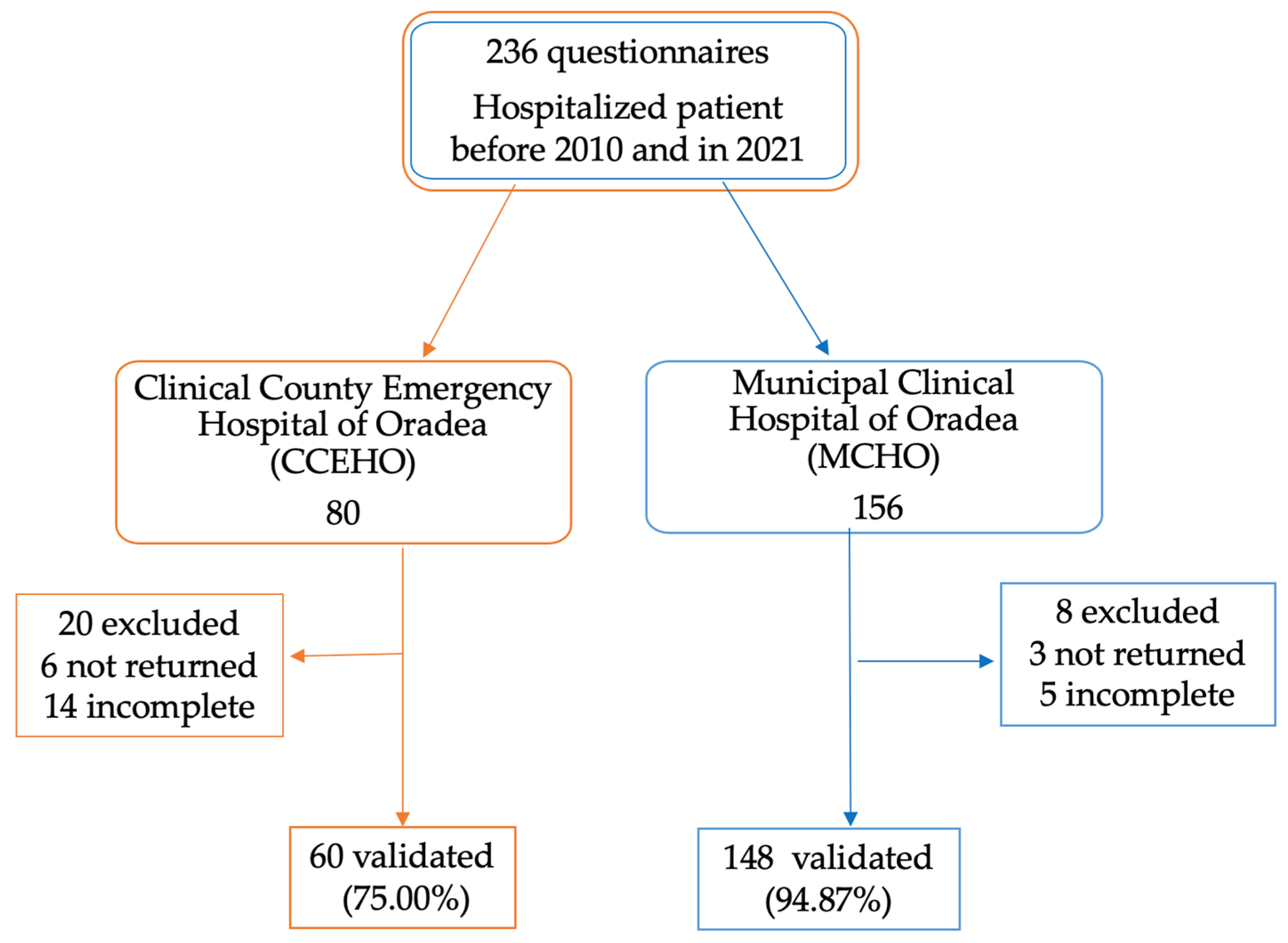
2. Materials and Methods
2.1. Methodology
- Patient data (items 1–5);
- Quality of medical care (items 6–15);
- Quality of hospital hotel services (items 16–23).
- A.
- The first option was in reference to inpatient hospitalization in the period 2000–2010;
- B.
- The second option was in reference to inpatient hospitalization in 2021.
2.2. Statistical Analysis
3. Results
3.1. Patient Data
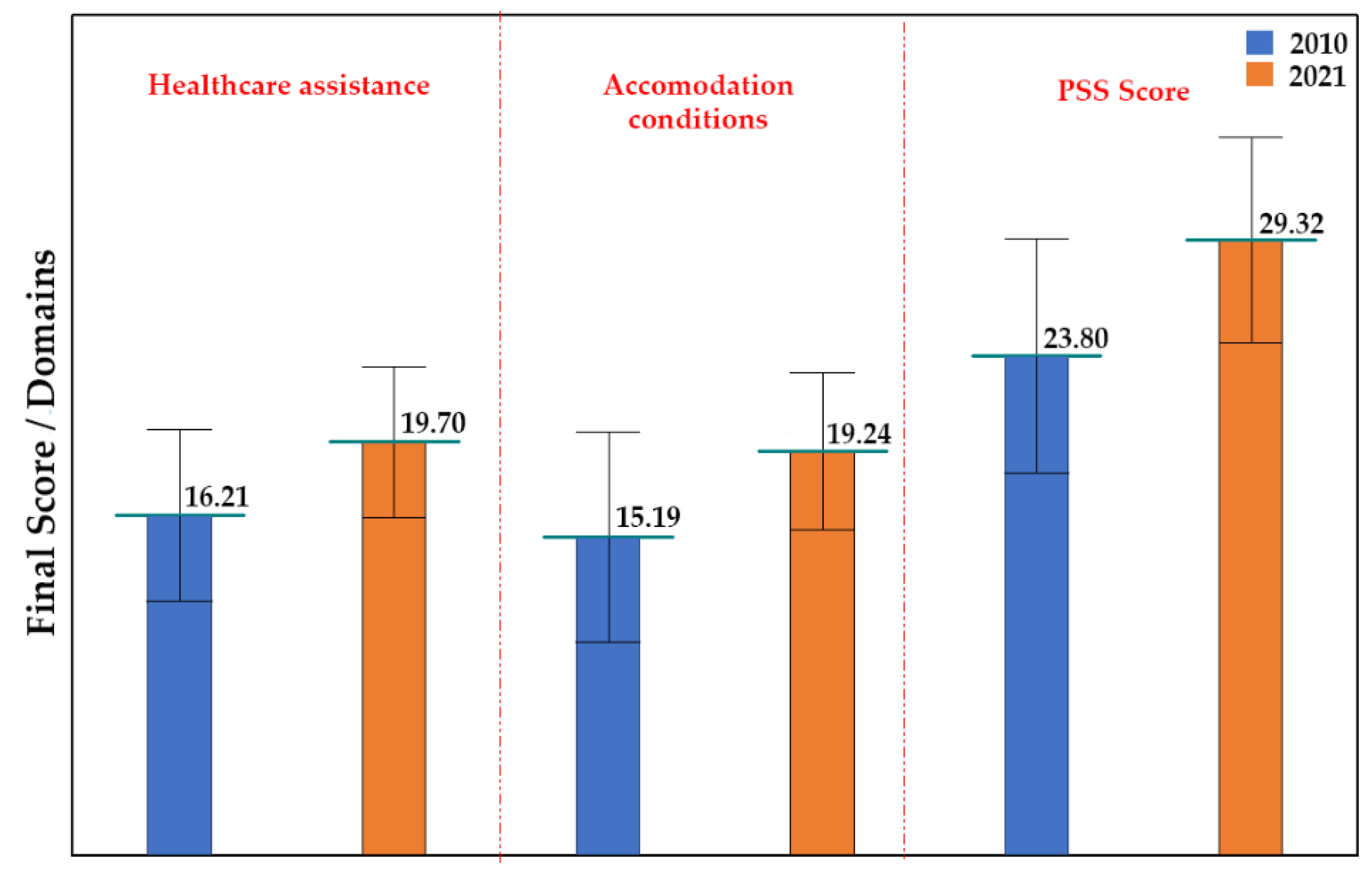
3.2. Medical Care
3.3. Hospital Accommodation Conditions
3.4. Patient Satisfaction Survey Score
3.5. Final Evaluation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xesfingi, S.; Vozikis, A. Patient satisfaction with the healthcare system: Assessing the impact of socio-economic and healthcare provision factors. BMC Health Serv. Res. 2016, 16, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, H.R.; Pronovost, P.; Diette, G.B. The advantages and disadvantages of process-based measures of health care quality. Int. J. Qual. Health Care 2001, 13, 469–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, G.; Kagwanja, N.; Whyle, E.; Gilson, L.; Molyneux, S.; Schaay, N.; Tsofa, B.; Barasa, E.; Olivier, J. Health system responsiveness: A systematic evidence mapping review of the global literature. Int. J. Equity Health 2021, 20, 112. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2000: Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Lege, nr. 95 din 14 Aprilie 2006. Available online: https://legislatie.just.ro/Public/DetaliiDocument/71139 (accessed on 14 February 2022).
- Ordonanţă de Urgenţă, nr. 48 din 2 Iunie 2010. Available online: https://legislatie.just.ro/Public/DetaliiDocumentAfis/119434 (accessed on 11 February 2022).
- Lege, nr. 118 din 30 Iunie 2010. Available online: https://legislatie.just.ro/Public/DetaliiDocument/119960 (accessed on 23 February 2022).
- Ordin Pentru Modificarea Anexei, nr. 1 la Ordinul Ministrului Sănătății nr. 1384/2010 Privind Aprobarea Modelului-Cadru al Contractului de Management şi a Listei Indicatorilor de Performanţă a Activităţii Managerului Spitalului Public. Available online: http://www.ms.ro/2018/04/12/ordin-pentru-modificarea-anexei-nr-1-la-ordinul-ministrului-sanatatii-nr-1384-2010-privind-aprobarea-modelului-cadru-al-contractului-de-management-si-a-listei-indicatorilor-de-performanta-a-activit/ (accessed on 22 February 2022).
- Molyneux, J. Nurses’ job satisfaction linked to patient satisfaction. Am. J. Nurs. 2011, 111, 16. [Google Scholar] [CrossRef] [PubMed]
- Batbaatar, E.; Dorjdagva, J.; Luvsannyam, A.; Savino, M.M.; Amenta, P. Determinants of patient satisfaction: A systematic review. Perspect. Public Health 2017, 137, 89–101. [Google Scholar] [CrossRef]
- Bungau, S.; Suciu, R.; Bumbu, A.; Cioca, G.; Tit, D.M. Study on Hospital Waste Management in Medical Rehabilitation Clinical Hospital, Baile Felix. J. Environ. Prot. Ecol. 2015, 16, 980–987. [Google Scholar]
- Westbrooke, L.A.; Carr, R.L. Implementation of a patient management system in a children hospital. Stud. Health Technol. Inform. 1997, 46, 469–474. [Google Scholar]
- Huang, J.-A.; Lai, C.-S.; Tsai, W.-C.; Weng, R.-H.; Hu, W.-H.; Yang, D.-Y. Determining factors of patient satisfaction for frequent users of emergency services in a medical center. J. Chin. Med. Assoc. 2004, 67, 403–410. [Google Scholar]
- Metodologie Microclimatul Locurilor de Muncă: Normative, Capacitate de Evaluare și Efecte Asupra Stării de Sănătate. 2022. Available online: https://insp.gov.ro/download/cnmrmc/Metodologii%20PNII/Medicina%20Muncii/04.Microclimatul-locurilor-de-munca_2022.pdf (accessed on 21 February 2022).
- Aziri, B. Job satisfaction: A literature review. Manag. Res. Pract. 2011, 3, 77–86. [Google Scholar]
- Haas, J.S.; Cook, E.F.; Puopolo, A.L.; Burstin, H.R.; Cleary, P.D.; Brennan, T.A. Is the professional satisfaction of general internists associated with patient satisfaction? J. Gen. Intern. Med. 2000, 15, 122–128. [Google Scholar] [CrossRef] [Green Version]
- Daina, L.G.; Sabău, M.; Daina, C.M.; Neamțu, C.; Tit, D.M.; Buhaș, C.L.; Bungau, C.; Aleya, L.; Bungau, S. Improving performance of a pharmacy in a Romanian hospital through implementation of an internal management control system. Sci. Total Environ. 2019, 675, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Uivarosan, D.; Bungau, S.; Tit, D.M.; Moisa, C.; Fratila, O.; Rus, M.; Bratu, O.G.; Diaconu, C.C.; Pantis, C. Financial Burden of Stroke Reflected in a Pilot Center for the Implementation of Thrombolysis. Medicina 2020, 56, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgovan, C.; Cosma, S.A.; Valeanu, M.; Juncan, A.M.; Rus, L.L.; Gligor, F.G.; Butuca, A.; Tit, D.M.; Bungau, S.; Ghibu, S. An Exploratory Research of 18 Years on the Economic Burden of Diabetes for the Romanian National Health Insurance System. Int. J. Environ. Res. Public Health 2020, 17, 4456. [Google Scholar] [CrossRef] [PubMed]
- Jankauskienė, D.; Jankauskaitė, I. Access and quality of health care system by opinion of patients in ten European countries. Manag. Health 2011, 15. Available online: http://journal.managementinhealth.com/index.php/rms/article/view/200/576 (accessed on 22 February 2021).
- Radu, F.; Radu, V.; Turkeș, M.C.; Ivan, O.R.; Tăbîrcă, A.I. A research of service quality perceptions and patient satisfaction: Case study of public hospitals in Romania. Int. J. Health Plan. Manag. 2022, 37, 1018–1048. [Google Scholar] [CrossRef]
- Cosma, S.A.; Bota, M.; Fleșeriu, C.; Morgovan, C.; Văleanu, M.; Cosma, D. Measuring Patients’ Perception and Satisfaction with the Romanian Healthcare System. Sustainability 2020, 12, 1612. [Google Scholar] [CrossRef] [Green Version]
- Bara, A.; van den Heuvel, W.; Maarse, J.; van Dijk, J. Users’ satisfaction with the Romanian health care system: An evaluation of recent health care reforms. Eur. J. Public Health 2002, 12, 39–40. [Google Scholar]
- Coţiu, M.; Crişan, I.; Catană, G.A. Patient Satisfaction with Healthcare-A Focus Group Exploratory Study. In Proceedings of the International Conference on Advancements of Medicine and Health Care through Technology, Cluj-Napoca, Romania, 5–7 June 2014; pp. 119–124. [Google Scholar]
- Burcea, M.; Toma, S.G.; Papuc, R.M. Patients’ satisfaction with the health care systemin the age of globalization: The case of Romania. Transylv. Rev. Adm. Sci. 2014, 10, 5–20. [Google Scholar]
- Francu, V.; Frâncu, O. Patients’ satisfaction, a measure of health care quality. Acta Med. 2012, 2, 147–148. [Google Scholar]
- Spitalul Clinic Județean de Urgență Oradea, Rapoarte Statistice Privind Chestionarele de Satisfacție Angajați, Anii 2015–2018. Available online: http://spitaljudetean-oradea.ro/web/wp-content/uploads/2015/07/chestionar-satisfactie-pacienti.pdf (accessed on 22 October 2021).
- Panda, B.; Thakur, H.P. Decentralization and health system performance–a focused review of dimensions, difficulties, and derivatives in India. BMC Health Serv. Res. 2016, 16, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Palese, A.; Gonella, S.; Fontanive, A.; Guarnier, A.; Barelli, P.; Zambiasi, P.; Allegrini, E.; Bazoli, L.; Casson, P.; Marin, M. The degree of satisfaction of in-hospital medical patients with nursing care and predictors of dissatisfaction: Findings from a secondary analysis. Scand. J. Caring Sci. 2017, 31, 768–778. [Google Scholar] [CrossRef] [PubMed]
- Prada, M.F.; Popescu, D.E.; Bungau, C. Building education, source of energy saving in Romania. In Proceedings of the 15th National Technical-Scientific Conference on Modern Technologies for the 3rd Millennium, Oradea, Romania, 27–28 November 2015; pp. 157–162. [Google Scholar]
- Ghemis, M.T.; Scurt, A.A.; Bob, C.; Bungau, C. An Analysis of Sustainability about Rehabilitation and Reconversion of an Old Building. In Proceedings of the 17th National Technical-Scientific Conference on Modern Technologies for the 3rd Millennium, Oradea, Romania, 22–23 March 2018; pp. 273–278. [Google Scholar]
- Prada, M.; Popescu, D.; Bungau, C.; Pancu, R.; Bungau, C. Parametric studies on European 20-20-20 energy policy targets in university environment. J. Environ. Prot. Ecol. 2017, 18, 1146–1157. [Google Scholar]
- Badulescu, D.; Bungău, C.; Badulescu, A. Sustainable development through sustainable businesses. an empirical research among master students. J. Environ. Prot. Ecol. 2015, 16, 1101–1108. [Google Scholar]
- Ilea, C.D.N.; Daina, L.G.; Bungau, S.; Tit, D.M.; Uivarosan, D.; Moleriu, L.; Petre, I.; Bungau, C.; Petre, I. Sustainable Management, Instable Legislation Regarding Wages, and Employee Satisfaction/Motivation in Two Romanian Hospitals. Sustainability 2020, 12, 909. [Google Scholar] [CrossRef] [Green Version]
- Bungau, C.; Blaga, F.; Gherghea, C. Method of analysis and audit used to implement 5s in operational management. In Proceedings of the 2nd Review of Management and Economic Engineering Management Conference: Management of Crisis or Crisis of Management, Cluj Napoca, Romania, 15–17 September 2011; pp. 36–47. [Google Scholar]
- Bungau, S.; Tit, D.M.; Fodor, K.; Cioca, G.; Agop, M.; Iovan, C.; Cseppento, D.C.N.; Bumbu, A.; Bustea, C. Aspects Regarding the Pharmaceutical Waste Management in Romania. Sustainability 2018, 10, 2788. [Google Scholar] [CrossRef] [Green Version]
- Cook, J. Laboratory Integration and Consolidation in a Regional Health System. Lab. Med. 2017, 48, e43–e52. [Google Scholar] [CrossRef]
- Badulescu, D.; Simut, R.; Badulescu, A.; Badulescu, A.-V. The relative effects of economic growth, environmental pollution and non-communicable diseases on health expenditures in European Union countries. Int. J. Environ. Res. Public Health 2019, 16, 5115. [Google Scholar] [CrossRef] [Green Version]
- Bungau, S.; Bungau, C.; Tit, D. Studies about last stage of product lifecycle management for a pharmaceutical product. J. Env. Prot. Ecol. 2015, 16, 56. [Google Scholar]
- Tit, D.M.; Bungau, S.; Nistor Cseppento, C.; Copolovici, D.; Buhas, C. Disposal of unused medicines resulting from home treatment in Romania. J. Environ. Prot. Ecol. 2016, 17, 1425–1433. [Google Scholar]







| Characteristics | No. | % |
|---|---|---|
| Gender | ||
| Male | 115 | 55.29 |
| Female | 93 | 44.71 |
| Age (years) | ||
| <30 | 14 | 6.73 |
| 30–60 | 97 | 46.63 |
| >60 | 97 | 46.63 |
| Living environment | ||
| Rural | 92 | 44.23 |
| Urban | 116 | 55.77 |
| Education | ||
| No education | 23 | 11.06 |
| Secondary | 142 | 68.27 |
| Higher | 43 | 20.67 |
| Patients’ Distribution | Nr. | % |
|---|---|---|
| Ward profile | ||
| Surgery | 33 | 15.87 |
| Medical | 64 | 30.77 |
| Oncology | 106 | 50.96 |
| Psychiatry | 5 | 2.40 |
| Inpatient hospitalization type | ||
| Scheduled | 146 | 70.19 |
| Emergency | 62 | 29.81 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dulău, D.; Craiut, L.; Tit, D.M.; Buhas, C.; Tarce, A.G.; Uivarosan, D. Effects of Hospital Decentralization Processes on Patients’ Satisfaction: Evidence from Two Public Romanian Hospitals across Two Decades. Sustainability 2022, 14, 4818. https://doi.org/10.3390/su14084818
Dulău D, Craiut L, Tit DM, Buhas C, Tarce AG, Uivarosan D. Effects of Hospital Decentralization Processes on Patients’ Satisfaction: Evidence from Two Public Romanian Hospitals across Two Decades. Sustainability. 2022; 14(8):4818. https://doi.org/10.3390/su14084818
Chicago/Turabian StyleDulău, Dorel, Lisa Craiut, Delia Mirela Tit, Camelia Buhas, Alexandra Georgiana Tarce, and Diana Uivarosan. 2022. "Effects of Hospital Decentralization Processes on Patients’ Satisfaction: Evidence from Two Public Romanian Hospitals across Two Decades" Sustainability 14, no. 8: 4818. https://doi.org/10.3390/su14084818








