A Case Study of Human Milk Banking with Focus on the Role of IoT Sensor Technology
Abstract
:1. Introduction
2. Background Study
2.1. Challenges of Producing and Maintaining Optimal Quality of Human Milk
2.2. Policies and Operation of Human Milk Bank Services
3. Processes Involved in Human Milk Handling
3.1. Screening and Selecting Donors
- has previously tested positive for HIV 1 or 2, hepatitis B or C, HTLV type I or II or syphilis;
- is at an increased risk of vCJD;
- is using, or has recently used, recreational drugs;
- currently smokes or uses nicotine replacement therapy (NRT);
- regularly exceeds recommended alcohol levels for breastfeeding mothers (1 to 2 units, once or twice a week);
- exceeds more than three caffeinated drinks (150–200 ml) daily.
3.2. Milk Collection and Handling
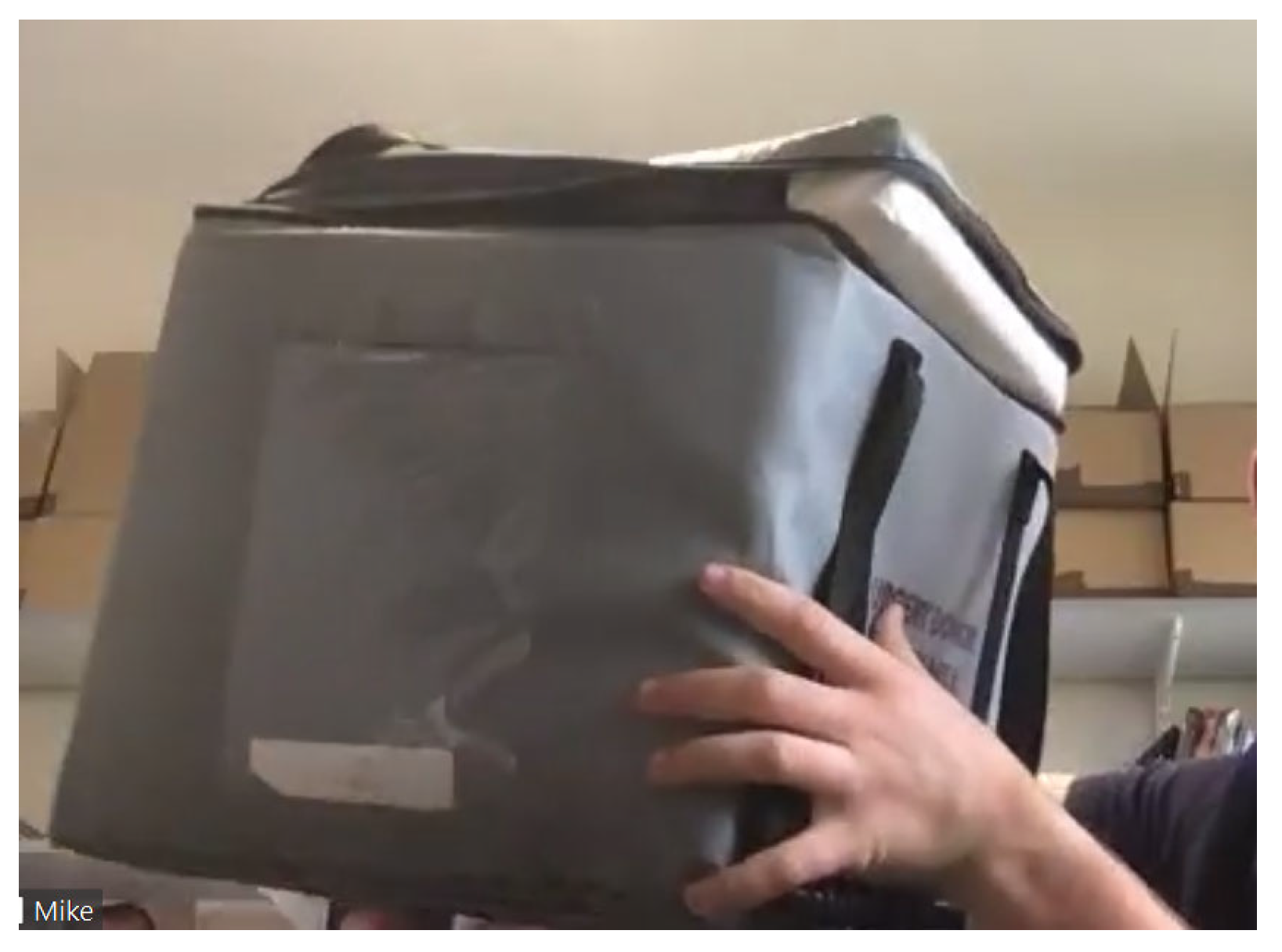
3.3. Transportation, Handling and Tracking
3.4. Pasteurisation
3.5. Bacteriological Testing of Milk (Selection and Classification)
3.6. Storage of Milk in HMBs
4. Methodology
4.1. Background
4.2. Hearts Milk Bank (HMB)
4.3. Operational Conditions
4.4. Problems
5. Adapting Internet of Things and Big Data Technologies to Monitor Temperature of Milk during Transportation for HMF—REAMIT Technology Demonstration
5.1. Strengths and Capabilities of IoT and Big Data Technologies
5.2. Saving Wastage of Milk and Improving Sustainability
- Reduced wastage of milk: In theory, the continuous monitoring of milk temperature during transportation helps to detect quality issues on time. If the temperature of milk deviates from optimal levels, this deviation can be immediately detected with automated data analytics algorithms. Stakeholders can be immediately notified so that corrective actions are taken rapidly. However, our experience shows that milk is almost always stored at optimal temperature during transport. However, this continuous monitoring provides quality assurance as shown in the next point below.
- Quality assurance of transported milk: Since the temperature of milk is monitored throughout transport, the organization obtains the reliability of assured quality of milk during transportation. Without this monitoring, while the organization made every effort to ensure optimal temperature, there was less reliability as temperature was not explicitly measured during the transportation of milk. It has to be noted that the organization has other means of quality assurance, for example by sending the milk to labs for testing before sending to hospitals. The monitoring of temperature of milk during transportation has added more levels of quality assurance.
- Improved milk availability: Stocks of DHM are still relatively limited and therefore precious. By helping to minimize wastage of DHM, these technologies may increase availability, which could contribute to saving the lives of vulnerable babies through the avoidance of life-threatening complications.
- Reduce costs: Continuous monitoring of temperature during milk transportation can help the organization reduce costs. For example, if the sensors indicate that milk is stored well below the lower threshold in which they have to be kept, it is an indication that too many resources are being used for cooling milk. This will help the organization to consider using lower energy for cooling—for example, by using fewer ice packs, which will reduce the cost of cooling.
- Improve sustainability: The above points highlight how monitoring the temperature of milk using IoT technology can help not only save milk for organisations, but also support the social cause of improving milk availability to society. There are environmental benefits as well. For example, by helping to optimize cooling effort during milk transportation, energy can be saved, which translates to reduced carbon emissions. Thus, these technologies contribute to overall sustainability.
6. Conclusions and Future Research
“The REAMIT team have been fantastic! They’ve provided everything from proof of concept to the innovative sensors that we’re using, that not only track temperature but are able to track humidity, acceleration, they can tell when the boxes will be actively moving—so we can really understand where the milk is, what conditions the milk is transported in and when it’s arrived”.
“The REAMIT project is a fantastic initiative, and they approached us about a year ago to see if we could work together to look at the cold chain technology and remote temperature sensing.
One of the big question marks that we have about our cold chain is how well the milk is maintained at temperature, while it’s being transported from donor’s houses or from hospitals into the milk bank, and then again from the milk bank into the hospitals or recipient’s families. It’s really critical that we address that quickly and REAMIT is helping us to do that”.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Binte Abu Bakar, S.Y.; Salim, M.; Clulow, A.J.; Nicholas, K.R.; Boyd, B.J. Human Milk Composition and the Effects of Pasteurisation on the Activity of Its Components. Trends Food Sci. Technol. 2021, 111, 166–174. [Google Scholar] [CrossRef]
- Meng, F.; Uniacke-Lowe, T.; Ryan, A.C.; Kelly, A.L. The Composition and Physico-Chemical Properties of Human Milk: A Review. Trends Food Sci. Technol. 2021, 112, 608–621. [Google Scholar] [CrossRef]
- Weaver, G.; Bertino, E.; Gebauer, C.; Grovslien, A.; Mileusnic-Milenovic, R.; Arslanoglu, S.; Barnett, D.; Boquien, C.-Y.; Buffin, R.; Gaya, A.; et al. Recommendations for the Establishment and Operation of Human Milk Banks in Europe: A Consensus Statement From the European Milk Bank Association (EMBA). Front. Pediatr. 2019, 7, 53. [Google Scholar] [CrossRef]
- WHO. Guidelines on Optimal Feeding of Low Birth-Weight Infants in Low-and Middle Income Countries; 2011. Available online: https://apps.who.int/iris/handle/10665/85670 (accessed on 1 December 2022).
- Zhang, N.; Li, J.Y.; Liu, X.W.; Jiang, Y.L.; Redding, S.R.; Ouyang, Y.Q. Factors Associated with Postpartum Women’s Knowledge, Attitude and Practice Regarding Human Milk Banks and Milk Donation: A Cross-Sectional Survey. Midwifery 2020, 91, 102837. [Google Scholar] [CrossRef]
- Committee on Nutrition; Section on Breastfeeding; Committee on Fetus and Newborn. Donor Human Milk for the High-Risk Infant: Preparation, Safety, and Usage Options in the United States. Pediatrics 2017, 139, e20163440. [Google Scholar] [CrossRef] [Green Version]
- Zanganeh, M.; Jordan, M.; Mistry, H. A systematic review of economic evaluations for donor human milk versus standard feeding in infants. Matern. Child Nutr. 2021, 17, e13151. [Google Scholar] [CrossRef]
- Israel-Ballard, K.; Engmann, C.; Cohen, J.; Mansen, K.; Parker, M.; Kelley, M.; Brooks, E.; Chatzixiros, E.; Clark, D.; Grummer-Strawn, L.; et al. Call to Action for Equitable Access to Human Milk for Vulnerable Infants. Lancet Glob. Health 2019, 7, e1484–e1486. [Google Scholar] [CrossRef]
- Steele, C. Best Practices for Handling and Administration of Expressed Human Milk and Donor Human Milk for Hospitalized Preterm Infants. Front. Nutr. 2018, 5, 76. [Google Scholar] [CrossRef] [Green Version]
- Aronyk, S.; Ryan, P.M.; O’Shea, C.-A.; Ryan, C.A. Waste Not, Want Not: Donor Human Milk Discard in Infants Is Related to Container Size. Acta Paediatr. 2020, 109, 2592–2593. [Google Scholar] [CrossRef]
- Shenker, N.; Tennant, M.; Rickard, L.; Huppertz, P.; Cheung, T.; Houston, R.; Liu, P.; Parkin, C.; Stephen, M. Understanding and Mitigating the Carbon Footprint of Human Milk Banking. In Proceedings of the Climate Change Working Group; BMJ Publishing Group Ltd. and Royal College of Paediatrics and Child Health: London, UK, 2022; p. A313. [Google Scholar]
- Astill, J.; Dara, R.A.; Campbell, M.; Farber, J.M.; Fraser, E.D.G.; Sharif, S.; Yada, R.Y. Transparency in Food Supply Chains: A Review of Enabling Technology Solutions. Trends Food Sci. Technol. 2019, 91, 240–247. [Google Scholar] [CrossRef]
- HMF Human Milk Foundation (2022). Available online: https://humanmilkfoundation.org/ (accessed on 1 December 2022).
- Molefe, L.; Henney, A.J. Donated Breastmilk Monitoring in the Western Cape's Milk Banks. In Proceedings of the 2022 Conference on Information Communications Technology and Society (ICTAS) IEEE, Durban, South Africa, 9–10 March 2022; pp. 1–6. [Google Scholar]
- WHO. The International Code of Marketing of Breast-Milk Substitutes; World Health Organization: Geneva, Switzerland, 2008.
- Bhat, B.V.; Adhisivam, B. Human Milk Banking and Challenges in Quality Control. Indian J. Pediatr. 2018, 85, 255–256. [Google Scholar] [CrossRef] [Green Version]
- Renfrew, M.; Craig, D.; Dyson, L.; McCormick, F.; Rice, S.; King, S.; Misso, K.; Stenhouse, E.; Williams, A. Breastfeeding Promotion for Infants in Neonatal Units: A Systematic Review and Economic Analysis. Health Technol. Assess. 2009, 13, 1–146. [Google Scholar] [CrossRef] [Green Version]
- NICE. The Operation of Donor Milk Bank Services; Donor Breast Milk Banks: London, UK, 2010. [Google Scholar]
- Paredes, D.E.; Ivo, M.L.; Lucia Arantes, S.; Ferreira Júnior, M.A.; de Queiroz Cardoso, A.I.; Schiaveto de Souza, A.; Silvia Martimbianco de Figueiredo, C.; Dos Santos Ferreira, R.; Kamiya, E.; Karol Gonçalves Sgarbi, A.; et al. Identification of the Causes of Waste Human Milk in a Human Milk Bank. Int. J. Innov. Educ. Res. 2019, 7, 452–459. [Google Scholar] [CrossRef]
- Muller, K.T.C.; Souza, A.I.P.; Cardoso, J.M.F.; Palhares, B.D. Knowledge and Adhesion to Donation of Human Milk of Women Who Gave Birth in a Public Hospital. Interações 2019, 20, 315–326. [Google Scholar] [CrossRef] [Green Version]
- Silva, E.S.; Jesus, L.E.; Santos, E.B.; Castro, N.A.; Fonseca, L.B. Donation of Breastmilk to Human Milk Bank: Knowing the Donor. Demetra Food Nutr. Health 2015, 10, 879–890. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Chan, C.S.; Vaucher, Y.E.; Stellwagen, L.M. Challenges in the Practice of Human Milk Nutrition in the Neonatal Intensive Care Unit. Early Hum. Dev. 2013, 89, S35–S38. [Google Scholar] [CrossRef]
- Simmer, K. The Knowns and Unknowns of Human. Paediatr. Programme 2011, 68, 49–64. [Google Scholar]
- Baumer, J.H. Guidelines for the Establishment and Operation of Human Milk Bank in the UK. Arch. Dis. Child. Educ. Pract. 2004, 89, ep27–ep28. [Google Scholar] [CrossRef] [Green Version]
- Hartmann, B.T.; Pang, W.W.; Keil, A.D.; Hartmann, P.E.; Simmer, K. Best Practice Guidelines for the Operation of a Donor Human Milk Bank in an Australian NICU. Early Hum. Dev. 2007, 83, 667–673. [Google Scholar] [CrossRef]
- Arnold, L.D.W. Global Health Policies That Support the Use of Banked Donor Human Milk: A Human Rights Issue. Int. Breastfeed. J. 2006, 1, 26. [Google Scholar] [CrossRef] [Green Version]
- Reyes-Foster, B.M.; Carter, S.K.; Hinojosa, M.S. Human Milk Handling and Storage Practices among Peer Milk-Sharing Mothers. J. Hum. Lact. 2017, 33, 173–180. [Google Scholar] [CrossRef]
- Eglash, A.; Simon, L. ABM Clinical Protocol #8: Human Milk Storage Information for Home Use for Full-Term Infants, Revised 2017. Breastfeed. Med. 2017, 12, 390–395. [Google Scholar] [CrossRef]
- Sosa, R.; Barness, L. Bacterial Growth in Refrigerated Human Milk. American J. Dis. Child. 1987, 141, 111–112. [Google Scholar] [CrossRef]
- Pardou, A.; Serruys, E.; Mascart-Lemone, F.; Dramaix, M.; Vis, H.L. Human Milk Banking: Influence of Storage Processes and of Bacterial Contamination on Some Milk Constituents. Neonatology 1994, 65, 302–309. [Google Scholar] [CrossRef]
- Eteng, M.U.; Ebong, P.E.; Eyong, E.U.; Ettarh, R.R. Storage beyond Three Hours at Ambient Temperature Alters the Biochemical and Nutritional Qualities of Breast Milk. Afr. J. Reprod. Health 2001, 5, 130–134. [Google Scholar] [CrossRef]
- Labiner-Wolfe, J.; Fein, S.B. How US Mothers Store and Handle Their Expressed Breast Milk. J. Hum. Lact. 2012, 29, 54–58. [Google Scholar] [CrossRef]
- Haiden, N.; Pimpel, B.; Assadian, O.; Binder, C.; Kreissl, A.; Repa, A.; Thanhäuser, M.; Roberts, C.D.; Berger, A. Comparison of Bacterial Counts in Expressed Breast Milk Following Standard or Strict Infection Control Regimens in Neonatal Intensive Care Units: Compliance of Mothers Does Matter. J. Hosp. Infect. 2016, 92, 226–228. [Google Scholar] [CrossRef]
- Chang, Y.-C.; Chen, C.-H.; Lin, M.-C. The Macronutrients in Human Milk Change after Storage in Various Containers. Pediatr. Neonatol. 2012, 53, 205–209. [Google Scholar] [CrossRef] [Green Version]
- Garza, C.; Johnson, C.A.; Harrist, R.; Nichols, B.L. Effects of Methods of Collection and Storage on Nutrients in Human Milk. Early Hum. Dev. 1982, 6, 295–303. [Google Scholar] [CrossRef]
- Takci, S.; Gulmez, D.; Yigit, S.; Dogan, O.; Dik, K.; Hascelik, G. Effects of Freezing on the Bactericidal Activity of Human Milk. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 146–149. [Google Scholar] [CrossRef]
- Goldblum, R.M.; Garza, C.; Johnson, C.A.; Harrist, R.; Nichols, B.L.; Goldman, A.S. Human Milk Banking I. Effects of Container upon Immunologic Factors in Mature Milk. Nutr. Res. 1981, 1, 449–459. [Google Scholar] [CrossRef]
- Rodrigo, R.; Amir, L.H.; Forster, D.A. Review of Guidelines on Expression, Storage and Transport of Breast Milk for Infants in Hospital, to Guide Formulation of Such Recommendations in Sri Lanka. BMC Pediatr. 2018, 18, 271. [Google Scholar] [CrossRef] [Green Version]
- Boersma, S. Expressing, Collecting and Storing of Human Milk; BFI Strategy for Ontario: Toronto, ON, Canada, 2019. [Google Scholar]
- Narayanan, I.; Prakash, K.; Prabhakar, A.K.; Gujral, V. V A Planned Prospective Evaluation of the Anti-Infective Property of Varying Quantities of Expressed Human Milk. Acta Paediatr. Scand. 1982, 71, 441–445. [Google Scholar] [CrossRef]
- Peila, C.; Emmerik, N.E.; Giribaldi, M.; Stahl, B.; Ruitenberg, J.E.; Van Elburg, R.M.; Moro, G.E.; Bertino, E.; Coscia, A.; Cavallarin, L. Human Milk Processing: A Systematic Review of Innovative Techniques to Ensure the Safety and Quality of Donor Milk. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 353–361. [Google Scholar] [CrossRef]
- Piyasena, P.; Mohareb, E.; McKellar, R.C. Inactivation of Microbes Using Ultrasound: A Review. Int. J. Food Microbiol. 2003, 87, 207–216. [Google Scholar] [CrossRef]
- Czank, C.; Simmer, K.; Hartmann, P.E. Simultaneous Pasteurization and Homogenization of Human Milk by Combining Heat and Ultrasound: Effect on Milk Quality. J. Dairy Res. 2010, 77, 183–189. [Google Scholar] [CrossRef]
- Balmer, S.E.; Wharton, B.A. Human Milk Banking at Sorrento Maternity Hospital, Birmingham. Arch. Dis. Child 1992, 67, 556–559. [Google Scholar] [CrossRef] [Green Version]
- Slutzah, M.; Codipilly, C.N.; Potak, D.; Clark, R.M.; Schanler, R.J. Refrigerator Storage of Expressed Human Milk in the Neonatal Intensive Care Unit. J. Pediatr. 2010, 156, 26–28. [Google Scholar] [CrossRef]
- Garg, H.; Sharma, V.; Purohit, S.R. Application of IoT in the Food Processing Industry. In Applications of Artificial Intelligence, Big Data and Internet of Things in Sustainable Development; Goundar, S., Purwar, A., Singh, A., Eds.; CRC Press: Boca Raton, FL, USA, 2022; pp. 183–202. [Google Scholar] [CrossRef]
- Kaur, A.; Singh, G.; Kukreja, V.; Sharma, S.; Singh, S.; Yoon, B. Adaptation of IoT with Blockchain in Food Supply Chain Management: An Analysis-Based Review in Development, Benefits and Potential Applications. Sensors 2022, 22, 8174. [Google Scholar] [CrossRef]
- Mejjaouli, S. Internet of Things based Decision Support System for Green Logistics. Sustainability 2022, 14, 14756. [Google Scholar] [CrossRef]
- da Costa, T.P.; Gillespie, J.; Pelc, K.; Shenker, N.; Weaver, G.; Ramanathan, R.; Murphy, F. An Organisational-Life Cycle Assessment (O-LCA) approach for Internet of Things (IoT) technologies implementation in a human milk bank, manuscript reference sustainability-2061581. Sustainability, 2022; under review. [Google Scholar]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramanathan, U.; Pelc, K.; Costa, T.P.d.; Ramanathan, R.; Shenker, N. A Case Study of Human Milk Banking with Focus on the Role of IoT Sensor Technology. Sustainability 2023, 15, 243. https://doi.org/10.3390/su15010243
Ramanathan U, Pelc K, Costa TPd, Ramanathan R, Shenker N. A Case Study of Human Milk Banking with Focus on the Role of IoT Sensor Technology. Sustainability. 2023; 15(1):243. https://doi.org/10.3390/su15010243
Chicago/Turabian StyleRamanathan, Usha, Katarzyna Pelc, Tamíris Pacheco da Costa, Ramakrishnan Ramanathan, and Natalie Shenker. 2023. "A Case Study of Human Milk Banking with Focus on the Role of IoT Sensor Technology" Sustainability 15, no. 1: 243. https://doi.org/10.3390/su15010243






