Impact of Introversion-Extraversion Personality Traits on Knowledge-Sharing Intention in Online Health Communities: A Multi-Group Analysis
Abstract
1. Introduction
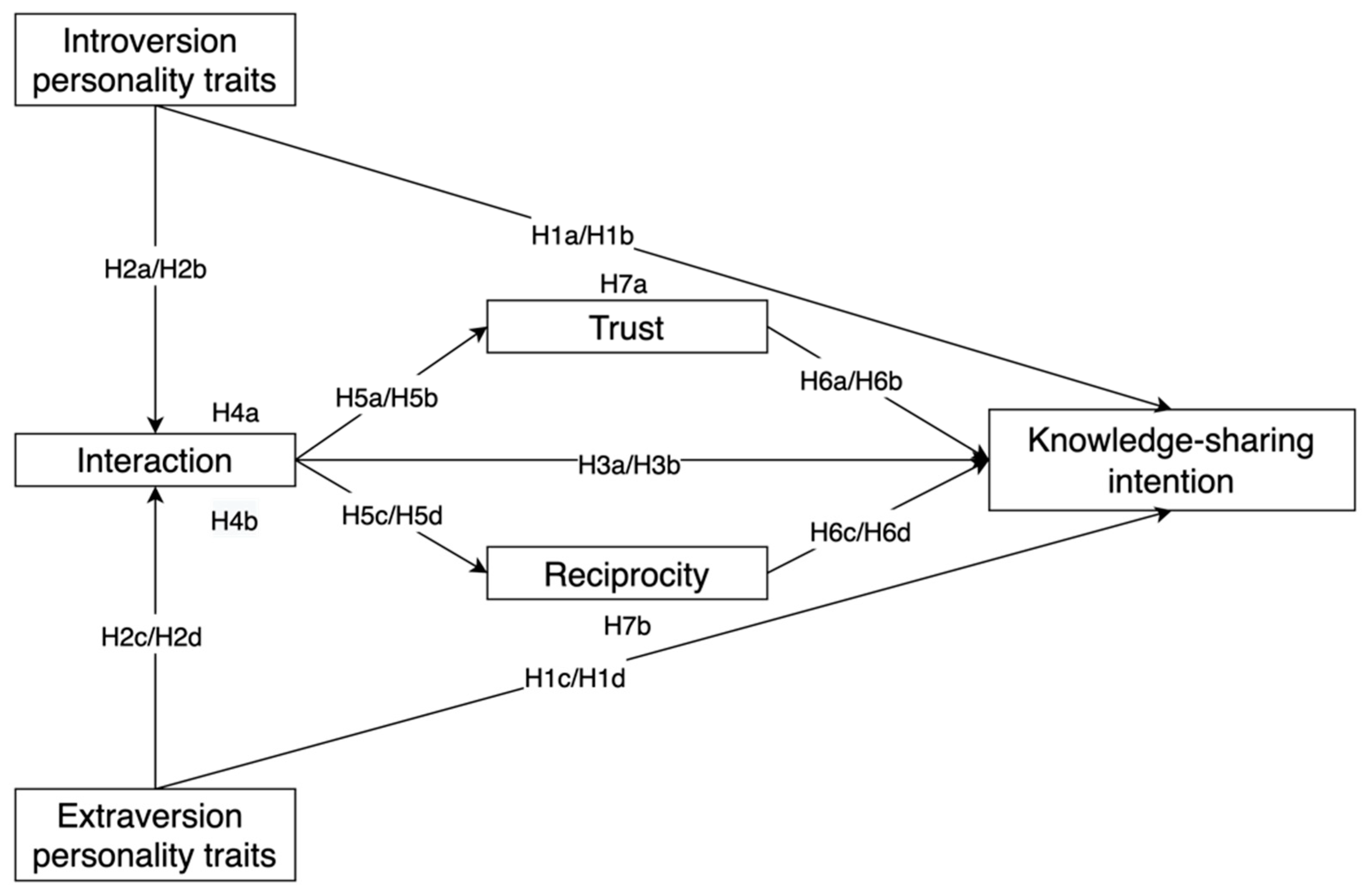
2. Theoretical Analysis and Research Hypothesis
2.1. Personality Traits
2.2. Social Capital Theory
2.3. Introversion-Extraversion Personality Traits and Knowledge-Sharing
2.4. Introversion-Extraversion Personality Traits and Structural Dimensional Capital
2.5. Structural Dimensional Capital and Knowledge-Sharing
2.6. The Mediating Role of Structural Dimensional Capital
2.7. Structural Dimensional Capital and Relationship Dimension Capital
2.8. Relationship Dimension Capital and Knowledge-Sharing
2.9. The Mediating Role of Relationship Dimension Capital
3. Methodology and Measurement
3.1. Sampling Strategy and Sample Collection
3.2. Measurement of Constructs
4. Data Analysis
4.1. Reliability and Validity
4.2. Confirmatory Factor Analysis
4.3. Common Method Variance Test
4.4. Hypotheses Testing and Multi-Group Analysis
4.4.1. Direct Effects Test
4.4.2. Indirect Effect Test
4.4.3. Multi-Group Analysis
5. Discussion
5.1. Theoretical Implications
5.2. Practical Implications
5.3. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Measurement Items | Factor Loading | |
|---|---|---|
| DO | PA | |
| Introversion (INT) | ||
| INT1: Shy | 0.792 | 0.727 |
| INT2: Quiet | 0.779 | 0.784 |
| INT3: Bashful | 0.866 | 0.888 |
| INT4: Withdrawn | 0.865 | 0.883 |
| Extraversion (EXT) | ||
| EXT1: Talkative | 0.747 | 0.804 |
| EXT2: Extroverted | 0.862 | 0.876 |
| EXT3: Bold | 0.789 | 0.824 |
| EXT4: Energetic | 0.775 | 0.804 |
| Interaction (INA) | ||
| INA1: I spend a lot of time interacting with some members in this OHC | 0.792 | 0.886 |
| INA1: I have frequent communication with some members in this OHC | 0.789 | 0.697 |
| INA1: I maintain close social relationships with some members in this OHC | 0.865 | 0.753 |
| Trust (TRU) | ||
| TRU1: Members in this OHCs will not take advantage of others even when the opportunity arises | 0.803 | 0.829 |
| TRU2: Members in this OHC will always keep the promises they make to one another | 0.805 | 0.841 |
| TRU3: Members in this OHC would not knowingly do anything to disrupt the conversation | 0.751 | 0.806 |
| TRU4: Members in this OHC are truthful in dealing with one another | 0.805 | 0.813 |
| Reciprocity (REC) | ||
| REC1: When I share knowledge in this OHC, I believe that my questions will be answered in the future | 0.827 | 0.855 |
| REC2: I believe that other members I interact with would help me if I was in need | 0.759 | 0.812 |
| REC3: When I share my knowledge in this OHC, I expect some other members to respond when I am in need | 0.774 | 0.825 |
| Knowledge-sharing (KSI) | ||
| KSI1: I intend to share knowledge with other members | 0.716 | 0.750 |
| KSI2: I am always willing to share knowledge with other members when they ask | 0.770 | 0.819 |
| KSI3: I am always trying to share knowledge with other members | 0.780 | 0.786 |
References
- Sun, Y.; Feng, Y.; Shen, X.-L.; Guo, X. Fear appeal, coping appeal and mobile health technology persuasion: A two-stage scenario-based survey of the elderly. Inf. Technol. People, 2022; online ahead-of-print. [Google Scholar] [CrossRef]
- Htay, M.N.N.; Parial, L.L.; Tolabing, M.C.; Dadaczynski, K.; Okan, O.; Leung, A.Y.M.; Su, T.T. Digital health literacy, online information-seeking behaviour, and satisfaction of COVID-19 information among the university students of East and South-East Asia. PLoS ONE 2022, 17, e0266276. [Google Scholar] [CrossRef] [PubMed]
- Scantlebury, A.; Booth, A.; Hanley, B. Experiences, practices and barriers to accessing health information: A qualitative study. Int. J. Med. Inform. 2017, 103, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Hao, D.; Zhang, R.; Bai, K. An integrated approach for service quality evaluation of online health communities based on q-rung orthopair fuzzy linguistic aggregation operators. J. Intell. Fuzzy Syst. 2022, 42, 1907–1924. [Google Scholar] [CrossRef]
- Atanasova, S.; Kamin, T.; Petric, G. Exploring the benefits and challenges of health professionals’ participation in online health communities: Emergence of (dis)empowerment processes and outcomes. Int. J. Med. Inform. 2017, 98, 13–21. [Google Scholar] [CrossRef]
- Rajak, M.; Shaw, K. An extension of technology acceptance model for mHealth user adoption. Technol. Soc. 2021, 67, 101800. [Google Scholar] [CrossRef]
- Shang, L.; Zuo, M.; Ma, D.; Yu, Q. The Antecedents and Consequences of Health Care Professional-Patient Online Interactions: Systematic Review. J. Med. Internet Res. 2019, 21, e13940. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Zhang, X.; Liu, L.; Ren, C. Converting readers to patients? From free to paid knowledge-sharing in online health communities. Inf. Process. Manag. 2021, 58, 102490. [Google Scholar] [CrossRef]
- Qiao, W.; Yan, Z.; Wang, X. Join or not: The impact of physicians’ group joining behavior on their online demand and reputation in online health communities. Inf. Process. Manag. 2021, 58, 102634. [Google Scholar] [CrossRef]
- Huang, K.-Y.; Chengalur-Smith, I.; Pinsonneault, A. Sharing Is Caring: Social Support Provision and Companionship Activities in Healthcare Virtual Support Communities. MIS Q. 2019, 43, 395–423. [Google Scholar] [CrossRef]
- Liu, N.; Tong, Y.; Chan, H.C. Dual effects of social support seeking in patient-centric online healthcare communities: A longitudinal study. Inf. Manag. 2020, 57, 103270. [Google Scholar] [CrossRef]
- Deng, S.; Lin, Y.; Liu, Y.; Chen, X.; Li, H. How Do Personality Traits Shape Information-Sharing Behaviour in Social Media? Exploring the Mediating Effect of Generalized Trust. Inf. Res. Int. Electron. J. 2017, 22, 763. [Google Scholar]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge sharing in online health communities: A social exchange theory perspective. Inf. Manage. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Shamlou, Z.; Saberi, M.K.; Amiri, M.R. Application of theory of planned behavior in identifying factors affecting online health information seeking intention and behavior of women. Aslib J. Inf. Manag. 2022, 74, 727–744. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Deng, Z.; Chen, X. Knowledge sharing motivations in online health communities: A comparative study of health professionals and normal users. Comput. Hum. Behav. 2017, 75, 797–810. [Google Scholar] [CrossRef]
- Allport, G.W. Personality: A Psychological Interpretation; Henry Holt: New York, NY, USA, 1937. [Google Scholar]
- Moon, Y.J.; Kim, W.G.; Armstrong, D.J. Exploring neuroticism and extraversion in flow and user generated content consumption. Inf. Manag. 2014, 51, 347–358. [Google Scholar] [CrossRef]
- Pour, M.J.; Taheri, F. Personality traits and knowledge sharing behavior in social media: Mediating role of trust and subjective well-being. Horiz. 2019, 27, 98–117. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T. Validation of the five-factor model of personality across instruments and observers. J. Personal. Soc. Psychol. 1987, 52, 81–90. [Google Scholar] [CrossRef]
- McLure Wasko, M.; Faraj, S. Why Should I Share? Examining Social Capital and Knowledge Contribution in Electronic Networks of Practice. MIS Q. 2005, 29, 35–57. [Google Scholar] [CrossRef]
- Ramezan, M. Intellectual capital and organizational organic structure in knowledge society: How are these concepts related? Int. J. Inf. Manag. 2011, 31, 88–95. [Google Scholar] [CrossRef]
- Han, S.H.; Yoon, S.W.; Chae, C. Building social capital and learning relationships through knowledge sharing: A social network approach of management students’ cases. J. Knowl. Manag. 2020, 24, 921–939. [Google Scholar] [CrossRef]
- Tsai, W.; Ghoshal, S. Social Capital and Value Creation: The Role of Intrafirm Networks. Acad. Manage. J. 1998, 41, 464–476. [Google Scholar] [CrossRef]
- Chiu, C.-M.; Hsu, M.-H.; Wang, E.T.G. Understanding knowledge sharing in virtual communities: An integration of social capital and social cognitive theories. Decis. Support Syst. 2006, 42, 1872–1888. [Google Scholar] [CrossRef]
- Chang, H.H.; Chuang, S.-S. Social capital and individual motivations on knowledge sharing: Participant involvement as a moderator. Inf. Manag. 2011, 48, 9–18. [Google Scholar] [CrossRef]
- Wu, W.-Y.; Sukoco, B.M. Why Should i Share? Examining Consumers’ Motives and Trust on Knowledge Sharing. J. Comput. Inf. Syst. 2010, 50, 11–19. [Google Scholar] [CrossRef]
- Hasan, S.; Koning, R. Conversations and idea generation: Evidence from a field experiment. Res. Policy 2019, 48, 103811. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, R. Association Between eHealth Literacy in Online Health Communities and Patient Adherence: Cross-sectional Questionnaire Study. J. Med. Internet Res. 2021, 23, e14908. [Google Scholar] [CrossRef]
- Yuchao, W.; Ying, Z.; Liao, Z. Health privacy information self-disclosure in online health community. Front. Public Health 2021, 8, 602792. [Google Scholar] [CrossRef]
- Wang, K.; Lv, Y.; Zhang, Z. Relationship between extroversion and social use of social networking sites. Soc. Behav. Personal. 2018, 46, 1597–1610. [Google Scholar] [CrossRef]
- Borgatti, S.P.; Cross, R. A relational view of information seeking and learning in social networks. Manag. Sci. 2003, 49, 432–445. [Google Scholar] [CrossRef]
- Cipolletta, S.; Mocellin, D. Online counseling: An exploratory survey of Italian psychologists’ attitudes towards new ways of interaction. Psychother. Res. 2018, 28, 909–924. [Google Scholar] [CrossRef]
- Zhang, C.-B.; Li, Y.-N.; Wu, B.; Li, D.-J. How WeChat can retain users: Roles of network externalities, social interaction ties, and perceived values in building continuance intention. Comput. Hum. Behav. 2017, 69, 284–293. [Google Scholar] [CrossRef]
- Chavez, L.; Ruiz, C.; Curras, R.; Hernandez, B. The role of travel motivations and social media use in consumer interactive behaviour: A uses and gratifications perspective. Sustainability 2020, 12, 8789. [Google Scholar] [CrossRef]
- Rukavina, T.V.; Viskic, J.; Poplasen, L.M.; Relic, D.; Marelic, M.; Jokic, D.; Sedak, K. Dangers and Benefits of Social Media on E-Professionalism of Health Care Professionals: Scoping Review. J. Med. Internet Res. 2021, 23, e25770. [Google Scholar] [CrossRef] [PubMed]
- Lefebvre, V.M.; Sorenson, D.; Henchion, M.; Gellynck, X. Social capital and knowledge sharing performance of learning networks. Int. J. Inf. Manag. 2016, 36, 570–579. [Google Scholar] [CrossRef]
- Cain, J.A.; Imre, I. Everybody wants some: Collection and control of personal information, privacy concerns, and social media use. New Media Soc. 2021, 24, 2705–2724. [Google Scholar] [CrossRef]
- Wang, W.-T.; Lin, Y.-L. Evaluating Factors Influencing Knowledge-Sharing Behavior of Students in Online Problem-Based Learning. Front. Psychol. 2021, 12, 691755. [Google Scholar] [CrossRef]
- Roslan, N.S.; Izhar, L.I.; Faye, I.; Saad, M.N.M.; Sivapalan, S.; Rahman, M.A. Review of EEG and ERP studies of extraversion personality for baseline and cognitive tasks. Personal. Individ. Differ. 2017, 119, 323–332. [Google Scholar] [CrossRef]
- Brindal, E.; Ryan, J.C.; Kakoschke, N.; Golley, S.; Zajac, I.T.; Wiggins, B. Individual differences and changes in lifestyle behaviours predict decreased subjective well-being during COVID-19 restrictions in an Australian sample. J. Public Health 2021, 44, 450–456. [Google Scholar] [CrossRef]
- Li, C.; Li, H.; Suomi, R.; Liu, Y. Knowledge sharing in online smoking cessation communities: A social capital perspective. Internet Res. 2021, 32, 111–138. [Google Scholar] [CrossRef]
- Zhang, J.; Ma, Y. The influence of social capital on users’ loyalty to virtual communities. Sci. Res. Manag. 2021, 42, 139–149. [Google Scholar] [CrossRef]
- Lu, Y.; Yang, D. Information exchange in virtual communities under extreme disaster conditions. Decis. Support Syst. 2011, 50, 529–538. [Google Scholar] [CrossRef]
- Masri, N.W.; You, J.-J.; Ruangkanjanases, A.; Chen, S.-C. The Effects of Customer Learning and Shopping Value on Intention Purchase and Reuse in a Digital Market: The Institutional Trust-Commitment Perspective. Sustainability 2021, 13, 4318. [Google Scholar] [CrossRef]
- Hsieh, P.-J. Determinants of Knowledge-Sharing Intentions for Shared Decision-Making Platforms. J. Comput. Inf. Syst. 2021, 62, 1088–1099. [Google Scholar] [CrossRef]
- Kim, D.J.; Salvacion, M.; Salehan, M.; Kim, D.W. An empirical study of community cohesiveness, community attachment, and their roles in virtual community participation. Eur. J. Inf. Syst. 2022, 1–28. [Google Scholar] [CrossRef]
- Yan, L.; Tan, Y. Feeling Blue? Go Online: An Empirical Study of Social Support Among Patients. Inf. Syst. Res. 2014, 25, 690–709. [Google Scholar] [CrossRef]
- Smedley, R.; Coulson, N.; Gavin, J.; Rodham, K.; Watts, L. Online social support for Complex Regional Pain Syndrome: A content analysis of support exchanges within a newly launched discussion forum. Comput. Hum. Behav. 2015, 51, 53–63. [Google Scholar] [CrossRef]
- Liang, B.; Scammon, D.L. E-Word-of-Mouth on health social networking sites: An opportunity for tailored health communication. J. Consum. Behav. 2011, 10, 322–331. [Google Scholar] [CrossRef]
- Sousa-Duarte, F.; Brown, P.; Mendes, A.M. Healthcare professionals’ trust in patients: A review of the empirical and theoretical literatures. Sociol. Compass 2020, 14, 1–15. [Google Scholar] [CrossRef]
- Ouyang, P.; Wang, J.-J. Physician’s online image and patient’s choice in the online health community. Internet Res. 2022, 32, 1952–1977. [Google Scholar] [CrossRef]
- Pearson, S.D.; Raeke, L.H. Patients’ trust in physicians: Many theories, few measures, and little data. J. Gen. Intern. Med. 2000, 15, 509–513. [Google Scholar] [CrossRef]
- Shaw, B.R.; McTavish, F.; Hawkins, R.; Gustafson, D.H.; Pingree, S. Experiences of women with breast cancer: Exchanging social support over the CHESS computer network. J. Health Commun. 2000, 5, 135–159. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Lin, Z.; Nie, J. How Personality and Social Capital Affect Knowledge Sharing Intention in Online Health Support Groups?: A Person-Situation Perspective. Int. J. Hum.-Comput. Interact. 2022, 38, 885–896. [Google Scholar] [CrossRef]
- Zhao, H.; Wang, J.; Zhang, H. Influence of social support on individual health knowledge adoption in online diabetes communities: The mediating role between cognition and emotion. Aslib J. Inf. Manag. 2022, 74, 1048–1069. [Google Scholar] [CrossRef]
- Sun, F.; Yang, F.; Zheng, S. Evaluation of the Liver Disease Information in Baidu Encyclopedia and Wikipedia: Longitudinal Study. J. Med. Internet Res. 2021, 23, e17680. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-L. Impact of communication on capital project performance: A mediated moderation model. Sustainability 2021, 13, 11301. [Google Scholar] [CrossRef]
- Choi, G.; Nam, C.; Kim, S.; Jung, H.J.; Lee, C.H. Where does knowledge-sharing motivation come from? The case of third-party developer in mobile platforms. J. Knowl. Manag. 2020, 24, 1681–1704. [Google Scholar] [CrossRef]
- Saucier, G. Mini-markers: A brief version of Goldberg’s unipolar big-five markers. J. Personal. Assess. 1994, 63, 506–516. [Google Scholar] [CrossRef]
- Huang, Q.; Davison, R.M.; Gu, J. Impact of personal and cultural factors on knowledge sharing in China. Asia Pac. J. Manag. 2008, 25, 451–471. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Chen, S.; Guo, X.; Wu, T.; Ju, X. Exploring the Online Doctor-Patient Interaction on Patient Satisfaction Based on Text Mining and Empirical Analysis. Inf. Process. Manag. 2020, 57, 102253. [Google Scholar] [CrossRef]
- Nahapiet, J.; Ghoshal, S. Social capital, intellectual capital, and the organizational advantage. Acad. Manag. Rev. 1998, 23, 242–266. [Google Scholar] [CrossRef]
| Category | Total (n = 571)) | Doctor (n = 243) | Patient (n = 328) | |
|---|---|---|---|---|
| Sex | Man | 324 (56.74%) | 160 (48.78%) | 164 (67.49%) |
| Woman | 247 (43.25%) | 168 (51.22%) | 79 (32.51%) | |
| Age | <25 | 46 (8.056%) | 31 (9.451%) | 15 (6.173%) |
| 25~30 | 149 (26.095%) | 101 (30.793%) | 48 (19.753%) | |
| 31~40 | 205 (35.902%) | 107 (32.622%) | 98 (40.329%) | |
| 41~50 | 118 (20.665%) | 55 (16.768%) | 63 (25.926%) | |
| >50 | 53 (9.282%) | 34 (10.366%) | 19 (7.819%) | |
| Education level | Below high school | 13 (2.277%) | 7 (2.134%) | 6 (2.469%) |
| College | 288 (50.438%) | 172 (52.439%) | 116 (47.737%) | |
| Master and above | 166 (29.072%) | 96 (29.268%) | 70 (28.807%) | |
| Monthly income | <2001 | 65 (11.384%) | 30 (9.146%) | 35 (14.403%) |
| 2001~4000 | 28 (4.904%) | 17 (5.183%) | 11 (4.527%) | |
| 4001~6000 | 11 (1.926%) | 6 (1.829%) | 5 (2.058%) | |
| 6001~8000 | 35 (6.13%) | 35 (10.671%) | 0 (0%) | |
| 8001~10000 | 352 (61.646%) | 213 (64.939%) | 139 (57.202%) | |
| >10000 | 184 (32.224%) | 80 (24.39%) | 104 (42.798%) | |
| Involving time | <6 months | 33 (5.779%) | 20 (6.098%) | 13 (5.35%) |
| 6~12 months | 38 (6.655%) | 22 (6.707%) | 16 (6.584%) | |
| 12~24 months | 53 (9.282%) | 34 (10.366%) | 19 (7.819%) | |
| 24~36 months | 110 (19.264%) | 75 (22.866%) | 35 (14.403%) | |
| >36 months | 337 (59.019%) | 177 (53.963%) | 160 (65.844%) | |
| Items | Doctors | Patients | ||||
|---|---|---|---|---|---|---|
| Cronbach’s Alpha | AVE | CR | Cronbach’s Alpha | AVE | CR | |
| INT | 0.893 | 0.683 | 0.896 | 0.889 | 0.678 | 0.893 |
| EXT | 0.869 | 0.631 | 0.872 | 0.895 | 0.685 | 0.897 |
| INA | 0.855 | 0.666 | 0.857 | 0.817 | 0.613 | 0.824 |
| TRU | 0.865 | 0.626 | 0.87 | 0.889 | 0.676 | 0.893 |
| REC | 0.822 | 0.62 | 0.83 | 0.864 | 0.69 | 0.87 |
| KSI | 0.796 | 0.571 | 0.8 | 0.827 | 0.617 | 0.828 |
| Mean | SD | INT | EXT | INA | TRU | REC | KSI | |
|---|---|---|---|---|---|---|---|---|
| Doctors | ||||||||
| INT | 4.383 | 1.507 | 0.826 | |||||
| EXT | 4.366 | 1.568 | 0.314 *** | 0.794 | ||||
| INA | 4.535 | 1.636 | 0.479 *** | 0.500 *** | 0.816 | |||
| TRU | 5.062 | 1.464 | 0.335 *** | 0.305 *** | 0.491 *** | 0.791 | ||
| REC | 4.680 | 1.602 | 0.322 *** | 0.290 *** | 0.421 *** | 0.288 *** | 0.787 | |
| KSI | 4.930 | 1.222 | 0.610 *** | 0.560 *** | 0.692 *** | 0.599 *** | 0.591 *** | 0.756 |
| Patients | ||||||||
| INT | 4.287 | 1.526 | 0.823 | |||||
| EXT | 4.740 | 1.636 | 0.268 *** | 0.828 | ||||
| INA | 4.977 | 1.518 | 0.098 | 0.145 ** | 0.783 | |||
| TRU | 5.152 | 1.468 | 0.078 | 0.071 | 0.147 ** | 0.822 | ||
| REC | 4.998 | 1.642 | 0.102 | 0.082 | 0.151 ** | 0.112 * | 0.831 | |
| KSI | 5.296 | 1.218 | 0.141 * | 0.328 *** | 0.330 *** | 0.146 ** | 0.182 *** | 0.785 |
| Regression Path | Doctors | Patients | Doctors-Patients Path Differences Comparison | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Path Coefficient | p | Result | Path Coefficient | p | Result | Differences | p | Result | |
| INA←INT | 0.403 | *** | H2a (S) | 0.089 | 0.174 | H2a (NS) | 0.314 | 0.003 | H2b (S) |
| INA←EXT | 0.439 | *** | H2c (S) | 0.147 | 0.026 | H2c (S) | 0.292 | *** | H2d (S) |
| TRU←INA | 0.581 | *** | H5a (S) | 0.185 | 0.004 | H5a (S) | 0.396 | *** | H5b (S) |
| REC←INA | 0.526 | *** | H5c (S) | 0.164 | 0.012 | H5c (S) | 0.362 | *** | H5d (S) |
| KSI←INT | 0.304 | *** | H1a (S) | 0.004 | 0.952 | H1a (NS) | 0.3 | *** | H1b (S) |
| KSI←EXT | 0.209 | *** | H1c (S) | 0.305 | *** | H1c (S) | −0.096 | 0.159 | H1d (NS) |
| KSI←INA | 0.205 | 0.009 | H3a (S) | 0.308 | *** | H3a (S) | −0.103 | 0.138 | H3b (NS) |
| KSI←TRU | 0.31 | *** | H6a (S) | 0.065 | 0.274 | H6a (NS) | 0.245 | 0.002 | H6b (S) |
| KSI←REC | 0.339 | *** | H6c (S) | 0.137 | 0.023 | H6c (S) | 0.202 | 0.009 | H6d (S) |
| Regression Path | Effect | SE | Bias Corrected (95%) | Percentile Method (95%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| LLCI | ULCI | p | LLCI | ULCI | p | ||||
| Doctors | INT→INA→KSI | 0.083 | 0.039 | 0.016 | 0.169 | 0.017 | 0.012 | 0.164 | 0.022 |
| EXT→INA→KSI | 0.09 | 0.04 | 0.018 | 0.179 | 0.016 | 0.014 | 0.173 | 0.022 | |
| INA→TRU→KSI | 0.18 | 0.037 | 0.116 | 0.263 | 0 | 0.112 | 0.259 | 0 | |
| INA→REC→KSI | 0.178 | 0.037 | 0.115 | 0.259 | 0 | 0.112 | 0.256 | 0 | |
| Patients | INT→INA→KSI | 0.028 | 0.022 | −0.008 | 0.08 | 0.131 | −0.01 | 0.075 | 0.171 |
| EXT→INA→KSI | 0.045 | 0.022 | 0.01 | 0.096 | 0.014 | 0.007 | 0.092 | 0.022 | |
| INA→TRU→KSI | 0.012 | 0.013 | −0.006 | 0.048 | 0.198 | −0.009 | 0.043 | 0.288 | |
| INA→REC→KSI | 0.022 | 0.013 | 0.003 | 0.059 | 0.016 | 0.001 | 0.052 | 0.037 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lv, M.; Sun, Y.; Shi, B. Impact of Introversion-Extraversion Personality Traits on Knowledge-Sharing Intention in Online Health Communities: A Multi-Group Analysis. Sustainability 2023, 15, 417. https://doi.org/10.3390/su15010417
Lv M, Sun Y, Shi B. Impact of Introversion-Extraversion Personality Traits on Knowledge-Sharing Intention in Online Health Communities: A Multi-Group Analysis. Sustainability. 2023; 15(1):417. https://doi.org/10.3390/su15010417
Chicago/Turabian StyleLv, Mian, Yongbo Sun, and Binbin Shi. 2023. "Impact of Introversion-Extraversion Personality Traits on Knowledge-Sharing Intention in Online Health Communities: A Multi-Group Analysis" Sustainability 15, no. 1: 417. https://doi.org/10.3390/su15010417
APA StyleLv, M., Sun, Y., & Shi, B. (2023). Impact of Introversion-Extraversion Personality Traits on Knowledge-Sharing Intention in Online Health Communities: A Multi-Group Analysis. Sustainability, 15(1), 417. https://doi.org/10.3390/su15010417






