The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework
Abstract
1. Introduction
What are the successful environmental sustainability activities reported in the scientific literature by internationally representative healthcare facilities? What indicators can be defined in order to form a comprehensive innovative framework for environmental sustainability assessment? How can the indicators of the innovative framework be qualitatively and numerically defined in such a way as to enable the assessment of organizational sustainability and allow the tracking of implementation progress?
2. Materials and Methods
- Defining the fields of the new innovative framework by integrating environmental, economic, and social sustainability requirements along with sustainable medical practices, which are organized into the four steps of the quality cycle;
- Collecting the latest medical practices from hospitals related to environmental sustainability that are reported and confirmed in international scientific studies by exploring the relevant databases and studying the latest medical scientific literature;
- Conceptualizing the content and evaluation grids of environmental responsibility-related indicators based on the successful healthcare practices extracted from the knowledge-based literature;
- Conceptualizing an indicator matrix of the innovative framework by establishing connections between the basic medical activities organized in the sequence of the quality cycle and the core subjects of the social responsibility standard;
- Validation in practice of the innovative framework through implementation and self-evaluation at an emergency hospital.
2.1. Innovative Framework Areas
2.2. Evidence of Environmental Sustainability in Healthcare Organizations
2.2.1. Indicators for Healthcare Service Design
2.2.2. Indicators for Healthcare Service Provision
2.2.3. Indicators for Healthcare Service Evaluation
2.2.4. Indicators for Continuous Improvement
2.3. Designing the Content of the Indicators and the Evaluation Model
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Indicator | PA4—Environmental Impact Plan |
|---|---|
| Description | Environmental impact reduction schemes that are developed in relation to the scope. |
| Evaluation question | Are you aware of the impact of your healthcare activities on the environment (atmosphere/soil/water)? Are the activities carried out polluting the atmosphere and/or soil and/or water? Are there greenhouse gases emitted into the atmosphere? Is the impact of waste on the environment known? How are they considered and what actions are set? Is there concern in the organization regarding the environmental impact on water, or are these effects taken into account? If so, how? What treatment is applied to organic waste? What treatment is applied to inorganic waste? What treatment is applied to toxic waste? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | The impact of own healthcare activities on the environment (atmosphere/soil/water) is estimated, but no initial environmental analysis is carried out. |
| 2 | Satisfactory | An initial environmental analysis is carried out to identify the environmental aspects associated with the materials used, the processes taking place in the organization, and the medical services performed at that time. The environmental aspects associated with the activities carried out under normal activity conditions, abnormal operating conditions (maintenance, cleaning, washing, maintenance), as well as in emergency situations (accidents) are identified. |
| 3 | Good | The degree of significance of the impact generated by the identified environmental aspect is evaluated and environmental aspects with significant impact are highlighted. |
| 4 | Very good | The list of environmental aspects identified as having a significant impact is the basis of the process for identifying the objectives and developing the management program. |
| 5 | Excellent | The identified environmental aspects that can generate emergency situations form the basis of emergency plans and the response capacity. |
| Indicator | PB4—Environmental Criteria for Selection of Materials Used in Interventions |
|---|---|
| Description | Selection of materials used during patient-centered medical care interventions according to environmental impact. |
| Evaluation questions | How are the materials to be used in interventions selected? Are specifications consulted if there is any reference to environmental information? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | There are no documents, materials, or resources related to this topic. Training materials, self-study, or environmental information resources are not available (not easy to obtain). They could be obtained from certain resource centers. |
| 2 | Satisfactory | The healthcare facility has identified existing and accessible resources regarding environmental protection (books, press releases, specific learning materials). Awareness-building resources are available. Within the healthcare facility there are structures/responsibilities that identify new resources available in the market. These are available in resource centers. |
| 3 | Good | The materials used in patient-centered medical care interventions take into account environmental protection and eco-friendly behavior. Inhalational anesthesia is recommended and intravenous sevoflurane and propofol are preferred. Documentation resources that are dedicated to the development of environmental awareness are recommended for medical personnel. The organization offers study resources on this topic. |
| 4 | Very good | Criteria or indicators that deal with how environmental protection is taken into account allow and facilitate the review of materials used in medical interventions. Criteria may relate to energy efficiency, green building design, alternative energy sources, low carbon transport, local food, waste reduction, and water conservation. Residual anesthetic gas capture systems are used. Documentation resources for awareness are re-ordered for medical staff and easily accessible to all staff. The organization’s policy regarding the design and production of materials used in interventions is defined and implemented in partnership with institutions working in the field of sustainability. |
| 5 | Excellent | The policy on the supply of materials used in patient-centered healthcare interventions systematically considers environmental protection issues as well as their content and accessibility. During the supply process of materials used in medical care interventions, the healthcare facility checks whether the material is produced in accordance with the environmental protection compliance policy. Materials used in the interventions are supplied in compliance with the criteria regarding environmental protection. The design policy of medical care interventions takes into account the protection of the environment and is implemented together with networks that work in the field of environmental protection at the municipal level, associations, non-profit organizations, and local or national institutions. |
| Indicator | IA41—Usage of Recycled Materials |
|---|---|
| Description | Recycled materials have priority in use. |
| Evaluation questions | Are the activities that produce the largest amount of waste known? What recycled materials are used in healthcare services? Are the used materials recycled? Are there resource reuse practices within the organization? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | There are no concerns or management related to recycled materials. Knowledge about raw materials and recycling possibilities is very limited. |
| 2 | Satisfactory | The quantity of recycled materials (reusable surgical gowns, drapes, laryngeal masks) used in the activities of the healthcare facility is quantified in relation to the volume of training activities for interventions. |
| 3 | Good | Various actions are taken to increase the consumption of recycled materials. The organization’s staff is made aware of the use of recycled materials. |
| 4 | Very good | An action plan aimed at increasing the consumption of recycled materials is established (operating procedures ensure that reusable gowns/surgical drapes/laryngeal/masks/etc. are not discarded prematurely). Some materials are derived from recycling. Recyclable raw materials are used. |
| 5 | Excellent | The consumption of materials continuously decreases as the same volume of materials used in the interventions. Raw materials are derived from recycling. Recyclable materials are preferred when making a selection. |
| Indicator | IA42—Waste Recycling |
|---|---|
| Description | Information about waste recycling within the healthcare facility. |
| Evaluation questions | What measures or methods are adopted to reduce the amount of waste and organize its selection? What can be done for staff and patient awareness? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | The categories of waste generated within the organization are identified: organic, inorganic, toxic. |
| 2 | Satisfactory | The impact of generated waste on the environment is known. The effects of one’s own activities on the environment are known. Waste is collected selectively and transported centrally at the organization level. |
| 3 | Good | The organization’s staff and patients are made aware of how waste is collected, the possibilities of recirculation, and the environmental impact they generate. |
| 4 | Very good | Toxic waste treatment measures are applied. There are agreements with companies specialized in the transport and treatment of waste. There are agreements with specialized companies for the collection, transport, and disposal of hazardous medical waste (laboratory mixtures, obsolete or unknown chemicals). |
| 5 | Excellent | Sustained actions are planned and carried out to reduce the environmental impact through a high degree of waste recycling, within the organization and through collaboration with economic agents authorized to collect and treat waste. |
| Indicator | IB4—Environmentally Friendly Transfer Interventions |
|---|---|
| Description | The existence of transfer interventions, which are more efficient for the environment. |
| Evaluation questions | Does the organization have transfer interventions that are more effective for the environment? For example, the use of electronic documentation accompanying the transfer, is the energy consumption involved evaluated? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | There is no knowledge about the environmental impact of the transfer interventions used. |
| 2 | Satisfactory | The means of transfer, the accompanying documents, and their impact on the environment are identified. Electronic medical records are used. |
| 3 | Good | Promotion of “eco-friendly” transport, reduced number of trips, the means of intervention, and remote communication (video communication, telediagnosis, etc.). Real-time transfer center documentation is accessible in the electronic medical records. |
| 4 | Very good | Contacts are established with other stakeholders in transfer interventions (municipalities, associations, etc.) and a partnership is being developed to promote transport reduction. When designing a transfer intervention, the issue of transport is considered and attempts are made to limit travel. Referring center clinical documentation is available prior to transport. Cross-talk is available and used. |
| 5 | Excellent | The healthcare facility works together with stakeholders to reduce the time and transfer modes (participation in information networks, adaptation of the medical service offered, etc.). |
| Indicator | EA4—Improvement of Environmental Consumption |
|---|---|
| Description | Detected aspects of improving environmental consumption through reusable materials, establishing recycling programs, modern equipment with low energy consumption. |
| Evaluation questions | Is there a list of planned actions aimed at improving environmental consumption? Does applying the programmed actions have the effect of reducing consumption? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | A list of planned actions aimed at improving environmental consumption is drawn up. A report on environmental protection is drawn up, which includes an environmental analysis that is the basis for the selection of significant environmental aspects. |
| 2 | Satisfactory | Based on the planned actions to improve environmental consumption, a program of measures is being developed. The operational control of hazardous substances is ensured in accordance with safety data sheets. |
| 3 | Good | Starting from the analysis of the planned actions to improve the environmental consumption of the healthcare facility, objectives are developed regarding the use of cover linen and reusable surgical linen, paper, and cardboard recycling, energy and water consumption. |
| 4 | Very good | Department managers establish the specific objectives of the areas for which there are managers in accordance with the general objectives. Investments are made in modern appliances and equipment with low energy consumption. The environmental objectives are included in the environmental management program. |
| 5 | Excellent | The purchase of modern high-performance medical equipment and medical equipment ensures a sustained pace of modernization of the hospital. Optimization is achieved by raising the awareness of health personnel and participating in training courses. Sustainable consumption is ensured and the hospital is a “green business.” |
| Indicator | RA4—Mechanisms for Monitoring Energy Consumption and Waste Generation |
|---|---|
| Description | Measurement of energy consumption: natural gas, electricity, fuel. Water consumption measurement. Measuring the amount of waste generated. |
| Evaluation questions | How is energy consumption tracked and (if necessary) what measures to reduce/optimize consumption are applied? How is water consumption tracked? Is a water conservation program implemented? How is the amount of waste generated measured? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | The sources of energy (electricity, gas, fuel, steam) consumed within the organization are identified. |
| 2 | Satisfactory | The amount of energy (electricity, gas, fuel, steam) and water consumed within the organization are quantified and distributed by location/activity. The amount of waste generated is measured. |
| 3 | Good | Actions are implemented to reduce energy consumption, water consumption, and the amount of waste generated. |
| 4 | Very good | Consistent limits are set for energy and water consumption, which are included in an action plan communicated to the healthcare facility staff. Studies and analyses are carried out to optimize energy and water consumption. |
| 5 | Excellent | Certification of premises with “low energy consumption” is practiced. The dominant share of energy consumption is represented by renewable energies. Rainwater is collected in tanks and used for cleaning, watering plants inside the building, and for small-scale energy production. |
| Indicator | RB4—Environmental Measures |
|---|---|
| Description | Environmental factors are quantified and environmental improvement measures are applied. |
| Evaluation questions | By what methods are environmental factors quantified? What environmental measures are taken to reduce the negative impact of the activity performed on the environment? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | - |
| 1 | Low | The objective of the organization is to monitor compliance with environmental protection legislation. In this sense, the protection of water, soil, and atmosphere is pursued. |
| 2 | Satisfactory | Monitoring of environmental factors and waste management is carried out. |
| 3 | Good | The activities intended for environmental protection are supervised according to a plan for inspections and analyses/determinations. |
| 4 | Very good | The plan for inspections and analyses/determinations contains the physical and chemical characteristics of the water samples necessary for analysis of the quality of the wastewater as well as samples (if they are requires). The sampling points are marked. The sampling of water and air is carried out in accordance with the provisions of the enforced standards, with the frequency established in the plan for inspections and analyses/determinations. |
| 5 | Excellent | The results of the environmental analyses are used to determine the performing areas and highlight the activities that require corrective/preventive actions. The monitoring of environmental performance indicators is a continuous process, tracking the amount of emissions, the number of environmental incidents/accidents, the specific amounts of pollutants, investments in environmental protection, and the number of complaints/lawsuits. |
References
- Coiera, E. Putting the technical back into socio-technical systems research. Int. J. Med. Inform. 2007, 76 (Suppl. 1), S98–S103. [Google Scholar] [CrossRef] [PubMed]
- Kjᴂrgård, B.; Land, B.; Pedersen, K.B. Health and sustainability. Health Promot. Int. 2014, 29, 558–568. [Google Scholar] [CrossRef] [PubMed]
- Errington, G.; Evans, C.; Watson, M.C. Searching for sustainability within public health policy: Insights from an injury prevention perspective. Eur. J. Public Health 2017, 27, 334–339. [Google Scholar] [CrossRef][Green Version]
- Pantzartzis, E.; Edum-Fotwe, F.T.; Price, A.D.F. Sustainable healthcare facilities: Reconciling bed capacity and local needs. Int. J. Sustain. Built Environ. 2017, 6, 54–68. [Google Scholar] [CrossRef]
- Maine, T. Towards a Metric of Sustainability. In ISOS Online Conference—In Search of Sustainability; Douglas, B., Furnass, B., Goldie, J., Eds.; ISOS: London, UK, 2003. [Google Scholar]
- Odum, H.T. Environmental Accounting: Emergy and Environmental Decision Making; Wiley: New York, NY, USA, 1996. [Google Scholar]
- Yang, A.; Farmer, P.; McGahan, A. ‘Sustainability’ in global health. Glob. Public Health 2010, 5, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Rapport, D.J. Sustainability science: An ecohealth perspective. Sustain. Sci. 2007, 2, 7784. [Google Scholar] [CrossRef]
- Savoldelli, A.; Landi, D.; Rizzi, C. Sustainability in Healthcare: Methods and Tools for the Assessment. Stud. Health Technol. Inform. 2023, 301, 186–191. [Google Scholar] [PubMed]
- Malone, S.; Prewitt, K.; Hackett, R.; Lin, J.C.; McKay, V.; Walsh-Bailey, C.; Luke, D.A. The Clinical Sustainability Assessment Tool: Measuring organizational capacity to promote sustainability in healthcare. Implement. Sci. Commun. 2021, 2, 77. [Google Scholar] [CrossRef]
- Lennox, L.; Maher, L.; Reed, J. Navigating the sustainability landscape: A systematic review of sustainability approaches in healthcare. Implement. Sci. 2018, 13, 27. [Google Scholar] [CrossRef]
- Shigayeva, A.; Coker, R.J. Communicable disease control programmes and health systems: An analytical approach to sustainability. Health Policy Plan. 2015, 30, 368–385. [Google Scholar] [CrossRef]
- Scheirer, M.A.; Dearing, J.W. An agenda for research on the sustainability of public health programs. Am. J. Public Health 2011, 101, 2059–2067. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Hays, C.; Center, H.; Daley, C. Building capacity and sustainable prevention innovations: A sustainability planning model. Eval. Program Plan. 2004, 27, 135–149. [Google Scholar] [CrossRef]
- Molero, A.; Calabrò, M.; Vignes, M.; Gouget, B.; Gruson, D. Sustainability in Healthcare: Perspectives and Reflections Regarding Laboratory Medicine. Ann. Lab. Med. 2021, 41, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Zdravkovic, D.; Radukic, S. Institutional framework for sustainable development in Serbia. Montenegrin J. Econ. 2012, 8, 27–36. [Google Scholar]
- Isaksson, R. Total quality management for sustainable development: Process based system models. Bus. Process Manag. J. 2006, 12, 632–645. [Google Scholar] [CrossRef]
- ISO 26000:2010; Guidance on Social Responsibility. ISO: Geneva, Switzerland, 2010. Available online: https://www.iso.org/standard/42546.html (accessed on 21 June 2023).
- ISO 9001:2015; Quality Management Systems—Requirements. ISO: Geneva, Switzerland, 2015. Available online: https://www.iso.org/standard/62085.html (accessed on 21 June 2023).
- ANMCS. Manualul Standardelor de Acreditare a Unitatilor Sanitare cu Paturi (Manual of Accreditation Standards for Sanitary Units with Beds). 2020. Available online: https://anmcs.gov.ro/web/wp-content/uploads/2021/02/Manualul-standardelor-deacreditare-2020.pdf (accessed on 3 July 2023).
- ANMCS. Standardele Autoritatii Nationale de Management al Calitatii in Sanatate Pentru Serviciile de Sanatate Acordate in Regim Ambulatoriu (Standards of the National Authority for Quality Management in Health for Outpatient Health Services). Available online: https://anmcs.gov.ro/web/standarde-ambulatoriu/ (accessed on 3 July 2023).
- Groene, O.; Kringos, D.; Sunol, R. On Behalf of the DUQuE Project. Seven Ways to Improve Quality and Safety in Hospitals. An Evidence-Based Guide. DUQuE Collaboration. 2014. Available online: www.duque.eu (accessed on 3 July 2023).
- Moldovan, F.; Moldovan, L.; Bataga, T. Assessment of Labor Practices in Healthcare Using an Innovatory Framework for Sustainability. Medicina 2023, 59, 796. [Google Scholar] [CrossRef]
- McGain, F.; Naylor, C. Environmental sustainability in hospitals—A systematic review and research agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef]
- Ingrassia, P.L.; Mangini, M.; Azzaretto, M.; Ciaramitaro, I.; Costa, L.; Burkle, F.M., Jr.; Della Corte, F.; Djalali, A. Hospital Disaster Preparedness in Italy: A preliminary study utilizing the World Health Organization Hospital Emergency Response Evaluation Toolkit. Minerva Anestesiol. 2016, 82, 1259–1266. [Google Scholar]
- Wurmb, T.; Scholtes, K.; Kolibay, F.; Rechenbach, P.; Vogel, U.; Kowalzik, B. Alarm- und Einsatzplanung im Krankenhaus: Vorbereitung auf Großschadenslagen [The Hospital Emergency Plan: Important Tool for Disaster Preparedness]. Anasthesiol. Intensiv. Notf. Schmerzther. 2017, 52, 594–605. [Google Scholar]
- MoradiMajd, P.; Seyedin, H.; Bagheri, H.; Tavakoli, N. Hospital Preparedness Plans for Chemical Incidents and Threats: A Systematic Review. Disaster Med. Public Health Prep. 2020, 14, 477–485. [Google Scholar] [CrossRef]
- Rebmann, T.; Gupta, N.K.; Charney, R.L. US Hospital Preparedness to Manage Unidentified Individuals and Reunite Unaccompanied Minors with Family Members During Disasters: Results from a Nationwide Survey. Health Secur. 2021, 19, 183–194. [Google Scholar] [CrossRef]
- Zhang, X.; Zhu, Y.; Li, B.; Tefsen, B.; Wang, Z.; Wells, M. We need to plan streamlined environmental impact assessment for the future X-Press Pearl disasters. Mar. Pollut. Bull. 2023, 188, 114705. [Google Scholar] [CrossRef]
- Jarousse, L.A. Environmental sustainability programs for hospitals. Hosp. Health Netw. 2012, 86, 33–40. [Google Scholar] [PubMed]
- Munasinghe, N.L.; O’Reilly, G.; Cameron, P. Establishing the Domains of a Hospital Disaster Preparedness Evaluation Tool: A Systematic Review. Prehospital Disaster Med. 2022, 37, 674–686. [Google Scholar] [CrossRef]
- Dowlati, M.; Seyedin, H.; Moslehi, S. Hospital Preparedness Measures for Biological Hazards: A Systematic Review and Meta-Synthesis. Disaster Med. Public Health Prep. 2021, 15, 790–803. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.K.; Nasrullah, S.M.; Quattrocchi, A.; Arcos González, P.; Castro Delgado, R. Hospital Surge Capacity Preparedness in Disasters and Emergencies: Protocol for a Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13437. [Google Scholar] [CrossRef] [PubMed]
- Sheikhbardsiri, H.; Raeisi, A.R.; Nekoei-Moghadam, M.; Rezaei, F. Surge Capacity of Hospitals in Emergencies and Disasters with a Preparedness Approach: A Systematic Review. Disaster Med. Public Health Prep. 2017, 11, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Wormer, B.A.; Augenstein, V.A.; Carpenter, C.L.; Burton, P.V.; Yokeley, W.T.; Prabhu, A.S.; Harris, B.; Norton, S.; Klima, D.A.; Lincourt, A.E.; et al. The green operating room: Simple changes to reduce cost and our carbon footprint. Am. Surg. 2013, 79, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.; Ma, S.; Ur Rehman, A.; Usmani, Y.S. Green Operation Strategies in Healthcare for Enhanced Quality of Life. Healthcare 2022, 11, 37. [Google Scholar] [CrossRef] [PubMed]
- Pradere, B.; Mallet, R.; de La Taille, A.; Bladou, F.; Prunet, D.; Beurrier, S.; Bardet, F.; Game, X.; Fournier, G.; Lechevallier, E.; et al. Sustainability Task Force of the French Association of Urology. Climate-smart Actions in the Operating Theatre for Improving Sustainability Practices: A Systematic Review. Eur. Urol. 2023, 83, 331–342. [Google Scholar] [CrossRef]
- Guetter, C.R.; Williams, B.J.; Slama, E.; Arrington, A.; Henry, M.C.; Möller, M.G.; Tuttle-Newhall, J.E.; Stein, S.; Crandall, M. Greening the operating room. Am. J. Surg. 2018, 216, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Rübsam, M.L.; Kruse, P.; Dietzler, Y.; Kropf, M.; Bette, B.; Zarbock, A.; Kim, S.C.; Hönemann, C. A call for immediate climate action in anesthesiology: Routine use of minimal or metabolic fresh gas flow reduces our ecological footprint. Can. J. Anaesth. 2023, 70, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Lindén-Søndersø, A.; Nielsen, N.; Bentzer, P. Klimateffekterna från anestesin kan minska [Climate footprint of halogenated inhalation anesthetics]. Lakartidningen 2019, 116, FR9L. [Google Scholar]
- Ryan, S.M.; Nielsen, C.J. Global warming potential of inhaled anesthetics: Application to clinical use. Anesth. Analg. 2010, 111, 92–98. [Google Scholar] [CrossRef]
- Sherman, J.; Le, C.; Lamers, V.; Eckelman, M. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth. Analg. 2012, 114, 1086–1090. [Google Scholar] [CrossRef]
- DiGiacomo, J.C.; Odom, J.W.; Ritota, P.C.; Swan, K.G. Cost containment in the operating room: Use of reusable versus disposable clothing. Am. Surg. 1992, 58, 654–656. [Google Scholar]
- Conrardy, J.; Hillanbrand, M.; Myers, S.; Nussbaum, G.F. Reducing medical waste. AORN J. 2010, 91, 711–721. [Google Scholar] [CrossRef]
- Overcash, M. A comparison of reusable and disposable perioperative textiles: Sustainability state-of-the-art 2012. Anesth. Analg. 2012, 114, 1055–1066. [Google Scholar] [CrossRef]
- Eckelman, M.; Mosher, M.; Gonzalez, A.; Sherman, J. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth. Analg. 2012, 114, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- Penn, E.; Yasso, S.F.; Wei, J.L. Reducing disposable equipment waste for tonsillectomy and adenotonsillectomy cases. Otolaryngol. Head Neck Surg. 2012, 147, 615–618. [Google Scholar] [CrossRef] [PubMed]
- Meiklejohn, D.A.; Chavarri, V.M. Cold Technique in Adult Tonsillectomy Reduces Waste and Cost. Ear Nose Throat J. 2021, 100 (Suppl. 5), 427S–430S. [Google Scholar] [CrossRef]
- Van Demark, R.E., Jr.; Smith, V.J.S.; Fiegen, A. Lean and Green Hand Surgery. J. Hand Surg. Am. 2018, 43, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Cerceo, E. Sustainability Initiatives in the Operating Room. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 663–672. [Google Scholar] [CrossRef] [PubMed]
- McGain, F.; White, S.; Mossenson, S.; Kayak, E.; Story, D. A survey of anesthesiologists’ views of operating room recycling. Anesth. Analg. 2012, 114, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.J.; Mears, S.C. Greening of orthopedic surgery. Orthopedics 2012, 35, e940–e944. [Google Scholar] [CrossRef]
- Kanclerski, K.; Głuszyński, P. Zasady bezpiecznego postepowania z odpadami w zakładach świadczacych usługi medyczne ze szczególnym uwzglednieniem odpadów zakaźnych [Safe management of waste generated in health care institutions especially with infectious waste]. Przegl. Epidemiol. 2008, 62, 801–809. [Google Scholar] [PubMed]
- Shum, P.L.; Kok, H.K.; Maingard, J.; Zhou, K.; Van Damme, V.; Barras, C.D.; Slater, L.A.; Chong, W.; Chandra, R.; Jhamb, A.; et al. Sustainability in interventional radiology: Are we doing enough to save the environment? CVIR Endovasc. 2022, 5, 60. [Google Scholar] [CrossRef] [PubMed]
- Tearle, P. Clinical waste management. Commun. Dis. Public Health 2001, 4, 234–236. [Google Scholar] [PubMed]
- Griffith, R.; Tengnah, C. Legal regulation of clinical waste in the community. Br. J. Community Nurs. 2006, 11, 33–37. [Google Scholar] [CrossRef]
- Wyssusek, K.H.; Keys, M.T.; van Zundert, A.A.J. Operating room greening initiatives—The old, the new, and the way forward: A narrative review. Waste Manag. Res. 2019, 37, 3–19. [Google Scholar] [CrossRef]
- Brewer, J. A disposable choice for hospital waste. Hosp. Mater. Manag. Q. 1993, 14, 12–25. [Google Scholar]
- Samutin, N.M.; Butorina, N.N.; Starodubova, N.Y.; Korneychuk, S.S.; Ustinov, A.K. Priority Technologies of the Medical Waste Disposal System. Gig Sanit 2015, 94, 35–37. [Google Scholar]
- Burd, M. Reducing the risks related to the handling and disposal of health-care waste. Prof. Nurse 2005, 20, 40–42. [Google Scholar]
- Blenkharn, J.I.; Odd, C. Sharps injuries in healthcare waste handlers. Ann. Occup. Hyg. 2008, 52, 281–286. [Google Scholar]
- Iwashyna, T.J. The incomplete infrastructure for interhospital patient transfer. Crit. Care Med. 2012, 40, 2470–2478. [Google Scholar] [CrossRef]
- Abraham, J.; Reddy, M.C. Challenges to inter-departmental coordination of patient transfers: A workflow perspective. Int. J. Med. Inform. 2010, 79, 112–122. [Google Scholar] [CrossRef]
- Haque, W.; Derksen, B.A.; Calado, D.; Foster, L. Using business intelligence for efficient inter-facility patient transfer. Stud. Health Technol. Inform. 2015, 208, 170–176. [Google Scholar]
- Hirschman, K.B.; Shaid, E.; McCauley, K.; Pauly, M.V.; Naylor, M.D. Continuity of Care: The Transitional Care Model. Online J. Issues Nurs. 2015, 20, 1. [Google Scholar] [CrossRef]
- Dunnion, M.E.; Kelly, B. From the emergency department to home. J. Clin. Nurs. 2005, 14, 776–785. [Google Scholar] [CrossRef]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. The Impact of the COVID-19 Pandemic on the Orthopedic Residents: A Pan-Romanian Survey. Int. J. Environ. Res. Public Health 2022, 19, 9176. [Google Scholar] [CrossRef]
- Sun, H.; Zhu, X.; Xu, X.; Shen, G.; Suo, Y.; Cao, L.; Yu, H.; Xu, J. Design and application of a new patient transfer device. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2019, 31, 1158–1159. [Google Scholar]
- Mikolaj, T.; Moldovan, L.; Chalupczak, A.; Moldovan, F. Computer aided learning process. Procedia Eng. 2017, 181, 1028–1035. [Google Scholar] [CrossRef]
- Mikolaj, T.; Moldovan, F.; Ciobanu, I.; Chalupczak, A.; Marin, A.G. Brain research Using Computer Test. Procedia Technol. 2016, 22, 1113–1120. [Google Scholar] [CrossRef]
- Herrigel, D.J.; Carroll, M.; Fanning, C.; Steinberg, M.B.; Parikh, A.; Usher, M. Interhospital transfer handoff practices among US tertiary care centers: A descriptive survey. J. Hosp. Med. 2016, 11, 413–417. [Google Scholar] [CrossRef]
- Usher, M.G.; Fanning, C.; Wu, D.; Muglia, C.; Balonze, K.; Kim, D.; Parikh, A.; Herrigel, D. Information handoff and outcomes of critically ill patients transferred between hospitals. J. Crit. Care 2016, 36, 240–245. [Google Scholar] [CrossRef]
- Hindmarsh, D.; Lees, L. Improving the safety of patient transfer from AMU using a written checklist. Acute Med. 2012, 11, 13–17. [Google Scholar] [CrossRef]
- Whitaker, M.W. Health care: A leader or a follower? Reducing disposable waste. Hosp. Mater. Manag. Q. 1992, 14, 1–10. [Google Scholar]
- Kirkland, L.L.; Parham, W.M.; Pastores, S.M. Approaching hospital administration about adopting cooling technologies. Crit. Care Med. 2009, 37 (Suppl. 7), S290–S294. [Google Scholar] [CrossRef]
- Koch, S.; Pecher, S. Neue Herausforderungen für die Anästhesie durch den Klimawandel [New challenges for anesthesia due to the climate change]. Anaesthesist 2020, 69, 453–462. [Google Scholar] [CrossRef]
- Sattler, B.; Hall, K. Healthy choices: Transforming our hospitals into environmentally healthy and safe places. Online J. Issues Nurs. 2007, 12, 3. [Google Scholar] [CrossRef]
- Shoham, M.A.; Baker, N.M.; Peterson, M.E.; Fox, P. The environmental impact of surgery: A systematic review. Surgery 2022, 172, 897–905. [Google Scholar] [CrossRef]
- Sullivan, G.A.; Petit, H.J.; Reiter, A.J.; Westrick, J.C.; Hu, A.; Dunn, J.B.; Gulack, B.C.; Shah, A.N.; Dsida, R.; Raval, M.V. Environmental Impact and Cost Savings of Operating Room Quality Improvement Initiatives: A Scoping Review. J. Am. Coll. Surg. 2023, 236, 411–423. [Google Scholar] [CrossRef]
- Bravo, D.; Gaston, R.G.; Melamed, E. Environmentally Responsible Hand Surgery: Past, Present, and Future. J. Hand Surg. Am. 2020, 45, 444–448. [Google Scholar] [CrossRef]
- Thornton, J.; McCally, M.; Orris, P.; Weinberg, J. Hospitals and plastics. Dioxin prevention and medical waste incinerators. Public Health Rep. 1996, 111, 298–313. [Google Scholar]
- Álvaro-Meca, A.; Sánchez-López, A.; Resino, R.; Tamayo, E.; Resino, S. Environmental factors are associated with hospital admissions for sepsis-related pneumonia: A bidirectional case-crossover design. Environ. Res. 2020, 191, 110102. [Google Scholar] [CrossRef]
- Phoon, K.M.; Afzal, I.; Sochart, D.H.; Asopa, V.; Gikas, P.; Kader, D. Environmental sustainability in orthopaedic surgery: A scoping review. Bone Jt. Open 2022, 3, 628–640. [Google Scholar] [CrossRef] [PubMed]
- Beloeil, H.; Albaladejo, P. Initiatives to broaden safety concerns in anaesthetic practice: The green operating room. Best Pract. Res. Clin. Anaesthesiol. 2021, 35, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Rohde, T.; Martinez, R. Equipment and Energy Usage in a Large Teaching Hospital in Norway. J. Healthc. Eng. 2015, 6, 419–433. [Google Scholar] [CrossRef] [PubMed]
- Serb, C. Think green. Hosp. Health Netw. 2008, 82, 22–26. [Google Scholar]
- Bush, H. The path to going green. Hosp. Health Netw. 2008, 82, 27–33. [Google Scholar]
- Candan Dönmez, Y.; Aslan, A.; Yavuz VAN Giersbergen, M. Environment-Friendly Practices in Operating Rooms in Turkey. J. Nurs Res. 2019, 27, e18. [Google Scholar] [CrossRef] [PubMed]
- Langstaff, K.; Brzozowski, V. Managing environmental sustainability in a healthcare setting. Healthc. Manag. Forum. 2017, 30, 84–88. [Google Scholar] [CrossRef]
- Sundell-Bergman, S.; de la Cruz, I.; Avila, R.; Hasselblad, S. A new approach to assessment and management of the impact from medical liquid radioactive waste. J. Environ. Radioact. 2008, 99, 1572–1577. [Google Scholar] [CrossRef] [PubMed]
- McGain, F.; Moore, G.; Black, J. Steam sterilisation’s energy and water footprint. Aust. Health Rev. 2017, 41, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Álvaro-Meca, A.; Sepúlveda-Crespo, D.; Resino, R.; Ryan, P.; Martínez, I.; Resino, S. Neighborhood environmental factors linked to hospitalizations of older people for viral lower respiratory tract infections in Spain: A case-crossover study. Environ. Health 2022, 21, 107. [Google Scholar] [CrossRef] [PubMed]
- Le, T.G.; Ngo, L.; Mehta, S.; Do, V.D.; Thach, T.Q.; Vu, X.D.; Nguyen, D.T.; Cohen, A. Effects of short-term exposure to air pollution on hospital admissions of young children for acute lower respiratory infections in Ho Chi Minh City, Vietnam. Res. Rep. Health Eff. Inst. 2012, 169, 5–83. [Google Scholar]
- Álvaro-Meca, A.; Goez, M.D.C.; Resino, R.; Matías, V.; Sepúlveda-Crespo, D.; Martínez, I.; Resino, S. Environmental factors linked to hospital admissions in young children due to acute viral lower respiratory infections: A bidirectional case-crossover study. Environ. Res. 2022, 212 Pt B, 113319. [Google Scholar] [CrossRef]
- Zanoni, P. Going green by reducing red. New alternative medical waste treatment technologies. Mich. Health Hosp. 1998, 34, 38–39. [Google Scholar]
- Alvim Ferraz, M.C.; Afonso, S.A. Dioxin emission factors for the incineration of different medical waste types. Arch. Environ. Contam. Toxicol. 2003, 44, 460–466. [Google Scholar] [CrossRef]
- Alvim-Ferraz, M.C.; Afonso, S.A. Incineration of healthcare wastes: Management of atmospheric emissions through waste segregation. Waste Manag. 2005, 25, 638–648. [Google Scholar] [CrossRef]
- Gautam, V.; Thapar, R.; Sharma, M. Biomedical waste management: Incineration vs. environmental safety. Indian J. Med. Microbiol. 2010, 28, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Piersanti, E.G.; Sgattone, L.; Di Stefano, L.; Migliorati, G. Environmental impact assessment of waste-water: Radionuclides use in hospitals (Abruzzo, Italy, 2000–2015). Vet. Ital. 2018, 54, 333–336. [Google Scholar] [PubMed]
- Bozoudis, V.; Sebos, I.; Tsakanikas, A. Action plan for the mitigation of greenhouse gas emissions in the hospital-based health care of the Hellenic Army. Environ. Monit. Assess. 2022, 194, 221. [Google Scholar] [CrossRef] [PubMed]
- Fernando, J.; Dawson, L. The Natural Hospital Environment: A Socio-Technical-Material perspective. Int. J. Med. Inform. 2014, 83, 140–158. [Google Scholar] [CrossRef]
- Kleber, J. Environmental Stewardship: The Nurse’s Role in Sustainability. Clin. J. Oncol. Nurs. 2018, 22, 354–356. [Google Scholar] [CrossRef]
- County Emergency Clinical Hospital of Targu Mures. Available online: https://www.spitalmures.ro/en/ (accessed on 3 July 2023).
- Moldovan, F.; Blaga, P.; Moldovan, L.; Bataga, T. An Innovative Framework for Sustainable Development in Healthcare: The Human Rights Assessment. Int. J. Environ. Res. Public Health 2022, 19, 2222. [Google Scholar] [CrossRef]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. An Investigation for Future Practice of Elective Hip and Knee Arthroplasties during COVID-19 in Romania. Medicina 2023, 59, 314. [Google Scholar] [CrossRef]
- Moldovan, L. Sustainability assessment framework for VET organizations. Sustainability 2015, 7, 7156–7174. [Google Scholar] [CrossRef]
- Moldovan, L. Framework indicators for European quality assurance in VET towards environmentally sustainable economy. Procedia Manuf. 2018, 22, 990–997. [Google Scholar] [CrossRef]
- Moldovan, L. Framework Development for European Quality Assurance in VET Towards Environmentally Sustainable Economy. Procedia Eng. 2017, 181, 1064–1071. [Google Scholar] [CrossRef]




| Value [S] | Importance Category | Description |
|---|---|---|
| 0 | Not relevant | X |
| 1 | Unimportant | The subject is of little importance to the healthcare facility and there is a marginal tendency for evaluation. |
| 2 | Reduced importance | Failure to comply with this requirement could adversely affect the activity of the healthcare facility. |
| 3 | Important | Failure to comply with the requirement could compromise the activity of the healthcare facility. It is essential to meet the requirements of the healthcare facility. |
| 4 | Very important | Failure to meet this requirement could jeopardize the successful provision of healthcare. Fulfilling the requirement is essential for the successful delivery of healthcare. |
| 5 | High importance | Failure to comply with the requirement may even compromise the existence of the healthcare facility. |
| Social Responsibility Quality Cycle | 1—Organizational Governance | 2—Human Rights | 3—Labor Practices | 4—Environment | 5—Fair Healthcare Practices | 6—Patient Issues | 7—Community Involvement and Development | |
|---|---|---|---|---|---|---|---|---|
| (P) Healthcare service design | PA—Healthcare service accreditation | PA1—Decision structures and processes | PA21—Healthcare service accessibility PA22—Medical care services for disadvantaged groups | PA3—Promotion of change and professional development | PA4—Environmental impact plan | PA5—Attitudes of profession towards accreditation | PA6—Performance information | PA7—Community involvement activities |
| PB—Patient-centered care intervention design | PB1—Quality assurance process design | PB2—Interventions with positive effects on patient satisfaction | PB3—Quality assurance of patient-centered medical interventions | PB4—Environ-mental criteria for selection of materials used in interventions | PB5—Effective intervention implementation | PB6—Patient self-care design and self-management | PB7—Content of the interventions adapted to the community | |
| (I) Healthcare service provision | IA—Healthcare service provision | IA1—Computerized support systems for clinical decisions | IA2—Specific medical approaches | I.A31—Continuous healthcare education IA32—Practice guideline implementation and dissemination | IA41—Usage of recycled materials IA42—Waste recycling | IA5—Promotion of patient safety culture | IA6—Critical features for improving the surveillance of patients with chronic conditions | IA71—Networking and partnership IA72—Involvement of volunteers and training networks |
| IB—Transfer assurance | IB1—Transfer evaluation mechanisms | IB2—Fair transfer interventions | IB3—Interventions for transfer improvement | IB4—Environmen-tally friendly transfer interventions | IB5—Features that affect transfer effectiveness | IB6—Interventions to reduce problems with outpatients | IB7—Involvement and participation of professional associations | |
| (E) Healthcare service evaluation | EA—Evaluation and involvement of local opinion leaders | EA1—Existence and recognition of local opinion leaders | EA2—Evaluation of current medical practices | EA3—Professional practices improvement | EA4—Improvement of environmental consumption | EA5—Effective work practices | EA6—Patient-specific issue management | EA7—Local opinion leaders involved in the community |
| EB—Satisfaction assessment | EB1—Monitoring mechanism assignment | EB2—Patient satisfaction degree | EB3—Medical staff satisfaction | Not relevant | Not relevant | EB6—Patient satisfaction degree regarding therapeutic benefits | EB7—Satisfaction regarding partnerships | |
| (R) Continuous improvement | RA—Self-assessment | RA1—Self-assessment tools | RA2—Freedom of expression assurance | RA3—Audit and feedback | RA4—Mechanisms for monitoring energy consumption and waste generation | RA5—Feedback to medical staff | RA6—Complaint management | RA7—Communitarian initiatives |
| RB—Healthcare service innovation | RB1—Changes to healthcare services | Not relevant | RB3—Medical organization supported by Six Sigma and Lean | RB4—Environmental measures | RB5—Safety checklists | RB6—Incident report | RB7—Educational visits | |
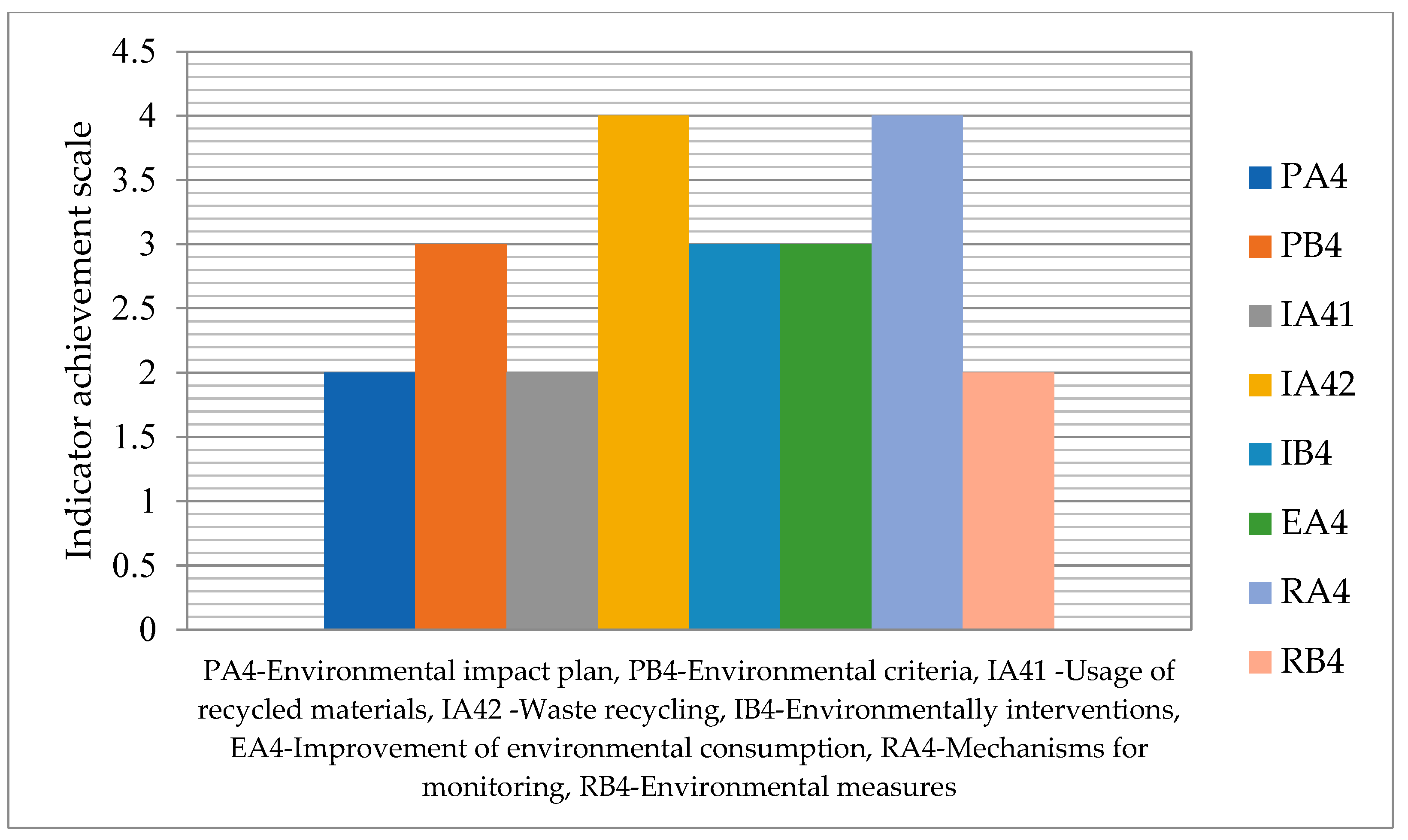
| No. | Indicator Descriptive | Importance [Ii] | Achievement [Ai] | Sustainability Indicator [Si = Ii × Ai] |
|---|---|---|---|---|
| 1 | PA4—Environmental impact plan | 5 | 2 | 10 |
| 2 | PB4—Environmental criteria for selection of materials used in interventions | 3 | 3 | 9 |
| 3 | IA41—Usage of recycled materials | 4 | 2 | 8 |
| 4 | IA42—Waste recycling | 4 | 4 | 16 |
| 5 | IB4—Environmentally friendly transfer interventions | 3 | 3 | 9 |
| 6 | EA4—Improvement of environmental consumption | 4 | 3 | 12 |
| 7 | RA4—Mechanisms for monitoring energy consumption and waste generation | 3 | 4 | 12 |
| 8 | RB4—Environmental measures | 2 | 2 | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moldovan, F.; Moldovan, L.; Bataga, T. The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework. Sustainability 2023, 15, 13402. https://doi.org/10.3390/su151813402
Moldovan F, Moldovan L, Bataga T. The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework. Sustainability. 2023; 15(18):13402. https://doi.org/10.3390/su151813402
Chicago/Turabian StyleMoldovan, Flaviu, Liviu Moldovan, and Tiberiu Bataga. 2023. "The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework" Sustainability 15, no. 18: 13402. https://doi.org/10.3390/su151813402
APA StyleMoldovan, F., Moldovan, L., & Bataga, T. (2023). The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework. Sustainability, 15(18), 13402. https://doi.org/10.3390/su151813402









