Validation of Instruments for the Improvement of Interprofessional Education through Educational Management: An Internet of Things (IoT)-Based Machine Learning Approach
Abstract
:1. Introduction
1.1. Literature Review
1.1.1. IPE and IPECP Definitions and Drivers
1.1.2. Background
1.1.3. Framework of Interprofessional Education
1.1.4. IPC (Interprofessional Practice)
1.1.5. Importance of IPECP and Its Future
1.1.6. IPECP Development and Core Competencies
1.1.7. Barriers to Implementation of IPE
1.1.8. The Influence of Management and Leadership on Interprofessional Education
1.1.9. Psychological Implications of IPE
1.1.10. Pedagogical Implications of IPE
1.1.11. Sustainability and IPE
- Government funding (government and professional);
- HEI funding;
- Faculty development programs;
- HEI organizational structures to support the integration of IPE into health professional curricula;
- Staff ownership and commitment across all disciplines involved in IPE programs [15].
1.1.12. Artificial Intelligence (AI) and the Internet of Things (IoT)
1.2. Objective and Purpose of the Research
1.2.1. Importance of This Research
1.2.2. Problem Statement
1.2.3. Research Objectives
- Bring the delivery of healthcare and education closer together;
- Develop a conceptual framework for calculating the impact of IPE;
- Strengthen the empirical base for IPE;
- Examine satisfaction levels with the components of the model related to leadership and improvement in interprofessional education and relate IPE to changes in collaborative behaviour.
1.2.4. Hypothesis
- Is there a gap between the educational management models of the health professions and interprofessional education?
- Does the execution of interprofessional education improve the knowledge of health professional learners and practitioners of their field of concern?
- Can health profession educational management theories and models improve interprofessional education and leadership?
2. Materials and Methods
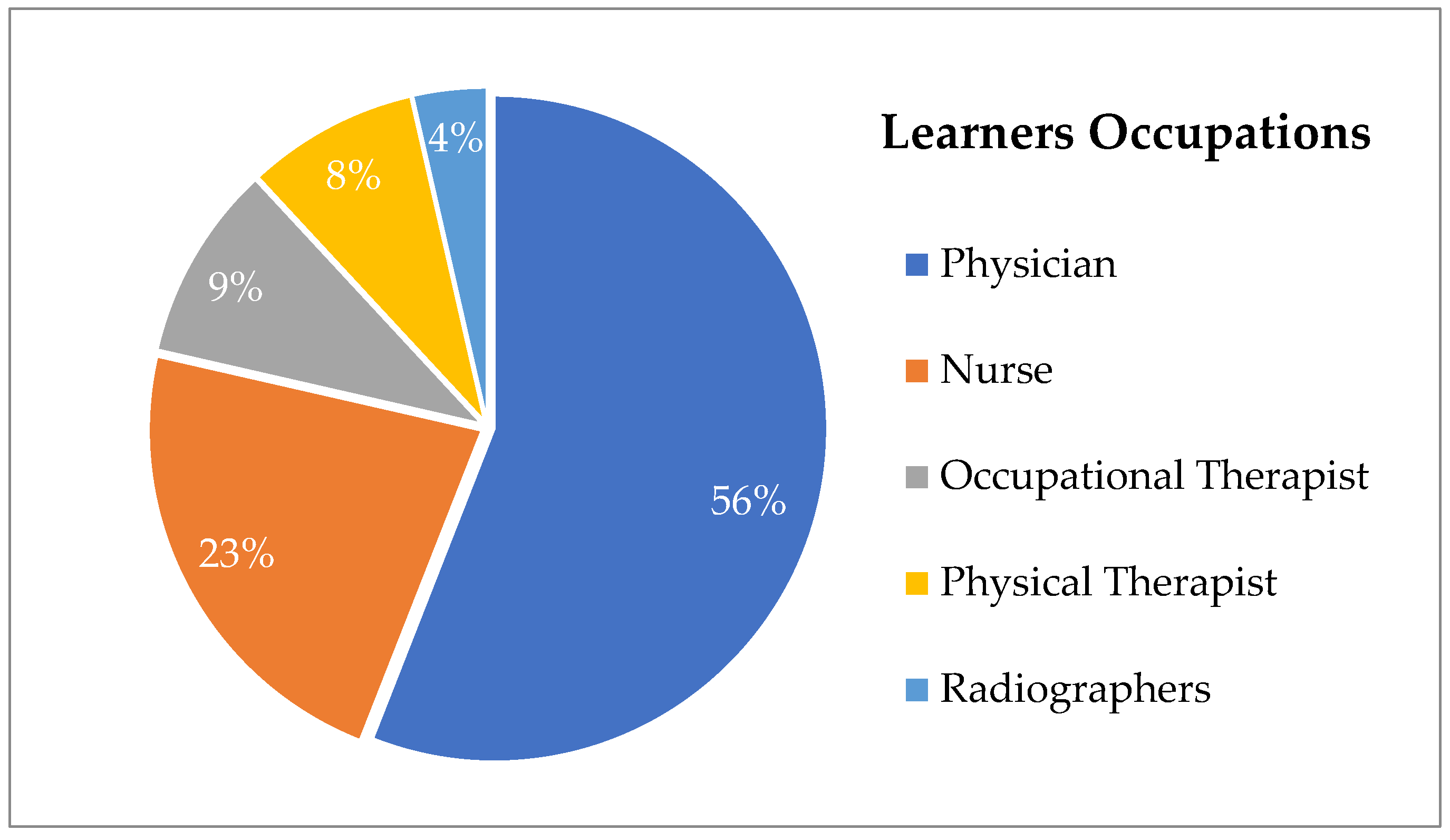
2.1. The Sample
2.2. Design and Model for the Research
2.3. Data Gathering and Analysis
2.3.1. Quantitative Approach
2.3.2. Qualitative Approach
2.3.3. Machine Learning-Based Approaches
RT Machine Learning-Based Approaches
SVM Machine Learning-Based Approaches
GPR Machine Learning-Based Approaches
Classical Linear Regression Model Machine Learning-Based Approaches
3. Results
3.1. Quantitative Approach
3.1.1. Interprofessional Collaborative Competencies Attainment Survey (ICCAS)
3.1.2. ICCAS and Paired-Samples T-Test
- Communication:
- 1.
- Promote effective communication among members of an interprofessional (IP) team.
- 2.
- Actively listen to IP team members’ ideas and concerns.
- 3.
- Express my ideas and concerns without being judgmental.
- 4.
- Provide constructive feedback to IP team members.
- 5.
- Express my ideas and concerns in a clear, concise manner.
- Collaboration:
- 6.
- Seek out IP team members to address issues.
- 7.
- Work effectively with IP team members to enhance care.
- 8.
- Learn with, from and about IP team members to enhance care.
- Roles and Responsibilities:
- 9.
- Identify and describe my abilities and contributions to the IP team.
- 10.
- Be accountable for my contributions to the IP team.
- 11.
- Understand the abilities and contributions of IP team members.
- 12.
- Recognize how others’ skills and knowledge complement and overlap with my own.
- Collaborative Patient/Family-Centred Approach:
- 13.
- Use an IP team approach with the patient to assess the health situation.
- 14.
- Use an IP team approach with the patient to provide whole person care.
- 15.
- Include the patient/family in decision-making.
- Conflict Management/Resolution:
- 16.
- Actively listen to the perspectives of IP team members.
- 17.
- Take into account the ideas of IP team members.
- 18.
- Address team conflict in a respectful manner.
- Team Functioning:
- 19.
- Develop an effective care plan with IP team members.
- 20.
- Negotiate responsibilities within overlapping scopes of practice [58].
3.1.3. RIPLS and Paired T-Test
3.2. Qualitative Approach
3.2.1. Open-Discussion Interviews
3.2.2. Chi-Square Test
- The existence of explicit shared goals facilitates collaboration and coordination between primary and specialized care. Please rate the current situation in your organization.
- Explicitly giving priority to the interests and preferences of patients in the interaction between levels of care favours collaboration and coordination between professionals working in the different levels. Please rate the current situation in your organization.
- Knowledge between professionals of each other’s values, specific competences and focus with respect to care, as well as of the environment in which each other work, has an impact on the development of team spirit and collaborative work. Knowing colleagues personally is also helpful. Please rate the current situation in your organization.
- Mutual trust makes interprofessional collaboration possible, reduces uncertainty and contributes to the formation of networks of multidisciplinary professionals focused on the needs of patients. Please rate the current situation in your organization.
- The existence of guidelines, issued by the corresponding Health Authority, that promote collaborative work between professionals from different levels of care, influences on the coordination and collaboration between professionals of both care levels. Please rate the current situation in your organization.
- Shared leadership between managers and clinicians at a local level allows for the development of collaboration between professionals and organizations. Please rate the current situation in your organization.
- Collaboration requires changes in clinical practice and in the distribution of responsibilities for both primary and specialized care professionals. Such changes require innovation that may or may not be supported by your organization. Please rate the current situation in your organization.
- For professionals of primary and specialized care to collaborate, they need forums, channels of communication and activities that enable them to come into contact with one another, discuss shared issues and establish links and agreements. Please rate the current situation in your organization.
- The preparation and establishment of protocols clarifies and makes it possible to negotiate how to share the responsibilities of each professional. Indeed, there are many mechanisms to formalize agreements and understandings between professionals in the two levels: care pathways, information systems, agreements between organizations or units, etc., as well as protocols. Please rate the current use of such mechanisms in your organization.
- The effective exchange of high-quality information between professionals is an element that facilitates collaboration and makes it possible to provide better care to patients. Please rate the current situation in your organization.
3.2.3. Cronbach’s Alpha
3.3. Machine Learning-Based Approaches
4. Discussion
Findings
5. Conclusions
6. Recommendations and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barr, H. Responding as Interprofessional Educators to the WHO Challenge. J. Taibah Univ. Med. Sci. 2016, 11, 505–509. [Google Scholar] [CrossRef]
- Ahn, D. Current trend of accreditation within medical education. Korean Med. Educ. Rev. 2020, 22, 9–15. [Google Scholar] [CrossRef]
- Bourgeault, I.L.; Grignon, M. A Comparison of the Regulation of Health Professional Boundaries across OECD Countries. Eur. J. Comp. Econ. 2013, 10, 199–223. [Google Scholar]
- Samuriwo, R. Interprofessional Collaboration—Time for a New. Theory of. Action? Front. Med. 2022, 9, 876715. [Google Scholar] [CrossRef] [PubMed]
- Eklund, W.; Kenner, C. Interprofessional Education and Practice: The Call for an Interprofessional Approach to Improve the Quality of Neonatal Care. Newborn Infant. Nurs. Rev. 2013, 13, 110–112. [Google Scholar] [CrossRef]
- Green, B.N.; Johnson, C.D. Interprofessional collaboration in research, education, and clinical practice: Working together for a better future. J. Chiropr. Educ. 2015, 29, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Thistlethwaite, J.E.; Forman, D.; Matthews, L.R.; Rogers, G.D.; Steketee, C.; Yassine, T. Competencies and frameworks in interprofessional education: A comparative analysis. Acad. Med. 2014, 89, 869–875. [Google Scholar] [CrossRef]
- Folkman, A.K.; Tveit, B.; Sverdrup, S. Leadership in Interprofessional Collaboration in Health Care. J. Multidiscip. Healthc. 2019, 12, 97–107. [Google Scholar] [CrossRef]
- van Diggele, C.; Roberts, C.; Burgess, A.; Mellis, C. Interprofessional education: Tips for design and implementation. BMC Med. Educ. 2020, 20 (Suppl. 2), 455. [Google Scholar] [CrossRef]
- Varpio, L.; Teunissen, P. Leadership in interprofessional healthcare teams: Empowering knotworking with followership. Med. Teach. 2021, 43, 32–37. [Google Scholar] [CrossRef]
- De’Bell, K.; Clark, R. Mindful Leadership in Interprofessional Teams. Int. J. Whole Pers. Care 2018, 5, 5–16. [Google Scholar] [CrossRef]
- Slater, C.E.; Keefe, B.; Jacobs, K. Impact of the Interprofessional Leadership in Healthcare Certificate on health professionals’ collaboration and leadership abilities. J. Interprof. Educ. Pract. 2023, 32, 100658. [Google Scholar] [CrossRef]
- Chou, E.; Grawey, T.; Paige, J.B. Psychological Safety as an Educational Value in Interprofessional Health Education. AMA J. Ethics 2023, 25, 338–343. [Google Scholar]
- Li, J.T.S.; Chau, J.P.C.; Wong, S.Y.S.; Lau, A.; Chan, W.S.; Yip, P.P.S.; Yang, Y.; Ku, F.K.T.; Sze, F.; King, I.K.C.; et al. Interprofessional Education—Situations of a University in Hong Kong and Major Hurdles to Teachers and Students. Front. Educ. 2022, 7, 653738. [Google Scholar] [CrossRef]
- Lawlis, T.R.; Anson, J.; Greenfield, D. Barriers and Enablers That Influence Sustainable Interprofessional Education: A Literature Review. J. Interprof. Care 2014, 28, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Greco, C.; Fortino, G.; Crispo, B.; Choo, K.-K.R. AI-Enabled IoT Penetration Testing: State-of-the-Art and Research Challenges. Enterp. Inf. Syst. 2022, 17, 2130014. [Google Scholar] [CrossRef]
- Mozumder, M.A.I.; Armand, T.P.T.; Uddin, S.M.I.; Athar, A.; Sumon, R.I.; Hussain, A.; Kim, H.C. Metaverse for Digital Anti-Aging Healthcare: An Overview of Potential Use Cases Based on Artificial Intelligence, Blockchain, IoT Technologies, Its Challenges, and Future Directions. Appl. Sci. 2023, 13, 5127. [Google Scholar] [CrossRef]
- Usman, A.G.; Ahmad, M.H.; Danraka, R.N.; Abba, S.I. The Effect of Ethanolic Leaves Extract of Hymenodictyon Floribundun on Inflammatory Biomarkers: A Data-Driven Approach. Bull. Natl. Res. Cent. 2021, 45, 128. [Google Scholar] [CrossRef]
- Rodriguez-Conde, I.; Campos, C.; Fdez-Riverola, F. Horizontally Distributed Inference of Deep Neural Networks for AI-Enabled IoT. Sensors 2023, 23, 1911. [Google Scholar] [CrossRef]
- Khalid, G.M.; Usman, A.G. Application of Data-Intelligence Algorithms for Modeling the Compaction Performance of New Pharmaceutical Excipients. Future J. Pharm. Sci. 2021, 7, 31. [Google Scholar] [CrossRef]
- Metekia, W.A.; Usman, A.G.; Ulusoy, B.; Abba, S.I.; Bali, K.C. Artificial Intelligence-Based Approaches for Modeling the Effects of Spirulina Growth Mediums on Total Phenolic Compounds. Saudi J. Biol. Sci. 2022, 29, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Alamrouni, A.; Aslanova, F.; Mati, S.; Maccido, H.S.; Jibril, A.A.; Usman, A.G.; Abba, S.I. Multi-Regional Modeling of Cumulative COVID-19 Cases Integrated with Environmental Forest Knowledge Estimation: A Deep Learning Ensemble Approach. Int. J. Environ. Res. Public. Health 2022, 19, 738. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, V.; Kaushik, A.; Furukawa, H.; Khosla, A. Review—Towards 5th Generation AI and IoT Driven Sustainable Intelligent Sensors Based on 2D MXENES and Borophene. ECS Sens. Plus 2022, 1, 013601. [Google Scholar] [CrossRef]
- Usman, A.G.; Işik, S.; Abba, S.I. Qualitative Prediction of Thymoquinone in the High-performance Liquid Chromatography Optimization Method Development Using Artificial Intelligence Models Coupled with Ensemble Machine Learning. Sep. Sci. Plus 2022, 5, 579–587. [Google Scholar] [CrossRef]
- Pandey, S.; Dixit, A.K.; Bahuguna, R.; Akram, S.V.; Pandey, V.; Kathuria, S. AI and IoT Enabled Technologies for Monitoring the Right to Health of Disabled People. In Proceedings of the 2022 5th International Conference on Contemporary Computing and Informatics (IC3I), Uttar Pradesh, India, 14–16 December 2022. [Google Scholar] [CrossRef]
- Ozsahin, D.U.; Balcioglu, O.; Usman, A.G.; Emegano, D.I.; Uzun, B.; Abba, S.I.; Ozsahin, I.; Yağdi, T.; Engin, C. Clinical Modelling of RVHF Using Pre-Operative Variables: A Direct and Inverse Feature Extraction Technique. Diagnostics 2022, 12, 3061. [Google Scholar] [CrossRef]
- Singh, Y.R.; Shah, D.B.; Maheshwari, D.; Shah, J.; Shah, S. Advances in AI-Driven Retention Prediction for Different Chromatographic Techniques: Unraveling the Complexity. Crit. Rev. Anal. Chem. 2023, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Usman, A.G.; Işik, S.; Abba, S.I. Hybrid Data-Intelligence Algorithms for the Simulation of Thymoquinone in HPLC Method Development. J. Iran. Chem. Soc. 2021, 18, 1537–1549. [Google Scholar] [CrossRef]
- Madaki, Z.; Abacioglu, N.; Usman, A.G.; Taner, N.; Şehirli, A.Ö.; Abba, S.I. Novel Hybridized Computational Paradigms Integrated with Five Stand-Alone Algorithms for Clinical Prediction of HCV Status among Patients: A Data-Driven Technique. Life 2022, 13, 79. [Google Scholar] [CrossRef]
- Jamei, M.; Karbasi, M.; Alawi, O.A.; Kamar, H.M.; Khedher, K.M.; Abba, S.I.; Yaseen, Z.M. Earth Skin Temperature Long-Term Prediction Using Novel Extended Kalman Filter Integrated with Artificial Intelligence Models and Information Gain Feature Selection. Sustain. Comput. Inform. Syst. 2022, 35, 100721. [Google Scholar] [CrossRef]
- Ughulu, J. The role of Artificial intelligence (AI) in Starting, automating and scaling businesses for Entrepreneurs. Sci. Prepr. 2022. [Google Scholar] [CrossRef]
- Kong, X.; Wu, Y.; Wang, H.; Xia, F. Edge Computing for Internet of Everything: A Survey. IEEE Internet Things J. 2022, 9, 23472–23485. [Google Scholar] [CrossRef]
- Gilbert, J.H.; Yan, J.; Hoffman, S.J. A WHO report: Framework for action on interprofessional education and collaborative practice. J. Allied Health 2010, 39 (Suppl. 1), 196–197. [Google Scholar] [PubMed]
- Smith, T.; Fowler-Davis, S.; Nancarrow, S.; Ariss, S.; Enderby, P. Leadership in Interprofessional Health and Social Care Teams: A Literature Review. Leadersh. Health Serv. 2018, 31, 452–467. [Google Scholar] [CrossRef] [PubMed]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Schmitz, C.C.; Radosevich, D.M.; Jardine, P.J.; MacDonald, C.J.; Trumpower, D.L.; Archibald, D. The Interprofessional Collaborative Competency Attainment Survey (ICCAS): A Replication Validation Study. J. Interprof. Care 2016, 31, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Solinís, R.N.; Zabalegui, I.B.; Arce, R.S.; Rodríguez, L.S.M.; Polanco, N.T. Development of a questionnaire to assess interprofessional collaboration between two different care levels. Int. J. Integr. Care 2013, 13, e015. [Google Scholar] [CrossRef] [PubMed]
- Tsionas, M.G.; Assaf, A.G. Regression Trees for Hospitality Data Analysis. Int. J. Contemp. Hosp. Manag. 2023; ahead of print. [Google Scholar] [CrossRef]
- Said, Z.; Sharma, P.; Tiwari, A.K.; Van Vang, L.; Huang, Z.; Van Ga, B.; Hoang, A.T. Application of Novel Framework Based on Ensemble Boosted Regression Trees and Gaussian Process Regression in Modelling Thermal Performance of Small-Scale Organic Rankine Cycle (ORC) Using Hybrid Nanofluid. J. Clean. Prod. 2022, 360, 132194. [Google Scholar] [CrossRef]
- Said, Z.; Sharma, P.; Sundar, L.S.; Nguyen, V.G.; Tran, V.D.; Le, V.V. Using Bayesian Optimization and Ensemble Boosted Regression Trees for Optimizing Thermal Performance of Solar Flat Plate Collector under Thermosyphon Condition Employing MWCNT-Fe3O4/Water Hybrid Nanofluids. Sustain. Energy Technol. Assess. 2022, 53, 102708. [Google Scholar] [CrossRef]
- Alnahit, A.O.; Mishra, A.K.; Khan, A.A. Stream Water Quality Prediction Using Boosted Regression Tree and Random Forest Models. Stoch. Environ. Res. Risk Assess. 2022, 36, 2661–2680. [Google Scholar] [CrossRef]
- Abedi, R.; Costache, R.; Shafizadeh-Moghadam, H.; Pham, Q.B. Flash-Flood Susceptibility Mapping Based on XGBoost, Random Forest and Boosted Regression Trees. Geocarto Int. 2021, 37, 5479–5496. [Google Scholar] [CrossRef]
- Nguyen, D.H.; Le, X.-H.; Anh, D.T.; Kim, S.-H.; Bae, D.-H. Hourly Streamflow Forecasting Using a Bayesian Additive Regression Tree Model Hybridized with a Genetic Algorithm. J. Hydrol. 2022, 606, 127445. [Google Scholar] [CrossRef]
- Luo, C.; Keshtegar, B.; Zhu, S.-P.; Niu, X. EMCS-SVR: Hybrid Efficient and Accurate Enhanced Simulation Approach Coupled with Adaptive SVR for Structural Reliability Analysis. Comput. Methods Appl. Mech. Eng. 2022, 400, 115499. [Google Scholar] [CrossRef]
- Ghali, U.M.; Usman, A.G.; Chellube, Z.M.; Degm, M.A.A.; Hoti, K.; Umar, H.; Abba, S.I. Advanced Chromatographic Technique for Performance Simulation of Anti-Alzheimer Agent: An Ensemble Machine Learning Approach. SN Appl. Sci. 2020, 2, 1871. [Google Scholar] [CrossRef]
- Adaryani, F.R.; Mousavi, S.J.; Jafari, F. Short-Term Rainfall Forecasting Using Machine Learning-Based Approaches of PSO-SVR, LSTM and CNN. J. Hydrol. 2022, 614, 128463. [Google Scholar] [CrossRef]
- Li, J.; Zhu, D.; Li, C. Comparative Analysis of BPNN, SVR, LSTM, Random Forest, and LSTM-SVR for Conditional Simulation of Non-Gaussian Measured Fluctuating Wind Pressures. Mech. Syst. Signal Process. 2022, 178, 109285. [Google Scholar] [CrossRef]
- Benaafi, M.; Yassin, M.; Usman, A.G.; Abba, S.I. Neurocomputing Modelling of Hydrochemical and Physical Properties of Groundwater Coupled with Spatial Clustering, GIS, and Statistical Techniques. Sustainability 2022, 14, 2250. [Google Scholar] [CrossRef]
- Abba, S.I.; Benaafi, M.; Usman, A.G.; Aljundi, I.H. Sandstone Groundwater Salinization Modelling Using Physicochemical Variables in Southern Saudi Arabia: Application of Novel Data Intelligent Algorithms. Ain Shams Eng. J. 2023, 14, 101894. [Google Scholar] [CrossRef]
- Ismail, S.; Abdulkadir, R.A.; Usman, A.G.; Abba, S.I. Development of Chemometrics-Based Neurocomputing Paradigm for Simulation of Manganese Extraction Using Solid-Phase Tea Waste. Model. Earth Syst. Environ. 2022, 8, 5031–5040. [Google Scholar] [CrossRef]
- Abba, S.I.; Benaafi, M.; Usman, A.G.; Aljundi, I.H. Inverse Groundwater Salinization Modeling in a Sandstone’s Aquifer Using Stand-Alone Models with an Improved Non-Linear Ensemble Machine Learning Technique. J. King Saud. Univ. Comput. Inf. Sci. 2022, 34, 8162–8175. [Google Scholar] [CrossRef]
- Rasol, M.; Pais, J.C.; Pérez-Gracia, V.; Solla, M.; Fernandes, F.M.C.P.; Fontul, S.; Ayala-Cabrera, D.; Schmidt, F.; Assadollahi, H. GPR Monitoring for Road Transport Infrastructure: A Systematic Review and Machine Learning Insights. Constr. Build. Mater. 2022, 324, 126686. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R.; Taylor, J. An Introduction to Statistical Learning: With Applications in Python; Springer: Berlin/Heidelberg, Germany, 2023. [Google Scholar] [CrossRef]
- Ghali, U.M.; Alhosen, M.; Degm, A.; Alsharksi, A.N.; Hoti, Q.; Usman, A.G. Development of computational intelligence algorithms for modelling the per-formance of humanin and its derivatives in HPLC optimization method development. IJSTR 2020, 9, 110–117. [Google Scholar]
- Benaafi, M.; Tawabini, B.; Abba, S.I.; Humphrey, J.; Al-Areeq, A.M.; Alhulaibi, S.A.; Usman, A.G.; Aljundi, I.H. Integrated Hydrogeological, Hydrochemical, and Isotopic Assessment of Seawater Intrusion into Coastal Aquifers in Al-Qatif Area, Eastern Saudi Arabia. Molecules 2022, 27, 6841. [Google Scholar] [CrossRef] [PubMed]
- Yassin, M.; Tawabini, B.; Al-Shaibani, A.; Adetoro, J.A.; Benaafi, M.; Al-Areeq, A.M.; Usman, A.G.; Abba, S.I. Geochemical and Spatial Distribution of Topsoil HMs Coupled with Modeling of Cr Using Chemometrics Intelligent Techniques: Case Study from Dammam Area, Saudi Arabia. Molecules 2022, 27, 4220. [Google Scholar] [CrossRef] [PubMed]
- Groß, J. Linear Regression; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Archibald, D.; Trumpower, D.; MacDonald, C.J. Validation of the interprofessional collaborative competency attainment survey (ICCAS). J. Interprof Care 2014, 28, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; Tata Mcgraw-Hill Ed: New Delhi, India, 1994. [Google Scholar]
- Mohammed, C.A.; Anand, R.; Ummer, V.S. Interprofessional Education (IPE): A framework for introducing teamwork and collaboration in health professions curriculum. Med. J. Armed Forces India 2021, 77 (Suppl. 1), S16–S21. [Google Scholar] [CrossRef]




| Pre-ICCAS | Post-ICCAS | |
|---|---|---|
| Valid | 6 | 6 |
| Missing | 0 | 0 |
| Paired Differences | t-Test | df | Sig. (2-Tailed) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | ||||||
| Lower | Upper | ||||||||
| Pair 1 | Pre- and post-ICCAS | 12.000 | 4.050 | 1.653 | 7.750 | 16.250 | 7.258 | 5 | 0.001 |
| Items | Paired Differences | t-Test | df | Sig. (2-Tailed) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | |||||
| Lower | Upper | |||||||
| Pair 1 * | −1.143 | 0.778 | 0.085 | −1.312 | −0.974 | −13.457 | 83 | 0.000 |
| Pair 2 * | −0.940 | 0.421 | 0.046 | −1.032 | −0.849 | −20.480 | 83 | 0.000 |
| Pair 3 * | −0.774 | 0.647 | 0.071 | −0.914 | −0.633 | −10.968 | 83 | 0.000 |
| Pair 4 * | −0.917 | 0.354 | 0.039 | −0.994 | −0.840 | −23.715 | 83 | 0.000 |
| Pair 5 * | −0.857 | 0.794 | 0.087 | −1.029 | −0.685 | −9.898 | 83 | 0.000 |
| Pair 6 * | −1.167 | 0.534 | 0.058 | −1.283 | −1.051 | −20.024 | 83 | 0.000 |
| Pair 7 * | −0.786 | 0.641 | 0.070 | −0.925 | −0.647 | −11.228 | 83 | 0.000 |
| Pair 8 * | −0.786 | 0.413 | 0.045 | −0.875 | −0.696 | −17.445 | 83 | 0.000 |
| Pair 9 * | −0.631 | 0.655 | 0.071 | −0.773 | −0.489 | −8.835 | 83 | 0.000 |
| Pair 10 * | −0.369 | 0.485 | 0.053 | −0.474 | −0.264 | −6.968 | 83 | 0.000 |
| Pair 11 * | −0.345 | 0.814 | 0.089 | −0.522 | −0.169 | −3.887 | 83 | 0.000 |
| Pair 12 * | −0.679 | 0.584 | 0.064 | −0.805 | −0.552 | −10.647 | 83 | 0.000 |
| Pair 13 * | −0.655 | 0.478 | 0.052 | −0.759 | −0.551 | −12.546 | 83 | 0.000 |
| Pair 14 * | −0.536 | 0.590 | 0.064 | −0.664 | −0.408 | −8.322 | 83 | 0.000 |
| Pair 15 * | −0.250 | 0.805 | 0.088 | −0.425 | −0.075 | −2.847 | 83 | 0.006 |
| Pair 16 * | −0.774 | 0.499 | 0.054 | −0.882 | −0.665 | −14.200 | 83 | 0.000 |
| Pair 17 * | −0.845 | 0.814 | 0.089 | −1.022 | −0.669 | −9.518 | 83 | 0.000 |
| Pair 18 * | −0.476 | 0.526 | 0.057 | −0.590 | −0.362 | −8.299 | 83 | 0.000 |
| Pair 19 * | −0.500 | 0.591 | 0.064 | −0.628 | −0.372 | −7.753 | 83 | 0.000 |
| ShGs | P-C A | MK | Trust | StGs | SL | SI | FMs | Protocol | ISs | |
|---|---|---|---|---|---|---|---|---|---|---|
| Chi-squared | 23.073 a | 58.815 b | 131.103 c | 47.741 d | 106.099 b | 52.667 e | 50.533 f | 48.988 g | 44.778 d | 75.605 b |
| df | 3 | 4 | 4 | 3 | 4 | 3 | 4 | 4 | 3 | 4 |
| Asymp. Sig. | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Cronbach’s Alpha | N of Items | |
|---|---|---|
| Pre- and Post ICCAS | 0.994 | 2 |
| 10 items Questionnaire | 0.941 | 10 |
| RIPLS and Paired t-Test pre-variables | 0.986 | 19 |
| RIPLS and Paired t-Test post-variables | 0.988 | 19 |
| ALC | EIC | PCF | ECC | SMI | WEE | LWE | IDA | BAC | UAC | RSA | UAA | UAP | IPD | ILP | TAI | ACR | DEP | NRO | PEC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALC | 1.0 | |||||||||||||||||||
| EIC | 0.3 | 1.0 | ||||||||||||||||||
| PCF | 0.7 | 0.4 | 1.0 | |||||||||||||||||
| ECC | 0.4 | 0.3 | 0.6 | 1.0 | ||||||||||||||||
| SMI | 0.4 | 0.3 | 0.6 | 0.5 | 1.0 | |||||||||||||||
| WEE | 0.5 | 0.6 | 0.7 | 0.6 | 0.4 | 1.0 | ||||||||||||||
| LWE | 0.5 | 0.7 | 0.7 | 0.5 | 0.6 | 0.8 | 1.0 | |||||||||||||
| IDA | 0.5 | 0.7 | 0.6 | 0.7 | 0.7 | 0.6 | 0.7 | 1.0 | ||||||||||||
| BAC | 0.5 | 0.6 | 0.8 | 0.7 | 0.6 | 0.7 | 0.7 | 0.7 | 1.0 | |||||||||||
| UAC | 0.6 | 0.6 | 0.7 | 0.4 | 0.4 | 0.5 | 0.6 | 0.5 | 0.6 | 1.0 | ||||||||||
| RSA | 0.5 | 0.6 | 0.5 | 0.6 | 0.2 | 0.6 | 0.5 | 0.6 | 0.6 | 0.7 | 1.0 | |||||||||
| UAA | 0.1 | 0.5 | 0.2 | 0.4 | 0.4 | 0.4 | 0.5 | 0.5 | 0.5 | 0.5 | 0.6 | 1.0 | ||||||||
| UAP | 0.1 | 0.4 | 0.2 | 0.5 | 0.1 | 0.5 | 0.3 | 0.3 | 0.5 | 0.4 | 0.6 | 0.7 | 1.0 | |||||||
| IPD | 0.6 | 0.3 | 0.2 | 0.3 | 0.4 | 0.4 | 0.4 | 0.5 | 0.2 | 0.4 | 0.5 | 0.5 | 0.5 | 1.0 | ||||||
| ILP | 0.3 | 0.7 | 0.4 | 0.5 | 0.4 | 0.6 | 0.7 | 0.7 | 0.6 | 0.7 | 0.7 | 0.8 | 0.6 | 0.5 | 1.0 | |||||
| TAI | 0.2 | 0.4 | 0.4 | 0.5 | 0.5 | 0.4 | 0.5 | 0.5 | 0.5 | 0.5 | 0.4 | 0.8 | 0.6 | 0.5 | 0.8 | 1.0 | ||||
| ACR | 0.7 | 0.2 | 0.6 | 0.3 | 0.5 | 0.5 | 0.4 | 0.4 | 0.3 | 0.6 | 0.4 | 0.0 | 0.1 | 0.6 | 0.2 | 0.2 | 1.0 | |||
| DEP | 0.5 | 0.4 | 0.5 | 0.3 | 0.4 | 0.6 | 0.6 | 0.5 | 0.3 | 0.6 | 0.5 | 0.4 | 0.3 | 0.6 | 0.7 | 0.4 | 0.5 | 1.0 | ||
| NRO | 0.3 | 0.1 | 0.5 | 0.5 | 0.6 | 0.4 | 0.4 | 0.4 | 0.7 | 0.4 | 0.3 | 0.4 | 0.5 | 0.4 | 0.4 | 0.7 | 0.3 | 0.3 | 1.0 | |
| PEC | 0.6 | 0.3 | 0.4 | 0.4 | 0.6 | 0.3 | 0.4 | 0.5 | 0.3 | 0.4 | 0.2 | 0.0 | −0.2 | 0.4 | 0.2 | 0.2 | 0.6 | 0.3 | 0.2 | 1.0 |
| Calibration | ||||
|---|---|---|---|---|
| R2 | CC | RMSE | MSE | |
| RT | 0.827 | 0.909 | 1.364 | 1.860 |
| SVM | 0.905 | 0.951 | 1.010 | 1.020 |
| GPR | 1.000 | 1.000 | 0.000 | 0.000 |
| LR | 0.939 | 0.969 | 0.810 | 0.656 |
| Validation | ||||
| RT | 0.821 | 0.906 | 1.366 | 1.867 |
| SVM | 0.900 | 0.949 | 1.062 | 1.127 |
| GPR | 1.000 | 1.000 | 0.000 | 0.000 |
| LR | 0.921 | 0.960 | 0.857 | 0.735 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamed, M.; Altinay, F.; Altinay, Z.; Dagli, G.; Altinay, M.; Soykurt, M. Validation of Instruments for the Improvement of Interprofessional Education through Educational Management: An Internet of Things (IoT)-Based Machine Learning Approach. Sustainability 2023, 15, 16577. https://doi.org/10.3390/su152416577
Mohamed M, Altinay F, Altinay Z, Dagli G, Altinay M, Soykurt M. Validation of Instruments for the Improvement of Interprofessional Education through Educational Management: An Internet of Things (IoT)-Based Machine Learning Approach. Sustainability. 2023; 15(24):16577. https://doi.org/10.3390/su152416577
Chicago/Turabian StyleMohamed, Mustafa, Fahriye Altinay, Zehra Altinay, Gokmen Dagli, Mehmet Altinay, and Mutlu Soykurt. 2023. "Validation of Instruments for the Improvement of Interprofessional Education through Educational Management: An Internet of Things (IoT)-Based Machine Learning Approach" Sustainability 15, no. 24: 16577. https://doi.org/10.3390/su152416577







