1. Introduction
Climate change has been described as the biggest potential public health threat that present and future generations face [
1]. As a consequence of climate change, extreme events such as heatwaves, heavy rain, storms, wildfires, and a range of others have increased in the last decade. Luber [
2] mentions that these events directly impact the morbidity and mortality of the population worldwide, and they indirectly impact them through fluctuating distribution of vectors, the increment of pollen counts, and the increment of air pollution.
Unfortunately, the attention given to disasters caused by climate change is greater than the importance of its effects on health. This fact is one of the reasons why it is crucial to address these threats from the public health perspective since the primary purpose of any action against the effects of climate change is to preserve people’s lives and health.
To address the impacts of climate change on health, all the country’s stakeholders must work together to adapt to climate change. Some of the most important among them are the organisations working to deliver health sector services since they are responsible for caring for the population’s health and helping improve their quality of life. As stated by Costello et al., the response to climate change requires a multidisciplinary and multisectoral public health movement that works together with other stakeholders, including academic institutions [
1]. This is supported by the 2015 Decision of the Conference of Parties (COP) in Paris, which emphasises the involvement of non-party stakeholders, including cities and other subnational authorities [
3].
Nevertheless, despite the importance of the participation of the health sector in developing climate change adaptation plans, there are still some barriers to it. After conducting interviews with health employees, one study [
2] concluded that institutional barriers obstructed the development of health adaptation strategies since they felt that the health sector was not perceived as an essential stakeholder in adaptation planning discussions. Furthermore, financial barriers, lack of communication and knowledge about climate change topics, and limited leadership are typical constraints in climate adaptation in the health sector [
4]. However, there is potentially a distinction in the performance between the private and public sector health systems, where the national picture might be different due to the financing and quality of service and their impacts on their managerial decisions and actions [
5]. These facts increase the vulnerability of the health sector and, of course, the population worldwide.
In this regard, the WHO affirmed that national and regional plans need to be bolstered to enable the development and implementation of health adaptation actions [
6]. National governments regularly state that they are preparing comprehensive health adaptation programmes. Nonetheless, they do not address specific health risks, likely because of the nature of national-level efforts and regulations designed to lead more focused activities at their subnational level [
7]. Since national plans are developed on a large scale, tracking a region’s specific needs is difficult. Therefore, each region should develop its Health Adaptation Plan to recognise specific vulnerabilities and needs in order to identify unique requirements such as budget, infrastructure, and others. However, what happens when the subnational level does not have a national plan to align with? This highlights the importance of developing an approach for the subnational levels that helps elaborate adaptation plans takes place.
On this matter, the UNFCCC and the WHO elaborated guidelines and tools to help countries develop their national Health Adaptation Plans [
6], which can also support the health sector at regional or local levels. Nevertheless, since they were designed and directed for national levels, if they are intended to be used in a subnational health organisation, these guidelines and tools need to adapt to their context, and guidance is required.
This research aims to identify an approach for developing subnational-level climate change adaptation plans for the health sector. This research will answer questions about what guidelines and tools are available for the health sector to undertake adaptation plans and what the main phases and steps are to develop them.
1.1. Climate Change
Global climate change is altering weather patterns and is projected to significantly exceed the climatic range humans have been used to experiencing [
8]. Climate change impacts the natural environment, economic activities, and health and well-being in every corner of the planet, and no region is immune [
9]. These climate-related events are predicted to pose significant direct and indirect health hazards, especially for city dwellers [
2].
Costello et al. stated that an integrated method to diminish the adverse effects of climate change on the population requires three levels of action [
1]. The first one is related to the mitigation measures to decrease the greenhouse emissions in order to downtrend the increase in global warming. The second level is to find the impacts of climate change on health, and the third is to adapt the public health system to respond to these adverse effects. These last two levels of action are developed in the following points.
1.2. Climate Change and Health
A rising number of studies show the alarming effects of climate change on human health. As the World Health Organization (WHO) reported, over the last 30 years, global warming and heavy precipitations have already claimed the lives of 150,000 people yearly [
10]. The WHO calculated that, between 2030 and 2050, an extra 250,000 people might die annually due to climate change’s effects [
9].
According to the IPCC, changes in extreme climate events such as floods, storms, heatwaves, and others increase the risks of climate-related diseases or even mortality rates [
11]. The outcome could be worsened by the population’s level of vulnerability and exposure. Therefore, to assess a particular city’s risk level, data regarding vulnerability, hazard, and exposure are needed.
Several studies have revealed that the distribution of food, arthropod, and vector and water-borne diseases is being affected by climate change. For example, after conducting interviews, meetings, workshops, and surveys, a study conducted in Queensland, Australia, identified the impacts of climate change on health and well-being. Some recognised impacts were changes in infectious and vector-borne diseases, increments in air pollution, heat stress, decreased water and food safety, augmentation of social inequality and vulnerability, and mental health [
12]. Another study revealed that, since 1990, the number of dengue cases every decade has doubled, which is an increment attributed to rapid urbanisation and climate change [
13].
The effects of climate change on human health have been categorised as direct and indirect [
9]. The first can result in morbidity and mortality due to the increasing frequency of hazards such as floods, storms, and heat waves due to changes in the weather. The indirect effects are water quality, air pollution, and land-use changes, which, in the future, according to the Urban Climate Change Research Network (UCCRN), are more likely to affect cities [
14]. Thus, the increase in the number of disasters due to climate change can augment the population’s risks of illnesses like respiratory diseases, allergies, dengue, and malaria, among others [
1,
15,
16].
Furthermore, climate change is harming the infrastructure needed to safeguard communities’ health and well-being, and it is impacting the operation of health care facilities [
12]. Different hazards can affect hospitals’ infrastructure and services in diverse ways. For instance, extreme temperatures such as heat and cold waves can affect a hospital’s ventilation system, and storms can cause energy loss in the building premises [
17].
The combination of both the increasing health effects on the population and the impacts on the infrastructure of hospitals can obstruct or hinder health services. For example, in 2005 in Sydney, heatwaves particularly affected vulnerable people, resulting in an increase in hospital admissions and putting additional strain on the existing infrastructure, which had insufficient surge capability to deal with the changed admission profiles and high demand [
18]. Another case is presented in a study conducted by Sinclair about the risk of overheating in healthcare buildings in Scotland. This research found that four out of five hospitals examined presented overheating issues at certain times of the year due to solar gain and poor natural ventilation. This overheating caused, besides direct risks to patients, the risk of microbiological growth, a possible rise of legionella cases, and an increase in fatigue in the medical staff, lowering their quality of performance [
19]. Other hazards related to climate change may significantly impact the operation of many health care facilities, which can affect the hospitals’ services and infrastructure [
17].
This suggests that climate change can affect the population’s health, the assets of the health care system, and the health services provided to the patients. Therefore, it is critical to estimate the impacts of climate change on health by applying a proper health risk assessment. The latter could be performed by considering recent past and present observations of the effects of climate variability on health and the influence of different modulating factors [
20]. Once the risks are recognised, applying different strategies in the health sector is crucial in order to prepare for and respond to the possible occurrence of adverse events in order to guarantee health care service continuity.
1.3. Climate Change Response Strategies: Adaptation
There are two strategies available to address climate change. The first one is the mitigation strategy related to primary prevention, which aims to reduce or stabilise the greenhouse gases in the atmosphere. The second is adaptation, related to secondary prevention, which refers to being prepared for climate change’s anticipated effects [
10]. Applying mitigation and adaptation responses benefits countries by making them not hampered by the adverse effects of climate change, allowing them to improve their citizens’ health and well-being [
9].
These strategies have been used by different sectors and levels of governance around the world. For example, in South Korea, there have been studies on waste management in hospitals, and the United Kingdom evaluates data on the health sector’s carbon footprint [
3].
While much attention has been paid to mitigating climate change’s effects, like the examples above, the progress on this subject is slow. Currently, the focus is shifting to developing climate change adaptation plans and systems [
21].
The adaptation strategy tries to respond to and manage the impacts and consequences of climate change. During the past decades, human activities have released greenhouse gases (GHG) that have caused damage to the atmosphere, and future effects on the environment and society are inevitable. For this reason, it is necessary to work on the adaptation strategies until the mitigation strategies take effect.
1.4. Adaptation to Climate Change in the Health Sector
As Patz, Grabow and Limaye stated, adaptation to climate change refers to reducing its effects on health [
15]. For example, preparing health authorities and medical facilities for extreme events can minimise mortality and morbidity. Likewise, public health epidemiological surveillance can detect infectious illness outbreaks in susceptible locations, which is necessary for timely response [
10].
In recent years, since the start of the COVID-19 pandemic, the health system’s lack of resilience and capability to respond to health emergencies has been notorious and worrying. Consequently, the urgency to improve and prepare health systems for future massive emergencies has emerged. Strengthening the health sector to be climate resilient not only contributes to responding appropriately to the effects of climate change but also to pandemics [
13] or other extreme adverse events.
1.5. Health Adaptation Plans
There is a clear requirement to facilitate understanding and to address the challenge health sector organisations face in gathering information about climate-related health risks and the development of climate change adaptation actions into a single document. This is when the importance of developing adaptation plans in the health sector occurs, and there is a need to establish an approach for producing this document.
One way is to consider the adaptation process as a project, and the literature shows different processes for planning and executing projects. According to the Guide of the Project Management Body of Knowledge (PMBoK), the project management processes are grouped into five distinct phases, which include initiation, planning, execution, monitoring, and closure [
22]. These phases have served as a foundational framework for numerous organisations as they formulate their guidelines for adaptation planning.
In the context of adaptation planning in the health sector, in 2010, the UNFCCC initiated the National Adaptation Plan process, recognising the need for adaptation planning and developing the technical guidelines to facilitate implementing this process in the Least Developed Countries (LDC). In these guidelines, the UNFCCC established four crucial elements of the formulation of National Adaptation Plans (NAPs) and the steps under these elements, which are as follows [
8]:
Lay the groundwork and address gaps: initiating the process by identifying the effects of climate change and vulnerability.
Preparatory elements: analysing current and future climate scenarios, estimating vulnerabilities, and recognising adaptation activities.
Implementation strategies: prioritising adaptation actions and implementing them.
Reporting, monitoring, and review: monitor, report, and update the National Adaptation Plan.
Aligned with the UNFCCC guidelines, the WHO developed Guidance to Protect Health from Climate Change through Health Adaptation Planning (HNAPs), describing the concepts of the planning process, key elements, and steps.
Other complementary documents have been published to establish the most critical elements and steps in order to elaborate on the adaptation plans. One of these publications is the WHO Operational Framework for Building Climate-Resilient Health Systems, which intends to guide countries in developing an approach to address the effects of climate change on health. This framework considers 10 components that can structure a Health Adaptation Plan, assign tasks and roles, and allocate human and financial resources.
To ensure informed planning, one of the most critical steps during the elaboration of a climate change adaptation plan is carrying out a Vulnerability and Adaptation Assessment (V&A), where a thorough analysis of the adverse effects of climate change on different health aspects is performed. Therefore, the WHO outlined a V&A process to assess the most vulnerable populations, identify health system and service weaknesses, and recognise climate-sensitive health risks [
6].
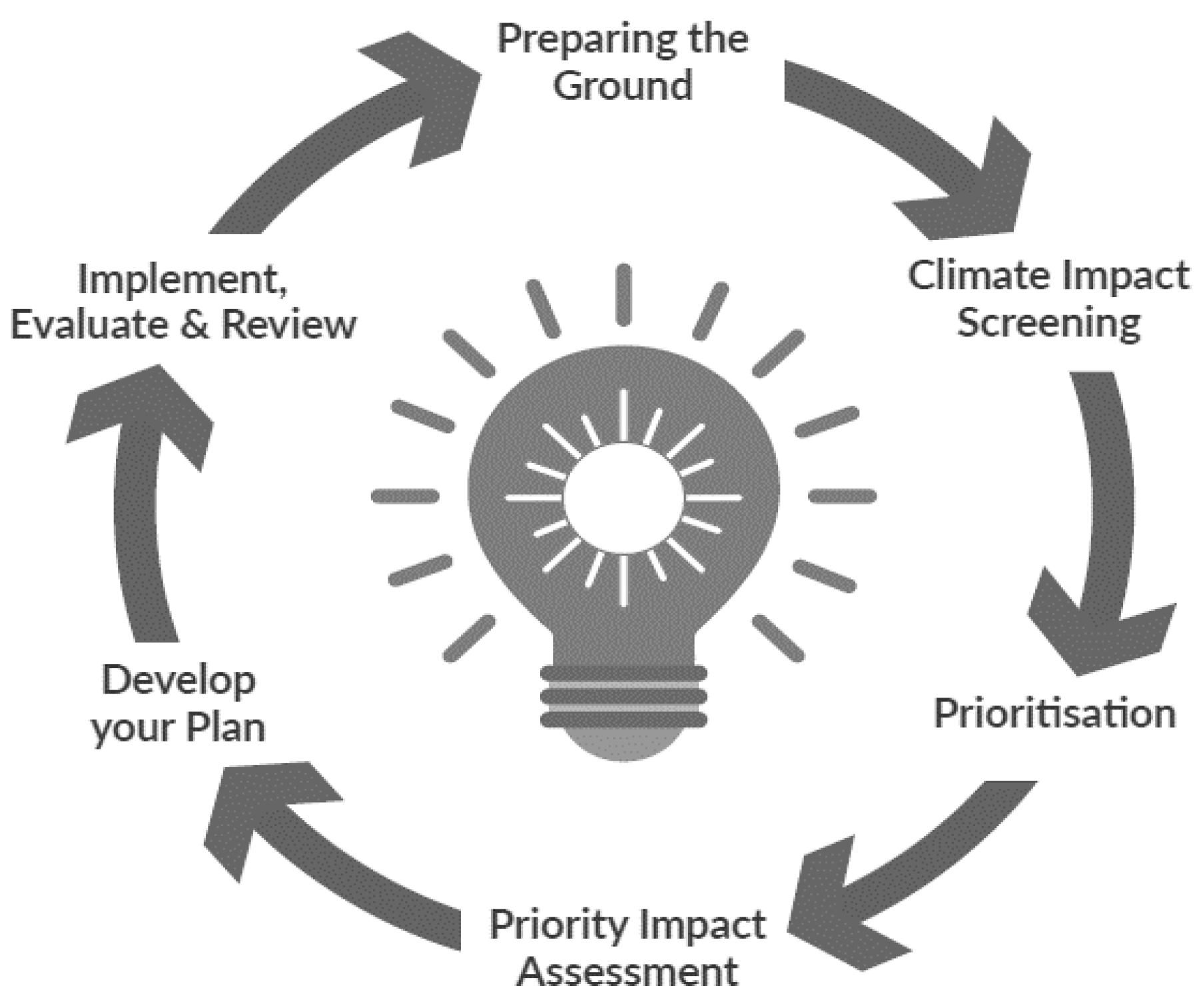
Although the WHO has published HNAP guidelines to help countries develop their plans, some governments have chosen to focus on their national realities and develop their own guidelines, as in the case of the Government of Ireland. The following figure shows the steps of a planning cycle set up by the Government of Ireland in its Sectoral Planning Guidelines for Climate Change Adaptation 2018 (see
Figure 1) [
23].
1.6. The Health Adaptation Planning Gap
Despite the importance of adaptation, there are a limited number of Health Adaptation Plans (henceforth referred to as HAPs in this research) worldwide, and there is scarce information about how to develop them. This crucial gap constrains the health sector from preparing for and reacting to future climate-related health impacts. Current guidelines and tools to create HAPs have information about the key aspects necessary for elaborating on them; nevertheless, they have not been gathered and analysed in a single document in order to provide sufficient information to help develop these plans.
Another gap is the knowledge on developing a HAP for an organisation at a subnational level if the national level has not yet elaborated on one. Considering that many countries do not have a HAP developed, it is difficult for subnational-level health organisations to take the initiative to create one if they do not have a model to follow, which, in the end, delays the start of the adaptation planning process or, even worse, this process never starts. For instance, NHS Scotland, the national body of the health system in Scotland, does not have a HAP and its NHS Boards, which are the regional bodies of their health system, and they have not yet formulated their plans. As per insights from the NHS Boards through a series of interviews, several obstacles emerged, such as a lack of human resources to handle the workload, which impede this initiative from commencing. Moreover, the absence of a national HAP further compounds the challenges associated with this undertaking.
Regarding this last issue, it can be argued that national-level guidelines, such as the ones provided by the WHO, can be adapted for use in subnational-level organisations. Making these guidelines more straightforward can promote the development of HAPs at subnational levels.
Therefore, it is necessary to tackle these gaps using different guidelines and tools, such as the ones provided by the UNFCCC, the WHO, and other organisations, by adapting them to the regional contexts while considering their organisational structure, the organisation’s current situation, their policies, available information regarding adaptation, human resources, and their financial capacity, among others.
2. Materials and Methods
This research adopts an inductive approach based on establishing research questions and then allowing themes and theory to emerge, and it applies qualitative multi-methods to reach its aim with two phases: (1) document collection (and selection), and (2) document analysis.
2.1. Phases of the Research
This research was carried out in two different phases. In the first phase, this study collected the guidelines and tools of the WHO, different countries, and existing HAPs at national and subnational levels to understand the current approaches to developing HAPs. In the second phase, these documents were coded to obtain the most suitable way to develop HAPs by recognising the elements and steps that should be followed (see
Figure 2).
2.2. Phase 1 Data Collection (and Selection)
Document analysis was applied in this research to search for information related to guidelines and tools to develop HAPs and existing adaptation plans, among other documents. The selection of these documents was limited to the last twenty years (since 2003), reflecting the timeline relating to the emergence of climate change adaptation as a concern.
Guidelines and tools for creating climate change adaptation plans are essential sources of knowledge for this study and provide a first understanding of what steps should be followed and what kinds of data are needed to create a HAP. This helped categorise the specific information required for the case study (such as stock on available information, stakeholders’ engagement, and the organisation’s current situation, among others). These guidelines and tools were mainly searched for on governmental and non-governmental websites. The most important source of data was the WHO website.
Health adaptation plans from diverse countries and worldwide organisations were searched for online. This search was performed to determine the most suitable approach for creating subnational HAPs, previous analysis, assessment, and comparison. Further, the data contained in these plans helped us to obtain information related to the structural content of a HAP and the level of detail in national and subnational adaptation plans. Existing HAPs were mainly found through Google search using words such as “health adaptation plans”.
These data were collected and selected using different inclusion and exclusion criteria (See
Table 1).
Since HAP guidelines and tools are not published in journals and bibliographic databases, the search for this information started on the World Health Organization webpage (
www.who.int accessed on 22 June 2022) and in the country/city-specific databases. In addition, other organisations’ websites for developing guidelines related to adaptation to climate change were consulted.
The literature search applied publication date restrictions to obtain information published from 2003 or after. Moreover, a snowball search was conducted on the considered books’ and journals’ reference lists to make this search optimal.
Furthermore, interviews were conducted with healthcare practitioners from the NHS Greater Glasgow and Clyde, a regional health organisation part of NHS Scotland (National Health Service Scotland), to understand what is missing in the adaptation process and to gain an initial understanding of the subject under research.
2.3. Phase 2 Data Analysis
In the process of qualitative data analysis in this research, thematic analysis was used. This study followed the steps outlined by Braun and Clarke [
25] to carry out the thematic analysis of the data. It is worth noting that this process was recursive since each step taken can feed into other steps. Due to the nature of this study, an inductive approach was used to analyse the codes created, and they were combined into main themes [
25]. The codes and themes were obtained from the analysed documents (guidelines, tools, and existing Health Adaptation Plans).
The coding process was undertaken for the data obtained from document analysis. The type of coding used in this research was descriptive coding, which assigns labels and groups similar topic data [
26]. The qualitative data research software QSR NVivo 10 was used to generate codes to guarantee quality information analysis [
27]. The main codes generated were related to the phases and steps of health adaptation planning. The output was later analysed in the present study.
3. Results and Discussion
3.1. Adapting Guidelines and Tools for Developing Health Adaptation Plans
Since the WHO is the highest-level governing body in health worldwide, the guidelines and tools developed by this organisation were crucial for understanding the essential elements and steps of developing HAPs. The “WHO Guidance to Protect Health from Climate Change through Health Adaptation Planning” (henceforth referred to as WHO Guidance in this research) was designed to ensure that the health component is integrated into the National Adaptation Planning process, and its main purpose is to support countries in HNAP development. It is one of the main tools used to develop adaptation plans in the health sector.
As the WHO affirmed, these guidelines are not mandatory and should be modified to fit each country’s context [
28]. Thus, as the WHO Guidance targets the Ministries of Health or equivalent national levels. If its use is intended to help develop an adaptation plan at a subnational level, it must be adapted to the organisation’s context.
A total of 15 guidelines were searched and screened. From these, after assessing and selecting them with the pre-defined inclusion and exclusion criteria, 11 guidelines were selected in the present study’s analysis (See
Table A1).
3.1.1. WHO Guidelines and Tools
From the guidelines and tools selected, two keys form the basis for developing HAPs. The WHO Guidance describes, in brief, the elements and steps for developing HAPs, whereas the “WHO Quality Criteria for Health National Adaptation Plans (HNAPs)” (henceforth referred to as WHO Quality Criteria in this document) was developed to be used in tandem with the mentioned guidance. Both documents deliver complete information about developing a HAP and what quality criteria should be undertaken for its success.
Regarding the Health Adaptation Planning process in the WHO Guidance, the four elements are laying the groundwork and addressing gaps; preparatory elements; implementing actions and reporting; and monitoring and reviewing [
6]. These elements are broadly related to the first four phases of a PMBoK project life cycle: initiating, planning, executing, and monitoring [
29]. The last phase of a project cycle is closing, which is not considered in the WHO Guidance since something that differentiates this adaptation planning process from a project is that it is iterative, periodically revised, and updated. These elements are discussed in the next sections.
To support this guidance, in 2021, the WHO Quality Criteria was published. It provides support by giving a set of criteria to develop quality HAPs, which can be adapted to particular contexts. The WHO Quality Criteria covers six topic areas. The first topic concerns leadership, highlighting that the health sector’s commitment is critical for effective adaptation planning. The second one is related to cross-sectoral coordination, where health-determining sectors such as water, agriculture, sanitation, and electricity are involved in all the phases of the plan development. Next is the comprehensive coverage of climate-sensitive health risks, which involves a Vulnerability and Adaptation Assessment and the prioritisation of risks. Following on from this, topic four presents comprehensive coverage of adaptation options and actions, including prioritising health adaptation actions according to the magnitude of risk, level of vulnerability, resources, and funding. Resourcing is another topic included in the quality criteria. Human and financial resource estimation is needed to assign or mobilise required resources for adaptation actions. Finally, the last topic is monitoring, evaluation, and reporting (M,E&R). This document states that the result of the M,E&R is helpful to determine compliance with the plan and its further improvement [
28].
This WHO Quality Criteria results from the WHO’s lessons learned while supporting the development of HNAPs and the assessment of existing HNAPs, reflecting the knowledge gained in the creation of that document. The presented case studies also help the user better comprehend the application of the criteria in different contexts. It helps the reader understand that following the steps and a framework are not enough, and good practices must also be followed to develop an efficient HAP. Hence, it is a valuable resource for any organisation to use while creating its HAP.
Additionally, the WHO Guidance and Quality Criteria documents provide links to other tools that help carry out different steps during the elaboration of the adaptation plans.
Figure 3 represents the relationship between these documents and which tools and materials feed the elements of the WHO Guidance, assisting with the creation of HAPs. Some examples of this are the WHO Climate Change and Health: Vulnerability and Adaptation Assessment [
30] and the Checklists to Assess Vulnerabilities in Health Care Facilities in the Context of Climate Change [
31]. These can be used during the recognition of climate-sensitive health risks in the HNAP preparatory element (the second element of the WHO Guidance). The first helps to assess policies and programmes related to resilience and current and future vulnerabilities at national and subnational levels, and the second helps users establish a baseline for climate change resilience in healthcare facilities. The description of the other available tools is provided in
Table A1.
Recognising the relationship between the abovementioned documents is intended to organise the tools available for their employment in each element. From a public health point of view, these documents are comprehensive, and their use in each step strengthens the adaptation planning process. However, some guidelines mentioned in the WHO Guidance do not exist or are not available online. That is the case with the “WHO conceptual framework for indicators to support health-oriented climate change adaptation”, a document whose purpose was to guarantee the addition of health indicators in the monitoring programmes of health-determining sectors [
6]. The absence of mentioned guidelines could compromise the correct use of these tools.
Although these guidelines were developed to help LDCs and are characterised by their practicality of use, if they were to be used by a subnational-level organisation, the high complexity in some of them and lack of detail in others could make them challenging to understand and use.
3.1.2. Other Adaptation Planning Guidelines
In addition, guidelines for creating sectoral adaptation plans from other countries were searched for in order to analyse how their content helps their different sectors, including the health sector, to develop their plans. However, information related to these documents is scarce, and only three were obtained for this study.
The first one is “Scotland Adapts: A Capability Framework for a Climate Ready Public Sector”, a document created by Adaptation Scotland. The framework is based on four adaptation capabilities and recommended actions that support an organisation’s progress within the public sector in different maturity stages (starting, intermediate, advanced, and mature) [
32]. These four capabilities are Organisational Culture and Resources, Understanding the Challenge, Planning and Implementation, and Working Together. It also mentions the Monitoring and Evaluation process’s importance for the long-term success of the adaptation. Although this capability framework is not a guideline for developing adaptation plans, it presents a flexible approach that intends to help organisations adapt to climate change and determine which identified capabilities can be related to the different phases of adaptation planning. Nevertheless, due to the nature of this document, it does not present a deep level of detail, but it helps to lay the groundwork for each stage.
Another guideline is “Sectoral Planning Guidelines for Climate Change Adaptation 2018” from the Government of Ireland. This adaptation planning guideline is structured around a six-step planning cycle, where the first two steps are focused on preparing the groundwork for developing the plan effectively and recognising the impacts of climate change. The third step focuses on prioritising these impacts, and step four involves an impact assessment according to this prioritisation. Steps five and six identify goals and adaptation actions to be implemented [
23]. The document is easy to use in any sector and, with comprehensive content, presents a good quality and quantity of information.
The third guideline is the one from the Santa Lucia Government, which, with the support of the Government of the United States, developed “Guidelines for the Development of Sectoral Adaptation Strategies and Action Plans”. This guideline builds on four phases. The first phase is stocktaking, focusing on understanding the context and calling for four steps (current circumstances, policy framework, vulnerability, and potential adaptation measure). The second phase is related to stakeholder validation of the stocktaking results, which involves reviewing and improving the results from the first phase. The third step entails prioritising adaptation measures, and the last phase includes two steps for finalising the plan: feedback and a final workshop [
33]. The guideline promotes joint work with the stakeholders by conducting workshops and meetings during the plan’s development.
Figure 3 presents the four previously mentioned approaches for developing adaptation plans. The phases (which are composed of a series of steps) of developing a HAP in the four different guidelines analysed are called elements (WHO), capabilities (Scotland Government), steps (Ireland Government), and phases (Santa Lucia Government). However, they were coded as “Elements”, as defined by the WHO [
6], for comparison purposes.
Even though these four guidelines present different approaches to developing HAPs, each of their elements can be aligned with the WHO Guidance’s elements since their contents are similar.
Figure 4 shows the relationship between the elements of the approaches of the governments of Scotland, Ireland, and Santa Lucia and those from the WHO.
Before adapting these guidelines for use in a subnational-level organisation, this relationship was the first step and is considered in the following sections during the coding process.
3.1.3. Existing Health Adaptation Plans
Data regarding existing Health Adaptation Plans are difficult to find; as a result, six HAPs were included in the present research. The first four are national-level plans from Ireland, Tanzania, North Macedonia, and Italy. The other two are subnational plans from NHS Bristol, North Somerset, and South Gloucestershire (BNSSG)—England, and Queensland—Australia (See
Table A2).
- (1)
National-Level Health Adaptation Plans
- (a)
Government of Ireland—Health Climate Change Sectoral Adaptation Plan 2019–2024
This plan follows the sectoral guidelines provided by the same government, and it shows the results of literature research for the recognition of health risks, as well as stakeholders’ workshops for the development of the plan. As a result, the plan presents a comprehensive analysis of climate-sensitive health risks and, due to the execution of workshops, the involvement of stakeholders in the whole process.
Their programmed actions are divided into actions areas such as leadership, severe weather events, and monitoring. They also describe coordinators of the activities and derivable timelines. However, the plan does not have information about the human and financial resources needed to carry out their actions, compromising their execution by not having resources designated or required for their implementation.
- (b)
Health–National Adaptation Plan (HNAP) to Climate Change in Tanzania 2018–2023
This plan is a good example of the application and adaptation of the guidelines and tools provided by the WHO. This strategic document follows the WHO Guidance for developing HNAPs. The objectives and the adaptation actions programmed in this plan are built by taking, as a base, the ten components of the WHO Operational Framework for building a climate-resilient health system [
34].
It is worth noting that each plan’s action describes its key performance indicator, responsible division or personnel, contributing institutions, and estimated budget. This information helps to monitor their progress and guarantee compliance of the actions with their designated responsibilities and budget.
- (c)
The National Climate Change Health Adaptation Strategy of the Former Yugoslav Republic of Macedonia 2011 (North Macedonia)
This adaptation plan was developed with the help of the WHO Regional Office for Europe in 2011, which was an early start for health adaptation planning. One aspect that stands out is that it does not comprehensively analyse the climate-sensitive health risks. Nevertheless, it counts as an action plan for implementing its adaptation strategy, in which each goal has a set of adaptation actions programmed with a time frame, responsible division or personnel, and indicators for monitoring. It does not have a budget included for the mentioned action plan.
- (d)
Environment and Health Risks from Climate Change and Variability in Italy 2007
Although this is not an adaptation plan, this document is an interesting example of the first approximations of health adaptation planning before the WHO’s guidelines and tools existed. This document was created by the “Italian Agency for Environmental Protection and Technical Services” in joint work with the WHO Regional Office for Europe. It extensively analyses the climate change impacts on health and strategies to reduce them, including mitigation and adaptation measures.
- (2)
Subnational-level Health Adaptation Plans
- (a)
NHS BNSSG Healthier Together Estates Climate Change Adaptation Plan 2021–2025
NHS Bristol, North Somerset, and South Gloucestershire (NHS BNSSG), an Integrated Care Board, is a subnational health organisation which is part of NHS England, the national body for the health system in England. This national-level organisation has still not developed its HAP; however, NHS BNSSG has developed its HAP despite that fact. This case exemplifies a subnational organisation that has developed a HAP without following a national Health Adaptation Plan.
NHS BNSSG starts by recognising the legislation and drivers for climate change adaptation relevant to its regional healthcare system [
35]. Further, it thoroughly analyses the impact on health and its healthcare system, which tries to identify the specific current and future climate-related health risks in its NHS jurisdiction area. On the other hand, this plan is a little weak in its adaptation and resilience solutions since it does not describe clear actions, responsible division or personnel, indicators, and other important aspects, which can make it difficult for this NHS organisation to monitor the implementation of the actions contained in this plan.
- (b)
Queensland Human Health and Wellbeing Climate Change Adaptation Plan 2018
This plan starts with a comprehensive stakeholder engagement process through discussion papers, online surveys, and workshops in order to recognise the current situation in terms of adaptation (such as policy framework and gaps, opportunities, barriers, and others) in Queensland. This produced positive results for the development of the plan since it was noticed that the stakeholders were engaged from the beginning of its creation, performing a detailed stocktaking of available information.
The identified impacts on health and well-being are still insufficient; however, priority adaptation measures were established according to the results obtained from the consultation with the stakeholders. These adaptation measures were developed with some examples of strategies and influencers. Nevertheless, this plan does not indicate programmed activities, budgets, or other factors. Therefore, although this plan has a good engagement process, it still lacks in delivering programmed adaptation actions.
3.1.4. Main Elements Identified in the Existing Health Adaptation Plans
These plans were analysed to identify what elements were included and to differentiate the type of information included in national and subnational-level plans.
Figure 5 shows the main components identified in the existing HAPs.
Accordingly, the main components noticed in these plans were: the current policy framework for health and climate change, impacts of climate change on health, implementation of strategies or adaptation measures, and monitoring and review.
3.1.5. Difference between National- and Subnational-Level Plans
Even though the plans analysed do not belong to the same country context, it was observed that the difference between national and subnational HAPs is founded on the level of detail in each section of the adaptation plans. While the national level recognises general climate change impacts on health and programme actions that have a broad spectrum, the subnational level focuses on specific health impacts, and the actions programmed are more specific than in the national ones.
After analysing guidelines, tools, and existing HAPs, while it is noticed that there is no unique approach for developing HAPs, determining the most critical aspects for a subnational level is necessary for the success of a plan. Recognising the organisation’s current position regarding adaptation, developing comprehensive Vulnerability and Adaptation Assessments, and programming adaptation actions to minimise the effects of climate change are the most critical aspects of a HAP.
3.2. The Phases and Steps for Developing Subnational Health Adaptation Plans
The phases and steps for developing subnational HAPs were determined by taking into consideration (1) WHO Guidelines and Tools, (2) other adaptation planning guidelines, and (3) existing health adaptation plans.
The analysis was performed by applying inductive coding using the software NVivo 10. These codes were grouped into themes according to similarities and the mentioned elements of health adaptation planning as defined by the WHO. The themes identified were the phases, while the codes and sub-codes were the steps and sub-steps.
Figure 6 shows the loop graph with the four phases (themes) adapted, and
Figure 7 presents the steps discerned during the coding process.
The adapted elements for creating HAPs were:
Laying the Groundwork and Addressing Gaps: This phase sets the foundations of the planning process since several aspects need to be defined at the beginning. It includes reviewing the available information from national and subnational organisations about climate change and health [
6], such as adaptation policies, programmes, and data regarding climate-sensitive health risks; engaging stakeholders; evaluating the organisation’s current situation (SWOT and gap analysis); and finding the suitable approaches to address gaps. It is convenient for any organisation to start by taking stock of the information regarding climate change adaptation since it could facilitate the development of their plans (see
Figure 8).
Climate-related Health Risks: Understanding the impacts of climate change on health, healthcare assets, and services is imperative, and this can be achieved by developing a Vulnerability and Adaptation Assessment [
6]. This assessment ensures that the HAP is evidence-based. The V&A involves the recognition of vulnerabilities and climate-sensitive health risks, that is, health outcomes, health systems, and facilities outcomes [
28]. It is a crucial aspect mentioned in most guidelines and tools since elaborating a thorough V&A helps the organisation develop a more detailed and efficient HAP.
The steps of the V&A process, according to the WHO [
30] and represented in
Figure 9, are clarified as follows:
The subnational-level plans reviewed show the recognition of the main climate-sensitive health risks that could impact their health system without detailed information or applying a complicated approach. While the WHO recommends the development of a V&A, it can be challenging for a subnational-level organisation to undertake due to its possible limitations in human and financial resources. Thus, two main steps were considered in this adapted phase: identification of climate-related health risks and vulnerability assessment. Considering existing Climate Change Risks Assessments (CCRAs), or any other kind of vulnerability or risk assessment, and delimiting and deepening its information according to the context of the organisation’s jurisdiction is also an option during this step.
Adaptation Actions: This phase includes the development of an adaptation strategy with its corresponding adaptation actions in order to address the results from the V&A. These actions could be developed considering the components for building climate resilience [
36]. Depending on the context, every programmed action may indicate who is responsible for the implementation, timeframe, performance indicators, and budget and financing options [
6].
Reporting, Monitoring, and Review: The last phase of the health adaptation planning process uses the performance indicators, designated timeframes, and division or people responsible for the actions in order to monitor the fulfilment of the goals and inform the progress of the adaptation [
6]. This also helps with its improvement in the iterative process.
3.3. Discussion
After analysing the guidelines, tools, and examples of Health Adaptation Plans, it was noticed that there are two main aspects to consider while developing them: “structure” and “quality”. Performing the required steps in the structural aspect and applying good criteria for the quality aspect could guarantee a successful HAP.
Regarding the “structural” aspect, a subnational-level plan should contain, as a minimum, policies supporting the health sector’s adaptation process, stakeholders involved in the planning and implementation of the HAP, identified climate-related health risks, programmed feasible adaptation actions outlining responsible personnel, timeframes, and the financial resources needed for carrying out the activities, and monitoring and evaluation for its update and improvement.
Regarding the “quality” aspect, the plan’s success could lie in applying the WHO Quality Criteria. The six topic areas covered in that guideline can help organisations to develop viable, comprehensive, and achievable adaptation plans.
On a different note, regarding the document analysis, even if the WHO guidelines and tools were mainly created to help LDCs, they could be used in subnational-level organisations since their issues while developing a plan are similar to those of LDCs. The framework is equally applicable in different countries at different development stages. However, it might be of specific significance in LDCs since they are particularly vulnerable to the impacts of climate change.
Subnational-level Health Adaptation Plans showed basic information about the impacts of climate change on their health systems and the adaptation measures to address these impacts. Nevertheless, some aspects to guarantee the implementation of those actions, such as financing, timelines, and others, are still lacking in these plans. Adaptation plans should have a minimum level of data to make evidence-based decisions and undertake the activities programmed in the plan.
This research provides insights into the little-explored health adaptation planning process. By analysing guidelines and tools (high-level approaches), this research tailored an approach explicitly designed for subnational organisations, recognising the unique challenges and intricacies faced at the regional level, to boost the health sector’s preparedness and resilience. That is the case of the NHS Greater Glasgow and Clyde, a health board part of NHS Scotland. Interviews with staff of this subnational organisation, as part of wider research, revealed that the day-to-day challenges, lack of expertise and resources in their organisation, and insufficient support from the national government make it difficult to undertake the health adaptation planning process. Although these professionals are eager to formulate their plan, they face distinct financial constraints. Consequently, they are hesitant to commence the development of an adaptation plan, as the absence of a budget for implementation could jeopardise their capacity to establish meaningful adaptation targets.
Subnational organisations serve as the dynamic, hands-on component of the healthcare system, where actions are implemented directly within healthcare assets and services. Thus, promoting and simplifying the development of HAPs at that level is crucial for enhancing the adaptive capacity and increasing the health system’s resilience. This research serves as a step forward in the ongoing pursuit of safeguarding public health in an era of climate uncertainty.
Ultimately, it is necessary to consult with subnational organizations in order to determine the effectiveness of this approach for developing Health Adaptation Plans, to harness real-world expertise and insights, and to ensure that this approach is not only theoretically sound but also practical and capable of delivering positive outcomes that benefit subnational healthcare organisations.
4. Conclusions
The WHO guidelines and tools propose a set of elements and recommendations to develop HAPs that assist countries and make the adaptation planning process more manageable. However, these guidelines can be hard to follow for subnational health organisations due to their limited resources. Thus, they need to be adapted for use in subnational organisations. Moreover, although the documentary analysis of guidelines, tools, and existing HAPs revealed no unique approach for developing HAPs at subnational levels, the synergy and use of these documents could greatly help the adaptation plan’s elaboration. The phases and steps proposed in this study are meant to help organisations with a lack of resources to develop their adaptation plans efficiently and effectively, and national governments can use the proposed approach as part of their policies to assist their subnational levels in developing their plans and standardising the planning within their health organisations.
Aside from the technical aspects, this research’s results had several implications. First, from the meagre information regarding health adaptation planning, adaptation seems to have been put at the end of the health sector’s agenda worldwide. The health sector is essential in climate change adaptation since it cares for people’s lives and health. Because of this, it is necessary for the health sector to be aware of the fact that adaptation must be undertaken now in order to ensure timely responses to the effects of climate change.
The climate change adaptation journey might be full of potholes and bumps. However, proper planning can help make it easier. The most critical aspect is that the organisation develops a HAP in any way or form possible, identifying the climate-related health risks and programming and executing actions to be prepared for the imminent impacts of climate change.