Short Communication: Differences in Levels of Free Amino Acids and Total Protein in Human Foremilk and Hindmilk
Abstract
:1. Introduction
2. Methods
2.1. Subjects
2.2. Milk Collection
2.3. Milk Sample Analysis
2.4. Statistics
2.5. Ethics
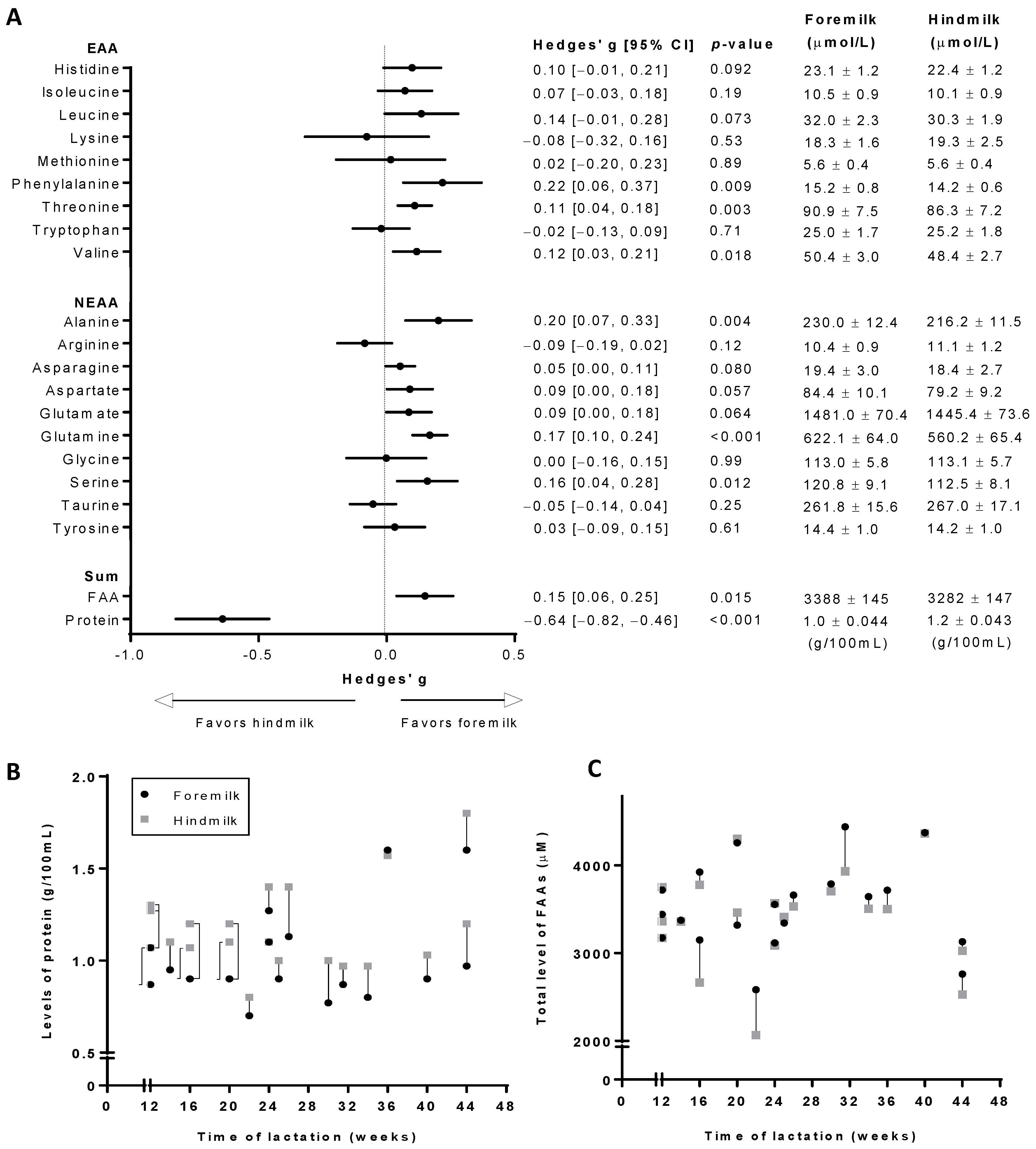
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgements
Conflicts of Interest
References
- Horta, B.L.; Loret de Mola, C.; Victora, C.G. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Lodge, C.J.; Tan, D.J.; Lau, M.X.; Dai, X.; Tham, R.; Lowe, A.J.; Bowatte, G.; Allen, K.J.; Dharmage, S.C. Breastfeeding and asthma and allergies: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 38–53. [Google Scholar] [CrossRef] [PubMed]
- Meijer, C.R.; Discepolo, V.; Troncone, R.; Mearin, M.L. Does infant feeding modulate the manifestation of celiac disease and type 1 diabetes? Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Adelman, A.S.; Rai, D.; Boettcher, J.; Lonnerdal, B. Amino acid profiles in term and preterm human milk through lactation: A systematic review. Nutrients 2013, 5, 4800–4821. [Google Scholar] [CrossRef] [PubMed]
- van Sadelhoff, J.H.J.; van de Heijning, B.J.M.; Stahl, B.; Amodio, S.; Rings, E.; Mearin, M.L.; Garssen, J.; Hartog, A. Longitudinal variation of amino acid levels in human milk and their associations with infant gender. Nutrients 2018, 10, 1233. [Google Scholar] [CrossRef] [PubMed]
- Gidrewicz, D.A.; Fenton, T.R. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014, 14, 216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, S.; Hepworth, A.R.; Prime, D.K.; Lai, C.T.; Trengove, N.J.; Hartmann, P.E. Variation in fat, lactose, and protein composition in breast milk over 24 hours: Associations with infant feeding patterns. J. Hum. Lact. 2013, 29, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Saarela, T.; Kokkonen, J.; Koivisto, M. Macronutrient and energy contents of human milk fractions during the first six months of lactation. Acta Paediatr. 2005, 94, 1176–1181. [Google Scholar] [CrossRef] [PubMed]
- Heon, M.; Goulet, C.; Levy, E.; Nuyt, A.M. Hindmilk: A head start in preterm nutrition. Enferm. Clin. 2009, 19, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Slusher, T.; Hampton, R.; Bode-Thomas, F.; Pam, S.; Akor, F.; Meier, P. Promoting the exclusive feeding of own mother’s milk through the use of hindmilk and increased maternal milk volume for hospitalized, low birth weight infants (<1800 grams) in nigeria: A feasibility study. J. Hum. Lact. 2003, 19, 191–198. [Google Scholar] [PubMed]
- Nielsen, S.D.; Beverly, R.L.; Dallas, D.C. Peptides released from foremilk and hindmilk proteins by breast milk proteases are highly similar. Front. Nutr. 2017, 4, 54. [Google Scholar] [CrossRef] [PubMed]
- Fusch, G.; Rochow, N.; Choi, A.; Fusch, S.; Poeschl, S.; Ubah, A.O.; Lee, S.Y.; Raja, P.; Fusch, C. Rapid measurement of macronutrients in breast milk: How reliable are infrared milk analyzers? Clin. Nutr. 2015, 34, 465–476. [Google Scholar] [CrossRef] [PubMed]
- Bishara, R.; Dunn, M.S.; Merko, S.E.; Darling, P. Nutrient composition of hindmilk produced by mothers of very low birth weight infants born at less than 28 weeks’ gestation. J. Hum. Lact. 2008, 24, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Dorea, J.G.; Horner, M.R.; Bezerra, V.L.; Campanate, M.L. Variation in major constituents of fore- and hindmilk of brazilian women. J. Trop. Pediatr. 1982, 28, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Hall, B. Uniformity of human milk. Am. J. Clin. Nutr. 1979, 32, 304–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neville, M.C.; Keller, R.P.; Seacat, J.; Casey, C.E.; Allen, J.C.; Archer, P. Studies on human lactation. I. Within-feed and between-breast variation in selected components of human milk. Am. J. Clin. Nutr. 1984, 40, 635–646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, M.R.; Chan, G.M.; Book, L.S. Comparison of macronutrient concentration of preterm human milk between two milk expression techniques and two techniques for quantitation of energy. J. Pediatr. Gastroenterol. Nutr. 1986, 5, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Valentine, C.J.; Hurst, N.M.; Schanler, R.J. Hindmilk improves weight gain in low-birth-weight infants fed human milk. J. Pediatr. Gastroenterol. Nutr. 1994, 18, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Demers-Mathieu, V.; Nielsen, S.D.; Underwood, M.A.; Borghese, R.; Dallas, D.C. Analysis of milk from mothers who delivered prematurely reveals few changes in proteases and protease inhibitors across gestational age at birth and infant postnatal age. J. Nutr. 2017, 147, 1152–1159. [Google Scholar] [CrossRef] [PubMed]
- Khaldi, N.; Vijayakumar, V.; Dallas, D.C.; Guerrero, A.; Wickramasinghe, S.; Smilowitz, J.T.; Medrano, J.F.; Lebrilla, C.B.; Shields, D.C.; German, J.B. Predicting the important enzymes in human breast milk digestion. J. Agric. Food Chem. 2014, 62, 7225–7232. [Google Scholar] [CrossRef] [PubMed]
- Dallas, D.C.; German, J.B. Enzymes in human milk. Nestle Nutr. Inst. Workshop Ser. 2017, 88, 129–136. [Google Scholar] [PubMed]
- Canadian Medical Association. Nutrient needs and feeding of premature infants. Nutrition committee, Canadian paediatric society. Can. Med. Assoc. J. 1995, 152, 1765–1785. [Google Scholar]
- Underwood, M.A. Human milk for the premature infant. Pediatr. Clin. North Am. 2013, 60, 189–207. [Google Scholar] [CrossRef] [PubMed]
- Ogechi, A.A.; William, O.; Fidelia, B.T. Hindmilk and weight gain in preterm very low-birthweight infants. Pediatr. Int. 2007, 49, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Hay, W.W.; Thureen, P. Protein for preterm infants: How much is needed? How much is enough? How much is too much? Pediatr. Neonatol. 2010, 51, 198–207. [Google Scholar] [CrossRef]
- Bernt, K.M.; Walker, W.A. Human milk as a carrier of biochemical messages. Acta Paediatr. 1999, 88, 27–41. [Google Scholar] [CrossRef]
- Briassouli, E.; Briassoulis, G. Glutamine randomized studies in early life: The unsolved riddle of experimental and clinical studies. Clin. Dev. Immunol. 2012, 2012, 749189. [Google Scholar] [CrossRef] [PubMed]
- Sarwar, G.; Botting, H.G.; Davis, T.A.; Darling, P.; Pencharz, P.B. Free amino acids in milks of human subjects, other primates and non-primates. Br. J. Nutr. 1998, 79, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Cruzat, V.; Macedo Rogero, M.; Noel Keane, K.; Curi, R.; Newsholme, P. Glutamine: Metabolism and immune function, supplementation and clinical translation. Nutrients 2018, 10, 1564. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.M.; Caspi, R.R. Glutamate joins the ranks of immunomodulators. Nat. Med. 2010, 16, 856–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganor, Y.; Levite, M. Glutamate in the Immune System: Glutamate Receptors in Immune Cells, Potent Effects, Endogenous Production and Involvement in Disease. Nerve-Driven Immunity: Neurotransmitters and Neuropeptides in the Immune System; Springer: Vienna, Austria, 2012; pp. 121–161. [Google Scholar]
- Roth, E. Nonnutritive effects of glutamine. J. Nutr. 2008, 138, 2025s–2031s. [Google Scholar] [CrossRef] [PubMed]
- Ruth, M.R.; Field, C.J. The immune modifying effects of amino acids on gut-associated lymphoid tissue. J. Anim. Sci. Biotechnol. 2013, 4, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blachier, F.; Boutry, C.; Bos, C.; Tome, D. Metabolism and functions of l-glutamate in the epithelial cells of the small and large intestines. Am. J. Clin. Nutr. 2009, 90, 814s–821s. [Google Scholar] [CrossRef] [PubMed]
- Jiao, N.; Wu, Z.; Ji, Y.; Wang, B.; Dai, Z.; Wu, G. l-glutamate enhances barrier and antioxidative functions in intestinal porcine epithelial cells. J. Nutr. 2015, 145, 2258–2264. [Google Scholar] [CrossRef] [PubMed]
- Rao, R.; Samak, G. Role of glutamine in protection of intestinal epithelial tight junctions. J. Epithel. Biol. Pharmacol. 2012, 5, 47–54. [Google Scholar] [PubMed]
- Rook, D.; Te Braake, F.W.; Schierbeek, H.; Longini, M.; Buonocore, G.; Van Goudoever, J.B. Glutathione synthesis rates in early postnatal life. Pediatr. Res. 2010, 67, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.H.; Kim, H. The roles of glutamine in the intestine and its implication in intestinal diseases. Int. J. Mol. Sci. 2017, 18. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.M.; Wu, G.; Galanko, J.A.; Chen, W.; Maynor, A.R.; Bose, C.L.; Rhoads, J.M. Reduced serum amino acid concentrations in infants with necrotizing enterocolitis. J. Pediatr. 2000, 137, 785–793. [Google Scholar] [CrossRef] [PubMed]
- van der Hulst, R.R.; von Meyenfeldt, M.F.; Soeters, P.B. Glutamine: An essential amino acid for the gut. Nutrition 1996, 12, S78–S81. [Google Scholar] [CrossRef]
- van Elburg, R.M.; Fetter, W.P.; Bunkers, C.M.; Heymans, H.S. Intestinal permeability in relation to birth weight and gestational and postnatal age. Arch. Dis. Child. Fetal Neonatal Edit. 2003, 88, F52–F55. [Google Scholar] [CrossRef]
- Weaver, L.T.; Laker, M.F.; Nelson, R. Intestinal permeability in the newborn. Arch. Dis. Child. 1984, 59, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Shao, X.M.; Neu, J. Immunonutrients and neonates. Eur. J. Pediatr. 2003, 162, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Neu, J. Glutamine in the fetus and critically ill low birth weight neonate: Metabolism and mechanism of action. J. Nutr. 2001, 131, 2585S–2589S. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Sadelhoff, J.H.J.; Mastorakou, D.; Weenen, H.; Stahl, B.; Garssen, J.; Hartog, A. Short Communication: Differences in Levels of Free Amino Acids and Total Protein in Human Foremilk and Hindmilk. Nutrients 2018, 10, 1828. https://doi.org/10.3390/nu10121828
Van Sadelhoff JHJ, Mastorakou D, Weenen H, Stahl B, Garssen J, Hartog A. Short Communication: Differences in Levels of Free Amino Acids and Total Protein in Human Foremilk and Hindmilk. Nutrients. 2018; 10(12):1828. https://doi.org/10.3390/nu10121828
Chicago/Turabian StyleVan Sadelhoff, Joris H. J., Dimitra Mastorakou, Hugo Weenen, Bernd Stahl, Johan Garssen, and Anita Hartog. 2018. "Short Communication: Differences in Levels of Free Amino Acids and Total Protein in Human Foremilk and Hindmilk" Nutrients 10, no. 12: 1828. https://doi.org/10.3390/nu10121828
APA StyleVan Sadelhoff, J. H. J., Mastorakou, D., Weenen, H., Stahl, B., Garssen, J., & Hartog, A. (2018). Short Communication: Differences in Levels of Free Amino Acids and Total Protein in Human Foremilk and Hindmilk. Nutrients, 10(12), 1828. https://doi.org/10.3390/nu10121828




