Assessment of Dietary Iodine Intake in School Age Children: The Cross-Sectional ANIVA Study
Abstract
1. Introduction
2. Methods
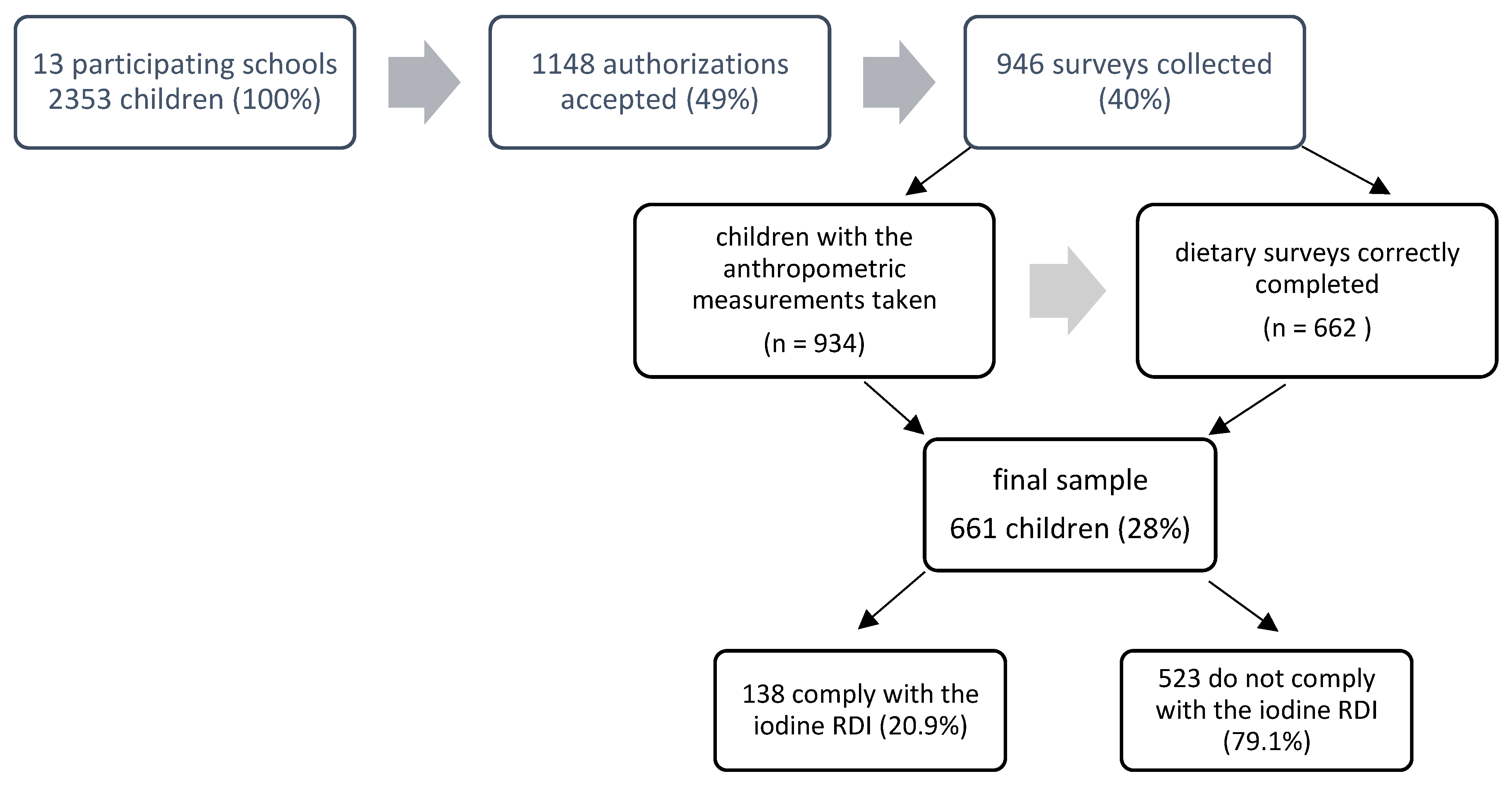
2.1. Population and Sample
2.2. Anthropometric Measures
2.3. Diet Assessment
2.4. Physical Activity
2.5. Socio-Educational Level
2.6. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ma, Z.F.; Skeaff, S.A. Iodine Deficiency Disorders and Their Elimination; Springer International Publishing: Cham, Switzerland, 2017. [Google Scholar]
- Zimmermann, M.B. Iodine Deficiency. Endocr. Rev. 2009, 30, 376–408. [Google Scholar] [CrossRef] [PubMed]
- Wayne, E.J.; Koutras, D.A. Clinical Aspects of Iodine Metabolism; Blackwell Scientific Publications: Oxford, UK, 1964. [Google Scholar]
- Andersson, M.; Takkouche, B.; Egli, I.; Allen, H.E.; Benoist, B.D. Current Global Iodine Status and Progress Over the Last Decade Towards the Elimination of Iodine Deficiency. Bull. World Health Organ. 2005, 83, 518–525. [Google Scholar] [PubMed]
- World Health Organization. Assessment of Iodine Deficiency Disorders and Monitoring their Elimination: A Guide for Programme Managers; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Laurberg, P.; Nøhr, S.; Pedersen, K.; Hreidarsson, A.; Andersen, S.; Pedersen, I.B.; Knudsen, N.; Perrild, H.; Jørgensen, T.; Ovesen, L. Thyroid Disorders in Mild Iodine Deficiency. Thyroid 2000, 10, 951–963. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. The Role of Iodine in Human Growth and Development. Semin. Cell Dev. Biol. 2011, 26, 645–652. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Sustaining the Elimination of Iodine Deficiency Disorders (IDD); World Health Organization: Geneva, Switzerland, 2005; Volume 6. [Google Scholar]
- Remer, T.; Johner, S.A.; Gartner, R.; Thamm, M.; Kriener, E. Iodine Deficiency in Infancy—A Risk for Cognitive Development. Dtsch. Med. Wochenschr. 2010, 135, 1551–1556. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.N. Iodine Deficiency in Children. Endocr. Dev. 2014, 26, 130–138. [Google Scholar] [PubMed]
- Tarim, O. Thyroid Hormones and Growth in Health and Disease. J. Clin. Res. Pediatr. Endocrinol. 2011, 3, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Rivkees, S.A.; Bode, H.H.; Crawford, J.D. Long-Term Growth in Juvenile Acquired Hypothyroidism. N. Engl. J. Med. 1988, 318, 599–602. [Google Scholar] [CrossRef] [PubMed]
- Abu, E.O.; Bord, S.; Horner, A.; Chatterjee, V.; Compston, J. The Expression of Thyroid Hormone Receptors in Human Bone. Bone 1997, 21, 137–142. [Google Scholar] [CrossRef]
- Bassett, J.D.; Williams, G.R. Critical Role of the Hypothalamic-pituitary-thyroid Axis in Bone. Bone 2008, 43, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Iodine Global Network (IGN). Two Decades of Progress against Iodine Deficiency: 1993–2015; IGN: Ottawa, ON, Canada, 2016; Volume 2017. [Google Scholar]
- Ma taix Verdú, J.; Nutrición, Y. Alimentación Humana. II. Situaciones Fisiológicas Y Patológicas, 2nd ed.; Ergon: Madrid, Spain, 2009. [Google Scholar]
- Vila, L. Avances En La Erradicación De La Deficiencia De Yodo En España. Endocrinología Nutrición 2010, 57, 87–89. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Child Growth Standards: Length/Height-for-Age. Weight-for-Age. Weight-for-Length. Weight-for-Height and Body Mass Index for Age; World Health Organization: Geneva, Switzerland, 2006; Volume 2018. [Google Scholar]
- Cuervo, M.; Abete, I.; Baladia, E.; Corbalan, M.; Manera, M.; Basulto, J.; Martinez, A. Ingestas Dietéticas De Referencia (IDR) Para La Población Española; EUNSA/Astrolabio: Pamplona, Spain, 2010. [Google Scholar]
- Trumbo, P.; Yates, A.A.; Schlicker, S.; Poos, M. Dietary reference intakes: vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. J. Am. Diet. Assoc. 2001, 101, 294–301. [Google Scholar] [CrossRef]
- Arrizabalaga, J.J.; Jalón, M.; Espada, M.; Cañas, M.; Arena, J.M.; Vila, L. Estado De Nutrición De Yodo Y Prevalencia De Concentraciones Anormales De TSH En La Población Escolar De 6-7 Años De La Comunidad Autónoma Del País Vasco. Endocrinol. Diabetes Nutr. 2018, 65, 245–310. [Google Scholar] [CrossRef] [PubMed]
- Soldin, O.P. Controversies in Urinary Iodine Determinations. Clin. Biochem. 2002, 35, 575–579. [Google Scholar] [CrossRef]
- World Health Organization; International Council for Control of Iodine Deficiency Disorders; UNICEF. Indicators for Assessing Iodine Deficiency Disorders and their Control through Salt Iodization; World Health Organization: Geneva, Switzerland, 1994. [Google Scholar]
- Stanbury, J.B.; Hetzel, B.S. Endemic Goiter and Endemic Cretinism; Iodine Nutrition in Health and Disease; Wiley: New York, NY, USA, 1980. [Google Scholar]
- Rasmussen, L.B.; Ovesen, L.; Christiansen, E. Day-to-Day and within-Day Variation in Urinary Iodine Excretion. Eur. J. Clin. Nutr. 1999, 53, 401. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Moon, S.J.; Kim, K.R.; Sohn, C.Y.; Oh, J.J. Dietary Iodine Intake and Urinary Iodine Excretion in Normal Korean Adults. Yonsei Med. J. 1998, 39, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Dunn, J.T.; Haar, F.V.D. A Practical Guide to the Correction of Iodine Deficiency; International Council for Control of Iodine Deficiency Disorders: The Hague, The Netherlands, 1990; Volume 3. [Google Scholar]
- Bert, R.C.; Mora, J.M.; Salud, J.P.; Farran, R.A. Estudio De Prevalencia De La Deficiencia De Yodo En Una Población Escolarizada De 6 Años. Anales Pediatría 2010, 72, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Arrizabalaga, J.J.; Larrañaga, N.; Espada, M.; Amiano, P.; Bidaurrazaga, J.; Latorre, K.; Gorostiza, E. Evolución Del Estado De Nutrición De Yodo En Los Escolares De La Comunidad Autónoma Del País Vasco. Endocrinol. Nutr. 2012, 59, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Roig, B.P.; Herráez, N.A.; Alfaro, A.M.; Rigual, F.C.; Moreno, S.S. Bocio Endémico Y Déficit De Yodo: ¿sigue Siendo Una Realidad En España? Anales Pediatría 2006, 65, 234–240. [Google Scholar] [CrossRef]
- Cantalapiedra, A.Z.; Pérez, L.R.; López, L.S.; Serrano, F.S.; Guerra, R.A.; Sánchez-Paya, J.; Alfonso, A.P.; Serrano, J.F. Situación Nutricional De Yodo En La Población Escolar De Alicante. Anales Pediatría 2007, 66, 260–266. [Google Scholar] [CrossRef]
- Vila, L.; Donnay, S.; Arena, J.; Arrizabalaga, J.; Pineda, J.; Garcia-Fuentes, E.; García-Rey, C.; Marín, J.; Serra-Prat, M.; Velasco, I. Iodine Status and Thyroid Function among Spanish Schoolchildren Aged 6–7 Years: The Tirokid Study. Br. J. Nutr. 2016, 115, 1623–1631. [Google Scholar] [CrossRef] [PubMed]
- Ballester, L.V.; Candil, S.D.; Reymunde, T.I.; Escofet, F.S.; Henzi, F.T.; Jaramillo, S.T.; Alcázar, J.; Tapias, M.J.; Torres, Y.; Puig-Domingo, M. Evaluación De Los Hábitos Alimentarios Relacionados Con La Ingesta De Yodo. El Estado Nutricional De Yodo Y Disfunción Tiroidea En Cuatro Poblaciones no Seleccionadas (Proyecto Tirobus). Endocrinol. Nutr. 2010, 57, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad Servicios Sociales e Igualdad. Recomendaciones Sobre Actividad Física. Sedentarismo Y Tiempo De Pantalla. 2015, 2018. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/Estrategia/docs/Tabla_resumen_Recomendaciones_ActivFisica.pdf (accessed on 11 April 2018).
- Sociedad Española de Nutrición Comunitaria. Pirámide De Alimentación Saludable. 2015, 2018. Available online: http://www.nutricioncomunitaria.org/es/noticia/piramide-de-la-alimentacion-saludable-senc-2015 (accessed on 11 April 2018).
- Goindi, G.; Karmarkar, M.; Kapil, U.; Jagannathan, J. Estimation of Losses of Iodine during Different Cooking Procedures. Asia Pac. J. Clin. Nutr. 1995, 4, 225–227. [Google Scholar] [PubMed]
- Arrizabalaga, J.J.; Jalón, M.; Espada, M.; Cañas, M.; Latorre, P.M. Concentración De Yodo En La Leche Ultrapasteurizada De Vaca. Aplicaciones En La Práctica Clínica Y En La Nutrición Comunitaria. Med. Clin. 2015, 145, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Real Decreto 1424/1983. De 27 De Abril. Por El Que Se Aprueba La Reglamentación Técnico-Sanitaria Para La Obtención. Circulación Y Venta De La Sal Y Salmueras Comestibles. (BOE Núm. 130. De 1 De Junio De 1983). 1983. Available online: https://www.boe.es/boe/dias/1983/06/01/pdfs/A15261-15264.pdf (accessed on 31 May 2018).
| Variables | RDI Compliant (n = 138; 20.9%) | RDI Non-Compliant (n = 523; 79.1%) | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys (n = 69; 50%) | Girls (n = 69; 50%) | p-Value (Boys vs. Girls) | Boys (n = 229; 43.8%) | Girls (n = 294; 56.2%) | p-Value (Boys vs. Girls) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| Age (years) | 7.5 | 1.1 | 7.5 | 1.1 | 0.917 | 7.5 | 1.1 | 7.6 | 1.1 | 0.350 | 0.642 |
| Weight (kg) | 29.9 | 7.2 | 29.8 | 7.2 | 0.928 | 30.7 | 8.2 | 31.2 | 8.5 | 0.508 | 0.126 |
| Height (m) | 1.3 | 0.1 | 1.3 | 0.1 | 1 | 1.3 | 0.1 | 1.3 | 0.1 | 1 | 0.493 |
| Weight z-score | 0.9 | 1.1 | 0.7 | 1.0 | 0.345 | 1.0 | 1.2 | 1.0 | 1.2 | 0.634 | 0.141 |
| Height z-score | 0.7 | 1.0 | 0.5 | 1.1 | 0.321 | 0.7 | 1.0 | 0.7 | 1.1 | 0.831 | 0.353 |
| BMI z-score | 0.8 | 1.2 | 0.7 | 1.0 | 0.677 | 0.8 | 1.4 | 0.8 | 1.4 | 1 | 0.364 |
| Mothers’ educational level (%) | |||||||||||
| Low | 17.5 | 13.0 | 0.477 | 21.8 | 26.5 | 0.215 | 0.061 | ||||
| Average | 42.0 | 42.0 | 1 | 45.5 | 37.8 | 0.077 | 0.368 | ||||
| High | 40.5 | 44.9 | 0.605 | 32.7 | 35.7 | 0.479 | 0.255 | ||||
| Fathers’ educational level (%) | |||||||||||
| Low | 37.7 | 36.2 | 0.860 | 41.5 | 38.1 | 0.431 | 0.789 | ||||
| Average | 40.6 | 43.5 | 0.730 | 38.9 | 38.4 | 0.920 | 0.882 | ||||
| High | 21.7 | 20.3 | 0.834 | 19.7 | 23.5 | 0.293 | 0.755 | ||||
| Level of physical activity (%) | |||||||||||
| Inadequate | 36.2 | 47.8 | 0.167 | 40.2 | 56.1 | 0.001 | 0.006 | ||||
| Adequate | 63.8 | 52.2 | 0.167 | 59.8 | 43.9 | 0.001 | 0.001 | ||||
| Nutrients | RDIs | RDI Compliant (n = 138; 20.9%) | RDI Non-Compliant (n = 523; 79.1%) | p-Value (Total) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys (n = 69; 50%) | Girls (n = 69; 50%) | p-Value (Boys vs. Girls) | Boys (n = 229; 73.8%) | Girls (n = 294; 56.2%) | p-Value (Boys vs. Girls) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| Iodine (μg) | <EAR | 174.9 | 168.2 | 149.8 | 34.4 | 0.227 | 87.9 | 18.7 | 85.5 | 13.8 | 0.013 | 0.001 |
| Iodine (μg) | <EAR | 138.0 * | 33.0 ** | 136.0 * | 35.0 ** | 0.620 | 88.0* | 25.0 ** | 85.3 * | 30.0 ** | 0.069 *** | 0.001 |
| Total energy (kcal) | <EAR | 2587.3 | 401.9 | 2533.6 | 504.0 | 0.760 | 2204.8 | 383.6 | 2071.6 | 363.2 | 0.001 | 0.001 |
| Proteins (g) | >EAR | 113.5 | 18.5 | 110.6 | 24.3 | 0.433 | 89.6 | 22.6 | 84.5 | 20.7 | 0.006 | 0.001 |
| Carbohydrates (g) | <EAR | 257.9 | 47.4 | 248.4 | 60.9 | 0.307 | 228.5 | 39.5 | 210.2 | 37.7 | 0.001 | 0.001 |
| Fat (g) | >EAR | 117.9 | 24.3 | 118.1 | 24.4 | 0.950 | 99.4 | 23.1 | 95.56 | 23.6 | 0.062 | 0.001 |
| Cholesterol (mg) | >EAR | 433.7 | 119.6 | 434.8 | 109.7 | 0.955 | 320.6 | 101.5 | 299.6 | 93.6 | 0.014 | 0.001 |
| Dietary fiber (g) | <AI | 20.2 | 5.7 | 19.0 | 5.4 | 0.190 | 18.2 | 10.9 | 16.7 | 5.3 | 0.039 | 0.003 |
| Vitamin B1 (mg) | <EAR | 1.7 | 0.5 | 1.7 | 0.8 | 0.857 | 1.5 | 0.5 | 1.4 | 0.5 | 0.101 | 0.001 |
| Vitamin B2 (mg) | <EAR | 2.3 | 0.6 | 2.5 | 2.4 | 0.410 | 1.9 | 0.5 | 1.7 | 0.5 | 0.001 | 0.001 |
| Niacin (mg) | <EAR | 46.0 | 9.8 | 43.9 | 10.8 | 0.244 | 34.7 | 9.2 | 32.9 | 8.3 | 0.013 | 0.001 |
| Vitamin B6 (mg) | <EAR | 2.5 | 0.7 | 2.7 | 2.4 | 0.396 | 2.1 | 0.6 | 2.0 | 0.6 | 0.044 | 0.001 |
| Folic acid (μg) | <EAR | 282.5 | 94.6 | 280.4 | 94.6 | 0.893 | 237.9 | 78.3 | 226.5 | 80.9 | 0.105 | 0.001 |
| Vitamin B12 (μg) | <EAR | 8.2 | 3.6 | 7.9 | 3.4 | 0.582 | 6.8 | 7.5 | 5.8 | 3.2 | 0.041 | 0.001 |
| Vitamin C | <EAR | 113.0 | 53.1 | 114.3 | 60.3 | 0.891 | 100.5 | 50.3 | 90.3 | 43.4 | 0.012 | 0.001 |
| Biotin (μg) | <EAR | 35.1 | 8.8 | 33.8 | 8.0 | 0.345 | 28.2 | 10.3 | 25.6 | 8.6 | 0.001 | 0.001 |
| Ac. Pantothenic (mg) | <EAR | 6.8 | 1.1 | 6.8 | 1.7 | 0.966 | 5.6 | 1.4 | 5.1 | 1.3 | 0.001 | 0.001 |
| Vitamin A (μg) | <EAR | 1174.4 | 599.0 | 1246.2 | 888.1 | 0.578 | 1113.5 | 1454.8 | 864.0 | 437.9 | 0.005 | 0.011 |
| Vitamin D (μg) | <EAR | 4.4 | 2.7 | 4.6 | 3.7 | 0.742 | 3.2 | 3.5 | 3.2 | 2.4 | 0.969 | 0.001 |
| Vitamin E (mg) | <EAR | 10.6 | 3.5 | 10.0 | 4.1 | 0.374 | 8.0 | 2.9 | 7.9 | 3.1 | 0.908 | 0.001 |
| Calcium (mg) | <EAR | 1166.4 | 234.2 | 1187.1 | 378.6 | 0.699 | 926.1 | 226.4 | 873.2 | 229.9 | 0.008 | 0.001 |
| Iron (mg) | <EAR | 15.8 | 5.2 | 15.1 | 4.6 | 0.405 | 13.3 | 4.8 | 12.3 | 3.9 | 0.010 | 0.001 |
| Magnesium (mg) | <AI | 343.4 | 77.5 | 338.9 | 79.9 | 0.736 | 276.2 | 74.4 | 263.5 | 60.2 | 0.031 | 0.001 |
| Zinc (mg) | <EAR | 11.3 | 1.8 | 11.0 | 2.5 | 0.471 | 9.3 | 2.4 | 8.8 | 2.1 | 0.004 | 0.001 |
| Selenium (mg) | <EAR | 154.5 | 39.3 | 143.6 | 40.6 | 0.111 | 107.3 | 30.1 | 103.9 | 28.9 | 0.080 | 0.001 |
| Sodium (mg) | <EAR | 2921.7 | 733.8 | 2945.4 | 1060.7 | 0.878 | 2209.0 | 737.7 | 2054.3 | 637.6 | 0.010 | 0.001 |
| Potassium (mg) | <EAR | 3356.8 | 544.4 | 3396.8 | 797.3 | 0.731 | 2725.5 | 621.2 | 2684.0 | 2088.8 | 0.771 | 0.001 |
| Fluoride (μg) | <AI | 376.3 | 297.9 | 344.0 | 195.6 | 0.453 | 335.1 | 317.8 | 321.6 | 289.2 | 0.610 | 0.243 |
| Phosphorus (mg) | <EAR | 1800.8 | 275.5 | 1808.5 | 390.9 | 0.894 | 1415.3 | 269.6 | 1327.4 | 285.1 | 0.001 | 0.001 |
| Consumption of Fish and Dairy Products | RDI Compliant (n = 138; 20.9%) | RDI non-Compliant (n = 523; 79.1%) | p-Value (Compliant Boys vs. Non-Compliant Boys) | p-Value (Compliant Girls vs. Non-Compliant Girls) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Boys (n = 69; 50%) | Girls (n = 69; 50%) | p-Value (Compliant vs. Non-Compliant) | Boys (n =229; 73.8%) | Girls (n = 294; 56.2%) | p-Value (Compliant vs. Non-Compliant | ||||
| % | % | % | % | ||||||
| Regular consumption of fish (at least 2 or 3 times / week) | Compliant | 20.3 | 15.9 | 0.659 | 19.2 | 21.1 | 0.661 | 0.843 | 0.337 |
| Non-compliant | 79.7 | 84.1 | 80.8 | 78.9 | |||||
| Consumption of dairy products at breakfast | Compliant | 8.7 | 4.3 | 0.493 | 3.1 | 6.1 | 0.147 | 0.094 | 0.778 |
| Non-compliant | 91.3 | 95.7 | 96.9 | 93.9 | |||||
| Consumption 2 yogurts and / or 40 g of cheese per day | Compliant | 30.4 | 29.0 | 1.000 | 19.7 | 23.8 | 0.288 | 0.058 | 0.370 |
| Non-compliant | 69.6 | 71.0 | 80.3 | 76.2 | |||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morales-Suárez-Varela, M.; Peraita-Costa, I.; Llopis-Morales, A.; Llopis-Gonzalez, A. Assessment of Dietary Iodine Intake in School Age Children: The Cross-Sectional ANIVA Study. Nutrients 2018, 10, 1884. https://doi.org/10.3390/nu10121884
Morales-Suárez-Varela M, Peraita-Costa I, Llopis-Morales A, Llopis-Gonzalez A. Assessment of Dietary Iodine Intake in School Age Children: The Cross-Sectional ANIVA Study. Nutrients. 2018; 10(12):1884. https://doi.org/10.3390/nu10121884
Chicago/Turabian StyleMorales-Suárez-Varela, María, Isabel Peraita-Costa, Agustín Llopis-Morales, and Agustín Llopis-Gonzalez. 2018. "Assessment of Dietary Iodine Intake in School Age Children: The Cross-Sectional ANIVA Study" Nutrients 10, no. 12: 1884. https://doi.org/10.3390/nu10121884
APA StyleMorales-Suárez-Varela, M., Peraita-Costa, I., Llopis-Morales, A., & Llopis-Gonzalez, A. (2018). Assessment of Dietary Iodine Intake in School Age Children: The Cross-Sectional ANIVA Study. Nutrients, 10(12), 1884. https://doi.org/10.3390/nu10121884





