Association between Adherence to the Japanese Food Guide Spinning Top and Sleep Quality in College Students
Abstract
1. Introduction
2. Methods
2.1. Study Participants
2.2. Assessment
2.3. Statistical Analysis
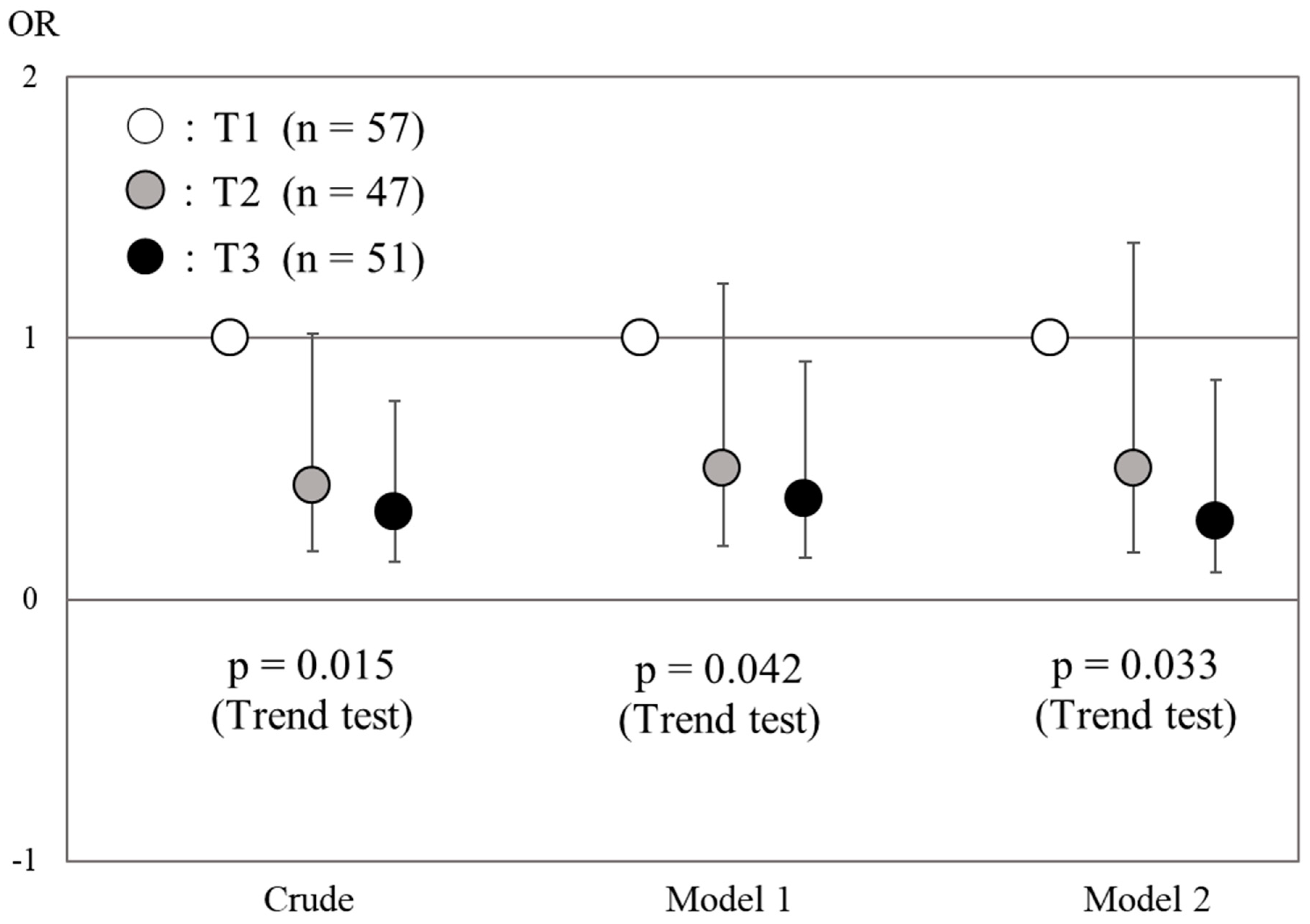
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ministry of Health, Labour and Welfare. Sleep Guidelines for Health Promotion 2014. Available online: http://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000047221.pdf (accessed on 28 October 2017).
- Suga, S.; Watabe, H.; Sakamaki, M.; Hasizume, M.; Tsuboi, K. Workers Sleep Quality and Psychological Factors as Determined by Shift System. Jpn. J. Psychosom. Med. 2006, 46, 293–300. [Google Scholar]
- Ministry of Health, Labour and Welfare. The Japan National Health and Nutrition Survey (NHNS). 2015. Available online: http://www.e-stat.go.jp/SG1/estat/GL08020103.do?_toGL08020103_&listID=000001 176863&requestSender=dsearch (accessed on 28 December 2017).
- NHK Broadcasting Culture Research Institute. NHK’s National Time Use Survey. Available online: https://www.nhk.or.jp/bunken/research/yoron/20160217_1.html (accessed on June 6 2018).
- Steptoe, A.; Peacey, V.; Wardle, J. Sleep duration and health in young adults. Arch. Intern. Med. 2006, 166, 1689–1692. [Google Scholar] [CrossRef] [PubMed]
- Yamamono, R.; Nomura, S. A study of sleep problems in undergraduates using Pittsburgh sleep quality index. Jpn. J. Psychosom. Med. 2009, 49, 817–825. [Google Scholar]
- Fukuda, K.; Ishihara, K. Age-related changes of sleeping pattern during adolescence. Psychiatry Clin. Neurosci. 2001, 55, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Oginska, H.; Pokorski, J. Fatigue and mood correlates of sleep length in three age-social groups: School children, students, and employees. Chronobiol. Int. 2006, 23, 1317–1328. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000, 97, 165–172. [Google Scholar] [CrossRef]
- Garaulet, M.; Ortega, F.; Ruiz, J.; Rey-Lopez, J.P.; Beghin, L.; Manios, Y.; Cuenca-Garcia, M.; Plada, M.; Diethelm, K.; Kafatos, A.; et al. Short sleep duration is associated with increased obesity markers in European adolescents: Effect of physical activity and dietary habits. The HELENA study. Int. J. Obes. 2011, 35, 1308–1317. [Google Scholar] [CrossRef]
- Tamakoshi, A.; Ohno, Y. Self-reported sleep duration as a predictor of all-cause mortality: Results from the JACC study, Japan. Sleep 2004, 27, 51–54. [Google Scholar]
- Hoevenaar-Blom, M.; Spijkerman, A.; Kromhout, D.; van den Berg, J.F.; Verschuren, W.M. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: The MORGEN study. Sleep 2011, 34, 1487–1492. [Google Scholar] [CrossRef]
- Shiraiwa, K.; Murata, S.; Horie, J.; Murata, J.; Miyazaki, J. Relationship between Sleep and Quality of Life in Elderly Community Residents. Japanese Journal of Health Promotion and Physical Therapy 2013, 3, 103–107. [Google Scholar] [CrossRef]
- Osada, Y. Effects of noise on sleep. J. INCE Jpn. 1985, 9, 248–253. [Google Scholar]
- Tsuzuki, K. Effects of thermal environment on human sleep and thermoregulation. Jpn. J. Biometeorol. 2014, 50, 125–134. [Google Scholar]
- Rubio-Arias, J.; Marin-Cascales, E.; Ramos-Campo, D.; Hernandez, A.V.; Pérez-López, F.R. Effect of exercise on sleep quality and insomnia in middle-aged women: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2017, 100, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, R.; Asakura, K.; Kobayashi, S.; Suga, H.; Sasaki, S. Low intake of vegetables, high intake of confectionary, and unhealthy eating habits are associated with poor sleep quality among middle-aged female Japanese workers. J. Occup. Health 2014, 56, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, S.E.; Martinez, C.; Oriol, R.A.; Yanez, D.; Castañeda, B.; Sanchez, E.; Gelaye, B.; Williams, M.A. Sleep quality, sleep patterns and consumption of energy drinks and other caffeinated beverages among peruvian college students. Health 2013, 5, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Kurotani, K.; Kochi, T.; Nanri, A.; Eguchi, M.; Kuwahara, K.; Tsuruoka, H.; Akter, S.; Ito, R.; Pham, N.M.; Kabe, I.; et al. Dietary patterns and sleep symptoms in Japanese workers: The furukawa nutrition and health study. Sleep Med. 2015, 16, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Ocke, M.C. Evaluation of methodologies for assessing the overall diet: dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef]
- Kuriyama, N.; Murakami, K.; Livingstone, M.B.E.; Okubo, H.; Kobayashi, S.; Suga, H.; Sasaki, S. Development of a food-based diet quality score for Japanese: associations of the score with nutrient intakes in young, middle-aged and older Japanese women. J. Nutr. Sci. 2016, 5, 1–11. [Google Scholar] [CrossRef]
- Sakai, H.; Murakami, K.; Kobayashi, S.; Suga, H.; Sasaki, S. Food-based diet quality score in relation to depressive symptoms in young and middle-aged Japanese women. Br. J. Nutr. 2017, 117, 1674–1681. [Google Scholar] [CrossRef]
- Kurotani, K.; Akter, S.; Kashino, I.; Goto, A.; Mizoue, T.; Noda, M.; Sasazuki, S.; Sawada, N.; Tsugane, S. Quality of diet and mortality among Japanese men and women: Japan public health center based prospective study. BMJ 2016, 352, 1–11. [Google Scholar] [CrossRef]
- Nishimura, T.; Murakami, K.; Livingstone, M.B.; Sasaki, S.; Uenishi, K. Adherence to the food-based Japanese dietary guidelines in relation to metabolic risk factors in young Japanese women. Br. J. Nutr. 2015, 114, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Agriculture, Forestry and Fisheries. Japanese Food Guide Spinning Top. Available online: http://www.maff.go.jp/j/balance_guide/index.html. (accessed on 28 October 2017).
- Radloff, L. The CES-D scale: A self-report depression scale for research in the general population. Apll. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Horne, JA.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Kitamura, S.; Hida, A.; Aritake, S.; Higuchi, S.; Enomoto, M.; Kato, M.; Vetter, C.; Roenneberg, T.; Mishima, K. Validity of the Japanese version of the Munich ChronoType questionnaire. Chronobiol. Int. 2014, 31, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.L.; Heitkemper, M.M. Circadian rhythmicity of cortisol and body temperature: morningness-eveningness effects. Chronobiol. Int. 2001, 18, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Baehr, E.; Revelle, W.; Eastman, C. Individual differences in the phase and amplitude of the human circadian temperature rhythm: with an emphasis on morningness-eveningness. J. Sleep Res. 2000, 9, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Kerkhof, G.A.; Van Dongen, H.P. Morning-type and evening-type individuals differ in the phase position of their endogenous circadian oscillator. Neurosci. Letters 1996, 218, 153–156. [Google Scholar] [CrossRef]
- Mongrain, V.; Lavoie, S.; Selmaoui, B.; Paquet, J.; Dumont, M. Phase relationships between sleep-wake cycle and underlying circadian rhythms in morningness-eveningness. J. Biol. Rhythms. 2004, 19, 248–257. [Google Scholar] [CrossRef]
- Doi, Y.; Minowa, M.; Uchiyama, M. Development of the Pittsburgh sleep quality index Japanese version. Jpn. J. Psychiatr. Treat 1998, 13, 755–763. [Google Scholar]
- Kim, K.; Uchiyama, M.; Okawa, M.; Liu, X.; Ogihara, R. An epidemiological study of insomnia among the Japanese general population. Sleep 2000, 23, 41–47. [Google Scholar] [CrossRef]
- Buysse, D.; Reynolds, C.; Monk, T.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef] [PubMed]
- Okubo, H.; Sasaki, S.; Rafamantanantsoa, H.; Ishikawa-Takata, K.; Okazaki, H.; Tabata, I. Validation of self-reported energy intake by a self-administered diet history questionnaire using the doubly labeled water method in 140 Japanese adults. Eur. J. Clin. Nutr. 2008, 62, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2003; p. 306. [Google Scholar]
- Willett, W.; Stampfer, M.J. Total energy intake: Implications for epidemiologic analysis. Am. J. Epidemiol. 1986, 124, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.H.; Chung, F.M.; Yang, C.C.; Kuo, T.B.; Hsu, N. Sleep quality and morningness-eveningness of shift nurses. J. Clin. Nurs. 2009, 18, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Minowa, M.; Tango, T. Impact and correlates of poor sleep quality in Japanese white-collar employees. Sleep 2003, 26, 467–471. [Google Scholar] [CrossRef]
- Winpenny, E.M.; Van Harmelen, A.L.; White, M.; van Sluijs, E.M.; Goodyer, I.M. Diet quality and depressive symptoms in adolescence: no cross-sectional or prospective associations following adjustment for covariates. Public Health Nutr. 2018, 21, 1–9. [Google Scholar] [CrossRef]
- Yokoyama, E.; Kaneita, Y.; Saito, Y.; Uchiyama, M.; Matsuzaki, Y.; Tamaki, T.; Munezawa, T.; Ohida, T. Association between depression and insomnia subtypes: A longitudinal study on the elderly in Japan. Sleep 2010, 33, 1693–1702. [Google Scholar] [CrossRef]
- Lin, H.; Tsai, P.; Fang, S.; Liu, J.F. Effect of kiwifruit consumption on sleep quality in adults with sleep problems. Asia Pac. J. Clin. Nutr. 2011, 20, 169–174. [Google Scholar]
- Tanaka, E.; Yatsuya, H.; Uemura, M.; Murata, C.; Otsuka, R.; Toyoshima, H.; Tamakoshi, K.; Sasaki, S.; Kawaguchi, L.; Aoyama, A. Associations of protein, fat, and carbohydrate intakes with insomnia symptoms among middle-aged Japanese workers. J. Epidemiol. 2013, 23, 132–138. [Google Scholar] [CrossRef]
- Choi, S.; DiSilvio, B.; Fernstrom, M.H.; Fernstrom, J.D. Effect of chronic protein ingestion on tyrosine and tryptophan levels and catecholamine and serotonin synthesis in rat brain. Nutr. Neurosci. 2011, 14, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Le Floc'h, N.; Otten, W.; Merlot, E. Tryptophan metabolism, from nutrition to potential therapeutic applications. Amino Acids 2011, 41, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Jonnakuty, C.; Gragnoli, C. What do we know about serotonin? J. Cell. Physiol. 2008, 217, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Dawson, D.; Encel, N. Melatonin and sleep in humans. J. Pineal Res. 1993, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Halson, S.L. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 2014, 44, 13–23. [Google Scholar] [CrossRef]
- Saint-Hilaire, Z.D.; Messaoudi, M.; Desor, D.; Kobayashi, T. Effects of a bovine alpha S1-Casein tryptic hydrolysate (CTH) on sleep disorder in Japanese general population. Open Sleep J. 2009, 2, 26–32. [Google Scholar] [CrossRef]
- Abbasi, B.; Kimiagar, M.; Sadeghniiat, K.; Shirazi, M.M.; Hedayati, M.; Rashidkhani, B. The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. J. Res. Med. Sci. 2012, 17, 1161–1169. [Google Scholar] [PubMed]
- Ministry of Health, Labour and Welfare. The Japan National Health and Nutrition Survey (NHNS). 2016. Available online: https://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h28-houkoku-06.pdf (accessed on 19 November 2018).
- Roenneberg, T.; Kuehnle, T.; Pramstaller, P.P.; Ricken, J.; Havel, M.; Guth, A.; Merrow, M. A marker for the end of adolescence. Curr. Biol. 2004, 14, R1038–R1039. [Google Scholar] [CrossRef]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. The Japan National Health and Nutrition Survey (NHNS). 2017. Available online: https://www.mhlw.go.jp/content/10904750/000351576.pdf. (accessed on 19 November 2018).
- Patton, D.F.; Mistlberger, R.E. Chronotype: Circadian adaptations to meal timing: neuroendocrine mechanisms. Front. Neurosci. 2013, 7, 185. [Google Scholar] [CrossRef]
- Wehrens, S.M.T.; Christou, S.; Isherwood, C.; Middleton, B.; Gibbs, M.A.; Archer, S.N.; Skene, D.J.; Johnston, J.D. Meal timing regulates the human circadian system. Curr. Biol. 2017, 27, 1768–1775. [Google Scholar] [CrossRef] [PubMed]
- Almoosawi, S.; Vingeliene, S.; Gachon, F.; Voortman, T.; Palla, L.; Johnston, J.D.; Dam, R.M.V.; Darimont, C.; Karagounis, L.G. Chronotype: Implications for epidemiologic studies on chrono-nutrition and cardiometabolic health. Adv. Nutr. 2018. [Google Scholar] [CrossRef]
- Yoshida, H.; Ishikawa, T.; Shiraishi, F.; Kobayashi, T. Effects of the timing of exercise on the night sleep. Psychiatry Clin. Neurosci. 1998, 52, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Halson, S.L. Nutrition, sleep and recovery. Eur. J. Sport Sci. 2008, 8, 119–126. [Google Scholar] [CrossRef]
| T1 | T2 | T3 | p Value | ||||
|---|---|---|---|---|---|---|---|
| (n = 57) | (n = 47) | (n = 51) | |||||
| Age *(years) | 20.0 | 0.7 | 20.0 | 0.8 | 20.0 | 0.8 | 0.974 |
| Height *(cm) | 165.8 | 7.7 | 166.0 | 9.3 | 163.8 | 10.0 | 0.255 |
| Weight *(kg) | 57.8 | 8.7 | 58.2 | 11.5 | 57.2 | 11.9 | 0.615 |
| BMI *(kg/m2) | 21.0 | 2.5 | 21.0 | 3.2 | 21.2 | 3.0 | 0.603 |
| Sex † | |||||||
| Men | 27 | 47.4 | 25 | 53.2 | 26 | 51.0 | 0.692 |
| Woman | 30 | 52.6 | 22 | 46.8 | 25 | 49.0 | |
| Residential Status † | |||||||
| Living Alone | 22 | 38.6 | 20 | 42.6 | 18 | 35.3 | 0.762 |
| Other | 35 | 61.4 | 27 | 57.4 | 33 | 64.7 | |
| Current Drinker ‡ | |||||||
| No | 27 | 47.4 | 32 | 68.1 | 39 | 76.5 | 0.001 |
| Yes | 30 | 52.6 | 15 | 31.9 | 12 | 23.5 | |
| Current Smoker ‡ | |||||||
| No | 51 | 89.5 | 45 | 95.7 | 48 | 94.1 | 0.350 |
| Yes | 6 | 10.5 | 2 | 4.3 | 3 | 5.9 | |
| Current Medical History ‡ | |||||||
| No | 53 | 94.6 | 45 | 97.8 | 47 | 92.2 | 0.634 |
| Yes | 3 | 5.4 | 1 | 2.2 | 4 | 7.8 | |
| Past Medical History ‡ | |||||||
| No | 49 | 89.1 | 40 | 87.0 | 41 | 85.4 | 0.574 |
| Yes | 6 | 10.9 | 6 | 13.0 | 7 | 14.6 | |
| T1 | T2 | T3 | p Value | ||||
|---|---|---|---|---|---|---|---|
| (n = 57) | (n = 47) | (n = 51) | |||||
| Total Food Guide Score ‡ | 33.1 | 3.4 | 41.2 | 1.4 | 49.3 | 4.5 | <0.001 |
| Total Energy (points) †,§ | 8.1 | 1.8 | 8.6 | 1.4 | 9.4 | 0.9 | <0.001 |
| Grain Dishes (points) †,§ | 7.6 | 1.8 | 8.4 | 1.5 | 8.7 | 1.2 | <0.001 |
| Vegetable Dishes (points) †,§ | 4.3 | 2.9 | 5.1 | 2.7 | 6.1 | 2.7 | 0.001 |
| Fish and Meat Dishes (points) †,§ | 5.3 | 4.0 | 6.9 | 3.4 | 7.0 | 3.4 | 0.003 |
| Milk and Milk Products (points) †,§ | 2.7 | 2.5 | 3.6 | 2.8 | 5.5 | 3.1 | <0.001 |
| Fruits (points) †,§ | 3.2 | 3.2 | 3.7 | 3.2 | 5.5 | 3.4 | <0.001 |
| Energy from confectioneries, sugar-sweetened beverages and alcoholic beverages (points) †,§ | 2.4 | 3.7 | 5.3 | 4.3 | 7.5 | 3.4 | <0.001 |
| Energy Intake | 2037 | 768 | 1892 | 550 | 1832 | 338 | 0.071 |
| Nutrient Intake *,‡ | |||||||
| Protein (g) | 62.1 | 14.2 | 64.9 | 11.2 | 66.5 | 10.9 | 0.094 |
| Fat (g) | 68.5 | 18.6 | 64.9 | 14.0 | 62.2 | 13.0 | 0.036 |
| Carbohydrate (g) | 265.5 | 50.8 | 272.2 | 34.2 | 282.3 | 34.4 | 0.025 |
| Food Group Intake * | |||||||
| Grains (g) ‡ | 420.1 | 135.5 | 465.2 | 132.3 | 499.3 | 115.4 | 0.001 |
| Potato (g) ‡ | 25.4 | 25.8 | 25.3 | 19.9 | 24.9 | 18.2 | 0.395 |
| Nuts and Seeds (g) ‡ | 0.8 | 1.5 | 0.7 | 1.5 | 2.2 | 4.3 | 0.225 |
| Green Yellow Vegetables (g) ‡ | 44.5 | 44.6 | 60.3 | 36.3 | 109.5 | 96.5 | <0.001 |
| Non Green Yellow Vegetables (g) ‡ | 70.3 | 51.1 | 85.7 | 56.1 | 97.7 | 62.0 | 0.008 |
| Mushrooms (g) ‡ | 4.6 | 6.6 | 9.1 | 9.1 | 8.9 | 11.5 | 0.015 |
| Seaweed (g) ‡ | 5.8 | 8.4 | 10.3 | 12.8 | 9.5 | 10.7 | 0.005 |
| Fish and Shellfish (g) ‡ | 39.2 | 40.2 | 42.6 | 28.4 | 49.5 | 28.4 | 0.113 |
| Meats (g) ‡ | 91.6 | 52.8 | 94.4 | 43.0 | 85.8 | 36.6 | 0.768 |
| Eggs (g) ‡ | 37.5 | 44.9 | 34.6 | 21.5 | 34.2 | 25.3 | 0.498 |
| Beans (g) ‡ | 37.4 | 33.4 | 40.2 | 27.6 | 50.1 | 46.1 | 0.062 |
| Milk and Milk Products (g) ‡ | 101.8 | 144.4 | 124.2 | 144.6 | 128.9 | 88.0 | 0.007 |
| Fruits (g) ‡ | 61.7 | 99.4 | 100.9 | 86.2 | 158.4 | 125.2 | <0.001 |
| Confectioneries (g) ‡ | 107.2 | 57.7 | 86.2 | 50.7 | 64.4 | 30.8 | <0.001 |
| Sugar-Sweetened Beverages (g) ‡ | 843.0 | 546.1 | 781.6 | 686.9 | 775.3 | 478.9 | 0.753 |
| Alcoholic Beverages (g) ‡ | 82.4 | 128.5 | 56.3 | 121.3 | 18.5 | 31.7 | 0.001 |
| T1 | T2 | T3 | p Value | |||||
|---|---|---|---|---|---|---|---|---|
| (n = 57) | (n = 47) | (n = 51) | ||||||
| Awaking Time * (h:min) | 7:46 | 1:10 | 7:26 | 1:06 | 7:31 | 1:12 | 0.152 | |
| Retiring Time * (h:min) | 24:08 | 1:04 | 23:54 | 0:56 | 23:44 | 1:02 | 0.087 | |
| Sleep Duration * (h:min) | 7:38 | 0:56 | 7:32 | 1:08 | 7:47 | 1:00 | 0.493 | |
| Midpoint of Sleep *,§ (h:min) | 3:49 | 0:30 | 3:43 | 0:33 | 3:56 | 0:29 | 0.236 | |
| PSQI Score *,† (points) | 7.3 | 2.5 | 6.1 | 2.2 | 6.1 | 2.5 | 0.003 | |
| <6 | 13 | 22.8 | 19 | 40.4 | 24 | 47.1 | 0.006 | |
| 6≤ | 44 | 77.2 | 28 | 59.6 | 27 | 52.9 | ||
| MEQ Score ‡ (points) | 47.3 | 7.1 | 49.6 | 7.6 | 50.4 | 7.0 | 0.025 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, K.; Ota, M.; Minematsu, A.; Motokawa, K.; Yokoyama, Y.; Yano, T.; Watanabe, Y.; Yoshizaki, T. Association between Adherence to the Japanese Food Guide Spinning Top and Sleep Quality in College Students. Nutrients 2018, 10, 1996. https://doi.org/10.3390/nu10121996
Yamamoto K, Ota M, Minematsu A, Motokawa K, Yokoyama Y, Yano T, Watanabe Y, Yoshizaki T. Association between Adherence to the Japanese Food Guide Spinning Top and Sleep Quality in College Students. Nutrients. 2018; 10(12):1996. https://doi.org/10.3390/nu10121996
Chicago/Turabian StyleYamamoto, Kaori, Masako Ota, Ayako Minematsu, Keiko Motokawa, Yuri Yokoyama, Tomohiro Yano, Yutaka Watanabe, and Takahiro Yoshizaki. 2018. "Association between Adherence to the Japanese Food Guide Spinning Top and Sleep Quality in College Students" Nutrients 10, no. 12: 1996. https://doi.org/10.3390/nu10121996
APA StyleYamamoto, K., Ota, M., Minematsu, A., Motokawa, K., Yokoyama, Y., Yano, T., Watanabe, Y., & Yoshizaki, T. (2018). Association between Adherence to the Japanese Food Guide Spinning Top and Sleep Quality in College Students. Nutrients, 10(12), 1996. https://doi.org/10.3390/nu10121996




