Short-Term Daily Intake of Polydextrose Fiber Does Not Shorten Intestinal Transit Time in Constipated Adults: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Outcomes
2.5. Sample Size, Randomization and Blinding
2.6. Statistics
3. Results
3.1. Participant Recruitment and Study Flow
3.2. Primary Endpoint
3.3. Secondary Endpoints
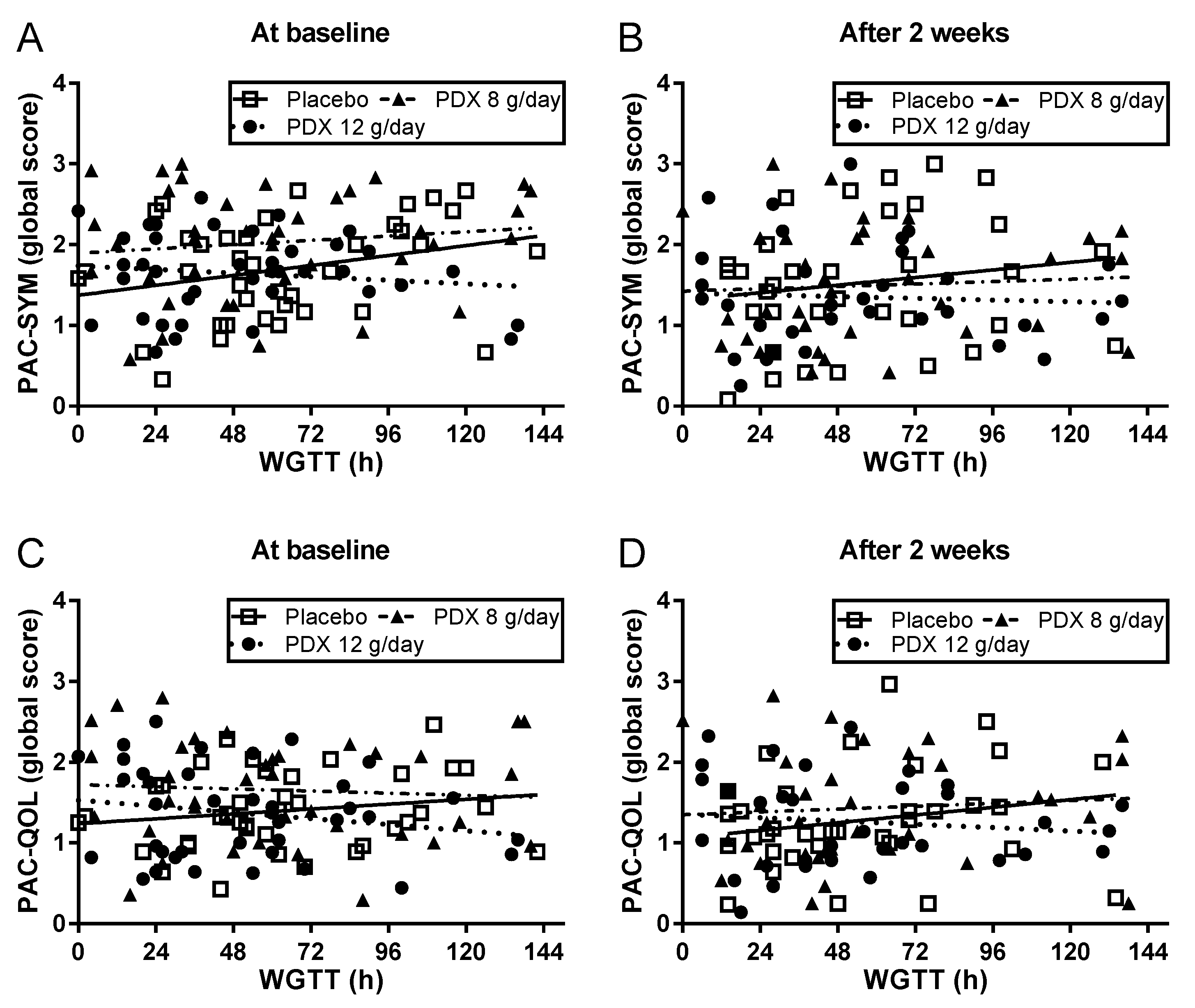
3.4. Patient-Reported Symptoms
3.5. Adverse Events
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mugie, S.M.; Benninga, M.A.; Di Lorenzo, C. Epidemiology of constipation in children and adults: A systematic review. Best Pract. Res. Clin. Gastroenterol. 2011, 25, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Suares, N.C.; Ford, A.C. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: Systematic review and meta-analysis. Am. J. Gastroenterol. 2011, 106, 1582–1591. [Google Scholar] [CrossRef] [PubMed]
- Cook, I.J.; Talley, N.J.; Benninga, M.A.; Rao, S.S.; Scott, S.M. Chronic constipation: Overview and challenges. Neurogastroenterol. Motil. 2009, 21 (Suppl. 2), 1–8. [Google Scholar] [CrossRef] [PubMed]
- Johanson, J.F.; Kralstein, J. Chronic constipation: A survey of the patient perspective. Aliment. Pharmacol. Ther. 2007, 25, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016, 150, 1393–1407. [Google Scholar] [CrossRef]
- Corazziari, E. Definition and epidemiology of functional gastrointestinal disorders. Best Pract. Res. Clin. Gastroenterol. 2004, 18, 613–631. [Google Scholar] [CrossRef] [PubMed]
- Shekhar, C.; Monaghan, P.J.; Morris, J.; Issa, B.; Whorwell, P.J.; Keevil, B.; Houghton, L.A. Rome III functional constipation and irritable bowel syndrome with constipation are similar disorders within a spectrum of sensitization, regulated by serotonin. Gastroenterology 2013, 145, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.K.; Palsson, O.S.; Turner, M.J.; Levy, R.L.; Feld, A.D.; von Korff, M.; Whitehead, W.E. Inability of the Rome III criteria to distinguish functional constipation from constipation-subtype irritable bowel syndrome. Am. J. Gastroenterol. 2010, 105, 2228–2234. [Google Scholar] [CrossRef] [PubMed]
- McCrea, G.L.; Miaskowski, C.; Stotts, N.A.; Macera, L.; Varma, M.G. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J. Pain Symptom Manag. 2009, 37, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Hammond, E.C. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am. J. Public Health Nations Health 1964, 54, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.F.; Ma, X.Q.; Wang, R.; Yan, X.Y.; Li, Z.S.; Zou, D.W.; He, J. Epidemiology of functional constipation and comparison with constipation-predominant irritable bowel syndrome: The Systematic Investigation of Gastrointestinal Diseases in China (SILC). Aliment. Pharmacol. Ther. 2011, 34, 1020–1029. [Google Scholar] [CrossRef] [PubMed]
- Bharucha, A.E.; Dorn, S.D.; Lembo, A.; Pressman, A. American Gastroenterological Association medical position statement on constipation. Gastroenterology 2013, 144, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.M.; van den Berg, M.M.; Benninga, M.A. Rectal sensorimotor dysfunction in constipation. Best Pract. Res. Clin. Gastroenterol. 2011, 25, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Dimidi, E.; Christodoulides, S.; Scott, S.M.; Whelan, K. Mechanisms of Action of Probiotics and the Gastrointestinal Microbiota on Gut Motility and Constipation. Adv. Nutr. 2017, 8, 484–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaheen, N.J.; Hansen, R.A.; Morgan, D.R.; Gangarosa, L.M.; Ringel, Y.; Thiny, M.T.; Russo, M.W.; Sandler, R.S. The burden of gastrointestinal and liver diseases, 2006. Am. J. Gastroenterol. 2006, 101, 2128–2138. [Google Scholar] [CrossRef] [PubMed]
- Peery, A.F.; Crockett, S.D.; Barritt, A.S.; Dellon, E.S.; Eluri, S.; Gangarosa, L.M.; Jensen, E.T.; Lund, J.L.; Pasricha, S.; Runge, T.; et al. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology 2015, 149, 1731–1741. [Google Scholar] [CrossRef] [PubMed]
- Prescriptions Dispensed in the Community: England 2002–2012. Health and Social Care Information Centre, UK. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/prescriptions-dispensed-in-the-community (accessed on 22 June 2018).
- Poulton, B.; Thomas, S. The nursing cost of constipation. Primary Health Care 1999, 9, 17–22. [Google Scholar]
- Belsey, J.; Greenfield, S.; Candy, D.; Geraint, M. Systematic review: Impact of constipation on quality of life in adults and children. Aliment. Pharmacol. Ther. 2010, 31, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Irvine, E.J.; Ferrazzi, S.; Pare, P.; Thompson, W.G.; Rance, L. Health-related quality of life in functional GI disorders: Focus on constipation and resource utilization. Am. J. Gastroenterol. 2002, 97, 1986–1993. [Google Scholar] [CrossRef] [PubMed]
- Wald, A.; Sigurdsson, L. Quality of life in children and adults with constipation. Best Pract. Res. Clin. Gastroenterol. 2011, 25, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Erdogan, A.; Rao, S.S.; Thiruvaiyaru, D.; Lee, Y.Y.; Coss, A.E.; Valestin, J.; O’Banion, M. Randomised clinical trial: Mixed soluble/insoluble fibre vs. psyllium for chronic constipation. Aliment. Pharmacol. Ther. 2016, 44, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Tack, J.; Camilleri, M.; Dubois, D.; Vandeplassche, L.; Joseph, A.; Kerstens, R. Association between health-related quality of life and symptoms in patients with chronic constipation: An integrated analysis of three phase 3 trials of prucalopride. Neurogastroenterol. Motil. 2015, 27, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Emmanuel, A.; Quigley, E.M.; Simrén, M.; Feng, Y.; Muller-Lissner, S.; Urbain, D.; Tack, J.; Bredenoord, A.J.; Sabate, J.M.; Yiannakou, Y.; et al. Factors affecting satisfaction with treatment in European women with chronic constipation: An internet survey. United Eur. Gastroenterol. J. 2013, 1, 375–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller-Lissner, S.; Tack, J.; Feng, Y.; Schenck, F.; Specht, G.R. Levels of satisfaction with current chronic constipation treatment options in Europe—An internet survey. Aliment. Pharmacol. Ther. 2013, 37, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Bharucha, A.E.; Pemberton, J.H.; Locke, G.R., III. American Gastroenterological Association technical review on constipation. Gastroenterology 2013, 144, 218–238. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Moayyedi, P.; Lacy, B.E.; Lembo, A.J.; Saito, Y.A.; Schiller, L.R.; Soffer, E.E.; Spiegel, B.M.; Quigley, E.M. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am. J. Gastroenterol. 2014, 109 (Suppl. 1), S2–S26. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, G.; Hamid, S.S.; Malfertheiner, P.; Thomsen, O.O.; Fernandez, L.B.; Garisch, J.; Thomson, A.; Goh, K.L.; Tandon, R.; Fedail, S.; et al. World Gastroenterology Organisation global guideline: Constipation—A global perspective. J. Clin. Gastroenterol. 2011, 45, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.E.; Jung, H.K.; Lee, T.H.; Jo, Y.; Lee, H.; Song, K.H.; Hong, S.N.; Lim, H.C.; Lee, S.J.; Chung, S.S.; et al. Guidelines for the Diagnosis and Treatment of Chronic Functional Constipation in Korea, 2015 Revised Edition. J. Neurogastroenterol. Motil. 2016, 22, 383–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tack, J.; Müller-Lissner, S.; Stanghellini, V.; Boeckxstaens, G.; Kamm, M.A.; Simren, M.; Galmiche, J.P.; Fried, M. Diagnosis and treatment of chronic constipation--a European perspective. Neurogastroenterol. Motil. 2011, 23, 697–710. [Google Scholar] [CrossRef] [PubMed]
- Buttriss, J.; Stokes, C. Dietary fibre and health: An overview. Nutr. Bull. 2008, 33, 186–200. [Google Scholar] [CrossRef]
- Christodoulides, S.; Dimidi, E.; Fragkos, K.C.; Farmer, A.D.; Whelan, K.; Scott, S.M. Systematic review with meta-analysis: Effect of fibre supplementation on chronic idiopathic constipation in adults. Aliment. Pharmacol. Ther. 2016, 44, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.S.; Yu, S.; Fedewa, A. Systematic review: Dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome. Aliment. Pharmacol. Ther. 2015, 41, 1256–1270. [Google Scholar] [CrossRef] [PubMed]
- Suares, N.C.; Ford, A.C. Systematic review: The effects of fibre in the management of chronic idiopathic constipation. Aliment. Pharmacol. Ther. 2011, 33, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Figdor, S.K.; Rennhard, H.H. Caloric utilization and disposition of [14C]polydextrose in the rat. J. Agric. Food Chem. 1981, 29, 1181–1189. [Google Scholar] [CrossRef] [PubMed]
- Do Carmo, M.M.; Walker, J.C.; Novello, D.; Caselato, V.M.; Sgarbieri, V.C.; Ouwehand, A.C.; Andreollo, N.A.; Hiane, P.A.; Dos Santos, E.F. Polydextrose: Physiological Function, and Effects on Health. Nutrients 2016, 8, 553. [Google Scholar] [CrossRef] [PubMed]
- Röytiö, H.; Ouwehand, A.C. The fermentation of polydextrose in the large intestine and its beneficial effects. Benef. Microbes 2014, 5, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Costabile, A.; Fava, F.; Röytiö, H.; Forssten, S.D.; Olli, K.; Klievink, J.; Rowland, I.R.; Ouwehand, A.C.; Rastall, R.A.; Gibson, G.R.; et al. Impact of polydextrose on the faecal microbiota: A double-blind, crossover, placebo-controlled feeding study in healthy human subjects. Br. J. Nutr. 2012, 108, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Hengst, C.; Ptok, S.; Roessler, A.; Fechner, A.; Jahreis, G. Effects of polydextrose supplementation on different faecal parameters in healthy volunteers. Int. J. Food Sci. Nutr. 2009, 60 (Suppl. 5), 96–105. [Google Scholar] [CrossRef] [PubMed]
- Matsuike, T.; Suzuki, Y.; Nozawa, H.; Nishino, H.; Matsushima, M.; Mori, Y. Effects of Polydextrose on Habitual Constipation with Melanosis Coli. J. Jpn. Assoc. Diet. Fiber Res. 2002, 6, 55–60. [Google Scholar]
- Matsuike, T.; Suzuki, Y.; Nozawa, H.; Nishino, H.; Mori, Y. Clinical Research of Polydextrose on Habitual Constipation. J. Jpn. Assoc. Diet. Fiber Res. 2002, 6, 17–20. [Google Scholar]
- Nakagawa, Y.; Okamatsu, H.; Fujii, Y. Effects of polydextrose feeding on the frequency and feeling of defecation in healthy female volunteers. J. Jpn. Soc. Nutr. Food Sci. 1990, 43, 95–101. [Google Scholar] [CrossRef]
- Timm, D.A.; Thomas, W.; Boileau, T.W.; Williamson-Hughes, P.S.; Slavin, J.L. Polydextrose and soluble corn fiber increase five-day fecal wet weight in healthy men and women. J. Nutr. 2013, 143, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Tomlin, J.; Read, N.W. A comparative study of the effects on colon function caused by feeding ispaghula husk and polydextrose. Aliment. Pharmacol. Ther. 1988, 2, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Achour, L.; Flourié, B.; Briet, F.; Pellier, P.; Marteau, P.; Rambaud, J.C. Gastrointestinal effects and energy value of polydextrose in healthy nonobese men. Am. J. Clin. Nutr. 1994, 59, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Boler, B.M.; Serao, M.C.; Bauer, L.L.; Staeger, M.A.; Boileau, T.W.; Swanson, K.S.; Fahey, G.C., Jr. Digestive physiological outcomes related to polydextrose and soluble maize fibre consumption by healthy adult men. Br. J. Nutr. 2011, 106, 1864–1871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Endo, K.; Kumemura, M.; Nakamura, K.; Fujisawa, T.; Suzuki, K.; Benno, Y.; Mitsuoka, T. Effect of high cholesterol diet and polydextrose supplementation on the microflora, bacterial enzyme activity, putrefactive products, volatile fatty acid (VFA) profile, weight, and pH of the feces in healthy volunteers. Bifidobact. Microflora 1991, 10, 53–64. [Google Scholar] [CrossRef]
- Jie, Z.; Bang-Yao, L.; Ming-Jie, X.; Hai-Wei, L.; Zu-Kang, Z.; Ting-Song, W.; Craig, S.A. Studies on the effects of polydextrose intake on physiologic functions in Chinese people. Am. J. Clin. Nutr. 2000, 72, 1503–1509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Block, G.; Gillespie, C.; Rosenbaum, E.H.; Jenson, C. A rapid food screener to assess fat and fruit and vegetable intake. Am. J. Prev. Med. 2000, 18, 284–288. [Google Scholar] [CrossRef] [Green Version]
- Lewis, S.J.; Heaton, K.W. Stool form scale as a useful guide to intestinal transit time. Scand. J. Gastroenterol. 1997, 32, 920–924. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, H.; Antov, S.; Bosaeus, I. Gastrointestinal and colonic segmental transit time evaluated by a single abdominal X-ray in healthy subjects and constipated patients. Scand. J. Gastroenterol. Suppl. 1988, 152, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Bouchoucha, M.; Thomas, S.R. Error analysis of classic colonic transit time estimates. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 279, G520–G527. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.; Kleinman, L.; Farup, C.; Taylor, L.; Miner, P., Jr. Psychometric validation of a constipation symptom assessment questionnaire. Scand. J. Gastroenterol. 1999, 34, 870–877. [Google Scholar] [PubMed]
- Yiannakou, Y.; Tack, J.; Piessevaux, H.; Dubois, D.; Quigley, E.M.M.; Ke, M.Y.; Da Silva, S.; Joseph, A.; Kerstens, R. The PAC-SYM questionnaire for chronic constipation: Defining the minimal important difference. Aliment. Pharmacol. Ther. 2017, 46, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Agachan, F.; Chen, T.; Pfeifer, J.; Reissman, P.; Wexner, S.D. A constipation scoring system to simplify evaluation and management of constipated patients. Dis. Colon Rectum 1996, 39, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Marquis, P.; De La Loge, C.; Dubois, D.; McDermott, A.; Chassany, O. Development and validation of the Patient Assessment of Constipation Quality of Life questionnaire. Scand. J. Gastroenterol. 2005, 40, 540–551. [Google Scholar] [CrossRef] [PubMed]
- Waller, P.A.; Gopal, P.K.; Leyer, G.J.; Ouwehand, A.C.; Reifer, C.; Stewart, M.E.; Miller, L.E. Dose-response effect of Bifidobacterium lactis HN019 on whole gut transit time and functional gastrointestinal symptoms in adults. Scand. J. Gastroenterol. 2011, 46, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Ding, C.; Ge, X.; Zhang, X.; Tian, H.; Wang, H.; Gu, L.; Gong, J.; Zhu, W.; Li, N. Efficacy of Synbiotics in Patients with Slow Transit Constipation: A Prospective Randomized Trial. Nutrients 2016, 8, 605. [Google Scholar] [CrossRef] [PubMed]
- Flourie, B.; Not, D.; Francois, C.; Prost à la Denise, M. Factors associated with impaired quality of life in French patients with chronic idiopathic constipation: A cross-sectional study. Eur. J. Gastroenterol. Hepatol. 2016, 28, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Tack, J.; Stanghellini, V.; Dubois, D.; Joseph, A.; Vandeplassche, L.; Kerstens, R. Effect of prucalopride on symptoms of chronic constipation. Neurogastroenterol. Motil. 2014, 26, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Panel on Dietetic Products, Nutrition and Allergies. Polydextrose and maintenance of normal defecation: Evaluation of a health claim pursuant to Article 13(5) of Regulation (EC) No 1924/2006. EFSA J. 2016, 14, e04480. [Google Scholar] [CrossRef]
- Figdor, S.K.; Bianchine, J.R. Caloric utilization and disposition of [14C]polydextrose in man. J. Agric. Food Chem. 1983, 31, 389–393. [Google Scholar] [CrossRef] [PubMed]
- McRorie, J.W., Jr.; McKeown, N.M. Understanding the Physics of Functional Fibers in the Gastrointestinal Tract: An Evidence-Based Approach to Resolving Enduring Misconceptions about Insoluble and Soluble Fiber. J. Acad. Nutr. Diet. 2016, 117, 251–264. [Google Scholar] [CrossRef] [PubMed]
- McRorie, J.W.; Chey, W.D. Fermented Fiber Supplements Are No Better Than Placebo for a Laxative Effect. Dig. Dis. Sci. 2016, 61, 3140–3146. [Google Scholar] [CrossRef] [PubMed]
- Khalif, I.L.; Quigley, E.M.; Konovitch, E.A.; Maximova, I.D. Alterations in the colonic flora and intestinal permeability and evidence of immune activation in chronic constipation. Dig. Liver Dis. 2005, 37, 838–849. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, G.; Chen, J.; Chen, X.; Chia, N.; O'Connor, H.M.; Wolf, P.G.; Gaskins, H.R.; Bharucha, A.E. Relationship Between Microbiota of the Colonic Mucosa vs Feces and Symptoms, Colonic Transit, and Methane Production in Female Patients With Chronic Constipation. Gastroenterology 2016, 150, 367–379. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Liu, W.; Alkhouri, R.; Baker, R.D.; Bard, J.E.; Quigley, E.M.; Baker, S.S. Structural changes in the gut microbiome of constipated patients. Physiol. Genom. 2014, 46, 679–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polymeros, D.; Beintaris, I.; Gaglia, A.; Karamanolis, G.; Papanikolaou, I.S.; Dimitriadis, G.; Triantafyllou, K. Partially hydrolyzed guar gum accelerates colonic transit time and improves symptoms in adults with chronic constipation. Dig. Dis. Sci. 2014, 59, 2207–2214. [Google Scholar] [CrossRef] [PubMed]
- Emmanuel, A.; Cools, M.; Vandeplassche, L.; Kerstens, R. Prucalopride improves bowel function and colonic transit time in patients with chronic constipation: An integrated analysis. Am. J. Gastroenterol. 2014, 109, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, B.; Irvine, J.E.; Tack, J.; Crowell, M.D.; Gwee, K.A.; Ke, M.; Schmulson Wasserman, M.J.; Whitehead, W.E. Design of Treatment Trials for Functional Gastrointestinal Disorders. In Rome IV Functional Gastrointestinal Disorders, 4th ed.; The Rome Foundation: Raleigh, NC, USA, 2017; Volume 2, pp. 1373–1444. [Google Scholar]
- Knowles, C.H.; Scott, S.M.; Rayner, C.; Glia, A.; Lindberg, G.; Kamm, M.A.; Lunniss, P.J. Idiopathic slow-transit constipation: An almost exclusively female disorder. Dis. Colon Rectum 2003, 46, 1716–1717. [Google Scholar] [CrossRef] [PubMed]
- Zakari, M.; Nee, J.; Hirsch, W.; Kuo, B.; Lembo, A.; Staller, K. Gender differences in chronic constipation on anorectal motility. Neurogastroenterol. Motil. 2017, 29. [Google Scholar] [CrossRef] [PubMed]



| Placebo (n = 39) | Polydextrose 8 g/day (n = 40) | Polydextrose 12 g/day (n = 40) | |
|---|---|---|---|
| Age (years), median (range, SD) | 30.9 (19–71, 16.0) | 29.2 (19–72, 15.7) | 46.8 (19–64, 15.1) |
| Female, n (%) | 36 (92.3) | 38 (95.0) | 37 (92.5) |
| BMI (kg/m2), mean (SD) | 23.9 (3.3) | 23.6 (2.9) | 23.7 (2.8) |
| Fiber intake, g/day (SD) | 15.3 (2.4) | 15.2 (2.3) | 14.2 (2.5) |
| CCCS, mean (SD) | 12.8 (3.3) | 13.6 (2.6) | 12.4 (2.7) |
| SBM (n/week), mean (SD) | 5.4 (3.0) | 4.9 (3.9) | 6.3 (4.4) |
| BSFS, mean (SD) | 2.8 (1.1) | 2.8 (1.1) | 3.0 (1.2) |
| Bloating, mean (SD) | 5.5 (2.4) | 6.4 (2.3) | 6.0 (2.2) |
| PAC-SYM (global), mean (SD) | 1.7 (0.6) | 2.0 (0.7) * | 1.6 (0.5) |
| PAC-QOL (global), mean (SD) | 1.4 (0.5) | 1.7 (0.6) * | 1.3 (0.6) |
| WGTT (hours), mean (SD) | 64 (35) | 62 (41) | 51 (34) |
| Placebo | Polydextrose 8 g/day | Polydextrose 12 g/day | Change from Baseline. Polydextrose 12 g/day vs. PLACEBO (ANCOVA Model) | |||||
|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | Mean Difference (95% CI) | p-Value | |
| Change in WGTT (h) | ||||||||
| 35 | −9.4 ± 27.0 | 35 | −0.9 ± 32.8 | 35 | 6.8 ± 26.1 | 11.8 (−1.3, 24.9) | 0.08 | |
| Change in Regional CTT (h) | ||||||||
| Right colon | 35 | −4.4 ± 17.1 | 35 | 0.5 ± 13.7 | 35 | −1.3 ± 11.6 | 0.5 (−5.2, 6.2) | 0.86 |
| Left colon | 35 | −1.6 ± 12.8 | 35 | 0.4 ± 18.5 | 35 | 9.4 ± 16.1 | 9.3 (2.2, 16.5) | 0.01 * |
| Rectosigmoid | 35 | −2.7 ± 16.5 | 35 | −1.7 ± 18.7 | 35 | −0.7 ± 14.0 | −0.7 (−7.0, 5.6) | 0.83 |
| Change in Stool Frequency (Number Per Week) | ||||||||
| SBM, 14 days | 36 | 0.6 ± 2.9 | 35 | 1.3 ± 3.3 | 36 | 0.7 ± 3.3 | 0.2 (−1.2, 1.7) | 0.77 |
| SBM, 28 days | 36 | 0.1 ± 2.7 | 34 | 0.8 ± 2.6 | 34 | −0.6 ± 3.3 | −0.4 (−1.6, 0.8) | 0.52 |
| CSBM, 14 days | 36 | 1.4 ± 2.6 | 35 | 1.1 ± 2.1 | 36 | 0.1 ± 2.1 | −1.0 (−2.1, 0.0) | 0.06 |
| CSBM, 28 days | 36 | 0.6 ± 2.1 | 34 | 1.0 ± 2.0 | 34 | −0.2 ± 2.3 | −0.5 (−1.5, 0.5) | 0.29 |
| Change in Stool Consistency | ||||||||
| BSFS, 14 days | 36 | 0.3 ± 1.4 | 34 | 0.2 ± 1.2 | 36 | 0.3 ± 1.1 | 0.2 (−0.3, 0.7) | 0.51 |
| BSFS, 28 days | 36 | 0.1 ± 1.2 | 34 | 0.3 ± 1.1 | 34 | 0.3 ± 1.2 | 0.4 (−0.1, 0.8) | 0.14 |
| Placebo | Polydextrose 8 g/day | Polydextrose 12 g/day | ||||
|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | |
| Change in Global Score | ||||||
| 14 days | 36 | −0.2 ± 0.6 | 35 | −0.5 ± 0.7 * | 36 | −0.2 ± 0.6 |
| 28 days | 36 | −0.2 ± 0.5 | 34 | −0.7 ± 0.6 ** | 34 | −0.4 ± 0.8 |
| Change in Abdominal Score | ||||||
| 14 days | 36 | −0.3 ± 0.7 | 35 | −0.6 ± 0.8 | 36 | −0.2 ± 0.7 |
| 28 days | 36 | −0.3 ± 0.8 | 34 | −0.8 ± 0.7 | 34 | −0.3 ± 0.9 |
| Change in Rectal Score | ||||||
| 14 days | 36 | 0.1 ± 0.6 | 35 | −0.4 ± 0.8 ** | 36 | −0.2 ± 0.7 * |
| 28 days | 36 | −0.1 ± 0.4 | 34 | −0.5 ± 0.7 ** | 34 | −0.3 ± 0.8 * |
| Change in Stool Score | ||||||
| 14 days | 36 | −0.2 ± 0.8 | 35 | −0.6 ± 1.0 | 36 | −0.3 ± 0.8 |
| 28 days | 36 | −0.2 ± 0.8 | 34 | −0.8 ± 0.9 ** | 34 | −0.4 ± 1.0 |
| Placebo | Polydextrose 8 g/day | Polydextrose 12 g/day | ||||
|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | |
| Change in PAC-QOL Global Score | ||||||
| 28 days | 36 | −0.1 ± 0.5 | 34 | −0.4 ± 0.6 * | 34 | −0.3 ± 0.7 |
| Change in PAC-QOL Satisfaction Score | ||||||
| 28 days | 36 | −0.1 ± 0.9 | 34 | −0.6 ± 0.9 * | 34 | −0.3 ± 1.2 |
| Change in Bloating Score | ||||||
| 28 days | 33 | 0.2 ± 1.9 | 32 | −1.0 ± 2.4 * | 33 | −0.6 ± 3.1 |
| Change in GCSS | ||||||
| 28 days | 36 | 0.2 ± 1.7 | 33 | 0.9 ± 1.8 * | 33 | 0.5 ± 1.9 |
| Placebo | Polydextrose 8 g/day | Polydextrose 12 g/day | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Subjects, n (% Group) | Events, n | Subjects, n (% Group) | Events, n | Subjects, n (% Group) | Events, n | ||
| Any AE/SAE | 24 (61.5%) | 69 | 29 (72.5%) | 71 | 30 (75.0%) | 81 | 0.39 |
| Abdominal discomfort | 0 (0%) | 0 | 1 (2.5%) | 1 | 1 (2.5%) | 1 | 1.00 |
| Abdominal distension | 3 (7.7%) | 4 | 6 (15%) | 6 | 3 (7.5%) | 3 | 0.32 |
| Abdominal pain | 9 (23.1%) | 18 | 11 (27.5%) | 18 | 8 (20.0%) | 12 | 0.74 |
| Flatulence | 0 (0%) | 0 | 1 (2.5%) | 1 | 0 (0%) | 0 | 1.00 |
| Nausea | 2 (5.1%) | 2 | 3 (7.5%) | 3 | 3 (7.5%) | 4 | 1.00 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duncan, P.I.; Enters-Weijnen, C.F.; Emami, N.; McLean, P.; Nunes, T.; Beaumont, M.; Crabbe, R.; Whelan, K.; Scott, S.M.; DeWit, N.J.; et al. Short-Term Daily Intake of Polydextrose Fiber Does Not Shorten Intestinal Transit Time in Constipated Adults: A Randomized Controlled Trial. Nutrients 2018, 10, 920. https://doi.org/10.3390/nu10070920
Duncan PI, Enters-Weijnen CF, Emami N, McLean P, Nunes T, Beaumont M, Crabbe R, Whelan K, Scott SM, DeWit NJ, et al. Short-Term Daily Intake of Polydextrose Fiber Does Not Shorten Intestinal Transit Time in Constipated Adults: A Randomized Controlled Trial. Nutrients. 2018; 10(7):920. https://doi.org/10.3390/nu10070920
Chicago/Turabian StyleDuncan, Peter I., Catherine F. Enters-Weijnen, Nashmil Emami, Peter McLean, Tiago Nunes, Maurice Beaumont, Rafael Crabbe, Kevin Whelan, S. Mark Scott, Niek J. DeWit, and et al. 2018. "Short-Term Daily Intake of Polydextrose Fiber Does Not Shorten Intestinal Transit Time in Constipated Adults: A Randomized Controlled Trial" Nutrients 10, no. 7: 920. https://doi.org/10.3390/nu10070920
APA StyleDuncan, P. I., Enters-Weijnen, C. F., Emami, N., McLean, P., Nunes, T., Beaumont, M., Crabbe, R., Whelan, K., Scott, S. M., DeWit, N. J., Weits, T., Bergonzelli, G., & Grobbee, D. E. (2018). Short-Term Daily Intake of Polydextrose Fiber Does Not Shorten Intestinal Transit Time in Constipated Adults: A Randomized Controlled Trial. Nutrients, 10(7), 920. https://doi.org/10.3390/nu10070920






