Vitamin B12 Status Upon Short-Term Intervention with a Vegan Diet—A Randomized Controlled Trial in Healthy Participants
Abstract
1. Introduction
2. Materials and Methods
2.1. Course of the Study
2.2. Inclusion and Exclusion Criteria
2.3. Randomization and Blinding
2.4. Selection of Target Parameters
2.5. Blood and Urine Analysis
2.6. Analysis of Serum tHcy, Cys, Cystathionine, GSH, Met, and MSO by LC-ESI-MS/MS
2.7. Analysis of Methylmalonic Acid (MMA) by LC-ESI-MS/MS (Sciex QTrap 6500+, Sciex)
2.8. Amino Acids Profiles
2.9. Fatty Acid Profiles
2.10. Analysis of Total Nitrite and Nitrate
2.11. Urine Analysis
2.12. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Analysis of Vitamin B12 Status before and after 4-Week Intervention
3.3. Proportion of Individuals with Abnormal Serum Parameters of Vitamin B12 Status after the 4-Week Trial
3.4. Analysis of Homocysteine Metabolism before and after the 4-Week Trial
3.5. Analysis of 25-OH-Vitamin D2/D3
3.6. Plasma Nitrite and Nitrate
3.7. Urine Analysis
3.8. Evaluation of Nutritional Protocols
3.9. Nutritional Assessment before and after 4-Week Intervention
3.10. Fatty Acid Profiles
4. Discussion
4.1. Effect of Diet on Markers of Vitamin B12 Status
4.2. Value of Holo-TC for the Assessment of Vitamin B12 Status with Respect to Diet
4.3. Biomarker Associations and Cut-Off Values for the Assessment of Vitamin B12 Status in Plant-Based Subjects
4.4. Effect of Diet on Metabolic Markers of Inflammation and Cardiovascular Health
4.5. Strengths and Limitations of This Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Šimčikas, S. Animal Charity Evaluators Is the Percentage of Vegetarians and Vegans in the U.S. Increasing? Available online: https://animalcharityevaluators.org/blog/is-the-percentage-of-vegetarians-and-vegans-in-the-u-s-increasing/#analysis (accessed on 21 March 2019).
- Berlin, J. Skopos Group 1,3 Millionen Deutsche Leben Vegan. Available online: https://www.skopos-group.de/news/13-millionen-deutsche-leben-vegan.html (accessed on 21 March 2019).
- Allen, L.H. How common is vitamin B-12 deficiency? Am. J. Clin. Nutr. 2009, 89, 693–696. [Google Scholar] [CrossRef] [PubMed]
- Hunt, A.; Harrington, D.; Robinson, S. Vitamin B12 deficiency. BMJ 2014, 349, 5226. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, F.; Yabuta, Y.; Bito, T.; Teng, F. Vitamin B12-Containing Plant Food Sources for Vegetarians. Nutrients 2014, 6, 1861–1873. [Google Scholar] [CrossRef] [PubMed]
- Hannibal, L.; Lysne, V.; Bjørke-Monsen, A.-L.; Behringer, S.; Grünert, S.C.; Spiekerkoetter, U.; Jacobsen, D.W.; Blom, H.J. Biomarkers and Algorithms for the Diagnosis of Vitamin B12 Deficiency. Front. Mol. Biosci. 2016, 3. [Google Scholar] [CrossRef]
- Blanco, A.; Blanco, G. Medical Biochemistry; Elsevier: Amsterdam, The Netherlands, 2017; ISBN 9780128035504. [Google Scholar]
- Nielsen, M.J.; Rasmussen, M.R.; Andersen, C.B.F.; Nexø, E.; Moestrup, S.K. Vitamin B12 transport from food to the body’s cells—a sophisticated, multistep pathway. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 345–354. [Google Scholar] [CrossRef]
- Johnson, L.R.; Kaunitz, J.D.; Said, H.M.; Ghishan, F.K.; Merchant, J.L.; Wood, J.D. Physiology of the Gastrointestinal Tract; Elsevier: Amsterdam, The Netherlands, 2012; ISBN 9780123820266. [Google Scholar]
- Schneede, J.; Ueland, P.M. Novel and established markers of cobalamin deficiency: Complementary or exclusive diagnostic strategies. Semin. Vasc. Med. 2005, 5, 140–155. [Google Scholar] [CrossRef]
- Ströhle, A.; Richter, M.; González-Gross, M.; Neuhäuser-Berthold, M.; Wagner, K.-H.; Leschik-Bonnet, E.; Egert, S. German Nutrition Society (DGE) The Revised D-A-CH-Reference Values for the Intake of Vitamin B12: Prevention of Deficiency and Beyond. Mol. Nutr. Food Res. 2019, 63, 1801178. [Google Scholar] [CrossRef]
- von Castel-Roberts, K.M.; Morkbak, A.L.; Nexo, E.; Edgemon, C.A.; Maneval, D.R.; Shuster, J.J.; Valentine, J.F.; Kauwell, G.P.; Bailey, L.B. Holo-transcobalamin is an indicator of vitamin B-12 absorption in healthy adults with adequate vitamin B-12 status. Am. J. Clin. Nutr. 2007, 85, 1057–1061. [Google Scholar] [CrossRef]
- Fedosov, S.N. Biochemical markers of vitamin B12 deficiency combined in one diagnostic parameter: The age-dependence and association with cognitive function and blood hemoglobin. Clin. Chim. Acta. 2013, 422, 47–53. [Google Scholar] [CrossRef]
- Basak, T.; Garg, G.; Bhardwaj, N.; Tanwar, V.S.; Seth, S.; Karthikeyan, G.; Sengupta, S. Low holo-transcobalamin levels are prevalent in vegetarians and is associated with coronary artery disease in Indian population. Biomarkers 2016, 21, 436–440. [Google Scholar] [CrossRef]
- Naik, S.; Mahalle, N.; Bhide, V. Identification of vitamin B 12 deficiency in vegetarian Indians. Br. J. Nutr. 2018, 119, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Carmel, R. Diagnosis and management of clinical and subclinical cobalamin deficiencies: Why controversies persist in the age of sensitive metabolic testing. Biochimie 2013, 95, 1047–1055. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, W. Vitamin B 12 Deficiency in Vegetarians. In Vegetarian and Plant-Based Diets in Health and Disease Prevention; Elsevier: Amsterdam, The Netherlands, 2017; pp. 791–808. ISBN 9780128039694. [Google Scholar]
- Herbert, V. Staging vitamin B−12 (cobalamin) status in vegetarians. Am. J. Clin. Nutr. 1994, 59, 1213–1222. [Google Scholar] [CrossRef] [PubMed]
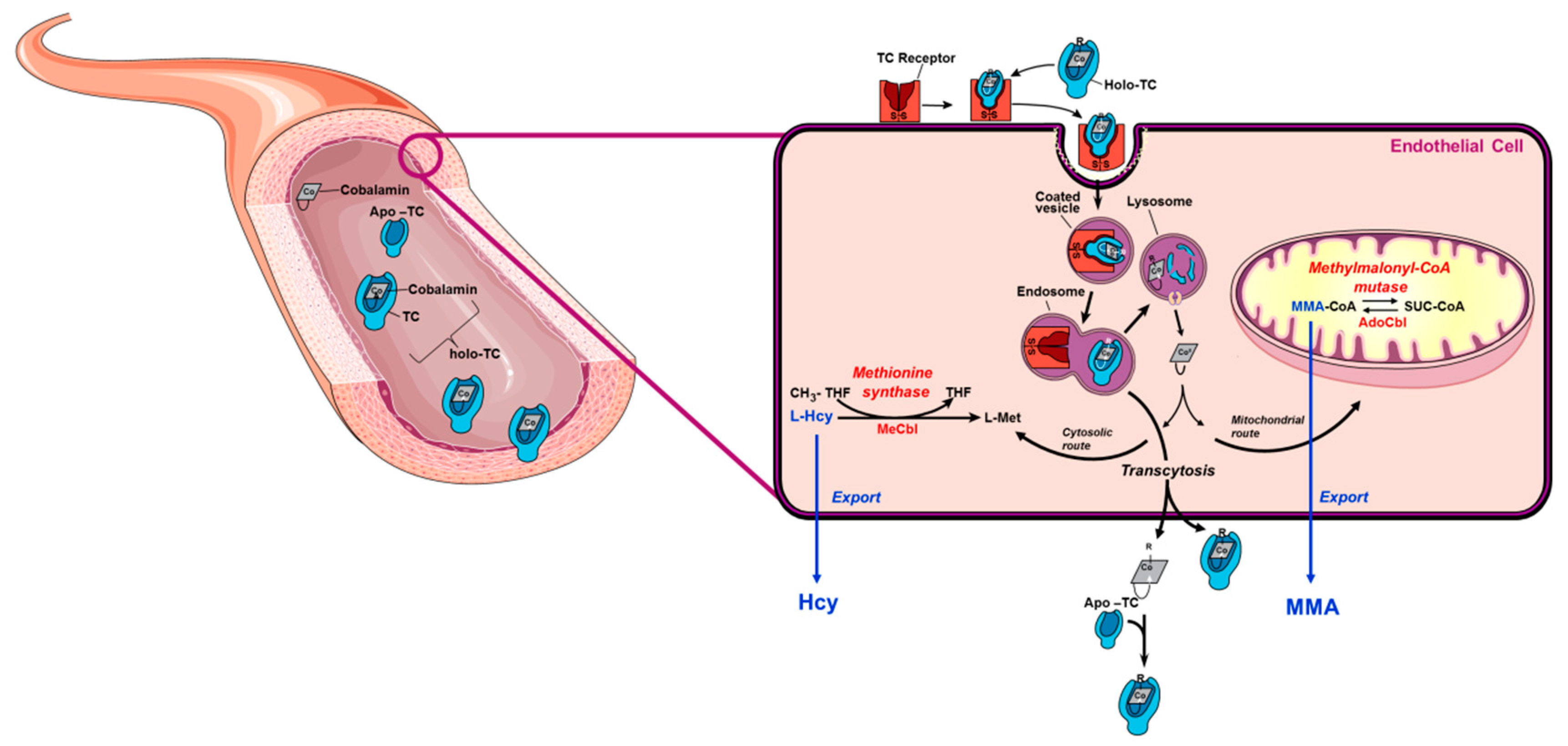
- Hannibal, L.; Bolisetty, K.; Axhemi, A.; DiBello, P.M.; Quadros, E.V.; Fedosov, S.; Jacobsen, D.W. Transcellular transport of cobalamin in aortic endothelial cells. FASEB J. 2018, 32, 5506–5519. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Ernährung Vollwertige Ernährung. Available online: https://www.dge.de/ernaehrungspraxis/vollwertige-ernaehrung/ (accessed on 14 May 2018).
- Hannibal, L.; Blom, H.J. Homocysteine and disease: Causal associations or epiphenomenons? Mol. Asp. Med. 2017, 53, 36–42. [Google Scholar] [CrossRef]
- Mashima, R.; Nakanishi-Ueda, T.; Yamamoto, Y. Simultaneous determination of methionine sulfoxide and methionine in blood plasma using gas chromatography-mass spectrometry. Anal. Biochem. 2003, 313, 28–33. [Google Scholar] [CrossRef]
- Behringer, S.; Wingert, V.; Oria, V.; Schumann, A.; Grünert, S.; Cieslar-Pobuda, A.; Kölker, S.; Lederer, A.-K.; Jacobsen, D.W.; Staerk, J.; et al. Targeted Metabolic Profiling of Methionine Cycle Metabolites and Redox Thiol Pools in Mammalian Plasma, Cells and Urine. Metabolites 2019, 9, 235. [Google Scholar] [CrossRef]
- Idborg, H.; Pawelzik, S.-C.; Perez-Manso, M.; Björk, L.; Hamrin, J.; Herlenius, E.; Jakobsson, P.-J. Evaluation of urinary prostaglandin E2 metabolite as a biomarker in infants with fever due to viral infection. Prostaglandins. Leukot. Essent. Fat. Acids 2014, 91, 269–275. [Google Scholar] [CrossRef]
- Blom, H.J.; van Rooij, A.; Hogeveen, M. A simple high-throughput method for the determination of plasma methylmalonic acid by liquid chromatography-tandem mass spectrometry. Clin. Chem. Lab. Med. 2007, 45, 645–650. [Google Scholar] [CrossRef]
- Krawinkel, M.B.; Strohm, D.; Weissenborn, A.; Watzl, B.; Eichholzer, M.; Bärlocher, K.; Elmadfa, I.; Leschik-Bonnet, E.; Heseker, H. Revised D-A-CH intake recommendations for folate: How much is needed? Eur. J. Clin. Nutr. 2014, 68, 719–723. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Ernährung e., V. Referenzwerte Vitamin B6. Available online: https://www.dge.de/wissenschaft/referenzwerte/vitamin-b6/ (accessed on 5 September 2019).
- Ulvik, A.; Hustad, S.; McCann, A.; Midttun, Ø.; Nygård, O.K.; Ueland, P.M. Ratios of One-Carbon Metabolites Are Functional Markers of B-Vitamin Status in a Norwegian Coronary Angiography Screening Cohort. J. Nutr. 2017, 147, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.A.B.; Ellis, F.R.; Dickerson, J.W.T. Studies of vegans: The fatty acid composition of plasma choline phosphoglycerides, erythrocytes, adipose tissue, and breast milk, and some indicators of susceptibility to ischemic heart disease in vegans and omnivore controls. Am. J. Clin. Nutr. 1978, 31, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Le, L.T.; Sabaté, J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients 2014, 6, 2131–2147. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Levin, S.; Barnard, N. Cardio-Metabolic Benefits of Plant-Based Diets. Nutrients 2017, 9, 848. [Google Scholar] [CrossRef]
- Kjeldsen-Kragh, J. Rheumatoid arthritis treated with vegetarian diets. Am. J. Clin. Nutr. 1999, 70, 594–600. [Google Scholar] [CrossRef]
- Kjeldsen-Kragh, J.; Haugen, M.; Borchgrevink, C.F.; Laerum, E.; Eek, M.; Mowinkel, P.; Hovi, K.; Førre, O. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. Lancet 1991, 338, 899–902. [Google Scholar] [CrossRef]
- Nexo, E.; Hoffmann-Lücke, E. Holotranscobalamin, a marker of vitamin B-12 status: Analytical aspects and clinical utility. Am. J. Clin. Nutr. 2011, 94, 359–365. [Google Scholar] [CrossRef]
- Golding, P.H. Holotranscobalamin (HoloTC, Active-B12) and Herbert’s model for the development of vitamin B12 deficiency: A review and alternative hypothesis. Springerplus 2016, 5, 668. [Google Scholar] [CrossRef]
- Keller, P.; Rufener, J.; Schild, C.; Fedosov, S.N.; Nissen, P.H.; Nexo, E. False low holotranscobalamin levels in a patient with a novel TCN2 mutation. Clin. Chem. Lab. Med. 2016, 54, 1739–1743. [Google Scholar] [CrossRef][Green Version]
- Green, R.; Allen, L.H.; Bjørke-Monsen, A.-L.; Brito, A.; Guéant, J.-L.; Miller, J.W.; Molloy, A.M.; Nexo, E.; Stabler, S.; Toh, B.-H.; et al. Vitamin B12 deficiency. Nat. Rev. Dis. Prim. 2017, 3, 17040. [Google Scholar] [CrossRef]
- Sobczyńska-Malefora, A.; Pangilinan, F.; Plant, G.T.; Velkova, A.; Harrington, D.J.; Molloy, A.M.; Brody, L.C. Association of a transcobalamin II genetic variant with falsely low results for the holotranscobalamin immunoassay. Eur. J. Clin. Investig. 2016, 46, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, W.; Obeid, R.; Schorr, H.; Geisel, J. The usefulness of holotranscobalamin in predicting vitamin B12 status in different clinical settings. Curr. Drug Metab. 2005, 6, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Solomon, L.R. Cobalamin-responsive disorders in the ambulatory care setting: Unreliability of cobalamin, methylmalonic acid, and homocysteine testing. Blood 2004, 105, 978–985. [Google Scholar] [CrossRef] [PubMed]
- Combs, G.F.; McClung, J.P. Vitamin B12. In The Vitamins; Elsevier: Amsterdam, The Netherlands, 2017; pp. 431–452. [Google Scholar]
- Joske, R.A. The vitamin B12 content of human liver tissue obtained by aspiration biopsy. Gut 1963, 4, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Fedosov, S.N. Physiological and Molecular Aspects of Cobalamin Transport. In Water Soluble Vitamins; Springer: Dordrecht, The Netherlands, 2012; pp. 347–367. [Google Scholar]
- Hall, C.A.; Green-Colligan, P.D.; Begley, J.A. Synthesis of transcobalamin II by cultured human hepatocytes. Biochim. Biophys. Acta Gen. Subj. 1985, 838, 387–389. [Google Scholar] [CrossRef]
- Soda, R.; Tavassoli, M.; Jacobsen, D.W. Receptor distribution and the endothelial uptake of transcobalamin II in liver cell suspensions. Blood 1985, 65, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Quadros, E.V.; Rothenberg, S.P.; Jaffe, E.A. Endothelial cells from human umbilical vein secrete functional transcobalamin II. Am. J. Physiol. Physiol. 1989, 256, 296–303. [Google Scholar] [CrossRef]
- Quadros, E.V.; Regec, A.L.; Khan, K.M.F.; Quadros, E.; Rothenberg, S.P. Transcobalamin II synthesized in the intestinal villi facilitates transfer of cobalamin to the portal blood. Am. J. Physiol. Liver Physiol. 1999, 277, 161–166. [Google Scholar] [CrossRef]
- Greibe, E.; Mahalle, N.; Bhide, V.; Heegaard, C.W.; Naik, S.; Nexo, E. Increase in circulating holotranscobalamin after oral administration of cyanocobalamin or hydroxocobalamin in healthy adults with low and normal cobalamin status. Eur. J. Nutr. 2018, 57, 2847–2855. [Google Scholar] [CrossRef]
- Metaxas, C.; Mathis, D.; Jeger, C.; Hersberger, K.E.; Arnet, I.; Walter, P. Early biomarker response and patient preferences to oral and intramuscular vitamin B12 substitution in primary care: A randomised parallel-group trial. Swiss Med. Wkly. 2017, 147, 14421. [Google Scholar]
- Donaldson, R.M.; Brand, M.; Serfilippi, D. Changes in Circulating Transcobalamin II after Injection of Cyanocobalamin. N. Engl. J. Med. 1977, 296, 1427–1430. [Google Scholar] [CrossRef] [PubMed]
- Hannibal, L. Invited commentary in response to: Identification of vitamin B 12 deficiency in vegetarian Indians. Br. J. Nutr. 2018, 119, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Müller, H.; de Toledo, F.W.; Resch, K.L. Fasting followed by vegetarian diet in patients with rheumatoid arthritis: A systematic review. Scand. J. Rheumatol. 2001, 30, 1–10. [Google Scholar] [PubMed]
- Norris, D.O.; Carr, J.A. Synthesis, Metabolism, and Actions of Bioregulators. In Vertebrate Endocrinology; Elsevier Inc., Ed.; Academic Press: Cambridge, MA, USA, 2013; pp. 537–543. ISBN 978-0-12-394815-1. [Google Scholar]
- Calder, P.C. Omega-3 fatty acids and inflammatory processes: From molecules to man. Biochem. Soc. Trans. 2017, 45, 1105–1115. [Google Scholar] [CrossRef]
- Kawahara, K.; Hohjoh, H.; Inazumi, T.; Tsuchiya, S.; Sugimoto, Y. Prostaglandin E2-induced inflammation: Relevance of prostaglandin E receptors. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2015, 1851, 414–421. [Google Scholar] [CrossRef]
- Bäck, M.; Yurdagul, A.; Tabas, I.; Öörni, K.; Kovanen, P.T. Inflammation and its resolution in atherosclerosis: Mediators and therapeutic opportunities. Nat. Rev. Cardiol. 2019, 16, 389–406. [Google Scholar] [CrossRef]
- Ferretti, A.; Nelson, G.J.; Schmidt, P.C.; Kelley, D.S.; Bartolini, G.; Flanagan, V.P. Increased dietary arachidonic acid enhances the synthesis of vasoactive eicosanoids in humans. Lipids 1997, 32, 435–439. [Google Scholar] [CrossRef]
- Innes, J.K.; Calder, P.C. Omega-6 fatty acids and inflammation. Prostaglandins Leukot. Essent. Fat. Acids 2018, 132, 41–48. [Google Scholar] [CrossRef]
- Seeds, M.C.; Bass, D.A. Regulation and metabolism of arachidonic acid. Clin. Rev. Allergy Immunol. 1999, 17, 5–26. [Google Scholar] [CrossRef]
- Ashworth, A.; Bescos, R. Dietary nitrate and blood pressure: Evolution of a new nutrient? Nutr. Res. Rev. 2017, 30, 208–219. [Google Scholar] [CrossRef]
- Kerley, C.P. A Review of Plant-based Diets to Prevent and Treat Heart Failure. Card. Fail. Rev. 2018, 4, 54–61. [Google Scholar] [CrossRef]
- Lidder, S.; Webb, A.J. Vascular effects of dietary nitrate (as found in green leafy vegetables and beetroot) via the nitrate-nitrite-nitric oxide pathway. Br. J. Clin. Pharmacol. 2013, 75, 677–696. [Google Scholar] [CrossRef] [PubMed]







| Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value | |
|---|---|---|---|
| Age (years) | 33.2 ± 11.2 | 29.9 ± 9.5 | 0.407 |
| Baseline: Body mass index (kg/m2) | 22.9 ± 2.2 | 23.3 ± 2.6 | 0.444 |
| End of study: Body mass index (kg/m2) | 22.7 ± 2.0 | 23.4 ± 2.6 | 0.240 |
| Gender (male/female, %) | 31/69 | 44/56 | 0.309 |
| Baseline | End | p-Value (Baseline-to-End) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value (Baselines) | Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value (End) | Time | Diet | Time × Diet | |
| Holotranscobalamin (pmol/L) | 67.3 ± 23.5 | 69.7 ± 29.7 | 0.901 | 43.6 ± 20.0 | 64.4 ± 28.7 | <0.001 | <0.001 | 0.098 | <0.001 |
| Methylmalonic acid (nmol/L) | 214.5 ± 129.6 | 220.0 ± 121.0 | 0.755 | 277.8 ± 330.0 | 213.1 ± 182.2 | 0.090 | 0.253 | 0.573 | 0.158 |
| Serum vitamin B12 (ng/mL) | 362.8 ± 110.9 | 391.2 ± 159.2 | 0.510 | 296.1 ± 94.1 | 391.8 ± 143.0 | <0.001 | <0.001 | 0.085 | <0.001 |
| 25-OH-vitamin D2/D3 (ng/mL) | 32.9 ± 15.6 | 29.6 ± 13.9 | 0.439 | 34.2 ± 15.3 | 31.4 ± 11.3 | 0.903 | 0.039 | 0.427 | 0.829 |
| Baseline | End | p-Value (Baseline-to-End) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value (Baselines) | Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value (End) | Time | Diet | Time × Diet | |
| Cystathionine (µmol/L) | 0.3 ± 0.1 | 0.3 ± 0.3 | 0.378 | 0.3 ± 0.3 | 0.6 ± 1.5 | 0.642 | 0.213 | 0.446 | 0.430 |
| Cysteine (µmol/L) | 206.7 ± 21.3 | 206.8 ± 19.6 | 0.475 | 167.9 ± 29.7 | 183.3 ± 19.2 | 0.321 | <0.001 | 0.641 | 0.378 |
| Glutathione (µmol/L) | 3.3 ± 1.1 | 3.3 ± 1.3 | 0.943 | 5.4 ± 1.8 | 4.8 ± 1.8 | 0.093 | <0.001 | 0.395 | 0.090 |
| Homocysteine (µmol/L) | 7.9 ± 2.5 | 8.8 ± 4.1 | 0.606 | 7.7 ± 4.2 | 7.2 ± 2.7 | 0.140 | 0.034 | 0.832 | 0.084 |
| Methionine (µmol/L) | 28.5 ± 4.1 | 27.7 ± 3.8 | 0.631 | 27.2 ± 3.1 | 27.7 ± 3.9 | 0.415 | 0.472 | 0.922 | 0.288 |
| Methionine sulfoxide (µmol/L) | 0.7 ± 0.2 | 0.7 ± 0.2 | 0.466 | 0.7 ± 0.2 | 0.7 ± 0.3 | 0.707 | 0.748 | 0.818 | 0.578 |
| Subject | Diet | B12 <200 ng/L | Holo-TC <35 pmol/L | MMA >300 nmol/L | tHcy >15 µmol/L | Abnormal Baseline Values |
|---|---|---|---|---|---|---|
| 5 | MD | + | + | |||
| 8 | MD | + | ||||
| 15 | MD | + | ||||
| 20 | MD | + | ||||
| 35 | MD | + | + | MMA + tHcy + | ||
| 39 | MD | + | tHcy + | |||
| 42 | MD | + | B12 + | |||
| 44 | MD | + | + | MMA + | ||
| 12 | VD | + | ||||
| 23 | VD | + | + | + | tHcy + | |
| 24 | VD | + | ||||
| 25 | VD | + | ||||
| 27 | VD | + | ||||
| 29 | VD | + | ||||
| 34 | VD | + | + | |||
| 41 | VD | + | ||||
| 48 | VD | + | + | + | B12 + MMA + | |
| 49 | VD | + | + | MMA + | ||
| 51 | VD | + |
| Baseline | End | p-Value (Baseline-to-End) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Vegan ± SD (n = 22) | Meat-Rich ± SD (n = 22) | p-Value (Baselines) | Vegan ± SD (n = 22) | Meat-Rich ± SD (n = 22) | p-Value (End) | Time | Diet | Time × Diet | |
| Intake of energy (kcal) | 2228.8 ± 915.0 | 2333.7 ± 859.1 | 0.549 | 2240.8 ± 894.8 | 2242.3 ± 762.7 | 0.213 | 0.588 | 0.468 | 0.291 |
| Kilojoule (kj) | 9388.6 ± 3747.8 | 9771.1 ± 3593.1 | 0.565 | 9068.5 ± 2949.8 | 10265.6 ± 4210.7 | 0.211 | 0.586 | 0.470 | 0.287 |
| Carbohydrates (g) | 245.5 ± 95.4 | 256.9 ± 136.9 | 0.897 | 276.0 ± 85.1 | 241.5 ± 91.8 | 0.001 | 0.688 | 0.670 | 0.209 |
| Percentage of energy intake | 47% | 47% | 54% | 41% | |||||
| Fat (g) | 86.4 ± 42.2 | 89.3 ± 43.5 | 0.751 | 68.8 ± 29.1 | 106.3 ± 47.4 | 0.143 | 0.611 | 0.091 | 0.002 |
| Percentage of energy intake | 37% | 36% | 31% | 40% | |||||
| Protein (g) | 86.9 ± 33.4 | 94.0 ± 41.3 | 0.474 | 79.5 ± 28.5 | 112.4 ± 44.4 | <0.001 | 0.413 | 0.020 | <0.001 |
| Percentage of energy intake | 16% | 17% | 15% | 19% | |||||
| Cholesterol (mg) | 332.9 ± 167.6 | 324.8 ± 140.3 | 0.787 | 28.7 ± 25.6 | 452.6 ± 185.5 | <0.001 | 0.003 | <0.001 | <0.001 |
| Saturated fatty acids (g) | 32.2 ± 15.0 | 34.1 ± 15.4 | 0.681 | 15.4 ± 5.7 | 43.9 ± 20.5 | <0.001 | 0.309 | <0.001 | <0.001 |
| Monounsaturated fatty acids (g) | 31.6 ± 17.5 | 31.6 ± 17.5 | 0.769 | 26.9 ± 14.1 | 38.4 ± 17.3 | 0.005 | 0.370 | 0.345 | 0.003 |
| Polyunsaturated fatty acids (g) | 15.1 ± 8.8 | 15.2 ± 8.3 | 0.565 | 19.6 ± 7.9 | 15.0 ± 7.0 | 0.063 | 0.025 | 0.121 | 0.193 |
| Fiber (g) | 27.8 ± 10.8 | 34.5 ± 25.6 | 0.342 | 45.7 ± 19.5 | 24.9 ± 11.05 | <0.001 | 0.171 | 0.077 | <0.001 |
| Salt (g) | 4.6 ± 2.2 | 5.0 ± 1.8 | 0.255 | 3.8 ± 1.8 | 6.1 ± 3.2 | 0.003 | 0.589 | 0.040 | 0.006 |
| Sugar (g) | 118.5 ± 61.4 | 114.0 ± 70.7 | 0.664 | 114.4 ± 32.8 | 108.1 ± 52.46 | 0.585 | 0.527 | 0.669 | 0.855 |
| Uric acid (mg) | 488.4 ± 236.2 | 491.9 ± 194.6 | 0.842 | 603.0 ± 279.5 | 603.6 ± 276.1 | 0.849 | 0.003 | 0.840 | 0.754 |
| Sodium (mg) | 2196.0 ± 1479.4 | 2216.9 ± 803.7 | 0.405 | 1692.7 ± 802.9 | 2736.3 ± 1427.6 | 0.002 | 0.844 | 0.105 | 0.007 |
| Potassium (mg) | 3663.7 ± 1316.1 | 3527.0 ± 1039.8 | 0.474 | 4186.2 ± 1794.4 | 3605.6± 1671.0 | 0.401 | 0.160 | 0.209 | 0.610 |
| Calcium (mg) | 841.1 ± 378.6 | 854.6 ± 244.9 | 0.534 | 645.1 ± 390.1 | 933.8 ± 447.3 | 0.029 | 0.556 | 0.107 | 0.051 |
| Magnesium (mg) | 401.6 ± 181.3 | 397.5 ± 149.5 | 0.681 | 505.4 ± 213.2 | 388.2 ± 172.9 | 0.107 | 0.080 | 0.113 | 0.214 |
| Copper (μg) | 1935.6 ± 877.7 | 1838.8 ± 693.9 | 0.787 | 2564.0 ± 974.2 | 1763.9 ± 703.5 | 0.008 | 0.018 | 0.011 | 0.040 |
| Fluoride (µg) | 1079.4 ± 908.3 | 1027.5 ± 342.5 | 0.265 | 912.7 ± 358.5 | 1055.7 ± 477.3 | 0.249 | 0.663 | 0.840 | 0.314 |
| Iodione (µg) | 118.3 ± 41.3 | 116.5 ± 40.7 | 0.787 | 62.6 ± 23.2 | 119.1 ± 52.8 | <0.001 | 0.004 | 0.007 | <0.001 |
| Iron (mg) | 11.9 ± 4.5 | 11.9 ± 4.6 | 0.824 | 14.8 ± 6.1 | 13.5 ± 5.4 | 0.579 | 0.004 | 0.398 | 0.736 |
| Phosphorus (mg) | 1344.2 ± 454.1 | 1423.2 ± 517.1 | 0.405 | 1193.2 ± 494.2 | 1602.6 ± 677.6 | 0.018 | 0.510 | 0.120 | 0.021 |
| Zinc (mg) | 10.8 ± 4.2 | 11.2 ± 4.7 | 0.647 | 9.0 ± 3.9 | 14.7 ± 6.4 | <0.001 | 0.109 | 0.026 | <0.001 |
| Retinol (mg) | 1963.7 ± 1256.0 | 2396.6 ± 2423.4 | 0.879 | 1924.5 ± 1210.0 | 2464.9 ± 2024.3 | 0.323 | 0.640 | 0.406 | 0.549 |
| β-carotene (µg) | 9317.3 ± 4797.7 | 7666.9 ± 4749.1 | 0.405 | 1130.3 ± 723.3 | 681.4 ± 621.7 | 0.050 | 0.571 | 0.064 | 0.107 |
| Vitamin B1 (mg) | 1.6 ± 1.0 | 1.5 ± 0.6 | 0.725 | 2.0 ± 0.8 | 1.8 ± 0.9 | 0.687 | 0.001 | 0.228 | 0.860 |
| Vitamin B2 (mg) | 1.6 ± 0.6 | 1.4 ± 0.7 | 0.787 | 1.3 ± 0.7 | 2.0 ± 0.8 | 0.003 | 0.510 | 0.040 | 0.004 |
| Niacin (mg) | 3686.4 ± 1858.5 | 3724.7 ± 1789.8 | 0.842 | 3431.2 ± 1629.0 | 4588.1 ± 1933.5 | 0.007 | 0.082 | 0.345 | 0.005 |
| Vitamin B6 (mg) | 2.0 ± 0.9 | 2.0 ± 0.7 | 0.916 | 2.3 ± 1.1 | 2.2 ± 1.0 | 0.930 | 0.055 | 0.603 | 0.934 |
| Folate (μg) | 345.9 ± 187.1 | 327.3 ± 126.0 | 0.842 | 509.1 ± 317.0 | 286.7 ± 117.2 | 0.007 | 0.038 | 0.012 | 0.010 |
| Vitamin B12 (μg) | 4.8 ± 2.1 | 5.9 ± 5.4 | 0.769 | 0.8 + ± 1.2 | 8.5 ± 4.1 | <0.001 | 0.602 | <0.001 | <0.001 |
| Vitamin C (mg) | 132.5 ± 77.1 | 131.8 ± 49.8 | 0.597 | 182.1 ± 78.9 | 119.5 ± 57.0 | 0.006 | 0.146 | 0.032 | 0.037 |
| Vitamin D (µg) | 1.9 ± 1.1 | 2.2 ± 1.8 | 0.434 | 2.1 ± 3.4 | 2.3 ± 1.2 | 0.217 | 0.931 | 0.367 | 0.210 |
| Vitamin E (mg) | 13.9 ± 7.8 | 12.9 ± 6.2 | 0.681 | 16.1 ± 7.6 | 12.4 ± 3.8 | 0.019 | 0.047 | 0.018 | 0.139 |
| Phenylalanine (mg) | 3837.4 ± 1519.3 | 4033.1 ± 1891.6 | 0.597 | 3036.6 ± 1514.6 | 4850.6 ± 1940.3 | <0.001 | 0.461 | 0.042 | <0.001 |
| Baseline | End | p-Value (Baseline-to-End) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value (Baselines) | Vegan ± SD (n = 26) | Meat-Rich ± SD (n = 27) | p-Value (End) | Time | Diet | Time × Diet | |
| Arachidonic acid (µM) | 4.3 ± 2.0 | 3.9 ± 1.7 | 0.790 | 3.3 ± 1.3 | 6.4 ± 8.0 | 0.046 | 0.111 | 0.080 | 0.043 |
| Docosahexaenoic acid (µM) + | 0.2 ± 0.2 | 0.1 ± 0.1 | 0.683 | 0.1 ± 0.1 | 0.3 ± 0.9 | 0.298 | 0.423 | 0.408 | 0.263 |
| Eicosanoic acid (µM) | 14.9 ± 6.4 | 11.2 ± 3.5 | 0.288 | 12.9 ± 5.7 | 14.2 ± 11.0 | 0.211 | 0.876 | 0.991 | 0.124 |
| Eicosenoic acid (µM) | 1.1 ± 0.4 | 0.8 ± 0.4 | 0.410 | 0.9 ± 0.3 | 0.8 ± 0.4 | 0.906 | 0.608 | 0.314 | 0.387 |
| Linoleic acid (µM) | 406.6 ± 179.3 | 484.2 ± 235.3 | 0.421 | 440.3 ± 193.3 | 401.5 ± 176.3 | 0.532 | 0.228 | 0.588 | 0.271 |
| Linolenic acid (µM) | 3.5 ± 1.4 | 2.3 ± 0.8 | 0.742 | 2.9 ± 1.3 | 2.3 ± 1.3 | 0.705 | 0.061 | 0.406 | 0.933 |
| Oleic acid (µM) | 97.0 ± 40.4 | 100.3 ± 48.7 | 1.000 | 92.7 ± 51.13 | 100.5 ± 59.7 | 0.602 | 0.338 | 0.714 | 0.648 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lederer, A.-K.; Hannibal, L.; Hettich, M.; Behringer, S.; Spiekerkoetter, U.; Steinborn, C.; Gründemann, C.; Zimmermann-Klemd, A.M.; Müller, A.; Simmet, T.; et al. Vitamin B12 Status Upon Short-Term Intervention with a Vegan Diet—A Randomized Controlled Trial in Healthy Participants. Nutrients 2019, 11, 2815. https://doi.org/10.3390/nu11112815
Lederer A-K, Hannibal L, Hettich M, Behringer S, Spiekerkoetter U, Steinborn C, Gründemann C, Zimmermann-Klemd AM, Müller A, Simmet T, et al. Vitamin B12 Status Upon Short-Term Intervention with a Vegan Diet—A Randomized Controlled Trial in Healthy Participants. Nutrients. 2019; 11(11):2815. https://doi.org/10.3390/nu11112815
Chicago/Turabian StyleLederer, Ann-Kathrin, Luciana Hannibal, Manuel Hettich, Sidney Behringer, Ute Spiekerkoetter, Carmen Steinborn, Carsten Gründemann, Amy Marisa Zimmermann-Klemd, Alexander Müller, Thomas Simmet, and et al. 2019. "Vitamin B12 Status Upon Short-Term Intervention with a Vegan Diet—A Randomized Controlled Trial in Healthy Participants" Nutrients 11, no. 11: 2815. https://doi.org/10.3390/nu11112815
APA StyleLederer, A.-K., Hannibal, L., Hettich, M., Behringer, S., Spiekerkoetter, U., Steinborn, C., Gründemann, C., Zimmermann-Klemd, A. M., Müller, A., Simmet, T., Schmiech, M., Maul-Pavicic, A., Samstag, Y., & Huber, R. (2019). Vitamin B12 Status Upon Short-Term Intervention with a Vegan Diet—A Randomized Controlled Trial in Healthy Participants. Nutrients, 11(11), 2815. https://doi.org/10.3390/nu11112815







