Percutaneous Endoscopic Gastrostomy versus Nasogastric Tube Feeding: Oropharyngeal Dysphagia Increases Risk for Pneumonia Requiring Hospital Admission
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Demographic and Clinical Data
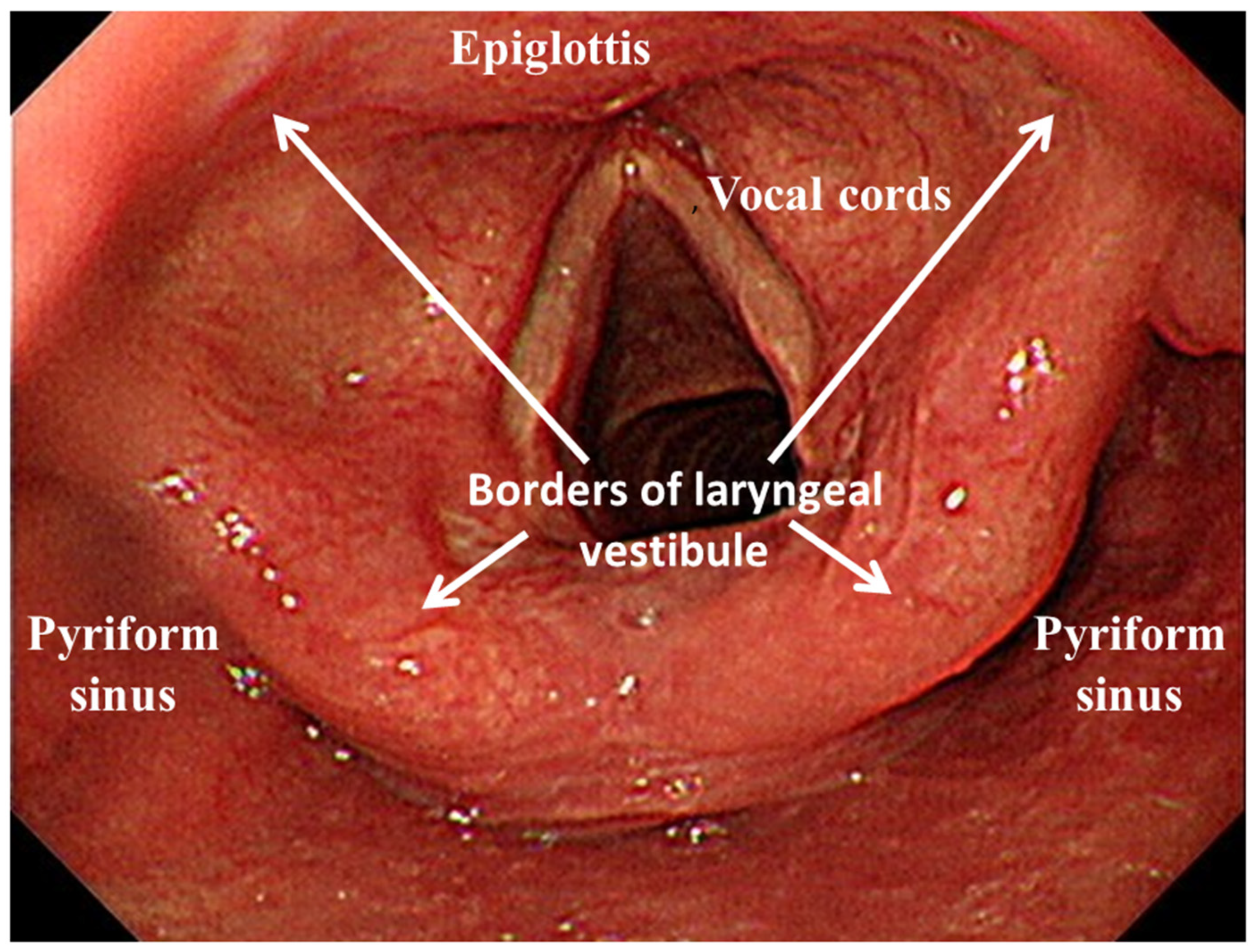
2.3. UGI Endoscopy with Pharyngolaryngeal Observations
2.4. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data
3.2. Incidence of Pneumonia
3.3. Risk Factor of Pneumonia
3.4. Cumulative Proportion of Pneumonia
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rowat, A. Enteral tube feeding for dysphagic stroke patients. Br. J. Nurs. 2015, 24, 138. [Google Scholar] [CrossRef]
- Gomes, C.A., Jr.; Andriolo, R.B.; Bennett, C.; Lustosa, S.A.; Matos, D.; Waisberg, D.R.; Waisberg, J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst. Rev. 2015, 5, CD008096. [Google Scholar] [CrossRef] [Green Version]
- Stroud, M.; Duncan, H.; Nightingale, J. Guidelines for enteral feeding in adult hospital patients. Gut 2003, 52, vii1–vii12. [Google Scholar] [CrossRef] [Green Version]
- Loser, C.; Aschl, G.; Hebuterne, X.; Mathus-Vliegen, E.M.; Muscaritoli, M.; Niv, Y.; Rollins, H.; Singer, P.; Skelly, R.H. ESPEN guidelines on artificial enteral nutrition--percutaneous endoscopic gastrostomy (PEG). Clin. Nutr. 2005, 24, 848–861. [Google Scholar]
- Pash, E. Enteral Nutrition: Options for Short-Term Access. Nutr. Clin. Pract. 2018, 33, 170–176. [Google Scholar] [CrossRef] [Green Version]
- Lin, L.C.; Li, M.H.; Watson, R. A survey of the reasons patients do not chose percutaneous endoscopic gastrostomy/jejunostomy (PEG/PEJ) as a route for long-term feeding. J. Clin. Nurs. 2011, 20, 802–810. [Google Scholar] [CrossRef]
- Mamun, K.; Lim, J. Role of nasogastric tube in preventing aspiration pneumonia in patients with dysphagia. Singap. Med. J. 2005, 46, 627–631. [Google Scholar]
- Metheny, N.A.; Schallom, L.; Oliver, D.A.; Clouse, R.E. Gastric residual volume and aspiration in critically ill patients receiving gastric feedings. Am. J. Crit. Care 2008, 17, 512–519. [Google Scholar]
- Abuksis, G.; Mor, M.; Plaut, S.; Fraser, G.; Niv, Y. Outcome of percutaneous endoscopic gastrostomy (PEG): Comparison of two policies in a 4-year experience. Clin. Nutr. 2004, 23, 341–346. [Google Scholar] [CrossRef]
- Moran, C.; O’Mahony, S. When is feeding via a percutaneous endoscopic gastrostomy indicated? Curr. Opin. Gastroenterol. 2015, 31, 137–142. [Google Scholar] [CrossRef]
- Jaafar, M.H.; Mahadeva, S.; Morgan, K.; Tan, M.P. Percutaneous endoscopic gastrostomy versus nasogastric feeding in older individuals with non-stroke dysphagia: A systematic review. J. Nutr. Health Aging 2015, 19, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, M.; Liu, C.; Ye, Y.; Huang, G. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for patients with head and neck cancer: A systematic review. J. Radiat. Res. 2014, 55, 559–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almirall, J.; Rofes, L.; Serra-Prat, M.; Icart, R.; Palomera, E.; Arreola, V.; Clave, P. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur. Respir. J. 2013, 41, 923–928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masiero, S.; Pierobon, R.; Previato, C.; Gomiero, E. Pneumonia in stroke patients with oropharyngeal dysphagia: A six-month follow-up study. Neurol. Sci. 2008, 29, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, T.; Horiuchi, A.; Nakayama, Y. Transnasal endoscopic evaluation of swallowing: A bedside technique to evaluate ability to swallow pureed diets in elderly patients with dysphagia. Can. J. Gastroenterol. 2013, 27, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Raju, G.S. Value of screening the laryngopharyngeal area during routine upper gastrointestinal endoscopy. Nat. Clin. Pract. Gastroenterol. Hepatol. 2005, 2, 22–23. [Google Scholar] [CrossRef]
- Chang, W.K.; Huang, H.H.; Lin, H.H.; Tsai, C.L. Evaluation of Oropharyngeal Dysphagia in Patients Who Underwent Percutaneous Endoscopic Gastrostomy: Stratification Risk of Pneumonia. JPEN J. Parenter. Enteral Nutr. 2019. [Google Scholar] [CrossRef]
- Scheel, R.; Pisegna, J.M.; McNally, E.; Noordzij, J.P.; Langmore, S.E. Endoscopic Assessment of Swallowing After Prolonged Intubation in the ICU Setting. Ann. Otol. Rhinol. Laryngol. 2016, 125, 43–52. [Google Scholar] [CrossRef]
- Baijens, L.W.; Clave, P.; Cras, P.; Ekberg, O.; Forster, A.; Kolb, G.F.; Leners, J.C.; Masiero, S.; Mateos-Nozal, J.; Ortega, O.; et al. European Society for Swallowing Disorders—European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clin. Interv. Aging 2016, 11, 1403–1428. [Google Scholar] [CrossRef] [Green Version]
- Neubauer, P.D.; Hersey, D.P.; Leder, S.B. Pharyngeal Residue Severity Rating Scales Based on Fiberoptic Endoscopic Evaluation of Swallowing: A Systematic Review. Dysphagia 2016, 31, 352–359. [Google Scholar] [CrossRef]
- Kim, J.; Oh, B.M.; Kim, J.Y.; Lee, G.J.; Lee, S.A.; Han, T.R. Validation of the videofluoroscopic dysphagia scale in various etiologies. Dysphagia 2014, 29, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Teasell, R.W.; McRae, M.; Marchuk, Y.; Finestone, H.M. Pneumonia associated with aspiration following stroke. Arch. Phys. Med. Rehabil. 1996, 77, 707–709. [Google Scholar] [CrossRef]
- Neubauer, P.D.; Rademaker, A.W.; Leder, S.B. The Yale Pharyngeal Residue Severity Rating Scale: An Anatomically Defined and Image-Based Tool. Dysphagia 2015, 30, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.; Langmore, S.E.; Ginsberg, S.; Dostie, A. The significance of accumulated oropharyngeal secretions and swallowing frequency in predicting aspiration. Dysphagia 1996, 11, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Farneti, D.; Fattori, B.; Nacci, A.; Mancini, V.; Simonelli, M.; Ruoppolo, G.; Genovese, E. The Pooling-score (P-score): Inter- and intra-rater reliability in endoscopic assessment of the severity of dysphagia. Acta Otorhinolaryngol. Ital. 2014, 34, 105–110. [Google Scholar] [PubMed]
- Ortega, O.; Martin, A.; Clave, P. Diagnosis and Management of Oropharyngeal Dysphagia Among Older Persons, State of the Art. J. Am. Med. Dir. Assoc. 2017, 18, 576–582. [Google Scholar] [CrossRef]
- Marik, P.E. Aspiration pneumonitis and aspiration pneumonia. N. Engl. J. Med. 2001, 344, 665–671. [Google Scholar] [CrossRef]
- Dziewas, R.; Beck, A.M.; Clave, P.; Hamdy, S.; Heppner, H.J.; Langmore, S.E.; Leischker, A.; Martino, R.; Pluschinski, P.; Roesler, A.; et al. Recognizing the importance of dysphagia: Stumbling blocks and stepping stones in the twenty-first century. Dysphagia 2017, 32, 78–82. [Google Scholar] [CrossRef] [Green Version]
- Granell, J.; Garrido, L.; Millas, T.; Gutierrez-Fonseca, R. Management of oropharyngeal Dysphagia in laryngeal and hypopharyngeal cancer. Int. J. Otolaryngol. 2012, 2012, 157630. [Google Scholar] [CrossRef]
- Srivanitchapoom, P.; Pandey, S.; Hallett, M. Drooling in Parkinson’s disease: A review. Parkinsonism Relat. Disord. 2014, 20, 1109–1118. [Google Scholar] [CrossRef] [Green Version]
- Satou, Y.; Oguro, H.; Murakami, Y.; Onoda, K.; Mitaki, S.; Hamada, C.; Mizuhara, R.; Yamaguchi, S. Gastroesophageal reflux during enteral feeding in stroke patients: A 24-hour esophageal pH-monitoring study. J. Stroke Cerebrovasc. Dis. 2013, 22, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Dziewas, R.; Warnecke, T.; Hamacher, C.; Oelenberg, S.; Teismann, I.; Kraemer, C.; Ritter, M.; Ringelstein, E.B.; Schaebitz, W.R. Do nasogastric tubes worsen dysphagia in patients with acute stroke? BMC Neurol. 2008, 8, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.Y.; Chen, J.M.; Ni, G.X. Effect of an indwelling nasogastric tube on swallowing function in elderly post-stroke dysphagia patients with long-term nasal feeding. BMC Neurol. 2019, 19, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, G.F.; Pisani, J.C.; Macedo, E.D.; Campos, A.C. The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr. Opin. Clin. Nutr. Metab. Care 2003, 6, 327–333. [Google Scholar] [CrossRef]
- Dennis, M.S.; Lewis, S.C.; Warlow, C.; Collaboration, F.T. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): A multicentre randomised controlled trial. Lancet 2005, 365, 764–772. [Google Scholar] [CrossRef]
- Carrion, S.; Cabre, M.; Monteis, R.; Roca, M.; Palomera, E.; Serra-Prat, M.; Rofes, L.; Clave, P. Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin. Nutr. 2015, 34, 436–442. [Google Scholar] [CrossRef]
- Pinto, G.; Zetola, V.; Lange, M.; Gomes, G.; Nunes, M.C.; Hirata, G.; Lagos-Guimaraes, H.N. Program to diagnose probability of aspiration pneumonia in patients with ischemic stroke. Int. Arch. Otorhinolaryngol. 2014, 18, 244–248. [Google Scholar] [CrossRef] [Green Version]
- Komiya, K.; Rubin, B.K.; Kadota, J.I.; Mukae, H.; Akaba, T.; Moro, H.; Aoki, N.; Tsukada, H.; Noguchi, S.; Shime, N.; et al. Prognostic implications of aspiration pneumonia in patients with community acquired pneumonia: A systematic review with meta-analysis. Sci. Rep. 2016, 6, 38097. [Google Scholar] [CrossRef]
- Weir, K.A.; McMahon, S.; Taylor, S.; Chang, A.B. Oropharyngeal aspiration and silent aspiration in children. Chest 2011, 140, 589–597. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.S.; Collard, H.R.; Raghu, G.; Sweet, M.P.; Hays, S.R.; Campos, G.M.; Golden, J.A.; King, T.E., Jr. Does chronic microaspiration cause idiopathic pulmonary fibrosis? Am. J. Med. 2010, 123, 304–311. [Google Scholar] [CrossRef] [Green Version]



| Variable | NGT (n = 130) | PEG (n = 97) | P Value |
|---|---|---|---|
| Age (years) | 67.1 ± 15.2 | 70.4 ± 14.7 | 0.102 |
| Gender | 0.268 | ||
| Female | 51 (39.2%) | 31 (32.0%) | 0.511 |
| Male | 79 (60.8%) | 66 (68.0%) | 0.368 |
| Body mass index (kg/m2) | 21.9 ± 4.1 | 22.3 ± 4.0 | 0.501 |
| Albumin (gm/dl) | 3.1 ± 0.5 | 3.2 ± 0.5 | 0.925 |
| Swallowing level scale score | 2.0 ± 0.9 | 2.1 ± 0.9 | 0.447 |
| Reasons for tube feeding, no (%) | 0.153 | ||
| Esophageal disorders | 48 (36.9%) | 38 (39.2%) | 0.872 |
| Neurological disorders | 50 (38.5%) | 45 (46.4%) | 0.436 |
| Head and neck tumors | 32 (24.6%) | 14 (14.4%) | 0.438 |
| Duration (days) | 741 ± 361 | 785 ± 338 | 0.348 |
| Pooling secretions severity, no (%) | 0.275 | ||
| Control group | 81 (62.3%) | 58 (59.8%) | 0.765 |
| Pharyngeal group | 27 (20.8%) | 15 (15.5%) | 0.674 |
| Laryngeal group | 22 (16.9%) | 24 (24.7%) | 0.516 |
| Occurrence of pneumonia, no (%) | 46 (35.4%) | 31 (32.0%) | 0.671 |
| Incidence of pneumonia (episodes/person-years) | 2.3 ± 3.4 | 2.0 ± 3.1 | 0.225 |
| Pooling Secretions Severity | NGT (n = 130) | PEG (n = 97) | Crude Odds Ratio (95% CI) | P Value | Adjusted Odds Ratio (95% CI) | P Value |
|---|---|---|---|---|---|---|
| Control group | 81 (62.3%) | 58 (59.8%) | Reference | Reference | ||
| Pharynx group | 27 (20.8%) | 15 (15.5%) | 1.35 (0.68–2.71) | 0.395 | 1.04 (0.39–2.78) | 0.935 |
| Larynx group | 22 (16.9%) | 24 (24.7%) | 1.73 (0.87–3.43) | 0.116 | 1.59 (0.68–3.75) | 0.285 |
| Variable | NGT (n = 130) | PEG (n = 97) | P Value |
|---|---|---|---|
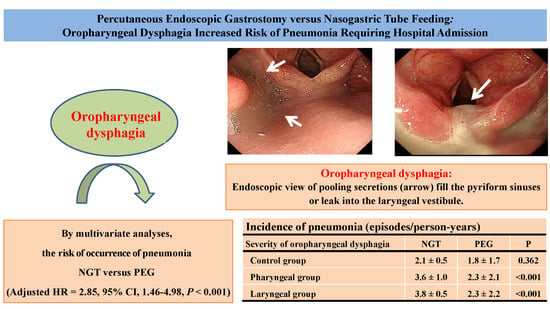
| Incidence of pneumonia (episodes/person-years) | |||
| Control group | 2.1 ± 0.5 | 1.8 ± 1.7 | 0.362 |
| Pharyngeal group | 3.6 ± 1.0 | 2.3 ± 2.1 | <0.001 |
| Laryngeal group | 3.8 ± 0.5 | 2.3 ± 2.2 | <0.001 |
| Variable | With Pneumonia (n = 77) | Without Pneumonia (n = 150) | Crude Odds Ratio (95% CI) | P Value | Adjusted Odds Ratio (95% CI) | P Value |
|---|---|---|---|---|---|---|
| Age (years) | 70.6 ± 14.3 | 67.4 ± 15.4 | 1.05 (0.92–1.09) | 0.126 | 1.03 (0.98–1.05) | 0.129 |
| Gender | ||||||
| Female | 25 (32.5%) | 57 (38.0%) | Reference | Reference | ||
| Male | 52 (67.5%) | 93 (62.0%) | 1.28 (0.71–2.28) | 0.467 | 1.21 (0.55–2.14) | 0.426 |
| NGT vs. PEG | ||||||
| PEG | 31 (40.3%) | 66 (44.0%) | Reference | Reference | ||
| NGT | 46 (59.7%) | 84 (56.0%) | 2.88 (1.63–5.08) | <0.001 | 2.85 (1.46–4.98) | <0.001 |
| Body mass index (kg/m2) | 21.6 ± 4.2 | 22.3 ± 4.0 | 0.97 (0.91–1.04) | 0.223 | 0.99 (0.91–1.08) | 0.835 |
| Albumin (gm/dL) | 3.1 ± 0.5 | 3.4 ± 0.6 | 0.36 (0.21–0.65) | 0.002 | 0.49 (0.21–1.43) | 0.168 |
| Swallowing level scale score | 2.0 ± 1.3 | 3.1 ± 2.3 | 0.72 (0.60–0.88) | 0.001 | 0.91 (0.70–1.18) | 0.433 |
| Reasons for feeding tube, no (%) | ||||||
| Esophageal disorders | 17 (22.1%) | 69 (46.0%) | 0.48 (0.28–0.85) | 0.004 | 0.35 (0.17–0.77) | 0.010 |
| Neurological disorders | 39 (50.6%) | 56 (37.3%) | 1.36 (1.11–2.78) | 0.001 | 1.27 (1.09–2.31) | 0.042 |
| Head and neck tumors | 21 (27.3%) | 25 (16.7%) | 1.63 (1.20–2.94) | 0.001 | 1.34 (1.10–2.45) | 0.038 |
| Pooling secretions severity, no (%) | ||||||
| Control group | 32 (41.6%) | 107 (71.3%) | Reference | Reference | ||
| Pharynx group | 23 (29.8%) | 23 (15.3%) | 3.34 (1.57–6.66) | 0.001 | 1.24 (0.99–2.08) | 0.051 |
| Larynx group | 22 (28.6%) | 20 (13.4%) | 3.66 (1.63–7.99) | 0.001 | 1.73 (1.16–2.24) | 0.023 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, W.-K.; Huang, H.-H.; Lin, H.-H.; Tsai, C.-L. Percutaneous Endoscopic Gastrostomy versus Nasogastric Tube Feeding: Oropharyngeal Dysphagia Increases Risk for Pneumonia Requiring Hospital Admission. Nutrients 2019, 11, 2969. https://doi.org/10.3390/nu11122969
Chang W-K, Huang H-H, Lin H-H, Tsai C-L. Percutaneous Endoscopic Gastrostomy versus Nasogastric Tube Feeding: Oropharyngeal Dysphagia Increases Risk for Pneumonia Requiring Hospital Admission. Nutrients. 2019; 11(12):2969. https://doi.org/10.3390/nu11122969
Chicago/Turabian StyleChang, Wei-Kuo, Hsin-Hung Huang, Hsuan-Hwai Lin, and Chen-Liang Tsai. 2019. "Percutaneous Endoscopic Gastrostomy versus Nasogastric Tube Feeding: Oropharyngeal Dysphagia Increases Risk for Pneumonia Requiring Hospital Admission" Nutrients 11, no. 12: 2969. https://doi.org/10.3390/nu11122969
APA StyleChang, W.-K., Huang, H.-H., Lin, H.-H., & Tsai, C.-L. (2019). Percutaneous Endoscopic Gastrostomy versus Nasogastric Tube Feeding: Oropharyngeal Dysphagia Increases Risk for Pneumonia Requiring Hospital Admission. Nutrients, 11(12), 2969. https://doi.org/10.3390/nu11122969