Examining Constructs of Parental Reflective Motivation towards Reducing Unhealthy Food Provision to Young Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Settings and Participants
2.2. Variables
2.3. Measurement Tools
2.4. Data Collection Procedure, Bias, and Sample Size
2.5. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Stage One: Measurement Stage of Structural Equation Modelling
Motivational Latent Constructs
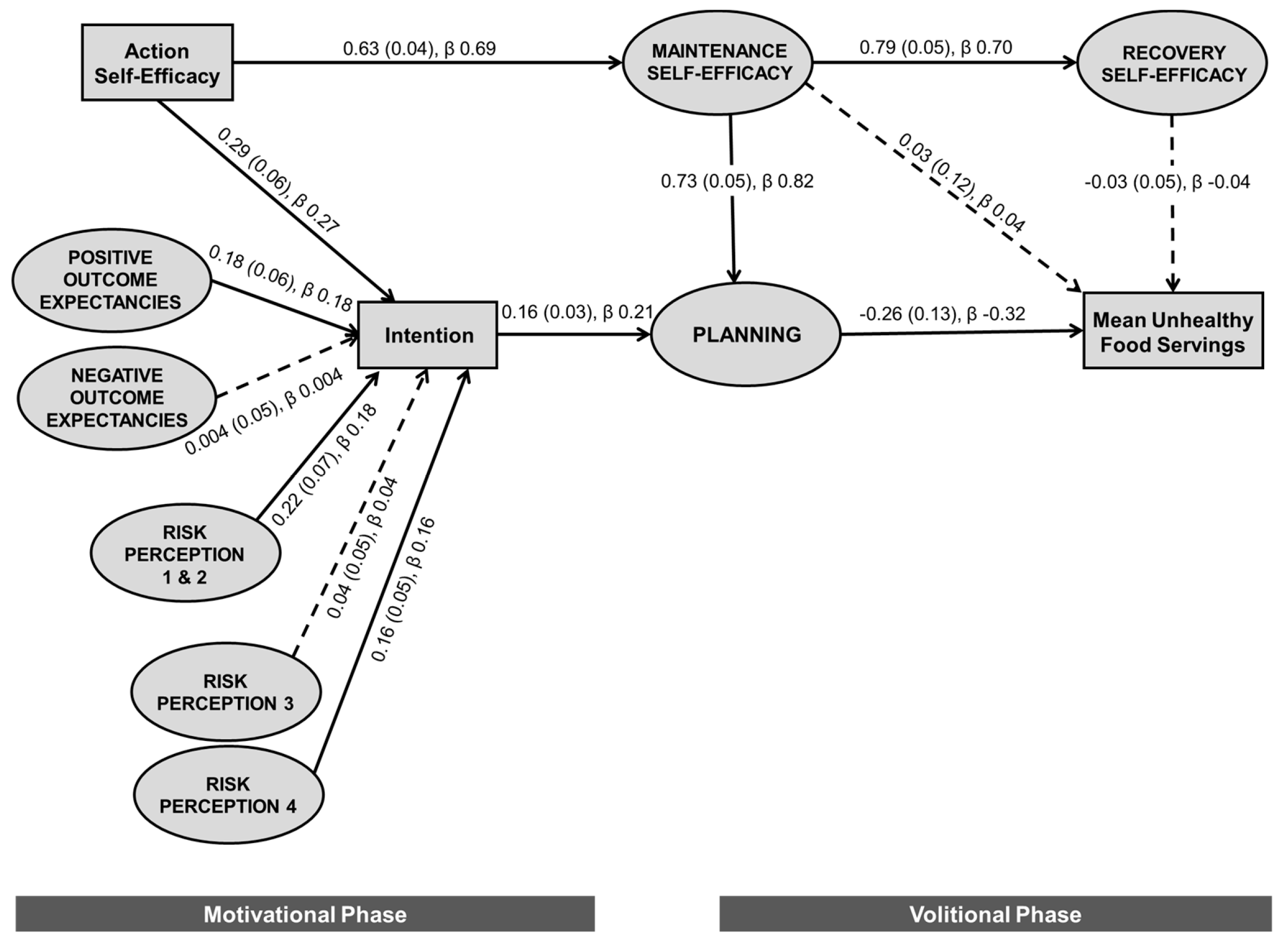
3.3. Stage Two: Structural Stage of Structural Equation Modelling
3.3.1. Confirming the Health Action Process Approach Structural Model
3.3.2. Exploring the Intention–Behavior Gap
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Future Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Bureau of Statistics. Australian Health Survey: Nutrition First Results - Foods and Nutrients, 2011-12. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.007main+features12011-12 (accessed on 3 September 2014).
- Johnson, B.J.; Bell, L.K.; Zarnowiecki, D.; Rangan, A.M.; Golley, R.K. Contribution of Discretionary Foods and Drinks to Australian Children’s Intake of Energy, Saturated Fat, Added Sugars and Salt. Children (Basel) 2017, 4, 104. [Google Scholar] [CrossRef] [PubMed]
- Mihrshahi, S.; Myton, R.; Partridge, S.R.; Esdaile, E.; Hardy, L.L.; Gale, J. Sustained low consumption of fruit and vegetables in Australian children: Findings from the Australian National Health Surveys. Health Promot. J. Austr. 2019, 30, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 2013, 113, 569–580. [Google Scholar] [CrossRef] [Green Version]
- Johnson, B.J.; Hendrie, G.A.; Golley, R. Reducing discretionary food and beverage intake in early childhood: A systematic review within an ecological framework. Public Health Nutr. 2016, 19, 1684–1695. [Google Scholar] [CrossRef]
- Schrempft, S.; van Jaarsveld, C.H.; Fisher, A.; Wardle, J. The Obesogenic Quality of the Home Environment: Associations with Diet, Physical Activity, TV Viewing, and BMI in Preschool Children. PLoS ONE 2015, 10, e0134490. [Google Scholar] [CrossRef]
- Yee, A.Z.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions; Silverback Publishing: Great Britain, UK, 2014. [Google Scholar]
- Van Allen, J.; Kuhl, E.S.; Filigno, S.S.; Clifford, L.M.; Connor, J.M.; Stark, L.J. Changes in parent motivation predicts changes in body mass index z-score (zBMI) and dietary intake among preschoolers enrolled in a family-based obesity intervention. J. Pediatr. Psychol. 2014, 39, 1028–1037. [Google Scholar] [CrossRef]
- Tipton, J.A. Using the Theory of Planned Behavior to understand caregivers’ intention to serve sugar-sweetened beverages to non-Hispanic Black preschoolers. J. Pediatr. Nurs. 2014, 29, 564–575. [Google Scholar] [CrossRef]
- Andrews, K.R.; Silk, K.S.; Eneli, I.U. Parents as health promoters: A theory of planned behavior perspective on the prevention of childhood obesity. J. Health Commun. 2010, 15, 95–107. [Google Scholar] [CrossRef]
- Arsenault, L.N.; Xu, K.; Taveras, E.M.; Hacker, K.A. Parents’ Obesity-Related Behavior and Confidence to Support Behavioral Change in Their Obese Child: Data From the STAR Study. Acad. Pediatr. 2014, 14, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.; Hesketh, K.; Silverii, A.; Abbott, G. Maternal self-efficacy regarding children’s eating and sedentary behaviours in the early years: Associations with children’s food intake and sedentary behaviours. Int. J. Pediatr. Obes. 2010, 5, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Taveras, E.M.; Mitchell, K.; Gortmaker, S.L. Parental confidence in making overweight-related behavior changes. Pediatrics 2009, 124, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R. Modeling Health Behavior Change: How to Predict and Modify the Adoption and Maintenance of Health Behaviors. Appl. Psychol. 2008, 57, 1–29. [Google Scholar] [CrossRef]
- McEachan, R.R.C.; Conner, M.; Taylor, N.J.; Lawton, R.J. Prospective prediction of health-related behaviours with the Theory of Planned Behaviour: A meta-analysis. Health Psychol. Rev. 2011, 5, 97–144. [Google Scholar] [CrossRef]
- Zoellner, J.M.; Porter, K.J.; Chen, Y.; Hedrick, V.E.; You, W.; Hickman, M.; Estabrooks, P.A. Predicting sugar-sweetened behaviours with theory of planned behaviour constructs: Outcome and process results from the SIPsmartER behavioural intervention. Psychol. Health 2017, 32, 509–529. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Dec. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Australian Dietary Guidelines. Available online: https://www.nhmrc.gov.au/about-us/publications/australian-dietary-guidelines (accessed on 28 August 2015).
- Blaine, R.E.; Kachurak, A.; Davison, K.K.; Klabunde, R.; Fisher, J.O. Food parenting and child snacking: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 146. [Google Scholar] [CrossRef]
- Campbell, K.; Abbott, G.; Spence, A.C.; Crawford, D.A.; McNaughton, S.A.; Ball, K. Home food availability mediates associations between mothers’ nutrition knowledge and child diet. Appetite 2013, 71, 1–6. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Viner Smith, E.; Golley, R.K. The reliability and relative validity of a diet index score for 4-11-year-old children derived from a parent-reported short food survey. Public Health Nutr. 2014, 17, 1486–1497. [Google Scholar] [CrossRef]
- Johnson, B.J.; Zarnowiecki, D.; Hendrie, G.A.; Golley, R.K. Predictors of parental discretionary choice provision using the health action process approach framework: Development and validation of a self-reported questionnaire for parents of 4-7-year-olds. Nutr. Diet. 2018, 75, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Hendrie, G.A.; Cox, D.N.; Coveney, J. Validation of the General Nutrition Knowledge Questionnaire in an Australian community sample. Nutr. Diet. 2008, 65, 72–77. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. How Australia Takes a Census. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/2903.0 (accessed on 12 August 2014).
- Zarnowiecki, D.; Ball, K.; Parletta, N.; Dollman, J. Describing socioeconomic gradients in children’s diets—does the socioeconomic indicator used matter? Int. J. Behav. Nutr. Phys. 2014, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Obesity: Preventing and Managing the Global Epidemic; World Health Organisation: Geneva, Switzerland, 2000. [Google Scholar]
- Pan, H.; Cole, T.J. LMSgrowth, a Microsoft Excel Add-In to Access Growth References Based on the LMS Method. 2.2 ed. 2017. Available online: https://www.healthforallchildren.co.uk/.2007(accessed on 1 July 2019).
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1246. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Socio-economic Indexes for Areas (SEIFA) 2011. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2033.0.55.001Main+Features12011? (accessed on 28 August 2015).
- Australian Bureau of Statistics. Postcode 2012 to Remoteness Area 2011 in 1270.0.55.006—Australian Statistical Geography Standard (ASGS): Correspondences, July 2011. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1270.0.55.006Main+Features1July%202011? (accessed on 8 June 2017).
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Hendrie, G.A.; Coveney, J.; Cox, D.N. Defining the complexity of childhood obesity and related behaviours within the family environment using structural equation modelling. Public Health Nutr. 2011, 15, 48–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khine, M.S. (Ed.) Application of Structural Equation Modelling in Education Research and Practice; Sense Publishers: Rotterdam, The Netherlands, 2013. [Google Scholar]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling, 2nd ed.; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 2004. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modelling with AMOS: Basic concepts, applications, and programming; Lawrence Erlbaum Associates Inc.: Mahwah, NJ, USA, 2001. [Google Scholar]
- Barg, C.J.; Latimer, A.E.; Pomery, E.A.; Rivers, S.E.; Rench, T.A.; Prapavessis, H.; Salovey, P. Examining predictors of physical activity among inactive middle-aged women: An application of the health action process approach. Psychol. Health 2012, 27, 829–845. [Google Scholar] [CrossRef] [Green Version]
- Parschau, L.; Barz, M.; Richert, J.; Knoll, N.; Lippke, S.; Schwarzer, R. Physical activity among adults with obesity: Testing the Health Action Process Approach. Rehabil. Psychol. 2014, 59, 42–49. [Google Scholar] [CrossRef]
- Renner, B.; Kwon, S.; Yang, B.H.; Paik, K.C.; Kim, S.H.; Roh, S.; Song, J.; Schwarzer, R. Social-cognitive predictors of dietary behaviors in South Korean men and women. Int. J. Behav. Med. 2008, 15, 4–13. [Google Scholar] [CrossRef] [Green Version]
- Riebl, S.K.; MacDougal, C.; Hill, C.; Estabrooks, P.A.; Dunsmore, J.C.; Savla, J.; Frisard, M.I.; Dietrich, A.M.; Davy, B.M. Beverage choices of adolescents and their parents using the Theory of Planned Behavior: A mixed methods analysis. J. Acad. Nutr. Diet. 2016, 116, 226–239 e221. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Schuz, B.; Ziegelmann, J.P.; Lippke, S. Adoption and Maintenance of Four Health Behaviors: Theory-Guided Longitudinal Studies on Dental Flossing, Seat Belt Use, Dietary Behavior, and Physical Activity. Ann. Behav. Med. 2007, 33, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Verhoeven, A.A.; Adriaanse, M.A.; de Vet, E.; Fennis, B.M.; de Ridder, D.T. Identifying the ‘if’ for ‘if-then’ plans: Combining implementation intentions with cue-monitoring targeting unhealthy snacking behaviour. Psychol. Health 2014, 29, 1476–1492. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 2011 Census QuickStats. Available online: http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/0 (accessed on 28 August 2015).
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall International Inc.: Upper Saddle River, NJ, USA, 1986. [Google Scholar]
- Rylatt, L.; Cartwright, T. Parental feeding behaviour and motivations regarding pre-school age children: A thematic synthesis of qualitative studies. Appetite 2016, 99, 285–297. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Parent | Characteristic | Child |
|---|---|---|---|
| Age, years (mean, SD) | 36.8 (5.3) | Age, years (mean, SD) | 5.3 (1.3) |
| Gender (%, count) | Gender (%, count) | ||
| Male | 5.1 (25) | Male | 47.5 (235) |
| Female | 94.9 (470) | Female | 52.5 (260) |
| BMI 1 (mean, SD) | 26.0 (5.5) | BMI z-score (mean, SD) | −0.15 (1.97) |
| Weight status (%, count) | Weight status (%, count) | ||
| Underweight | 1.3 (6) | Underweight | 22.8 (107) |
| Healthy weight | 52.7 (252) | Healthy weight | 57.4 (270) |
| Overweight | 28.0 (134) | Overweight | 12.1 (57) |
| Obesity | 18.0 (86) | Obesity | 7.7 (36) |
| Number of children living at home (<18 years old) (%, count) | Education setting attendance (%, count) | ||
| Child care center | 22.9 (122) | ||
| 1 | 16.4 (81) | Family day care | 1.9 (10) |
| 2 | 54.9 (272) | Kindergarten | 21.1 (112) |
| 3 | 22.2 (110) | Primary school | 50.4 (268) |
| 4 or more | 6.4 (32) | n/a 5 | 3.8 (20) |
| Relationship to child (%, count) | Median (IQR) mean servings of unhealthy foods | 2.7 (2.7) | |
| Mother | 93.5 (463) | ||
| Father | 5.1 (25) | ||
| Caregiver or other | 1.4 (7) | ||
| Marital status (%, count) | Residential area (%, count) | ||
| Married/Living as married | 90.3 (447) | Metropolitan | 73.1 (362) |
| Single/Separated | 9.7 (48) | Non-metropolitan | 26.9 (133) |
| Education level (%, count) | |||
| High school completion or below | 7.6 (38) | ||
| Tech or trade qualification | 18.6 (92) | ||
| Tertiary degree or higher | 73.7 (365) | ||
| Employment status (%, count) | |||
| Employed | 68.7 (340) | ||
| Not in the workforce 2 | 31.3 (155) | ||
| Annual household income 3 (%, count) | |||
| Less than $52,000 | 14.4 (64) | ||
| $52,000 to $103,999 | 33.4 (149) | ||
| $104,000 and over | 52.3 (233) | ||
| SEIFA 4 Index of Advantage and Disadvantage (%, count) | |||
| Low | 19.2 (95) | ||
| Medium | 33.4 (165) | ||
| High | 47.4 (234) |
| Latent Constructs | Factor Loading 1 | |
|---|---|---|
| Items | β | Unstandardized Coefficient (SE) |
| Risk perception 1—absolute risk | ||
| child’s activity levels | 0.793 | 0.779 (0.044) |
| child’s overall diet | 0.878 | 0.952 (0.044) |
| Risk perception 2—absolute risk | ||
| other children the same age | 0.888 | 0.918 (0.039) |
| other children the same size | 0.916 | 0.912 (0.037) |
| Risk perception 3—severity assessment | ||
| being overweight | 0.749 | 0.823 (0.045) |
| tooth decay | 0.753 | 0.614 (0.033) |
| behavioral issues | 0.789 | 0.709 (0.036) |
| too much energy and associated nutrients | 0.794 | 0.733 (0.037) |
| Risk perception 4 2—risk for child | ||
| becoming overweight | 0.927 | 0.879 (0.093) |
| developing tooth decay | 0.687 | 0.556 (0.063) |
| Positive outcome expectancies | ||
| be healthy | 0.649 | 0.530 (0.038) |
| healthy eating habits | 0.736 | 0.552 (0.034) |
| eat more fruit and vegetables | 0.764 | 0.735 (0.044) |
| environmentally-friendly | 0.380 | 0.331 (0.043) |
| Negative outcome expectancies | ||
| throw a tantrum or pester | 0.569 | 0.504 (0.044) |
| miss out on having treats | 0.582 | 0.410 (0.035) |
| affect family time | 0.564 | 0.404 (0.036) |
| overeat unhealthy foods when available | 0.565 | 0.482 (0.043) |
| miss out on eating what their friends eat | 0.602 | 0.465 (0.038) |
| Latent Constructs | Factor Loading 1 | |
|---|---|---|
| Items | β | Unstandardized Coefficient (SE) |
| Maintenance self-efficacy 1 | ||
| partner is undermining you | 0.697 | 0.733 (0.043) |
| financial pressures | 0.792 | 0.752 (0.037) |
| school/child care holidays | 0.750 | 0.689 (0.037) |
| takes a long time to make it habit | 0.749 | 0.666 (0.036) |
| food marketing on television | 0.659 | 0.626 (0.040) |
| family time | 0.609 | 0.562 (0.039) |
| Maintenance self-efficacy 2 | ||
| child is pestering for unhealthy foods | 0.936 | 0.822 (0.031) |
| child is resistant to limiting unhealthy foods | 0.949 | 0.819 (0.030) |
| Maintenance self-efficacy 3 | ||
| you are tired | 0.944 | 0.902 (0.033) |
| having a very busy day | 0.921 | 0.874 (0.033) |
| Action planning | ||
| weekdays | 0.914 | 0.805 (0.033) |
| weekend days | 0.845 | 0.775 (0.035) |
| packing lunchbox | 0.696 | 0.570 (0.034) |
| takeaway meals and snacks | 0.612 | 0.587 (0.041) |
| Coping planning 1 | ||
| friends undermine my plans | 0.924 | 0.877 (0.036) |
| relatives undermine my plans | 0.813 | 0.738 (0.036) |
| Coping planning 2 | ||
| certain situations | 0.768 | 0.689 (0.037) |
| set-backs when unhealthy foods have been provided | 0.863 | 0.791 (0.037) |
| Recovery self-efficacy 2 | ||
| small relapse (2 days) | 0.793 | 0.661 (0.032) |
| moderate relapse (2-6 weeks) | 0.927 | 0.785 (0.030) |
| large relapse (weeks-months) | 0.846 | 0.763 (0.034) |
| Higher Order Construct | Factor Loading | |
|---|---|---|
| First Order Constructs | β | Unstandardized Coefficient (SE) |
| Risk perception | ||
| Risk perception 1—absolute risk | 0.894 | 0.893 (0.054) |
| Risk perception 2—absolute risk | 0.820 | 0.819 (0.052) |
| Maintenance self-efficacy | ||
| Maintenance self-efficacy 1 | 0.912 | 0.911 (0.041) |
| Maintenance self-efficacy 2 | 0.845 | 0.844 (0.040) |
| Maintenance self-efficacy 3 | 0.797 | 0.796 (0.041) |
| Planning | ||
| Action planning | 0.783 | 0.782 (0.046) |
| Coping planning 1 | 0.600 | 0.599 (0.050) |
| Coping planning 2 | 0.837 | 0.835 (0.048) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnson, B.J.; Hendrie, G.A.; Zarnowiecki, D.; Huynh, E.K.; Golley, R.K. Examining Constructs of Parental Reflective Motivation towards Reducing Unhealthy Food Provision to Young Children. Nutrients 2019, 11, 1507. https://doi.org/10.3390/nu11071507
Johnson BJ, Hendrie GA, Zarnowiecki D, Huynh EK, Golley RK. Examining Constructs of Parental Reflective Motivation towards Reducing Unhealthy Food Provision to Young Children. Nutrients. 2019; 11(7):1507. https://doi.org/10.3390/nu11071507
Chicago/Turabian StyleJohnson, Brittany J., Gilly A. Hendrie, Dorota Zarnowiecki, Elisabeth K. Huynh, and Rebecca K. Golley. 2019. "Examining Constructs of Parental Reflective Motivation towards Reducing Unhealthy Food Provision to Young Children" Nutrients 11, no. 7: 1507. https://doi.org/10.3390/nu11071507
APA StyleJohnson, B. J., Hendrie, G. A., Zarnowiecki, D., Huynh, E. K., & Golley, R. K. (2019). Examining Constructs of Parental Reflective Motivation towards Reducing Unhealthy Food Provision to Young Children. Nutrients, 11(7), 1507. https://doi.org/10.3390/nu11071507






