The Sex–Gender Effects in the Road to Tailored Botanicals
Abstract
1. Introduction
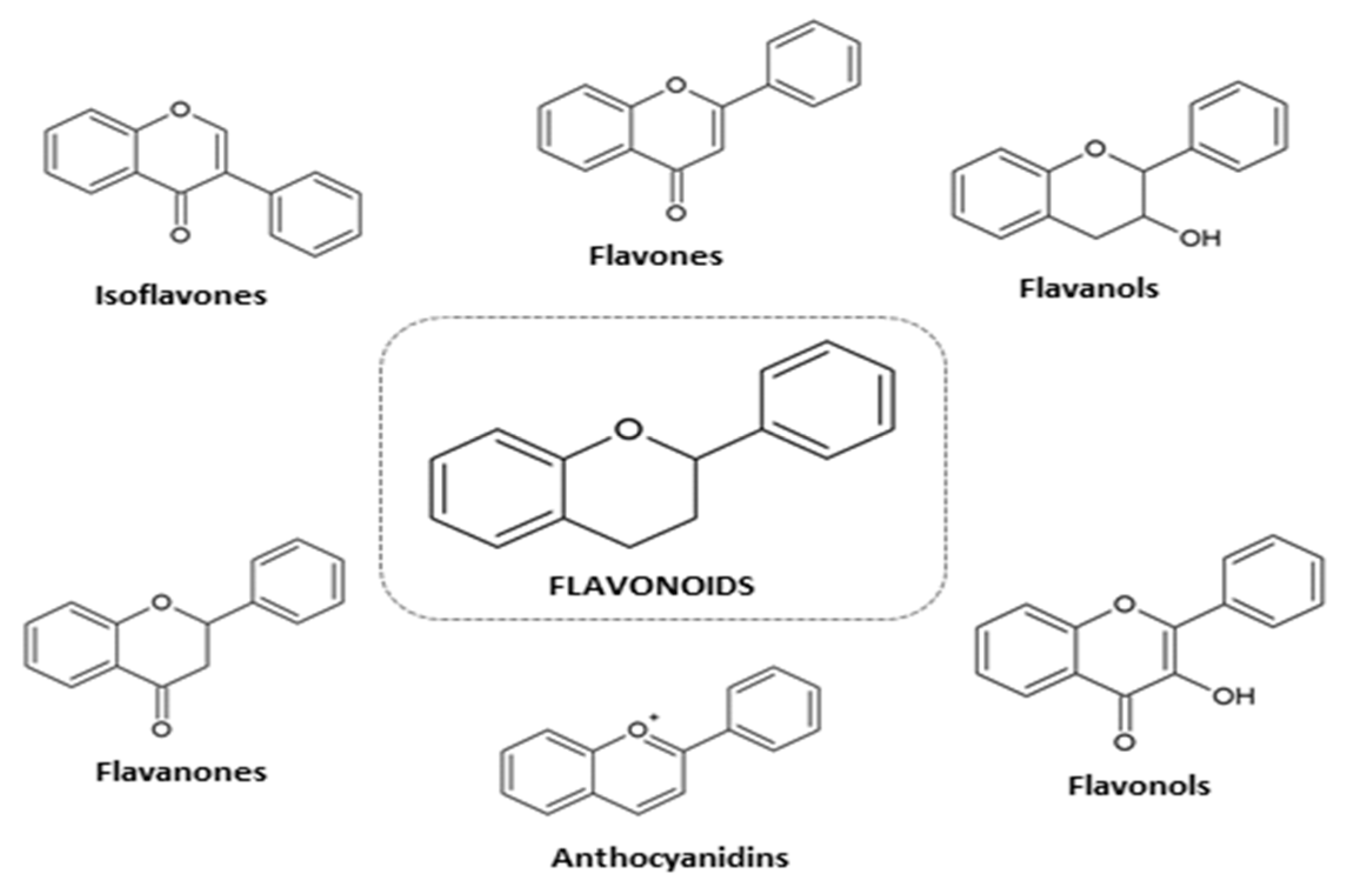
2. Plant Materials
3. Sex Differences in Plants
4. Pharmacokinetics of Phenols: Influence of Sex–Gender
4.1. Absorption
4.2. Metabolism
4.3. Distribution
4.4. Elimination
5. Microbiota
6. Interactions
7. Development: Pregnancy, Lactation, and Developmental Trajectory
7.1. Pregnancy
7.2. Lactation
7.3. Galactagogues Based on Herbs
7.4. Breast Milk
7.5. Soy-Milk Formula
7.6. Developmental Trajectory
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Barnes, P.M.; Bloom, B.; Nahin, R.L. Complementary and alternative medicine use among adults and children: United States, 2007. Natl. Health Stat. Rep. 2008, 12, 1–23. [Google Scholar]
- Matulka, R.A. Dietary Supplements in the U.S. and Abroad: Similarities and Differences; Burdock Group: Orlando, FL, USA, 2016. [Google Scholar]
- Smith, T.; Kawa, K.; Eckl, V.; Morton, C.; Stredney, R. Herbal supplement sales in US increased 8.5% in 2017, topping $8 billion. HerbalGram 2018, 119, 62–71. [Google Scholar]
- National Institute of Health. Dietary Supplement Label Database. Available online: https://dsld.nlm.nih.gov/dsld/ (accessed on 25 November 2018).
- National Institute of Health. Complementary, Alternative, or Integrative Health: What’s in a Name? National Center for Complementary and Integrative Medicine, Ed.; NCCIH: Washington, DC, USA, 2016.
- Dietz, B.M.; Hajirahimkhan, A.; Dunlap, T.L.; Bolton, J.L. Botanicals and their bioactive phytochemicals for women’s health. Pharmacol. Rev. 2016, 68, 1026–1073. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. What Is Gender? What Is Sex? Canadian Institutes of Health Research. Available online: http://www.cihr-irsc.gc.ca/e/48642.html (accessed on 26 April 2019).
- WHO. Gender, Equity and Human Rights. Available online: https://www.who.int/gender-equity-rights/understanding/gender-definition/en/ (accessed on 26 April 2019).
- European Institute for Gender Equality. Concepts and Definitions. Available online: https://eige.europa.eu/gender-mainstreaming/concepts-and-definitions (accessed on 26 April 2019).
- Australian Government. Australian Government Guidelines on the Recognition of Sex and Gender Attorney General’s Department. Available online: https://www.ag.gov.au/Pages/default.aspx (accessed on 26 April 2019).
- Marino, M.; Masella, R.; Bulzomi, P.; Campesi, I.; Malorni, W.; Franconi, F. Nutrition and human health from a sex-gender perspective. Mol. Asp. Med. 2011, 32, 1–70. [Google Scholar] [CrossRef] [PubMed]
- Regitz-Zagrosek, V. Sex and Gender Differences in Pharmacology; Springer: Berlin, Germany, 2012; Volume 214. [Google Scholar]
- Rienks, J.; Barbaresko, J.; Nothlings, U. Association of isoflavone biomarkers with risk of chronic disease and mortality: A systematic review and meta-analysis of observational studies. Nutr. Rev. 2017, 75, 616–641. [Google Scholar] [CrossRef] [PubMed]
- Rietjens, I.; Louisse, J.; Beekmann, K. The potential health effects of dietary phytoestrogens. Br. J. Pharmacol. 2017, 174, 1263–1280. [Google Scholar] [CrossRef]
- Cory, H.; Passarelli, S.; Szeto, J.; Tamez, M.; Mattei, J. The role of polyphenols in human health and food systems: A mini-review. Front. Nutr. 2018, 5, 87. [Google Scholar] [CrossRef]
- Tresserra-Rimbau, A.; Lamuela-Raventos, R.M.; Moreno, J.J. Polyphenols, food and pharma. Current knowledge and directions for future research. Biochem. Pharmacol. 2018, 156, 186–195. [Google Scholar] [CrossRef]
- Kim, Y.S.; Unno, T.; Kim, B.-Y.; Park, M.-S. Sex differences in gut microbiota. World J. Mens Health 2019, 37, e15. [Google Scholar] [CrossRef]
- Elderman, M.; de Vos, P.; Faas, M. Role of microbiota in sexually dimorphic immunity. Front. Immunol. 2018, 9, 1018. [Google Scholar] [CrossRef]
- Campesi, I.; Marino, M.; Cipolletti, M.; Romani, A.; Franconi, F. Put “gender glasses” on the effects of phenolic compounds on cardiovascular function and diseases. Eur. J. Nutr. 2018, 57, 2677–2691. [Google Scholar] [CrossRef] [PubMed]
- Corella, D.; Coltell, O.; Portoles, O.; Sotos-Prieto, M.; Fernandez-Carrion, R.; Ramirez-Sabio, J.B.; Zanon-Moreno, V.; Mattei, J.; Sorli, J.V.; Ordovas, J.M. A guide to applying the sex-gender perspective to nutritional genomics. Nutrients 2018, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.N.; Barker, D.J.; Clark, P.M.; Cox, L.J.; Fall, C.; Osmond, C.; Winter, P.D. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ 1991, 303, 1019–1022. [Google Scholar] [CrossRef]
- Weng, J.K. The evolutionary paths towards complexity: A metabolic perspective. New Phytol. 2014, 201, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, S.; Piccolella, S.; Galasso, S.; Fiorentino, A.; Kretschmer, N.; Pan, S.P.; Bauer, R.; Monaco, P. Influence of harvest season on chemical composition and bioactivity of wild rue plant hydroalcoholic extracts. Food Chem. Toxicol. 2016, 90, 102–111. [Google Scholar] [CrossRef]
- Rieger, G.; Muller, M.; Guttenberger, H.; Bucar, F. Influence of altitudinal variation on the content of phenolic compounds in wild populations of Calluna vulgaris, Sambucus nigra, and Vaccinium myrtillus. J. Agric. Food Chem. 2008, 56, 9080–9086. [Google Scholar] [CrossRef] [PubMed]
- Schilter, B.; Andersson, C.; Anton, R.; Constable, A.; Kleiner, J.; O’Brien, J.; Renwick, A.G.; Korver, O.; Smit, F.; Walker, R. Guidance for the safety assessment of botanicals and botanical preparations for use in food and food supplements. Food Chem. Toxicol. 2003, 41, 1625–1649. [Google Scholar] [CrossRef]
- Simpraga, M.; Takabayashi, J.; Holopainen, J.K. Language of plants: Where is the word? J. Integr. Plant Biol. 2016, 58, 343–349. [Google Scholar] [CrossRef]
- Dicke, M.; van Loon, J.J.; Soler, R. Chemical complexity of volatiles from plants induced by multiple attack. Nat. Chem. Biol. 2009, 5, 317–324. [Google Scholar] [CrossRef]
- Perez-Jimenez, J.; Fezeu, L.; Touvier, M.; Arnault, N.; Manach, C.; Hercberg, S.; Galan, P.; Scalbert, A. Dietary intake of 337 polyphenols in French adults. Am. J. Clin. Nutr. 2011, 93, 1220–1228. [Google Scholar] [CrossRef]
- Jefferson, W.N.; Patisaul, H.B.; Williams, C.J. Reproductive consequences of developmental phytoestrogen exposure. Reproduction 2012, 143, 247–260. [Google Scholar] [CrossRef]
- Romani, A.; Lapucci, C.; Cantini, C.; Ieri, F.; Mulinacci, N.; Visioli, F. Evolution of minor polar compounds and antioxidant capacity during storage of bottled extra virgin olive oil. J. Agric. Food Chem. 2007, 55, 1315–1320. [Google Scholar] [CrossRef]
- Rodriguez-Morato, J.; Boronat, A.; Kotronoulas, A.; Pujadas, M.; Pastor, A.; Olesti, E.; Perez-Mana, C.; Khymenets, O.; Fito, M.; Farre, M.; et al. Metabolic disposition and biological significance of simple phenols of dietary origin: Hydroxytyrosol and tyrosol. Drug Metab. Rev. 2016, 48, 218–236. [Google Scholar] [CrossRef]
- Zimmermann, P.; Zentgraf, U. The correlation between oxidative stress and leaf senescence during plant development. Cell. Mol. Biol. Lett. 2005, 10, 515–534. [Google Scholar]
- Ben Ahmed, Z.; Yousfi, M.; Viaene, J.; Dejaegher, B.; Demeyer, K.; Mangelings, D.; Vander Heyden, Y. Seasonal, gender and regional variations in total phenolic, flavonoid, and condensed tannins contents and in antioxidant properties from Pistacia atlantica ssp. leaves. Pharm. Biol. 2017, 55, 1185–1194. [Google Scholar] [CrossRef]
- Ruuhola, T.; Nybakken, L.; Randriamanana, T.; Lavola, A.; Julkunen-Tiitto, R. Effects of long-term UV-exposure and plant sex on the leaf phenoloxidase activities and phenolic concentrations of Salix myrsinifolia (Salisb.). Plant Physiol. Biochem. 2018, 126, 55–62. [Google Scholar] [CrossRef]
- Xu, X.; Zhao, H.; Zhang, X.; Hanninen, H.; Korpelainen, H.; Li, C. Different growth sensitivity to enhanced UV-B radiation between male and female Populus cathayana. Tree Physiol. 2010, 30, 1489–1498. [Google Scholar] [CrossRef]
- Koczka, N.; Moczar, Z.; Stefanovits-Banyai, E.; Ombodi, A. Differences in antioxidant properties of ginkgo leaves collected from male and female trees. Acta Pharm. 2015, 65, 99–104. [Google Scholar] [CrossRef]
- Galambosi, B.; Galambosi, Z.S.; Slacanin, I. Comparison of natural and cultivated roseroot (Rhodiola rosea L.) roots in Finland. J. Med. Spice Plants 2007, 12, 141–147. [Google Scholar]
- Wang, L.; Sun, R.; Zhang, Q.; Luo, Q.; Zeng, S.; Li, X.; Gong, X.; Li, Y.; Lu, L.; Hu, M.; et al. An update on polyphenol disposition via coupled metabolic pathways. Expert Opin. Drug Metab. Toxicol. 2019, 15, 151–165. [Google Scholar] [CrossRef]
- Morton, M.S.; Arisaka, O.; Miyake, N.; Morgan, L.D.; Evans, B.A. Phytoestrogen concentrations in serum from Japanese men and women over forty years of age. J. Nutr. 2002, 132, 3168–3171. [Google Scholar] [CrossRef]
- Franconi, F.; Campesi, I. Pharmacogenomics, pharmacokinetics and pharmacodynamics: Interaction with biological differences between men and women. Br. J. Pharmacol. 2014, 171, 580–594. [Google Scholar] [CrossRef]
- Franconi, F.; Campesi, I. Sex and gender influences on pharmacological response: An overview. Expert Rev. Clin. Pharmacol. 2014, 7, 469–485. [Google Scholar] [CrossRef]
- Yang, L.; Li, Y.; Hong, H.; Chang, C.W.; Guo, L.W.; Lyn-Cook, B.; Shi, L.; Ning, B. Sex Differences in the expression of drug-metabolizing and transporter genes in human liver. J. Drug Metab. Toxicol. 2012, 3, 1000119. [Google Scholar] [CrossRef]
- Fernandes, I.; de Freitas, V.; Mateus, N. Anthocyanins and human health: How gastric absorption may influence acute human physiology. Nutr. Aging 2014, 2, 1–14. [Google Scholar]
- Couteau, D.; McCartney, A.L.; Gibson, G.R.; Williamson, G.; Faulds, C.B. Isolation and characterization of human colonic bacteria able to hydrolyse chlorogenic acid. J. Appl. Microbiol. 2001, 90, 873–881. [Google Scholar] [CrossRef]
- Murtaza, G.; Ullah, N.; Mukhtar, F.; Nawazish, S.; Muneer, S. Phytotherapeutics: The emerging role of intestinal and hepatocellular transporters in drug interactions with botanical supplements. Molecules 2017, 22, 1699. [Google Scholar] [CrossRef]
- Jia, X.; Chen, J.; Lin, H.; Hu, M. Disposition of flavonoids via enteric recycling: Enzyme-transporter coupling affects metabolism of biochanin A and formononetin and excretion of their phase II conjugates. J. Pharmacol. Exp. Ther. 2004, 310, 1103–1113. [Google Scholar] [CrossRef]
- Merino, G.; van Herwaarden, A.E.; Wagenaar, E.; Jonker, J.W.; Schinkel, A.H. Sex-dependent expression and activity of the ATP-binding cassette transporter breast cancer resistance protein (BCRP/ABCG2) in liver. Mol. Pharmacol. 2005, 67, 1765–1771. [Google Scholar] [CrossRef]
- Yang, Z.; Kulkarni, K.; Zhu, W.; Hu, M. Bioavailability and pharmacokinetics of genistein: Mechanistic studies on its ADME. Anticancer Agents Med. Chem. 2012, 12, 1264–1280. [Google Scholar] [CrossRef]
- Coldham, N.G.; Sauer, M.J. Pharmacokinetics of [(14)C]Genistein in the rat: Gender-related differences, potential mechanisms of biological action, and implications for human health. Toxicol. Appl. Pharmacol. 2000, 164, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Vieira, A.T.; Castelo, P.M.; Ribeiro, D.A.; Ferreira, C.M. Influence of oral and gut microbiota in the health of menopausal women. Front. Microbiol. 2017, 8, 1884. [Google Scholar] [CrossRef] [PubMed]
- Balan, P.; Chong, Y.S.; Umashankar, S.; Swarup, S.; Loke, W.M.; Lopez, V.; He, H.G.; Seneviratne, C.J. Keystone species in pregnancy gingivitis: A snapshot of oral microbiome during pregnancy and postpartum period. Front. Microbiol. 2018, 9, 2360. [Google Scholar] [CrossRef] [PubMed]
- Marin, L.; Miguelez, E.M.; Villar, C.J.; Lombo, F. Bioavailability of dietary polyphenols and gut microbiota metabolism: Antimicrobial properties. Biomed Res. Int. 2015, 2015, 905215. [Google Scholar] [CrossRef] [PubMed]
- Manach, C.; Williamson, G.; Morand, C.; Scalbert, A.; Remesy, C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am. J. Clin. Nutr. 2005, 81, 230S–242S. [Google Scholar] [CrossRef]
- Di, L. The role of drug metabolizing enzymes in clearance. Expert Opin. Drug Metab. Toxicol. 2014, 10, 379–393. [Google Scholar] [CrossRef]
- Hernandez, J.P.; Mota, L.C.; Huang, W.; Moore, D.D.; Baldwin, W.S. Sexually dimorphic regulation and induction of P450s by the constitutive androstane receptor (CAR). Toxicology 2009, 256, 53–64. [Google Scholar] [CrossRef]
- Lamba, V.; Lamba, J.; Yasuda, K.; Strom, S.; Davila, J.; Hancock, M.L.; Fackenthal, J.D.; Rogan, P.K.; Ring, B.; Wrighton, S.A.; et al. Hepatic CYP2B6 expression: Gender and ethnic differences and relationship to CYP2B6 genotype and CAR (constitutive androstane receptor) expression. J. Pharmacol. Exp. Ther. 2003, 307, 906–922. [Google Scholar] [CrossRef]
- Uno, Y.; Takata, R.; Kito, G.; Yamazaki, H.; Nakagawa, K.; Nakamura, Y.; Kamataki, T.; Katagiri, T. Sex- and age-dependent gene expression in human liver: An implication for drug-metabolizing enzymes. Drug Metab. Pharmacokinet. 2017, 32, 100–107. [Google Scholar] [CrossRef]
- Kawamoto, T.; Kakizaki, S.; Yoshinari, K.; Negishi, M. Estrogen activation of the nuclear orphan receptor CAR (constitutive active receptor) in induction of the mouse Cyp2b10 gene. Mol. Endocrinol. 2000, 14, 1897–1905. [Google Scholar] [CrossRef]
- Bright, A.S.; Herrera-Garcia, G.; Moscovitz, J.E.; You, D.; Guo, G.L.; Aleksunes, L.M. Regulation of drug disposition gene expression in pregnant mice with CAR receptor activation. Nucl. Recept. Res. 2016, 3, 101193. [Google Scholar] [CrossRef] [PubMed]
- Tolson, A.H.; Wang, H. Regulation of drug-metabolizing enzymes by xenobiotic receptors: PXR and CAR. Adv. Drug Deliv. Rev. 2010, 62, 1238–1249. [Google Scholar] [CrossRef] [PubMed]
- Spruiell, K.; Jones, D.Z.; Cullen, J.M.; Awumey, E.M.; Gonzalez, F.J.; Gyamfi, M.A. Role of human pregnane X receptor in high fat diet-induced obesity in pre-menopausal female mice. Biochem. Pharmacol. 2014, 89, 399–412. [Google Scholar] [CrossRef] [PubMed]
- Sachar, M.; Kelly, E.J.; Unadkat, J.D. Mechanisms of CYP3A induction during pregnancy: Studies in HepaRG cells. AAPS J. 2019, 21, 45. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Tang, Y.; Guo, C.; Wang, J.; Boral, D.; Nie, D. Nuclear receptors in the multidrug resistance through the regulation of drug-metabolizing enzymes and drug transporters. Biochem. Pharmacol. 2012, 83, 1112–1126. [Google Scholar] [CrossRef] [PubMed]
- Hukkanen, J. Induction of cytochrome P450 enzymes: A view on human in vivo findings. Expert Rev. Clin. Pharmacol. 2012, 5, 569–585. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Choi, J.M. Sex-specific regulation of immune responses by PPARs. Exp. Mol. Med. 2017, 49, e364. [Google Scholar] [CrossRef] [PubMed]
- Jalouli, M.; Carlsson, L.; Ameen, C.; Linden, D.; Ljungberg, A.; Michalik, L.; Eden, S.; Wahli, W.; Oscarsson, J. Sex difference in hepatic peroxisome proliferator-activated receptor alpha expression: Influence of pituitary and gonadal hormones. Endocrinology 2003, 144, 101–109. [Google Scholar] [CrossRef]
- Dunn, S.E.; Ousman, S.S.; Sobel, R.A.; Zuniga, L.; Baranzini, S.E.; Youssef, S.; Crowell, A.; Loh, J.; Oksenberg, J.; Steinman, L. Peroxisome proliferator-activated receptor (PPAR)α expression in T cells mediates gender differences in development of T cell-mediated autoimmunity. J. Exp. Med. 2007, 204, 321–330. [Google Scholar] [CrossRef]
- Mohammadi-Bardbori, A.; Bengtsson, J.; Rannug, U.; Rannug, A.; Wincent, E. Quercetin, resveratrol, and curcumin are indirect activators of the aryl hydrocarbon receptor (AHR). Chem. Res. Toxicol. 2012, 25, 1878–1884. [Google Scholar] [CrossRef]
- Pastorkova, B.; Vrzalova, A.; Bachleda, P.; Dvorak, Z. Hydroxystilbenes and methoxystilbenes activate human aryl hydrocarbon receptor and induce CYP1A genes in human hepatoma cells and human hepatocytes. Food Chem. Toxicol. 2017, 103, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Stejskalova, L.; Pavek, P. The function of cytochrome P450 1A1 enzyme (CYP1A1) and aryl hydrocarbon receptor (AhR) in the placenta. Curr. Pharm. Biotechnol. 2011, 12, 715–730. [Google Scholar] [CrossRef] [PubMed]
- Moon, Y.J.; Wang, X.; Morris, M.E. Dietary flavonoids: Effects on xenobiotic and carcinogen metabolism. Toxicol. In Vitro 2006, 20, 187–210. [Google Scholar] [CrossRef] [PubMed]
- Zendulka, O.; Totusek, J.; Sulcova, A. Intersexual differences in inhibitory influence of trans-resveratrol on activity of cytochrome P450 2D2 in rats. Neuro Endocrinol. Lett. 2009, 30, 88–91. [Google Scholar] [PubMed]
- Garcia-Villalba, R.; Larrosa, M.; Possemiers, S.; Tomas-Barberan, F.A.; Espin, J.C. Bioavailability of phenolics from an oleuropein-rich olive (Olea europaea) leaf extract and its acute effect on plasma antioxidant status: Comparison between pre- and postmenopausal women. Eur. J. Nutr. 2014, 53, 1015–1027. [Google Scholar] [CrossRef] [PubMed]
- Suarez, M.; Valls, R.M.; Romero, M.P.; Macia, A.; Fernandez, S.; Giralt, M.; Sola, R.; Motilva, M.J. Bioavailability of phenols from a phenol-enriched olive oil. Br. J. Nutr. 2011, 106, 1691–1701. [Google Scholar] [CrossRef]
- Dellinger, R.W.; Garcia, A.M.; Meyskens, F.L., Jr. Differences in the glucuronidation of resveratrol and pterostilbene: Altered enzyme specificity and potential gender differences. Drug Metab. Pharmacokinet. 2014, 29, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.T.; Shim, J.Y.; Nagai, M.; Bai, H.W. Molecular modelling study of the mechanism of high-potency inhibition of human catechol-O-methyltransferase by (−)-epigallocatechin-3-O-gallate. Xenobiotica 2008, 38, 130–146. [Google Scholar] [CrossRef]
- Lorenz, M.; Paul, F.; Moobed, M.; Baumann, G.; Zimmermann, B.F.; Stangl, K.; Stangl, V. The activity of catechol-O-methyltransferase (COMT) is not impaired by high doses of epigallocatechin-3-gallate (EGCG) in vivo. Eur. J. Pharmacol. 2014, 740, 645–651. [Google Scholar] [CrossRef]
- McCane, A.M.; DeLory, M.J.; Timm, M.M.; Janetsian-Fritz, S.S.; Lapish, C.C.; Czachowski, C.L. Differential COMT expression and behavioral effects of COMT inhibition in male and female Wistar and alcohol preferring rats. Alcohol 2018, 67, 15–22. [Google Scholar] [CrossRef]
- Fanali, G.; di Masi, A.; Trezza, V.; Marino, M.; Fasano, M.; Ascenzi, P. Human serum albumin: From bench to bedside. Mol. Aspects Med. 2012, 33, 209–290. [Google Scholar] [CrossRef] [PubMed]
- Mohos, V.; Bencsik, T.; Boda, G.; Fliszar-Nyul, E.; Lemli, B.; Kunsagi-Mate, S.; Poor, M. Interactions of casticin, ipriflavone, and resveratrol with serum albumin and their inhibitory effects on CYP2C9 and CYP3A4 enzymes. Biomed. Pharmacother. 2018, 107, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Poór, M.; Li, Y.; Kunsági-Máté, S.; Petrik, J.; Vladimir-Knežević, S.; Kőszegi, T. Molecular displacement of warfarin from human serum albumin by flavonoid aglycones. J. Lumin. 2013, 142, 122–127. [Google Scholar] [CrossRef]
- Margalef, M.; Pons, Z.; Iglesias-Carres, L.; Arola, L.; Muguerza, B.; Arola-Arnal, A. Gender-related similarities and differences in the body distribution of grape seed flavanols in rats. Mol. Nutr. Food Res. 2016, 60, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Bircsak, K.M.; Aleksunes, L.M. Interaction of Isoflavones with the BCRP/ABCG2 drug transporter. Curr. Drug Metab. 2015, 16, 124–140. [Google Scholar] [CrossRef] [PubMed]
- Visioli, F.; Galli, C.; Grande, S.; Colonnelli, K.; Patelli, C.; Galli, G.; Caruso, D. Hydroxytyrosol excretion differs between rats and humans and depends on the vehicle of administration. J. Nutr. 2003, 133, 2612–2615. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Perles, R.; Aunon, D.; Ferreres, F.; Gil-Izquierdo, A. Physiological linkage of gender, bioavailable hydroxytyrosol derivatives, and their metabolites with systemic catecholamine metabolism. Food Funct. 2017, 8, 4570–4581. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Ros, R.; Rabassa, M.; Cherubini, A.; Urpi-Sarda, M.; Bandinelli, S.; Ferrucci, L.; Andres-Lacueva, C. High concentrations of a urinary biomarker of polyphenol intake are associated with decreased mortality in older adults. J. Nutr. 2013, 143, 1445–1450. [Google Scholar] [CrossRef]
- Lu, L.J.; Anderson, K.E. Sex and long-term soy diets affect the metabolism and excretion of soy isoflavones in humans. Am. J. Clin. Nutr. 1998, 68, 1500S–1504S. [Google Scholar] [CrossRef]
- Abelson, B.; Sun, D.; Que, L.; Nebel, R.A.; Baker, D.; Popiel, P.; Amundsen, C.L.; Chai, T.; Close, C.; DiSanto, M.; et al. Sex differences in lower urinary tract biology and physiology. Biol. Sex Differ. 2018, 9, 45. [Google Scholar] [CrossRef]
- Adlercreutz, H.; Pulkkinen, M.O.; Hamalainen, E.K.; Korpela, J.T. Studies on the role of intestinal bacteria in metabolism of synthetic and natural steroid hormones. J. Steroid Biochem. 1984, 20, 217–229. [Google Scholar] [CrossRef]
- Wu, P.; Chen, Y.; Zhao, J.; Zhang, G.; Chen, J.; Wang, J.; Zhang, H. Urinary microbiome and psychological factors in women with overactive bladder. Front. Cell. Infect. Microbiol. 2017, 7, 488. [Google Scholar] [CrossRef]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef]
- Li, H.; He, J.; Jia, W. The influence of gut microbiota on drug metabolism and toxicity. Expert Opin. Drug Metab. Toxicol. 2016, 12, 31–40. [Google Scholar] [CrossRef]
- Edogawa, S.; Peters, S.A.; Jenkins, G.D.; Gurunathan, S.V.; Sundt, W.J.; Johnson, S.; Lennon, R.J.; Dyer, R.B.; Camilleri, M.; Kashyap, P.C.; et al. Sex differences in NSAID-induced perturbation of human intestinal barrier function and microbiota. FASEB J. 2018, 32, 6615–6625. [Google Scholar] [CrossRef]
- Haro, C.; Rangel-Zuniga, O.A.; Alcala-Diaz, J.F.; Gomez-Delgado, F.; Perez-Martinez, P.; Delgado-Lista, J.; Quintana-Navarro, G.M.; Landa, B.B.; Navas-Cortes, J.A.; Tena-Sempere, M.; et al. Intestinal microbiota is influenced by gender and body mass index. PLoS ONE 2016, 11, e0154090. [Google Scholar] [CrossRef]
- Sinha, T.; Vich Vila, A.; Garmaeva, S.; Jankipersadsing, S.A.; Imhann, F.; Collij, V.; Bonder, M.J.; Jiang, X.; Gurry, T.; Alm, E.J.; et al. Analysis of 1135 gut metagenomes identifies sex-specific resistome profiles. Gut Microbes 2018, 10, 358–366. [Google Scholar] [CrossRef]
- Santos-Marcos, J.A.; Rangel-Zuniga, O.A.; Jimenez-Lucena, R.; Quintana-Navarro, G.M.; Garcia-Carpintero, S.; Malagon, M.M.; Landa, B.B.; Tena-Sempere, M.; Perez-Martinez, P.; Lopez-Miranda, J.; et al. Influence of gender and menopausal status on gut microbiota. Maturitas 2018, 116, 43–53. [Google Scholar] [CrossRef]
- Baker, J.M.; Al-Nakkash, L.; Herbst-Kralovetz, M.M. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas 2017, 103, 45–53. [Google Scholar] [CrossRef]
- Pollet, R.M.; D’Agostino, E.H.; Walton, W.G.; Xu, Y.; Little, M.S.; Biernat, K.A.; Pellock, S.J.; Patterson, L.M.; Creekmore, B.C.; Isenberg, H.N.; et al. An atlas of beta-Glucuronidases in the human intestinal microbiome. Structure 2017, 25, 967–977. [Google Scholar] [CrossRef]
- Ridlon, J.M.; Ikegawa, S.; Alves, J.M.; Zhou, B.; Kobayashi, A.; Iida, T.; Mitamura, K.; Tanabe, G.; Serrano, M.; De Guzman, A.; et al. Clostridium scindens: A human gut microbe with a high potential to convert glucocorticoids into androgens. J. Lipid Res. 2013, 54, 2437–2449. [Google Scholar] [CrossRef]
- Wankhade, U.D.; Zhong, Y.; Lazarenko, O.P.; Chintapalli, S.V.; Piccolo, B.D.; Chen, J.R.; Shankar, K. Sex-specific changes in gut microbiome composition following blueberry consumption in C57BL/6J mice. Nutrients 2019, 11, 313. [Google Scholar] [CrossRef]
- Barrea, L.; Annunziata, G.; Muscogiuri, G.; Laudisio, D.; Di Somma, C.; Maisto, M.; Tenore, G.C.; Colao, A.; Savastano, S. Trimethylamine N-oxide, Mediterranean diet, and nutrition in healthy, normal-weight adults: Also a matter of sex? Nutrition 2018, 62, 7–17. [Google Scholar] [CrossRef]
- Coecke, S.; Debast, G.; Phillips, I.R.; Vercruysse, A.; Shephard, E.A.; Rogiers, V. Hormonal regulation of microsomal flavin-containing monooxygenase activity by sex steroids and growth hormone in co-cultured adult male rat hepatocytes. Biochem. Pharmacol. 1998, 56, 1047–1051. [Google Scholar] [CrossRef]
- Ayesh, R.; Mitchell, S.C.; Smith, R.L. Dysfunctional N-oxidation of trimethylamine and the influence of testosterone treatment in man. Pharmacogenetics 1995, 5, 244–246. [Google Scholar] [CrossRef]
- Neuman, H.; Koren, O. The pregnancy microbiome. Nestle Nutr. Inst. Workshop Ser. 2017, 88, 1–9. [Google Scholar]
- Asher, G.N.; Corbett, A.H.; Hawke, R.L. Common herbal dietary supplement-drug interactions. Am. Fam. Physician 2017, 96, 101–107. [Google Scholar]
- Mensink, G.B.; Fletcher, R.; Gurinovic, M.; Huybrechts, I.; Lafay, L.; Serra-Majem, L.; Szponar, L.; Tetens, I.; Verkaik-Kloosterman, J.; Baka, A.; et al. Mapping low intake of micronutrients across Europe. Br. J. Nutr. 2013, 110, 755–773. [Google Scholar] [CrossRef]
- Eurostat. Women Use Medicine More Often Than Men European Commision. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20170505-1?inheritRedirect=true& (accessed on 15 April 2014).
- Levy, I.; Attias, S.; Ben-Arye, E.; Goldstein, L.; Schiff, E. Potential drug interactions with dietary and herbal supplements during hospitalization. Intern. Emerg. Med. 2017, 12, 301–310. [Google Scholar] [CrossRef]
- Rowland, A.; Miners, J.O.; Mackenzie, P.I. The UDP-glucuronosyltransferases: Their role in drug metabolism and detoxification. Int. J. Biochem. Cell Biol. 2013, 45, 1121–1132. [Google Scholar] [CrossRef]
- Murphy, P.A.; Kern, S.E.; Stanczyk, F.Z.; Westhoff, C.L. Interaction of St. John’s Wort with oral contraceptives: Effects on the pharmacokinetics of norethindrone and ethinyl estradiol, ovarian activity and breakthrough bleeding. Contraception 2005, 71, 402–408. [Google Scholar] [CrossRef]
- Herb Research Foundation. St. John’s Wort Banned in France. Available online: http://www.herbs.org/current/sjwfrance.htm (accessed on 29 September 2015).
- Borrelli, F.; Izzo, A.A. Herb-drug interactions with St John’s wort (Hypericum perforatum): An update on clinical observations. AAPS J. 2009, 11, 710–727. [Google Scholar] [CrossRef]
- De Lima Toccafondo Vieira, M.; Huang, S.M. Botanical-drug interactions: A scientific perspective. Planta Med. 2012, 78, 1400–1415. [Google Scholar] [CrossRef]
- Ostertag, L.M.; Kroon, P.A.; Wood, S.; Horgan, G.W.; Cienfuegos-Jovellanos, E.; Saha, S.; Duthie, G.G.; de Roos, B. Flavan-3-ol-enriched dark chocolate and white chocolate improve acute measures of platelet function in a gender-specific way--a randomized-controlled human intervention trial. Mol. Nutr. Food Res. 2013, 57, 191–202. [Google Scholar] [CrossRef]
- Dearden, L.; Bouret, S.G.; Ozanne, S.E. Sex and gender differences in developmental programming of metabolism. Mol. Metab. 2018, 15, 8–19. [Google Scholar] [CrossRef]
- Saunders, E.J.; Saunders, J.A. Drug therapy in pregnancy: The lessons of diethylstilbestrol, thalidomide, and bendectin. Health Care Women Int. 1990, 11, 423–432. [Google Scholar] [CrossRef]
- Forster, D.A.; Denning, A.; Wills, G.; Bolger, M.; McCarthy, E. Herbal medicine use during pregnancy in a group of Australian women. BMC Pregnancy Childbirth 2006, 6, 21. [Google Scholar] [CrossRef]
- Bishop, J.L.; Northstone, K.; Green, J.R.; Thompson, E.A. The use of complementary and alternative medicine in pregnancy: Data from the Avon Longitudinal Study of Parents and Children (ALSPAC). Complement. Ther. Med. 2011, 19, 303–310. [Google Scholar] [CrossRef]
- Cuzzolin, L.; Francini-Pesenti, F.; Verlato, G.; Joppi, M.; Baldelli, P.; Benoni, G. Use of herbal products among 392 Italian pregnant women: Focus on pregnancy outcome. Pharmacoepidemiol. Drug Saf. 2010, 19, 1151–1158. [Google Scholar] [CrossRef]
- Kennedy, D.A.; Lupattelli, A.; Koren, G.; Nordeng, H. Herbal medicine use in pregnancy: Results of a multinational study. BMC Complement. Altern. Med. 2013, 13, 355. [Google Scholar] [CrossRef]
- Volqvartz, T.; Vestergaard, A.L.; Aagaard, S.K.; Andreasen, M.F.; Lesnikova, I.; Uldbjerg, N.; Larsen, A.; Bor, P. Use of alternative medicine, ginger and licorice among Danish pregnant women—A prospective cohort study. BMC Complement. Altern. Med. 2019, 19, 5. [Google Scholar] [CrossRef]
- Louik, C.; Gardiner, P.; Kelley, K.; Mitchell, A.A. Use of herbal treatments in pregnancy. Am. J. Obstet. Gynecol. 2010, 202, 439.e1–439.e10. [Google Scholar] [CrossRef]
- Yimam, M.; Lee, Y.C.; Hyun, E.J.; Jia, Q. Reproductive and developmental toxicity of orally administered botanical composition, UP446-Part I: Effects on embryo-fetal development in New Zealand White rabbits and Sprague Dawley rats. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2015, 104, 141–152. [Google Scholar] [CrossRef]
- McLay, J.S.; Izzati, N.; Pallivalapila, A.R.; Shetty, A.; Pande, B.; Rore, C.; Al Hail, M.; Stewart, D. Pregnancy, prescription medicines and the potential risk of herb-drug interactions: A cross-sectional survey. BMC Complement. Altern. Med. 2017, 17, 543. [Google Scholar] [CrossRef]
- Pariente, G.; Leibson, T.; Carls, A.; Adams-Webber, T.; Ito, S.; Koren, G. Pregnancy-associated changes in pharmacokinetics: A systematic review. PLoS Med. 2016, 13, e1002160. [Google Scholar] [CrossRef]
- Todaka, E.; Sakurai, K.; Fukata, H.; Miyagawa, H.; Uzuki, M.; Omori, M.; Osada, H.; Ikezuki, Y.; Tsutsumi, O.; Iguchi, T.; et al. Fetal exposure to phytoestrogens--the difference in phytoestrogen status between mother and fetus. Environ. Res. 2005, 99, 195–203. [Google Scholar] [CrossRef]
- Bourque, S.L.; Dolinsky, V.W.; Dyck, J.R.; Davidge, S.T. Maternal resveratrol treatment during pregnancy improves adverse fetal outcomes in a rat model of severe hypoxia. Placenta 2012, 33, 449–452. [Google Scholar] [CrossRef]
- Jarrell, J.; Foster, W.G.; Kinniburgh, D.W. Phytoestrogens in human pregnancy. Obstet. Gynecol. Int. 2012, 2012, 850313. [Google Scholar] [CrossRef]
- North, K.; Golding, J. A maternal vegetarian diet in pregnancy is associated with hypospadias. The ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. BJU Int. 2000, 85, 107–113. [Google Scholar] [CrossRef]
- Jacobsen, B.K.; Jaceldo-Siegl, K.; Knutsen, S.F.; Fan, J.; Oda, K.; Fraser, G.E. Soy isoflavone intake and the likelihood of ever becoming a mother: The Adventist Health Study-2. Int. J. Womens Health 2014, 6, 377–384. [Google Scholar] [CrossRef]
- Vanegas, J.C.; Afeiche, M.C.; Gaskins, A.J.; Minguez-Alarcon, L.; Williams, P.L.; Wright, D.L.; Toth, T.L.; Hauser, R.; Chavarro, J.E. Soy food intake and treatment outcomes of women undergoing assisted reproductive technology. Fertil. Steril. 2015, 103, 749–755. [Google Scholar] [CrossRef]
- Kim, J.; Kim, S.; Huh, K.; Kim, Y.; Joung, H.; Park, M. High serum isoflavone concentrations are associated with the risk of precocious puberty in Korean girls. Clin. Endocrinol. 2011, 75, 831–835. [Google Scholar] [CrossRef]
- Samavati, R.; Ducza, E.; Hajagos-Toth, J.; Gaspar, R. Herbal laxatives and antiemetics in pregnancy. Reprod. Toxicol. 2017, 72, 153–158. [Google Scholar] [CrossRef]
- Ouzir, M.; El Bairi, K.; Amzazi, S. Toxicological properties of fenugreek (Trigonella foenum graecum). Food Chem. Toxicol. 2016, 96, 145–154. [Google Scholar] [CrossRef]
- Kolding, L.; Pedersen, L.H.; Henriksen, T.B.; Olsen, J.; Grzeskowiak, L.E. Hypericum perforatum use during pregnancy and pregnancy outcome. Reprod. Toxicol. 2015, 58, 234–237. [Google Scholar] [CrossRef]
- Raikkonen, K.; Pesonen, A.K.; Heinonen, K.; Lahti, J.; Komsi, N.; Eriksson, J.G.; Seckl, J.R.; Jarvenpaa, A.L.; Strandberg, T.E. Maternal licorice consumption and detrimental cognitive and psychiatric outcomes in children. Am. J. Epidemiol. 2009, 170, 1137–1146. [Google Scholar] [CrossRef]
- Strandberg, T.E.; Jarvenpaa, A.L.; Vanhanen, H.; McKeigue, P.M. Birth outcome in relation to licorice consumption during pregnancy. Am. J. Epidemiol. 2001, 153, 1085–1088. [Google Scholar] [CrossRef]
- Nazari, S.; Rameshrad, M.; Hosseinzadeh, H. Toxicological effects of Glycyrrhiza glabra (Licorice): A review. Phytother. Res. 2017, 31, 1635–1650. [Google Scholar] [CrossRef]
- Qiu, J.X.; Zhou, Z.W.; He, Z.X.; Zhang, X.; Zhou, S.F.; Zhu, S. Estimation of the binding modes with important human cytochrome P450 enzymes, drug interaction potential, pharmacokinetics, and hepatotoxicity of ginger components using molecular docking, computational, and pharmacokinetic modeling studies. Drug Des. Devel. Ther. 2015, 9, 841–866. [Google Scholar]
- Banihani, S.A. Ginger and testosterone. Biomolecules 2018, 8, 119. [Google Scholar] [CrossRef]
- Sondergaard, K. Ginger, pregnancy nausea and possible fetal injuries (testosterone effect). Ugeskr. Laeger 2008, 170, 359. [Google Scholar]
- Marx, W.; McKavanagh, D.; McCarthy, A.L.; Bird, R.; Ried, K.; Chan, A.; Isenring, L. The effect of Ginger (Zingiber officinale) on platelet aggregation: A systematic literature review. PLoS ONE 2015, 10, e0141119. [Google Scholar]
- Gonzalez-Nahm, S.; Mendez, M.; Robinson, W.; Murphy, S.K.; Hoyo, C.; Hogan, V.; Rowley, D. Low maternal adherence to a Mediterranean diet is associated with increase in methylation at the MEG3-IG differentially methylated region in female infants. Environ. Epigenet. 2017, 3, dvx007. [Google Scholar] [CrossRef]
- Malireddy, S.; Kotha, S.R.; Secor, J.D.; Gurney, T.O.; Abbott, J.L.; Maulik, G.; Maddipati, K.R.; Parinandi, N.L. Phytochemical antioxidants modulate mammalian cellular epigenome: Implications in health and disease. Antioxid. Redox Signal. 2012, 17, 327–339. [Google Scholar] [CrossRef]
- Facchinetti, F.; Pedrielli, G.; Benoni, G.; Joppi, M.; Verlato, G.; Dante, G.; Balduzzi, S.; Cuzzolin, L. Herbal supplements in pregnancy: Unexpected results from a multicentre study. Hum. Reprod. 2012, 27, 3161–3167. [Google Scholar] [CrossRef]
- Budzynska, K.; Gardner, Z.E.; Dugoua, J.J.; Low Dog, T.; Gardiner, P. Systematic review of breastfeeding and herbs. Breastfeed. Med. 2012, 7, 489–503. [Google Scholar] [CrossRef]
- Sim, T.F.; Sherriff, J.; Hattingh, H.L.; Parsons, R.; Tee, L.B. The use of herbal medicines during breastfeeding: A population-based survey in Western Australia. BMC Complement. Altern. Med. 2013, 13, 317. [Google Scholar] [CrossRef]
- Zuppa, A.A.; Sindico, P.; Orchi, C.; Carducci, C.; Cardiello, V.; Romagnoli, C. Safety and efficacy of galactogogues: Substances that induce, maintain and increase breast milk production. J. Pharm. Pharm. Sci. 2010, 13, 162–174. [Google Scholar] [CrossRef]
- Zapantis, A.; Steinberg, J.G.; Schilit, L. Use of herbals as galactagogues. J. Pharm. Pract. 2012, 25, 222–231. [Google Scholar] [CrossRef]
- Bazzano, A.N.; Cenac, L.; Brandt, A.J.; Barnett, J.; Thibeau, S.; Theall, K.P. Maternal experiences with and sources of information on galactagogues to support lactation: A cross-sectional study. Int. J. Womens Health 2017, 9, 105–113. [Google Scholar] [CrossRef]
- Sahin, B.; Kaymaz, N.; Yildirim, S. Herbal remedies for perceived inadequate milk supply are perhaps not as safe as women think: A brief case report. Women Birth 2016, 29, e133. [Google Scholar] [CrossRef]
- National Institute of Health. Goat’s Rue; U.S. National Library of Medicine: Washington, DC, USA, 2018.
- Galante, L.; Milan, A.M.; Reynolds, C.M.; Cameron-Smith, D.; Vickers, M.H.; Pundir, S. Sex-specific human milk composition: The role of infant sex in determining early life nutrition. Nutrients 2018, 10, 1194. [Google Scholar] [CrossRef]
- Powe, C.E.; Knott, C.D.; Conklin-Brittain, N. Infant sex predicts breast milk energy content. Am. J. Hum. Biol. 2010, 22, 50–54. [Google Scholar] [CrossRef]
- Fujita, M.; Roth, E.; Lo, Y.J.; Hurst, C.; Vollner, J.; Kendell, A. In poor families, mothers’ milk is richer for daughters than sons: A test of Trivers-Willard hypothesis in agropastoral settlements in Northern Kenya. Am. J. Phys. Anthropol. 2012, 149, 52–59. [Google Scholar] [CrossRef]
- Romaszko, E.; Wiczkowski, W.; Romaszko, J.; Honke, J.; Piskula, M.K. Exposure of breastfed infants to quercetin after consumption of a single meal rich in quercetin by their mothers. Mol. Nutr. Food Res. 2014, 58, 221–228. [Google Scholar] [CrossRef]
- Patisaul, H.B. Endocrine disruption by dietary phyto-oestrogens: Impact on dimorphic sexual systems and behaviours. Proc. Nutr. Soc. 2017, 76, 130–144. [Google Scholar] [CrossRef]
- Jonker, J.W.; Merino, G.; Musters, S.; van Herwaarden, A.E.; Bolscher, E.; Wagenaar, E.; Mesman, E.; Dale, T.C.; Schinkel, A.H. The breast cancer resistance protein BCRP (ABCG2) concentrates drugs and carcinogenic xenotoxins into milk. Nat. Med. 2005, 11, 127–129. [Google Scholar] [CrossRef]
- Tamaki, H.; Satoh, H.; Hori, S.; Ohtani, H.; Sawada, Y. Inhibitory effects of herbal extracts on breast cancer resistance protein (BCRP) and structure-inhibitory potency relationship of isoflavonoids. Drug Metab. Pharmacokinet. 2010, 25, 170–179. [Google Scholar] [CrossRef]
- Moossavi, S.; Sepehri, S.; Robertson, B.; Bode, L.; Goruk, S.; Field, C.J.; Lix, L.M.; de Souza, R.J.; Becker, A.B.; Mandhane, P.J.; et al. Composition and variation of the human milk microbiota are influenced by maternal and early-life factors. Cell Host Microbe 2019, 25, 324–335. [Google Scholar] [CrossRef]
- Urbaniak, C.; Angelini, M.; Gloor, G.B.; Reid, G. Human milk microbiota profiles in relation to birthing method, gestation and infant gender. Microbiome 2016, 4, 1. [Google Scholar] [CrossRef]
- Baumann-Dudenhoeffer, A.M.; D’Souza, A.W.; Tarr, P.I.; Warner, B.B.; Dantas, G. Infant diet and maternal gestational weight gain predict early metabolic maturation of gut microbiomes. Nat. Med. 2018, 24, 1822–1829. [Google Scholar] [CrossRef]
- Fernandez, L.; Ruiz, L.; Jara, J.; Orgaz, B.; Rodriguez, J.M. Strategies for the preservation, restoration and modulation of the human milk microbiota. Implications for human milk banks and neonatal intensive care units. Front. Microbiol. 2018, 9, 2676. [Google Scholar] [CrossRef]
- National Toxicology Program; National Institute of Environmental Health Science. Draft NTP Brief on Soy Infant Formula; National Institutes of Health, Ed.; U.S. Department of Health and Human Services: Washington, DC, USA, 2010.
- Adgent, M.A.; Daniels, J.L.; Rogan, W.J.; Adair, L.; Edwards, L.J.; Westreich, D.; Maisonet, M.; Marcus, M. Early-life soy exposure and age at menarche. Paediatr. Perinat. Epidemiol. 2012, 26, 163–175. [Google Scholar] [CrossRef]
- D’Aloisio, A.A.; DeRoo, L.A.; Baird, D.D.; Weinberg, C.R.; Sandler, D.P. Prenatal and infant exposures and age at menarche. Epidemiology 2013, 24, 277–284. [Google Scholar] [CrossRef]
- D’Aloisio, A.A.; Baird, D.D.; DeRoo, L.A.; Sandler, D.P. Early-life exposures and early-onset uterine leiomyomata in black women in the Sister Study. Environ. Health Perspect. 2012, 120, 406–412. [Google Scholar] [CrossRef]
- Upson, K.; Sathyanarayana, S.; Scholes, D.; Holt, V.L. Early-life factors and endometriosis risk. Fertil. Steril. 2015, 104, 964–971. [Google Scholar] [CrossRef]
- Newbold, R.R.; Banks, E.P.; Bullock, B.; Jefferson, W.N. Uterine adenocarcinoma in mice treated neonatally with Genistein. Cancer Res. 2001, 61, 4325–4328. [Google Scholar]
- McCarver, G.; Bhatia, J.; Chambers, C.; Clarke, R.; Etzel, R.; Foster, W.; Hoyer, P.; Leeder, J.S.; Peters, J.M.; Rissman, E.; et al. NTP-CERHR expert panel report on the developmental toxicity of soy infant formula. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2011, 92, 421–468. [Google Scholar] [CrossRef]
- Setchell, K.D.; Zimmer-Nechemias, L.; Cai, J.; Heubi, J.E. Exposure of infants to phyto-oestrogens from soy-based infant formula. Lancet 1997, 350, 23–27. [Google Scholar] [CrossRef]
- Irvine, C.H.; Fitzpatrick, M.G.; Alexander, S.L. Phytoestrogens in soy-based infant foods: Concentrations, daily intake, and possible biological effects. Proc. Soc. Exp. Biol. Med. 1998, 217, 247–253. [Google Scholar] [CrossRef]
- Cao, Y.; Calafat, A.M.; Doerge, D.R.; Umbach, D.M.; Bernbaum, J.C.; Twaddle, N.C.; Ye, X.; Rogan, W.J. Isoflavones in urine, saliva, and blood of infants: Data from a pilot study on the estrogenic activity of soy formula. J. Expo. Sci. Environ. Epidemiol. 2009, 19, 223–234. [Google Scholar] [CrossRef]
- Koleva, P.T.; Tun, H.M.; Konya, T.; Guttman, D.S.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Sears, M.R.; Scott, J.A.; et al. Sex-specific impact of asthma during pregnancy on infant gut microbiota. Eur. Respir. J. 2017, 50, 1700280. [Google Scholar] [CrossRef]
- Harding, J.E.; Cormack, B.E.; Alexander, T.; Alsweiler, J.M.; Bloomfield, F.H. Advances in nutrition of the newborn infant. Lancet 2017, 389, 1660–1668. [Google Scholar] [CrossRef]
- Roseboom, T.J.; Painter, R.C.; van Abeelen, A.F.; Veenendaal, M.V.; de Rooij, S.R. Hungry in the womb: What are the consequences? Lessons from the Dutch famine. Maturitas 2011, 70, 141–145. [Google Scholar] [CrossRef]
- Griffin, R.M.; Hayward, A.D.; Bolund, E.; Maklakov, A.A.; Lummaa, V. Sex differences in adult mortality rate mediated by early-life environmental conditions. Ecol. Lett. 2018, 21, 235–242. [Google Scholar] [CrossRef]
- Broere-Brown, Z.A.; Baan, E.; Schalekamp-Timmermans, S.; Verburg, B.O.; Jaddoe, V.W.; Steegers, E.A. Sex-specific differences in fetal and infant growth patterns: A prospective population-based cohort study. Biol. Sex Differ. 2016, 7, 65. [Google Scholar] [CrossRef]
- Brown, Z.A.; Schalekamp-Timmermans, S.; Tiemeier, H.W.; Hofman, A.; Jaddoe, V.W.; Steegers, E.A. Fetal sex specific differences in human placentation: A prospective cohort study. Placenta 2014, 35, 359–364. [Google Scholar] [CrossRef]
- Melamed, N.; Meizner, I.; Mashiach, R.; Wiznitzer, A.; Glezerman, M.; Yogev, Y. Fetal sex and intrauterine growth patterns. J. Ultrasound Med. 2013, 32, 35–43. [Google Scholar] [CrossRef]
- Ford, N.D.; Behrman, J.R.; Hoddinott, J.F.; Maluccio, J.A.; Martorell, R.; Ramirez-Zea, M.; Stein, A.D. Exposure to improved nutrition from conception to age 2 years and adult cardiometabolic disease risk: A modelling study. Lancet Glob. Health 2018, 6, e875–e884. [Google Scholar] [CrossRef]
- Marks, K.J.; Hartman, T.J.; Taylor, E.V.; Rybak, M.E.; Northstone, K.; Marcus, M. Exposure to phytoestrogens in utero and age at menarche in a contemporary British cohort. Environ. Res. 2017, 155, 287–293. [Google Scholar] [CrossRef]
- Raikkonen, K.; Martikainen, S.; Pesonen, A.K.; Lahti, J.; Heinonen, K.; Pyhala, R.; Lahti, M.; Tuovinen, S.; Wehkalampi, K.; Sammallahti, S.; et al. Maternal Licorice consumption during pregnancy and pubertal, cognitive, and psychiatric outcomes in children. Am. J. Epidemiol. 2017, 185, 317–328. [Google Scholar] [CrossRef]
- Simmler, C.; Pauli, G.F.; Chen, S.N. Phytochemistry and biological properties of glabridin. Fitoterapia 2013, 90, 160–184. [Google Scholar] [CrossRef]
- Jefferson, W.N.; Padilla-Banks, E.; Newbold, R.R. Adverse effects on female development and reproduction in CD-1 mice following neonatal exposure to the phytoestrogen genistein at environmentally relevant doses. Biol. Reprod. 2005, 73, 798–806. [Google Scholar] [CrossRef]
- Gorski, J.C.; Huang, S.M.; Pinto, A.; Hamman, M.A.; Hilligoss, J.K.; Zaheer, N.A.; Desai, M.; Miller, M.; Hall, S.D. The effect of echinacea (Echinacea purpurea root) on cytochrome P450 activity in vivo. Clin. Pharmacol. Ther. 2004, 75, 89–100. [Google Scholar] [CrossRef]
- Gurley, B.J.; Gardner, S.F.; Hubbard, M.A.; Williams, D.K.; Gentry, W.B.; Cui, Y.; Ang, C.Y. Cytochrome P450 phenotypic ratios for predicting herb-drug interactions in humans. Clin. Pharmacol. Ther. 2002, 72, 276–287. [Google Scholar] [CrossRef]
- Gurley, B.J.; Gardner, S.F.; Hubbard, M.A.; Williams, D.K.; Gentry, W.B.; Cui, Y.; Ang, C.Y. Clinical assessment of effects of botanical supplementation on cytochrome P450 phenotypes in the elderly: St John’s wort, garlic oil, Panax ginseng and Ginkgo biloba. Drugs Aging 2005, 22, 525–539. [Google Scholar] [CrossRef]
- Showande, S.J.; Fakeye, T.O.; Kajula, M.; Hokkanen, J.; Tolonen, A. Potential inhibition of major human cytochrome P450 isoenzymes by selected tropical medicinal herbs-Implication for herb-drug interactions. Food Sci. Nutr. 2018, 7, 44–55. [Google Scholar] [CrossRef]
- Mukherjee, P.K.; Ponnusankar, S.; Pandit, S.; Hazam, P.K.; Ahmmed, M.; Mukherjee, K. Botanicals as medicinal food and their effects on drug metabolizing enzymes. Food Chem. Toxicol. 2011, 49, 3142–3153. [Google Scholar] [CrossRef]
- Satoh, T.; Fujisawa, H.; Nakamura, A.; Takahashi, N.; Watanabe, K. Inhibitory effects of eight green tea catechins on cytochrome P450 1A2, 2C9, 2D6, and 3A4 activities. J. Pharm. Pharm. Sci. 2016, 19, 188–197. [Google Scholar] [CrossRef]
- Guo, Y.; Chen, Y.; Tan, Z.R.; Klaassen, C.D.; Zhou, H.H. Repeated administration of berberine inhibits cytochromes P450 in humans. Eur. J. Clin. Pharmacol. 2012, 68, 213–217. [Google Scholar] [CrossRef]
- Foster, B.C.; Foster, M.S.; Vandenhoek, S.; Krantis, A.; Budzinski, J.W.; Arnason, J.T.; Gallicano, K.D.; Choudri, S. An in vitro evaluation of human cytochrome P450 3A4 and P-glycoprotein inhibition by garlic. J. Pharm. Pharm. Sci. 2001, 4, 176–184. [Google Scholar]
- Yin, O.Q.; Tomlinson, B.; Waye, M.M.; Chow, A.H.; Chow, M.S. Pharmacogenetics and herb-drug interactions: Experience with Ginkgo biloba and omeprazole. Pharmacogenetics 2004, 14, 841–850. [Google Scholar] [CrossRef]
- Kalsotra, A.; Anakk, S.; Boehme, C.L.; Strobel, H.W. Sexual dimorphism and tissue specificity in the expression of CYP4F forms in Sprague Dawley rats. Drug Metab. Dispos. 2002, 30, 1022–1028. [Google Scholar] [CrossRef]
- Gurley, B.J.; Swain, A.; Hubbard, M.A.; Williams, D.K.; Barone, G.; Hartsfield, F.; Tong, Y.; Carrier, D.J.; Cheboyina, S.; Battu, S.K. Clinical assessment of CYP2D6-mediated herb-drug interactions in humans: Effects of milk thistle, black cohosh, goldenseal, kava kava, St. John’s wort, and Echinacea. Mol. Nutr. Food Res. 2008, 52, 755–763. [Google Scholar] [CrossRef]
- Lown, K.S.; Bailey, D.G.; Fontana, R.J.; Janardan, S.K.; Adair, C.H.; Fortlage, L.A.; Brown, M.B.; Guo, W.; Watkins, P.B. Grapefruit juice increases felodipine oral availability in humans by decreasing intestinal CYP3A protein expression. J. Clin. Investig. 1997, 99, 2545–2553. [Google Scholar] [CrossRef]
- Gurley, B.J.; Gardner, S.F.; Hubbard, M.A.; Williams, D.K.; Gentry, W.B.; Carrier, J.; Khan, I.A.; Edwards, D.J.; Shah, A. In vivo assessment of botanical supplementation on human cytochrome P450 phenotypes: Citrus aurantium, Echinacea purpurea, milk thistle, and saw palmetto. Clin. Pharmacol. Ther. 2004, 76, 428–440. [Google Scholar] [CrossRef]
- Hajda, J.; Rentsch, K.M.; Gubler, C.; Steinert, H.; Stieger, B.; Fattinger, K. Garlic extract induces intestinal P-glycoprotein, but exhibits no effect on intestinal and hepatic CYP3A4 in humans. Eur. J. Pharm. Sci. 2010, 41, 729–735. [Google Scholar] [CrossRef]
- Misaka, S.; Yatabe, J.; Muller, F.; Takano, K.; Kawabe, K.; Glaeser, H.; Yatabe, M.S.; Onoue, S.; Werba, J.P.; Watanabe, H.; et al. Green tea ingestion greatly reduces plasma concentrations of nadolol in healthy subjects. Clin. Pharmacol. Ther. 2014, 95, 432–438. [Google Scholar] [CrossRef]


| Parameters | Male/Female |
|---|---|
| Fat | +F (human) |
| Muscular mass | +M (human) |
| Body weight | +M (human) |
| Height | +M (human) |
| Heart rate | −M (human) |
| Regional blood flow | +M (human) |
| Plasma volume | +F (human) |
| Total water | +M (human) |
| Gastric pH [acidity] | +M (human) |
| Gastric emptying | +M (human) |
| Gastro-intestinal mobility | +M (human) |
| Glomerular filtration rate | +M (human) |
| CYP1A2 | +M (human) |
| CYP2A6 | +F (human) |
| CYP2A7 | +F (rat) |
| CYP2E1 | +M (human) |
| CYP3A4 | +F (human) |
| CYP3A | only in males (pig) |
| CYP3A5 | +M (human) |
| CYP3A7 | +F (human) |
| CYP3A9 | +F (human) |
| CYP2B6 | +M (human) |
| CYP2C9 | = (human) |
| CYP2C19 | = (human) |
| CYP2D6 | +M (human) |
| CYP7A1 | +F (human) |
| COMT | +M (human) |
| GST | +M (rat) |
| GSTA1/A2 | +F (human) |
| UDP-glucuronosyl-transferases | +M [UGT1A6 (pig); UGT2b1 (liver); UGT2b5/37/38 (kidney); UGT1a6 (lung); UGT2b15; UGT2b17] +F [UGT 1a1 (human); UGT 1a5 (liver); UGT 1a2 (kidney); UGT 2b35 (brain)] |
| SULT1A1 | +F than men with high androgen levels (human) |
| SULT1E1 liver | only in males (rat) |
| Oatp1 | = (rat) |
| Oatp2 | = (rat) |
| Oatp4 | +F = (rat) |
| P-glycoprotein | +M (human) |
| Liver SLC3A1 | +F (human) |
| Liver SLC13A1 | +M (human) |
| Liver SLC10A1 | +F (human) |
| Liver ACSL4 | +F (human) |
| Species | Enzyme/Transporters | Phenols/Herbs | Type of Activity | References |
|---|---|---|---|---|
| Pig | CYP 1A1 | Genistein | Inh | [6] |
| Pig | CYP 1A1 | Daidzein | Inh | [6] |
| Pig | CYP 1A1 | Biochanin | Ind | [6] |
| Pig | CYP 1A1 | Equol | Inh | [6] |
| Pig | CYP 1A1 | Rutin | Inh | [17] |
| Pig | CYP 1A1 | Myricetin | Inh | [17] |
| Pig | CYP 1A1 | p-couamric acid | Inh | [17] |
| Pig | CYP 1A1 | Gallic acid | Inh | [17] |
| Pig | CYP 1A1 | Caffeic acid | Inh | [17] |
| Human | CYP1A2 | Echinacea purpurea | Inh | [186] |
| Human | CYP1A2 | Garlic oil | = | [187,188] |
| Human | CYP1A2 | Allium sativum | Inh | [189] |
| Human | CYP1A2 | Matricaria recutita | Inh | [190] |
| Human | CYP1A2 | Gongronema latifolium, | Inh | [189] |
| Human | CYP1A2 | Moringa oleifera | Inh | [189] |
| Human | CYP1A2 | CG (-)-catechin-3-O-gallate, GCG (-)-gallocatechin-3-O-gallate, EGCG | Inh | [191] |
| Human | CYP1A2 | Berberine | Inh | [192] |
| Rat | CYP1A2 | Genistein | Inh | [48] and cited literature |
| Human | CYP1A | Mangifera indica | Inh | [189] |
| Human cancer cell | CYP1A4 | Genistein | Inh | [48] and cited literature |
| Human | CYP2B6 | Allium sativum | Inh | [189] |
| Human | CYP2B6 | Mangifera indica | Inh | [189] |
| Human | CYP2E1 | Garlic oil | Inh | [187] |
| Human | CYP2E1 | Piper methysticum | Inh | [188] |
| Human | CYP2E1 | St John’s wort | Ind | [187] |
| Pig | CYP2E1 | Quercetin | Inh (male) | [19] |
| Pig | CYP2E1 | Rutin | Inh | [19] |
| Pig | CYP2E1 | Myricetin | Inh | [19] |
| Pig | CYP2E1 | p-couamric acid | Inh | [19] |
| Pig | CYP2E1 | Gallic acid | Inh | [19] |
| Pig | CYP2E1 | Caffeic acid | Inh | [19] |
| Rat | CYP2C | Genistein | Inh | [48] and cited literature |
| Human | CYP2C8 | Allium sativum | Inh | [189] |
| Human | CYP2C8 | Mangifera indica | Inh | [189] |
| Human | CYP2C9 | Mangifera indica | Inh | [189] |
| Human | CYP2C9 | Allium sativum | Inh (2c9*1) = | [193] [189] |
| Human | CYP2C9 | Matricaria recutita | Inh | [190] |
| Human | CYP2C9 | (-)-epicatechin-3-O-gallate ECG, (-)- epigallocatechin, EGC CG (-)-catechin-3-O-gallate, | Inh | [191] |
| Human | CYP2C9 | Berberine | Inh | [192] |
| Human | CYP2C19 | Achillea millefolium | Inh | [190] |
| Human | CYP2C19 | Ginkgo biloba | Ind | [194] |
| Rat | CYP2D2 | Isorhamnetin | Inh | [17,64] |
| Rat | CYP2D2 | Resveratrol | Inh | [72,195] |
| Human | CYP2D6 | Hydrastis Canadensis | Inh | [196] |
| Human | CYP2D6 | Allium sativum | = | [189,193] |
| Human | CYP2D6 | Garlic oil | = | [187,188] |
| Human | CYP2D6 | Cimicifuga racemosa | Inh | [188] |
| Human | CYP2D6 | Mangifera indica | Inh | [189] |
| Human | CYP2D6 | Alstonia boonei | Inh | [189] |
| Rat | CYP2D6 | Alstonia scholaris | Inh | [190] |
| Human | CYP2D6 | Matricaria recutita | Inh | [190] |
| Human | CYP2D6 | Picralima nitida | Inh | [189] |
| Human | CYP2D6 | Berberine | Inh | [192] |
| Human | CYP3A4 | St John’s wort | Ind Ind | [45] [187] |
| Human | intestinal CYP3A4 | Grapefruit juice | Inh = | [197] |
| Human | liver CYP3A4 intestinal CYP3A4 | Echinacea purpurea | Inh Ind | [186] [198] |
| Rat | CYP3A | Genistein | Inh | [48] and cited literature |
| Pig | CYP3A | Myricetin | Inh (male) | [17] |
| Human | CYP3A4 | Allium sativum | Inh = | [193] [199] |
| Human | CYP3A4 | Matricaria recutita | Inh | [190] |
| Human | CYP3A4 | Picralima nitida | Inh | [189] |
| Human | CYP3A4 | Achillea millefolium | Inh | [190] |
| Human | CYP3A4 | CG (-)-catechin-3-O-gallate, GCG (-)-gallocatechin-3-O-gallate, EGCG | Inh | [191] |
| Human | CYP3A4 | Berberine | Inh | [192] |
| Human | CYP3A5 | Allium Sativum | Inh = | [193] [199] |
| Sheep | BCRP | Genistein | Ind | [45] |
| Human | Oatp1A2 | Green tea extract | Inh | [200] |
| Human | P-glycoprotein/MDR1 | Garlic extract | Ind | [199] |
| Human | P-glycoprotein/MDR1 | St John’s wort | Inh | [45] |
| Rat | P-glycoprotein/MDR1 | St John’s wort | Inh | [45] |
| Human cancer cell line | UDP | Genistein | Ind | [48] and cited literature |
| Human | SULT | Genistein | Inh | [48] and cited literature |
| Human | COMT | Epigallocatechin-3-gallate | Inh | [68] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campesi, I.; Romani, A.; Franconi, F. The Sex–Gender Effects in the Road to Tailored Botanicals. Nutrients 2019, 11, 1637. https://doi.org/10.3390/nu11071637
Campesi I, Romani A, Franconi F. The Sex–Gender Effects in the Road to Tailored Botanicals. Nutrients. 2019; 11(7):1637. https://doi.org/10.3390/nu11071637
Chicago/Turabian StyleCampesi, Ilaria, Annalisa Romani, and Flavia Franconi. 2019. "The Sex–Gender Effects in the Road to Tailored Botanicals" Nutrients 11, no. 7: 1637. https://doi.org/10.3390/nu11071637
APA StyleCampesi, I., Romani, A., & Franconi, F. (2019). The Sex–Gender Effects in the Road to Tailored Botanicals. Nutrients, 11(7), 1637. https://doi.org/10.3390/nu11071637







