Water and Beverage Consumption among a Nationally Representative Sample of Children and Adolescents in the United Arab Emirates
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Sociodemographic Characteristics and Water Intake
3.2. Mean Water Intake by Age Group
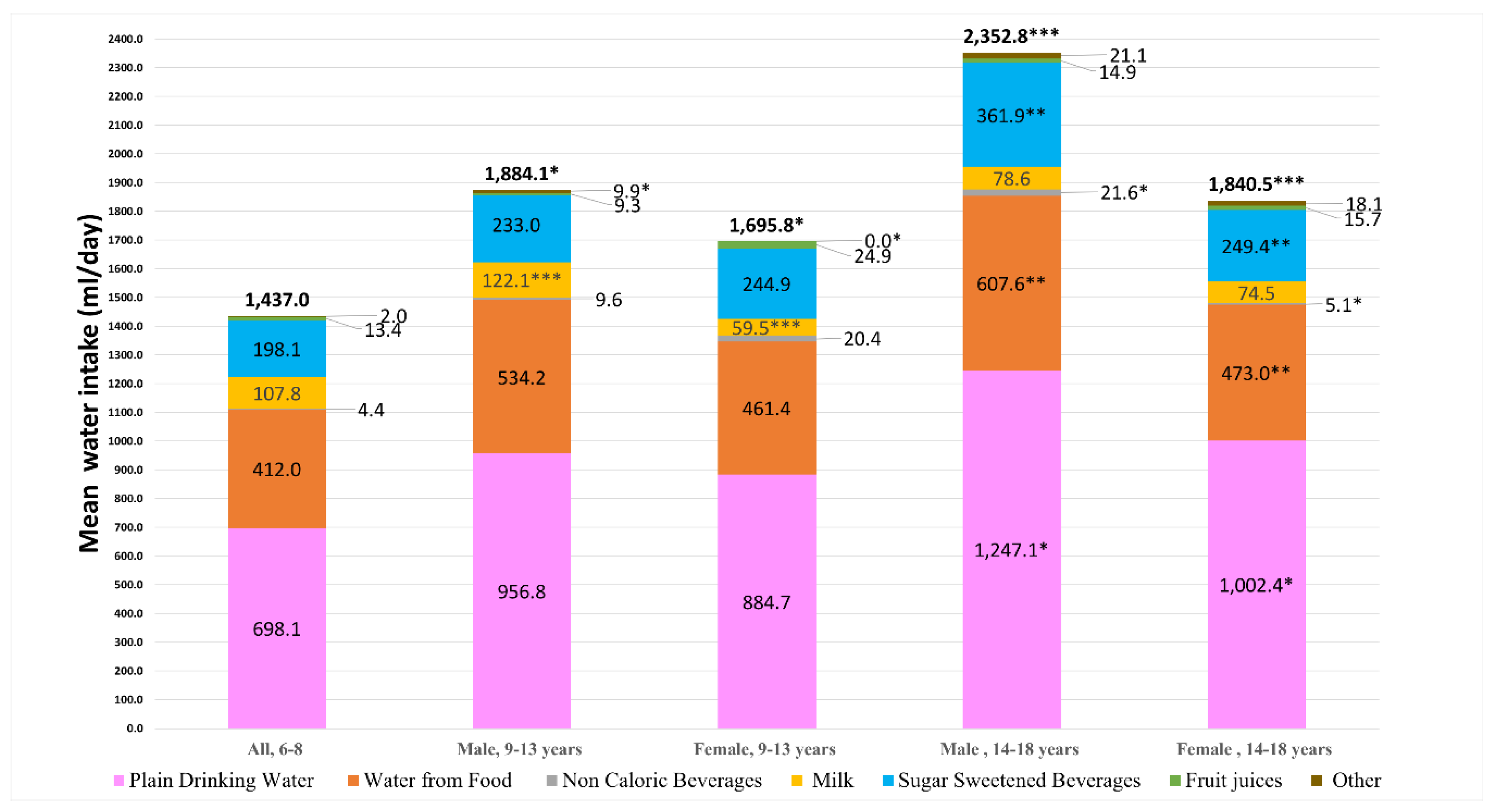
3.3. Total Daily Water Intake from All Sources by Age Group and Sex
3.4. Comparison of Participants’ Water Intake and IOM Recommendations
3.5. Comparison of Participants’ Water Intake and EFSA Recommendations
3.6. Mean Water-to-Energy Ratio by Age Group and Sex
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jéquier, E.; Constant, F. Water as an essential nutrient: The physiological basis of hydration. Eur. J. Clin. Nutr. 2010, 64, 115–123. [Google Scholar] [CrossRef]
- Grandjean, A.C.; Reimers, K.J.; Buyckx, M.E. Hydration: Issues for the 21st century. Nutr. Rev. 2003, 61, 261–271. [Google Scholar] [CrossRef]
- Chan, J.; Knutsen, S.F.; Blix, G.G.; Lee, J.W.; Fraser, G.E. Water, other fluids, and fatal coronary heart disease: The Adventist Health Study. Am. J. Epidemiol. 2002, 155, 827–833. [Google Scholar] [CrossRef]
- Roussel, R.; Fezeu, L.; Bouby, N.; Balkau, B.; Lantieri, O.; Alhenc-Gelas, F.; Marre, M.; Bankir, L.; DESIR Study Group. Low water intake and risk for new-onset hyperglycemia. Diabetes Care. 2011, 34, 2551–2554. [Google Scholar] [CrossRef]
- Lotan, Y.; Daudon, M.; Bruyère, F.; Talaska, G.; Strippoli, G.; Johnson, R.J.; Tack, I. Impact of fluid intake in the prevention of urinary system diseases: A brief review. Curr. Opin. Nephrol. Hypertens. 2013, 22, S1–S10. [Google Scholar] [CrossRef]
- Brooks, D.R.; Ramirez-Rubio, O.; Amador, J.J. CKD in Central America: A hot issue. Am. J. Kidney Dis. 2012, 59, 481–484. [Google Scholar] [CrossRef]
- Peraza, S.; Wesseling, C.; Aragon, A.; Leiva, R.; García-Trabanino, R.A.; Torres, C.; Jakobsson, K.; Elinder, C.G.; Hogstedt, C. Decreased kidney function among agricultural workers in El Salvador. Am. J. Kidney Dis. 2012, 59, 531–540. [Google Scholar] [CrossRef]
- Bar-David, Y.; Urkin, J.; Landau, D.; Bar-David, Z.; Pilpel, D. Voluntary dehydration among elementary school children residing in a hot arid environment. J. Hum. Nutr. Diet. 2009, 22, 455–460. [Google Scholar] [CrossRef]
- Aphamis, G.; Stavrinou, P.S.; Andreou, E.; Giannaki, C.D. Hydration status, total water intake and subjective feelings of adolescents living in a hot environment, during a typical school day. Int. J. Adolesc. Med. Health 2019. [Google Scholar] [CrossRef]
- Bar-Or, O.; Dotan, R.; Inbar, O.; Rotshtein, A.; Zonder, H. Voluntary hypohydration in 10- to 12-year-old boys. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1980, 48, 104–108. [Google Scholar] [CrossRef]
- Popkin, B.M.; D’Anci, K.E.; Rosenberg, I.H. Water, hydration, and health. Nutr. Rev. 2010, 68, 439–458. [Google Scholar] [CrossRef]
- Pross, N. Effects of dehydration on brain functioning: A life-span perspective. Ann. Nutr. Metab. 2017, 70, 30–36. [Google Scholar] [CrossRef]
- D’Anci, K.E.; Constant, F.; Rosenberg, I.H. Hydration and cognitive function in children. Nutr. Rev. 2006, 64, 457–464. [Google Scholar]
- Maughan, R.J. Impact of mild dehydration on wellness and on exercise performance. Eur. J. Clin. Nutr. 2003, 57, S19. [Google Scholar] [CrossRef]
- Institute of Medicine (US); Panel on Dietary Reference Intakes for Electrolytes, & Water. DRI, Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate; National Academy Press: Washington, DC, USA, 2005. [Google Scholar]
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific opinion on dietary reference values for water. EFSA J. 2010, 8, 1459. [Google Scholar]
- Drewnowski, A.; Rehm, C.D.; Constant, F. Water and beverage consumption among children age 4-13y in the United States: Analyses of 2005–2010 NHANES data. Nutr. J. 2013, 12, 85. [Google Scholar] [CrossRef]
- Piernas, C.; Barquera, S.; Popkin, B.M. Current patterns of water and beverage consumption among Mexican children and adolescents aged 1–18 years: Analysis of the Mexican National Health and Nutrition Survey 2012. Public Health Nutr. 2014, 17, 2166–2175. [Google Scholar] [CrossRef]
- Vieux, F.; Maillot, M.; Constant, F.; Drewnowski, A. Water and beverage consumption patterns among 4 to 13-year-old children in the United Kingdom. BMC Public Health 2017, 17, 479. [Google Scholar] [CrossRef]
- Vieux, F.; Maillot, M.; Constant, F.; Drewnowski, A. Water and beverage consumption among children aged 4–13 years in France: Analyses of INCA 2 (Étude Individuelle Nationale des Consommations Alimentaires 2006–2007) data. Public Health Nutr. 2016, 19, 2305–2314. [Google Scholar] [CrossRef]
- Jomaa, L.; Hwalla, N.; Constant, F.; Naja, F.; Nasreddine, L. Water and beverage consumption among children aged 4–13 years in Lebanon: Findings from a National Cross-Sectional Study. Nutrients 2016, 8, 554. [Google Scholar] [CrossRef]
- Sui, Z.; Zheng, M.; Zhang, M.; Rangan, A. Water and beverage consumption: Analysis of the Australian 2011–2012 National Nutrition and Physical Activity Survey. Nutrients 2016, 8, 678. [Google Scholar] [CrossRef]
- Ng, S.W.; Zaghloul, S.; Ali, H.I.; Harrison, G.; Yeatts, K.; El Sadig, M.; Popkin, B.M. Nutrition Transition in the United Arab Emirates (UAE). Eur. J. Clin. Nutr. 2011, 65, 1328–1337. [Google Scholar] [CrossRef]
- Wang, Y.C.; Ludwig, D.S.; Sonneville, K.; Gortmaker, S.L. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch. Pediatr. Adolesc. Med. 2009, 163, 336–343. [Google Scholar] [CrossRef]
- AlBlooshi, A.; Shaban, S.; AlTunaiji, M.; Fares, N.; AlShehhi, L.; AlShehhi, H.; AlMazrouei, A.; Souid, A.K. Increasing obesity rates in school children in United Arab Emirates. Obes. Sci. Pract. 2016, 2, 196–202. [Google Scholar] [CrossRef]
- Ng, S.W.; Zaghloul, S.; Ali, H.I.; Harrison, G.; Popkin, B.M. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf States. Obes. Rev. 2011, 12, 1–13. [Google Scholar] [CrossRef]
- Ali, H.I.; Ng, S.W.; Zaghloul, S.; Harrison, G.G.; Qazaq, H.S.; El Sadig, M.; Yeatts, K. High proportion of 6 to 18-year-old children and adolescents in the United Arab Emirates are not meeting dietary recommendations. Nutr. Res. 2013, 33, 447–456. [Google Scholar] [CrossRef]
- Raper, N.; Perloff, B.; Ingwersen, L.; Steinfeldt, L.; Anand, J. An overview of USDA’s dietary intake data system. J. Food Compos. Anal. 2004, 17, 545–555. [Google Scholar] [CrossRef]
- Moshfegh, A.J.; Rhodes, D.G.; Baer, D.J.; Murayi, T.; Clemens, J.C.; Rumpler, W.V.; Paul, D.R.; Sebastian, R.S.; Kuczynski, K.J.; Ingwersen, L.A.; et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 2008, 88, 324–332. [Google Scholar] [CrossRef]
- Conway, J.M.; Ingwersen, L.A.; Vinyard, B.T.; Moshfegh, A.J. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am. J. Clin. Nutr. 2003, 77, 1171–1178. [Google Scholar] [CrossRef]
- Conway, J.M.; Ingwersen, L.A.; Moshfegh, A.J. Accuracy of dietary recall using the USDA five-step multiple-pass method in men: An observational validation study. J. Am. Diet. Assoc. 2004, 104, 595–603. [Google Scholar] [CrossRef]
- Montgomery, C.; Reilly, J.J.; Jackson, D.M.; Kelly, L.A.; Slater, C.; Paton, J.Y.; Grant, S. Validation of energy intake by 24-h multiple pass recall: Comparison with total energy expenditure in children aged 5-7 years. Br. J. Nutr. 2005, 93, 671–676. [Google Scholar] [CrossRef]
- Walker, J.L.; Ardouin, S.; Burrows, T. The validity of dietary assessment methods to accurately measure energy intake in children and adolescents who are overweight or obese: A systematic review. Eur. J. Clin. Nutr. 2018, 72, 185. [Google Scholar] [CrossRef]
- Börnhorst, C.; Bel-Serrat, S.; Pigeot, I.; Huybrechts, I.; Ottavaere, C.; Sioen, I.; De Henauw, S.; Mouratidou, T.; Mesana, M.I.; Westerterp, K.; et al. Validity of 24-h recalls in (pre-) school aged children: Comparison of proxy-reported energy intakes with measured energy expenditure. Clin. Nutr. 2014, 33, 79–84. [Google Scholar] [CrossRef]
- Kuwait Institute for Scientific Research. Kuwait Food Instruction Booklet; KISR: Kuwait City, Kuwait, 2010. [Google Scholar]
- Zaghloul, S.; Al-Hooti, S.N.; Al-Hamad, N.; Al-Zenki, S.; Alomirah, H.; Alayan, I.; Al-Attar, H.; Al-Othman, A.; Al-Shami, E.; Al-Somaie, M.; et al. Evidence for nutrition transition in Kuwait: Over-consumption of macronutrients and obesity. Public Health Nutr. 2013, 16, 596–607. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef]
- Malik, M.; Bakir, A. Prevalence of overweight and obesity among children in the United Arab Emirates. Obes. Rev. 2007, 8, 15–20. [Google Scholar] [CrossRef]
- Al-Nakeeb, Y.; Lyons, M.; Collins, P.; Al-Nuaim, A.; Al-Hazzaa, H.; Duncan, M.J.; Nevill, A. Obesity, physical activity and sedentary behavior amongst British and Saudi youth: A cross-cultural study. Int. J. Environ. Res. Public Health 2012, 9, 1490–1506. [Google Scholar] [CrossRef]
- Booth, M. Assessment of physical activity: An international perspective. Res. Q. Exerc. Sport 2000, 71, 114–120. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M. Health-enhancing physical activity among Saudi adults using the International Physical Activity Questionnaire (IPAQ). Public Health Nutr. 2007, 10, 59–64. [Google Scholar] [CrossRef]
- Hagstromer, M.; Oja, P.; Sjostrom, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Qahoush, R.; Stotts, N.; Alawneh, M.S.; Froelicher, E.S. Physical activity in Arab women in Southern California. Eur. J. Cardiovasc. Nurs. 2010, 9, 263–271. [Google Scholar] [CrossRef]
- ESHA Research. ESHA Food Processor v.10.4; ESHA Research: Salem, OR, USA, 2010. [Google Scholar]
- Kuwait Institute for Scientific Research. Food Composition Tables for Kuwait Composite Dishes; Kuwait Institute for Scientific Research: Kuwait City, Kuwait, 1998. [Google Scholar]
- Dashti, B.H.; Al-Awadi, F.; Khalafawi, M.S.; Al-Zenki, S.; Sawaya, W. Nutrient contents of some traditional Kuwaiti dishes: Proximate composition, and phytate content. Food Chem. 2001, 74, 169–175. [Google Scholar] [CrossRef]
- Al-Amiri, H.A.; Al-Otaibi, J.A.; Al-Foudari, M.Y.; Heji, A.H.B. The nutritive value of selected commonly consumed Kuwaiti dishes. Int. J. Food Sci. Nutr. 2009, 60, 668–676. [Google Scholar] [CrossRef]
- Committee on Sports Medicine and Fitness. Climatic heat stress and the exercising child and adolescent. Pediatrics 2000, 106, 158–159. [Google Scholar] [CrossRef]
- Walia, T.; Brigi, C.; Odeh, R.; Maree, B.H.; Yarub, K.R. Parental perceptions and drinking water source among pediatric population in the United Arab Emirates. J. Int. Oral Health 2019, 11, 61–65. [Google Scholar] [CrossRef]
- International Bottled Water Association. Available online: https://www.bottledwater.org/economics/industry-statistics (accessed on 27 May 2019).
- Shomar, B.; Hawari, J. Desalinated drinking water in the GCC countries—The need to address consumer perceptions. Environ. Res. 2017, 158, 203–211. [Google Scholar] [CrossRef]
- Maraqa, M.A.; Ghoudi, K. Survey of public attitude towards bottled and tap water quality in the UAE. Glob. Nest J. 2015, 17, 607–617. [Google Scholar]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Després, J.P.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A Meta-analysis. Diabetes Care 2010, 33, 2477–2483. [Google Scholar] [CrossRef]
- Scharf, R.J.; DeBoer, M.D. Sugar-Sweetened Beverages and Children’s Health. Annu. Rev. Public Health 2016, 37, 273–293. [Google Scholar] [CrossRef]
- UAE Government. Available online: https://government.ae/en/information-and-services/finance-and-investment/taxation/excise-tax (accessed on 27 May 2019).
- Warren, J.; Guelinckx, I.; Livingstone, B.; Potischman, N.; Nelson, M.; Foster, E.; Holmes, B. Challenges in the assessment of total fluid intake in children and adolescents: A discussion paper. Eur. J. Nutr. 2018, 57, 43–51. [Google Scholar] [CrossRef]
- Grummon, A.H.; Sokol, R.L.; Hecht, C.A.; Patel, A.I. Assessing Beverage Intake in Children and Adolescents: State of the Science, Recommendations and Resources for Evaluation; University of California, Agriculture and Natural Resources: Oakland, CA, USA, 2018. [Google Scholar]
- Malisova, O.; Athanasatou, A.; Pepa, A.; Husemann, M.; Domnik, K.; Braun, H.; Mora-Rodriguez, R.; Ortega, J.F.; Fernandez-Elias, V.E.; Kapsokefalou, M. Water intake and hydration indices in healthy European adults: The European Hydration Research Study (EHRS). Nutrients 2016, 8, 204. [Google Scholar] [CrossRef]



| Variables | n | Total Water Intake ‡ | Plain Drinking Water ‡ | Water from Beverages §,‡ | Water from Food ‡ | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Ψ ± SEM | Coefficient (95% CI) | Mean Ψ ± SEM | Coefficient (95% CI) | Mean Ψ ± SEM | Coefficient (95% CI) | Mean Ψ ± SEM | Coefficient (95% CI) | ||
| All | 527 | 1778.4 ± 33.79 | 917.3 ± 26.05 | 376.39 ± 12.10 | 484.7 ± 11.81 | ||||
| Age (n = 527) | |||||||||
| 6–10 years Ω | 255 | 1561.1 ± 35.68 | 776.9 ± 27.35 | 347.4 ± 15.92 | 436.8 ±15.14 | ||||
| 11–18 years | 272 | 1982.1 ± 53.46 | 421.02 (293.07, 548.97 ***) | 1049.0 ± 41.99 | 272.09 (172.27, 371.91 ***) | 403.6 ± 17.95 | 56.17 (8.80, 103.54 *) | 529.6 ± 17.54 | 92.76 (46.99, 138.53 ***) |
| Sex (n = 527) | |||||||||
| Male Ω | 258 | 1899.1 ± 50.58 | 966.4 ± 37.58 | 419.2 ± 17.31 | 513.5 ± 18.29 | ||||
| Female | 269 | 1662.7 ± 43.98 |
−236.37 (−367.71, −105.02 ***) | 870.3 ± 35.97 |
−96.12 (−198.26, 6.03) | 335.3 ± 16.57 |
−83.89 (−130.94, −36.84 **) | 457.1 ± 14.92 | −56.36 (−102.55, −10.17 *) |
| BMI (n = 518) | |||||||||
| Underweight Ω | 70 | 1592.4 ± 91.09 | 822.4 ± 73.65 | 341.2 ± 30.25 | 428.8 ± 26.93 | ||||
| Normal | 281 | 1781.5 ± 48.06 |
189.11 (−14.89, 393.12) | 931.8 ± 39.66 |
109.40 (−48.34, 267.15) | 384.7 ± 16.45 |
43.54 (−29.42, 116.49) | 464.9 ± 13.87 | 36.17 (−33.76, 106.10) |
| Overweight | 94 | 1821.2 ± 66.76 |
228.80 (−12.30, 469.90) | 917.0 ± 42.76 |
94.59 (−91.84, 281.02) | 389.5 ± 30.32 |
48.29 (−37.93, 134.51) | 514.7 ± 30.03 | 85.92 (3.27, 168.56 *) |
| Obese | 73 | 1894.8 ± 97.34 |
302.47 (47.00, 557.94 *) | 993.4 ± 61.36 |
171.00 (−26.55, 368.54) | 358.7 ± 33.69 |
17.57 (−73.79, 108.93) | 542.7 ± 43.56 | 113.91 (26.33, 201.48 *) |
| Physical Activity level (n = 501) | |||||||||
| Low Ω | 187 | 1767.2 ± 64.64 | 889.9 ± 49.91 | 391.9 ± 19.44 | 485.4 ± 20.96 | ||||
| Moderate | 129 | 1730.7 ± 55.29 |
−36.45 (−212.35, 139.46) | 904.5 ± 41.29 |
14.54 (−121.93, 151.01) | 358.7 ± 26.26 |
−33.14 (−96.25, 29.96) | 467.5 ± 24.70 | −17.84 (−79.34, 43.65) |
| High | 185 | 1844.8 ± 56.57 |
77.62 (−81.75, 236.99) | 975.0 ± 44.89 |
85.08 (−38.56, 208.72) | 377.2 ± 20.78 |
−14.68 (−71.86, 42.49) | 492.6 ± 18.69 | 7.22 (−48.50, 62.94) |
| Quintiles of wealth (n = 492) | |||||||||
| 1 Ω | 73 | 1721.3 ± 70.59 | 903.9 ± 55.12 | 329.5 ± 30.03 | 487.9 ± 30.03 | ||||
| 2 | 111 | 1765.5 ± 73.25 |
44.25 (−184.46, 272.97) | 902.9 ± 55.88 |
−1.02 (−178.81, 176.77) | 391.6 ± 25.48 |
61.58 (−20.25, 143.41) | 471.6 ± 27.81 | −16.30 (−95.84, 63.24) |
| 3 | 89 | 1861.4 ± 108.26 |
140.10 (−99.57, 379.76) | 965.8 ± 87.69 |
61.88 (−124.42, 248.19) | 391.5 ± 33.90 |
62.05 (−23.70, 147.80) | 504.1 ± 31.56 | 16.16 (−67.19, 99.52) |
| 4 | 97 | 1673.3 ± 66.45 |
−47.94 (−283.11, 187.23) | 884.2 ± 51.84 |
−19.73 (−202.54, 163.08) | 354.2 ± 27.62 |
24.72 (−59.42, 108.86) | 435.0 ± 21.60 | −52.93 (−134.72, 28.85) |
| 5 | 122 | 1798.9 ± 66.85 |
77.58 (−147.00, 302.16) | 916.3 ± 49.55 |
12.41 (−162.17, 186.99) | 388.0 ± 23.89 |
58.55 (−21.81, 138.91) | 494.5 ± 24.44 | 6.62 (−71.48, 84.73) |
| Residence type (n = 527) | |||||||||
| Urban Ω | 282 | 1774.1 ± 45.36 | 924.6 ± 35.09 | 364.9 ± 16.31 | 484.6 ± 15.8 | ||||
| Rural | 245 | 1783.4 ± 50.65 |
9.32 (−123.88, 142.52) | 908.9 ± 38.92 |
−15.69 (−118.39, 87.01) | 389.6 ± 18.03 | 24.76 (−22.90, 72.42) | 484.8 ± 17.75 | 0.25 (−46.30, 46.80) |
| Variables | Total Water Intake ‡ | Plain Drinking Water ‡ | Water from Beverages §,‡ | Water from Food ‡ | ||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI | |
| Age | ||||||||
| 6–10 years Ω | ||||||||
| 11–18 years | 419.48 | 280.77, 558.20 *** | 287.34 | 176.87, 397.80 *** | 47.75 | −3.44, 98.94 | 84.40 | 35.84, 132.96 ** |
| Sex | ||||||||
| Male Ω | ||||||||
| Female | −227.94 | −368.92, −86.96 ** | −88.88 | −201.14, 23.38 | −83.77 | −135.80, −31.75 ** | −55.29 | −104.64, −5.94 * |
| BMI | ||||||||
| Underweight Ω | ||||||||
| Normal | 110.33 | −95.33, 316.00 | 74.16 | −89.61, 237.94 | 35.94 | −39.96, 111.84 | 0.23 | −71.77, 72.23 |
| Overweight | 175.41 | −67.53, 418.34 | 60.29 | −133.16, 253.74 | 54.00 | −35.65, 143.66 | 61.11 | −23.93, 146.16 |
| Obese | 237.66 | −21.74, 497.07 | 118.90 | −87.67, 325.47 | 35.18 | −60.55, 130.91 | 83.58 | −7.23, 174.39 |
| Physical Activity level | ||||||||
| Low Ω | ||||||||
| Moderate | −15.93 | −192.73, 160.88 | 31.05 | −109.74, 171.84 | −33.30 | −98.55, 31.95 | −13.68 | −75.57, 48.22 |
| High | 83.47 | −83.29, 250.23 | 98.35 | −34.44, 231.14 | −33.68 | −95.23, 27.86 | 18.80 | −39.58, 77.18 |
| Quintiles of wealth | ||||||||
| 1 Ω | ||||||||
| 2 | −10.66 | −242.38, 221.07 | −27.63 | −212.16, 156.89 | 50.87 | −34.65, 136.38 | −33.89 | −115.01, 47.23 |
| 3 | 139.95 | −104.76, 384.67 | 67.98 | −126.89, 262.86 | 39.89 | −50.42, 130.20 | 32.08 | −53.59, 117.75 |
| 4 | −70.24 | −307.37, 166.89 | −42.76 | −231.59, 146.07 | 19.81 | −67.70, 107.32 | −47.29 | −130.31, 35.72 |
| 5 | 24.16 | −201.87, 250.20 | −28.51 | −208.51, 151.48 | 40.73 | −42.68, 124.15 | 11.94 | −67.19, 91.07 |
| Residence type | ||||||||
| Urban Ω | ||||||||
| Rural | −9.42 | −149.26, 130.43 | −26.72 | −138.08, 84.64 | 13.02 | −38.59, 64.62 | 4.29 | −44.67, 53.25 |
| Variable | All Participants (n = 527) | 6–8 Years (n = 160) | 9–13 Years (n = 196) | 14–18 Years (n = 171) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean Intake (mL/day) | % of TWI | Mean Intake(mL/day) | % of TWI | Mean Intake (mL/day) | % of TWI | Mean Intake (mL/day) | % of TWI | |
| Total water intake | 1778.4 ± 33.79 | 100 | 1437.0 ± 38.96 a | 100 | 1793.8 ± 47.07 b | 100 | 2080.2 ± 73.92 c | 100 |
| Plain drinking water | 917.3 ± 26.05 | 51.6 | 698.1 ± 30.73 a | 48.6 | 922.2 ± 36.58 b | 51.4 | 1116.9 ± 58.20 c | 53.7 |
| Bottled water | 755.8 ± 26.94 | 42.5 | 577.0 ± 35.22 a | 40.2 | 741.1 ± 43.41 b | 41.3 | 940.0 ± 54.58 c | 45.2 |
| Tap water | 161.5 ± 20.43 | 9.1 | 121.1 ± 24.14 a | 8.4 | 181.1 ± 28.81 a | 10.1 | 176.9 ± 48.63 a | 8.5 |
| Non-caloric beverages | 11.0 ± 2.13 | 0.6 | 4.4 ± 2.24 a | 0.3 | 14.8 ± 4.07 a | 0.9 | 12.8 ± 4.10 a | 0.6 |
| Sugar-sweetened beverages | 246.9 ± 10.90 | 13.9 | 198.1 ± 15.65 a | 13.8 | 238.7 ± 18.02 a | 13.3 | 302.0 ± 21.47 b | 14.5 |
| Fruit juices | 15.3 ± 2.71 | 0.9 | 13.4 ± 4.35 a | 0.9 | 16.8 ± 4.67 a | 1 | 15.3 ± 4.96 a | 0.8 |
| Milk | 91.8 ± 5.95 | 5.2 | 107.8 ± 12.50 a | 7.5 | 92.1 ± 8.99 a | 5.2 | 76.4 ± 9.58 a | 3.7 |
| Other | 8.9 ± 1.97 | 0.5 | 2.0 ± 1.52 a | 0.2 | 5.2 ± 2.05 a | 0.3 | 19.5 ± 5.33 b | 0.9 |
| Food | 484.7 ± 11.81 | 27.3 | 412.0 ± 16.57 a | 28.7 | 499.3 ± 19.72 b | 27.9 | 536.0 ± 23.06 b | 25.8 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, H.I.; Al Dhaheri, A.S.; Elmi, F.; Ng, S.W.; Zaghloul, S.; Ohuma, E.O.; Qazaq, H.S. Water and Beverage Consumption among a Nationally Representative Sample of Children and Adolescents in the United Arab Emirates. Nutrients 2019, 11, 2110. https://doi.org/10.3390/nu11092110
Ali HI, Al Dhaheri AS, Elmi F, Ng SW, Zaghloul S, Ohuma EO, Qazaq HS. Water and Beverage Consumption among a Nationally Representative Sample of Children and Adolescents in the United Arab Emirates. Nutrients. 2019; 11(9):2110. https://doi.org/10.3390/nu11092110
Chicago/Turabian StyleAli, Habiba I., Ayesha S. Al Dhaheri, Fadima Elmi, Shu Wen Ng, Sahar Zaghloul, Eric O. Ohuma, and Husain S. Qazaq. 2019. "Water and Beverage Consumption among a Nationally Representative Sample of Children and Adolescents in the United Arab Emirates" Nutrients 11, no. 9: 2110. https://doi.org/10.3390/nu11092110
APA StyleAli, H. I., Al Dhaheri, A. S., Elmi, F., Ng, S. W., Zaghloul, S., Ohuma, E. O., & Qazaq, H. S. (2019). Water and Beverage Consumption among a Nationally Representative Sample of Children and Adolescents in the United Arab Emirates. Nutrients, 11(9), 2110. https://doi.org/10.3390/nu11092110







