Abstract
Several factors affect dental implant osseointegration, including surgical issues, bone quality and quantity, and host-related factors, such as patients’ nutritional status. Many micronutrients might play a key role in dental implant osseointegration by influencing some alveolar bone parameters, such as healing of the alveolus after tooth extraction. This scoping review aims to summarize the role of dietary supplements in optimizing osseointegration after implant insertion surgery. A technical expert panel (TEP) of 11 medical specialists with expertise in oral surgery, bone metabolism, nutrition, and orthopedic surgery performed the review following the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) model. The TEP identified micronutrients from the “European Union (EU) Register of nutrition and health claims made on foods” that have a relationship with bone and tooth health, and planned a PubMed search, selecting micronutrients previously identified as MeSH (Medical Subject Headings) terms and adding to each of them the words “dental implants” and “osseointegration”. The TEP identified 19 studies concerning vitamin D, magnesium, resveratrol, vitamin C, a mixture of calcium, magnesium, zinc, and vitamin D, and synthetic bone mineral. However, several micronutrients are non-authorized by the “EU Register on nutrition and health claims” for improving bone and/or tooth health. Our scoping review suggests a limited role of nutraceuticals in promoting osseointegration of dental implants, although, in some cases, such as for vitamin D deficiency, there is a clear link among their deficit, reduced osseointegration, and early implant failure, thus requiring an adequate supplementation.
Keywords:
dietary supplements; dental implants; osseointegration; vitamin D; magnesium; resveratrol; ascorbic acid; zinc; calcium; bone 1. Introduction
Osseointegration is defined as “a process whereby a clinically asymptomatic rigid fixation of alloplastic materials is achieved and maintained in bone during functional loading” [1]. Osseointegration is involved in dental implants healing, thus leading to a functional unit that may rehabilitate one or more missing teeth, supporting dental prosthesis.
In addition to key factors that affect the osseointegration, such as the surgical technique, bone quality and quantity, postoperative inflammation or infection, smoking habits, and implant material and surface [2,3,4,5,6,7], other factors should be taken into account, including the immunological and nutritional status of the host. Alongside the promotion of a healthy diet, such as the Mediterranean one, to achieve a desirable general health status, recently, increasing attention was paid to promoting the consumption of micronutrients that could have benefits on health and resistance to diseases [8].
Several micronutrients affecting bone metabolism were demonstrated to have an influence on skeletal system; in particular, calcium, fluorides, magnesium, potassium, vitamin B6, vitamin D, and zinc positively influence bone health, reducing the risk of fracture [9]. In addition, fat-, carbohydrate-, and cholesterol-rich diets and reduced calcium intake exhibit detrimental influences on jaw bone and alveolar bone [10]. Therefore, a specific diet regimen and micronutrients might play a key role in the different phases of dental implant osseointegration.
Recent evidence demonstrated that some nutritional regimens directly influence alveolar bone parameters in experimental models of periodontitis [11,12,13], orthodontic tooth movement [14], and bone repair after tooth extraction [15]. In particular, it was demonstrated that diet (in its different meanings of macro- and micronutrients) can affect the healing of the alveolus after tooth extraction, influencing both the morphology and the quality of alveolar bone [15].
Bone tissue repair mechanisms and bone metabolism are strongly influenced by nutritional aspects and are crucial to obtaining proper bone restoration optimizing osseointegration processes.
The aim of this scoping review is to summarize the state of the art regarding the role of micronutrients, currently available in nutraceuticals or dietary supplements, on dental implantology, highlighting which of them, supported by evidence-based medicine (EBM), might effectively have an influence on the achievement and the maintenance of osseointegration after implant insertion surgery.
2. Materials and Methods
In performing this scoping review, we followed the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) model [16].
As a first step, a technical expert panel (TEP) consisting of 11 medical specialists was established. In particular, the TEP was composed of two oral surgeons with expertise in osseointegrated dental implants, two periodontists with expertise in peri-implant oral tissues physiology and pathology, three bone specialists, two experts on scoping review methodology, one nutritionist, and one orthopedic surgeon.
2.1. Search Strategy
The TEP selected micronutrients from the “European Union (EU) Register of nutrition and health claims made on foods” that have a relationship with bone and tooth health, included in dietary supplements and nutraceuticals. Therefore, the TEP planned a research on PubMed (Public MedLine, run by the National Center of Biotechnology Information, NCBI, of the National Library of Medicine of Bethesda, Bethesda, MD, USA), selecting micronutrients as MeSH (Medical Subject Headings) terms; to each of them, the following terms were added to run the PubMed Search Builder: “dental implants”, “osseointegration”. For example: (“Vitamin D” [Mesh]) AND “Dental Implants” [Mesh]) (see Supplementary Materials, Table S1).
2.2. Study Selection
According to the objective of the study, the TEP defined the characteristics of the sources of evidence, considering for eligibility any researches published in medical literature in the last 10 years (last update on 16 October 2019), including only those in the English language.
2.3. Data Extraction and Quality Assessment
All types of studies were included in our scoping review, both pre-clinical (in vitro and animal studies) and clinical studies. Methodological quality assessment was made according to the EBM pyramid: meta-analysis, systematic review, randomized controlled trial (RCT), cohort study, case–control study, case series, and case report.
Finally, the TEP summarized the resulting micronutrients with effective and safe daily doses that improve bone and tooth health.
3. Results
From the micronutrients listed in the “EU Register of nutrition and health claims made on foods”, the TEP selected the following 18 nutraceuticals that may have influence on bone and teeth: calcium, fluorides, magnesium, potassium, resveratrol, vitamin C (ascorbic acid), vitamin D, vitamin E (alpha-tocopherol), vitamin K2 (menaquinone-7, MK7), zinc, vitamin A, vitamin B1 (thiamine), vitamin B2 (riboflavin), vitamin B3 (niacinamide), vitamin B5 (pantothenic acid), vitamin B6, vitamin B7 (biotin), and vitamin B12 (Table 1). However, according to the “EU Register of nutrition and health claims made on foods”, fluoride is non-authorized for supporting bone mineralization, and potassium is non-authorized for maintaining tooth mineralization, whereas vitamin B2, vitamin E, vitamin A, vitamin B1, vitamin B2, vitamin B3, vitamin B6, vitamin B7, and vitamin B12 are non-authorized for both functions. Moreover, potassium and zinc are not considered to influence tooth metabolism, while vitamin K2, resveratrol, and vitamin B5 are not recommended for bone and tooth metabolism according to the “EU Register of nutrition and health claims made on foods”. Among these substances, we found studies concerning nutraceuticals and dental implants or osseointegration only for vitamin D, magnesium, resveratrol, vitamin C, a mixture of calcium, magnesium, zinc, and vitamin D, and synthetic bone mineral (a supplement containing calcium, phosphate, magnesium, zinc, fluoride, and carbonate).

Table 1.
Effects of selected micronutrients on bone and tooth health.
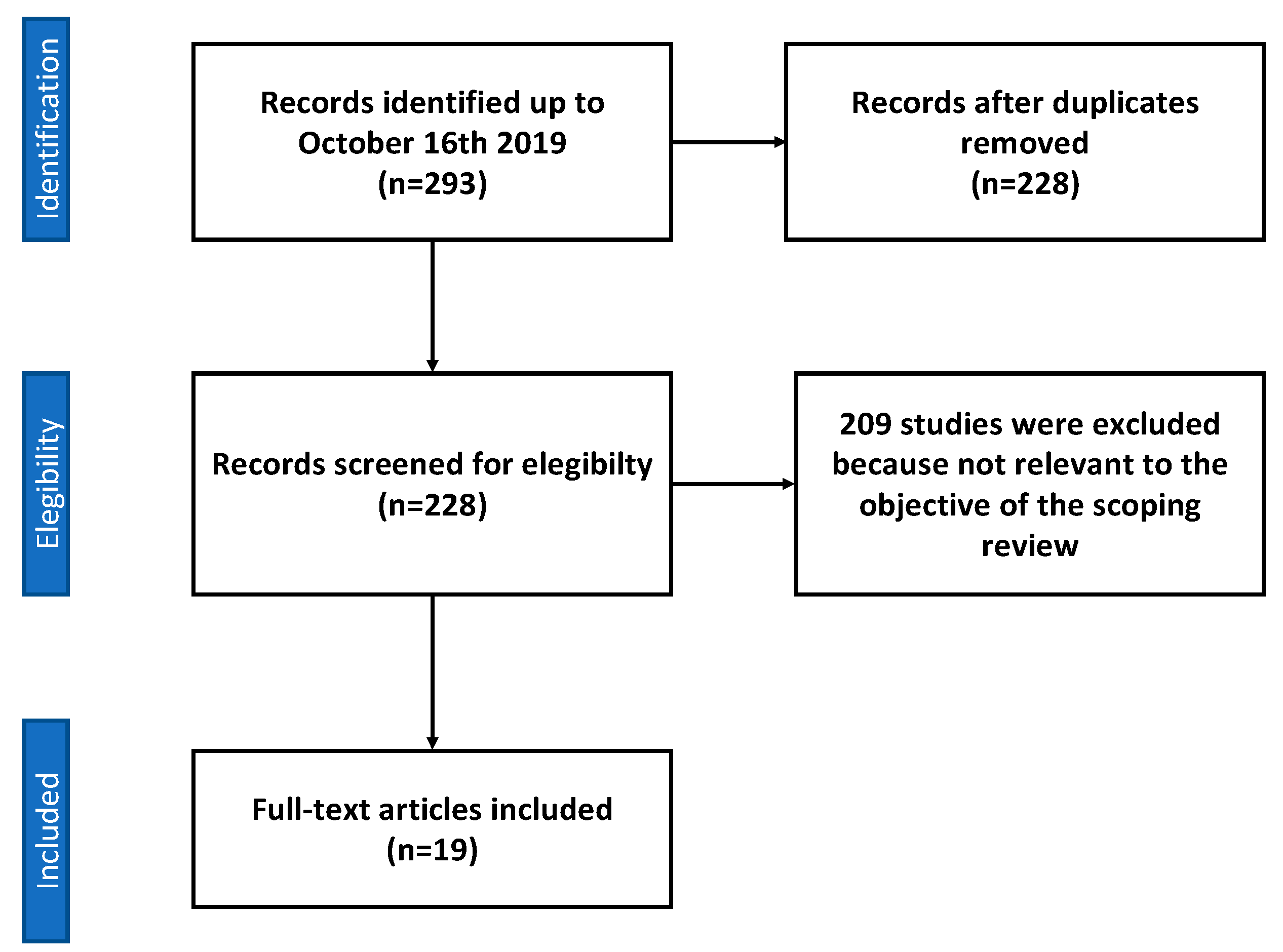
In particular, we included 11 studies concerning vitamin D, of which five were clinical studies (three retrospective studies, one case series, and one case report), and six were preclinical studies on animals: two preclinical studies on animals concerning magnesium, two preclinical studies on animals for resveratrol, one preclinical study on animals concerning the supplementation with a combination of calcium, magnesium, zinc and vitamin D, two preclinical studies on animals concerning synthetic bone mineral (composed by dicalcium phosphate dihydrate and magnesium and zinc chlorides), and one clinical study concerning vitamin C supplementation (Figure 1, Table 2).
Figure 1.
Flow diagram of sources selection process.

Table 2.
Relevant data from each study included in the scoping review.
3.1. Vitamin D
3.1.1. Animal Studies
In our scoping review, we included six preclinical studies on animal models, more precisely, on rats.
Liu et al., in 2014 [34], found that vitamin D supplementation in rats affected by chronic kidney disease (CKD) improved bone-to-implant contact (BIC) compared to CKD rats that did not receive vitamin D, making this finding comparable to that of rats without CKD. Also, the bone volume in the circumferential zone within 100 mm of the implant surface increased after vitamin D administration. At two weeks, the push-in test showed significantly better results for the vitamin D-treated group compared to untreated CKD mice.
Zhou et al., in 2012 [35], demonstrated that vitamin D supplementation in osteoporotic rats, eight weeks after implantation, improved bone volume, osseointegration, mean trabecular number, mean trabecular thickness, and trabecular connective density, while it decreased trabecular separation, as well as increased bone area density, BIC, and the maximal push-out force.
Wu et al., in 2012 [36], inserted titanium implants in diabetic rats and evaluated the effects of different kinds of diabetes therapies. The combined therapy with insulin and vitamin D showed the best effects on osseointegration, bone volume, mean trabecular thickness, mean trabecular number, connective density, mean trabecular separation, push out force, shear strength, BIC, and bone area ratio. Treatments with vitamin D or insulin only showed better results compared to untreated diabetic rats, but worse than the combined therapy. All the parameters listed above, in the combined treatment group, resulted similar to those of the control healthy group.
Akhavan et al., in 2012 [37], evaluated the effects of vitamin D supplementation on BIC in diabetic rats compared to a placebo group. At three weeks, the vitamin D group showed higher values of BIC compared to the placebo group, and also at six weeks, even if in a non-statistically significant way, leading the authors to conclude that vitamin D seems to not have an effect on the osseointegration of implants in diabetic rats.
Dvorak et al., in 2012 [38], showed that, in osteoporotic rats, a vitamin D depletion led to a significant decrease in BIC in the cortical area. In rats that received a vitamin D-free diet, followed by vitamin D repletion, no significant difference could be found compared to the control group that received a standard vitamin D diet.
Kelly et al., in 2008 [39], found that vitamin D deficiency, 14 days after implantation, led to a lower push-in test and a decreased BIC compared to a normal vitamin D status.
3.1.2. Clinical Studies
The clinical studies on vitamin D that we included in this scoping review were three retrospective studies, one case series, and one case report.
From the retrospective studies of Mangano et al. of 2016 [31] and 2018 [29], it emerged that, in patients with vitamin D deficiency, there were a higher percentage of early dental implant failures (failures that occurred before prosthesis positioning, EDIF). However, although there was a clear trend toward an increased incidence of EDIF with lower serum 25(OH)D, no statistically significant difference was found among the three groups with different vitamin D status.
In the retrospective study of Wagner et al. of 2017 [30], osteoporosis was shown to have a significant negative influence on marginal bone loss around implants, but vitamin D significantly affected the marginal bone loss at the mesial and distal implant aspect, showing beneficial effects on the peri-implant bone formation.
Fretwurst et al., in 2016 [32], reported two cases of implant failures occurring within 15 days of surgery in patients with vitamin D deficiency; in one patient, there were even two consecutive implant failures. In both patients, after vitamin D supplementation, implants were placed successfully. The authors also noticed that failures were sometimes associated with pain and discomfort in vitamin D-deficient patients.
Also, Bryce and Macbeth, in 2014 [33], reported a case of missed osseointegration in a patient affected by severe vitamin D deficiency.
3.1.3. Magnesium
We included two animal studies that evaluated the effects of magnesium deficiency on osseointegration of titanium implants. The deficiency of magnesium led to lower cortical bone thickness, lower values of removal torque of the implants, and lower bone mineral density (BMD) [40,41]. In detail, Bellucci et al., in 2011 [40], found that a 90% reduction of magnesium intake, 90 days after implant insertion, led to lower BMD values. In the magnesium reduction group, upper and lower cortical thicknesses were significantly reduced, as well as the removal torque of the implants. On the other hand, the radiographic bone density and cortical thickness around the implants resulted similar between the two groups.
Del Barrio et al., in 2010 [41], reported that only a 90% reduced magnesium intake resulted in low BMD after implant insertion compared to both a 75% magnesium intake reduction and a normal magnesium intake.
3.1.4. Resveratrol
We found two animal studies that evaluated the effects of resveratrol intake on the osseointegration of titanium implants.
In 2018, Ribeiro et al. [42] demonstrated that supplementation of resveratrol led to an improvement in counter-torque and BIC in rats exposed to cigarette smoking, compared to rats exposed to cigarette smoking but receiving placebo. This finding seems quite relevant, considering that detrimental effects of smoking on oral health in terms of increased postoperative infections and marginal bone loss in patients receiving dental implants are well established [48,49,50]. Also, Casarin et al., in 2014 [43], demonstrated that resveratrol intake had positive effects on the biomechanical retention of the implants, because there were significantly higher average counter-torque values for implant removal in rats that received resveratrol.
3.1.5. Mixtures of Micronutrients
Pimentel et al., in 2016 [44], evaluated the effects of a mixture of calcium, magnesium, zinc, and vitamin D on rats that received titanium implants. They found that there was no statistically significant difference among the counter-torque values for implant removal, bone volume, and BIC in the placebo group when compared to the micronutrient group.
Takahashi et al., in 2016 [45], evaluated the effects of supplementation with synthetic bone mineral (SBM), a mixture of calcium phosphate dihydrate and magnesium and zinc chlorides, on titanium implants in osteoporotic rats. They found significantly higher bone volume and lower bone surface ratio in the SBM group. Moreover, the trabecular thickness increased significantly from two to four weeks after implant insertion in treated group, while the improvement of the same parameters was not significant in the control group. Also, other histomorphometric parameters significantly improved in SBM group, such as the trabecular star volume, although the between-group difference in terms of trabecular number was not significant. Finally, rats receiving SBM showed enhanced bone formation, evaluated by micro-computed tomography (micro-CT), both at two and at four weeks compared to rats fed without SBM.
Also, Watanabe et al., in 2015 [46], evaluated the effects of SBM on osseointegration in rats. They found that pull-out strength in the treated group was six times higher than in the control group two weeks after implantation and twice higher at four weeks. The BMD in the SBM group was approximately double compared to the control group at two weeks and more than double at four weeks. BMD color imaging showed that the control group colors mainly ranged from blue to yellow at two and four weeks after implantation, while the SBM group mainly occupied the orange and red end of the spectrum at two and four weeks after implantation. Given that blue and light blue, green and yellow, and orange and red represent low, medium, and high BMD, respectively, the BMD color imaging indicated that peri-implant bone had a higher BMD in the SBM group than in the control group. Fluorescence microscopy imaging of the control group revealed no green fluorescence at two weeks after implantation. However, green fluorescence was clearly observed in the SBM group at two and four weeks after implantation, while irregular bands appeared around the implants in the control group at four weeks.
3.2. Vitamin C
Li et al., in 2018 [47], evaluated the effects of vitamin C supplementation on four populations: patients receiving dental implants by guided bone regeneration (GBR), patients treated with Bio-Oss collagen, patients with chronic periodontitis receiving dental implants, and a control group without any bone grafting or periodontal disease. The authors found that vitamin C supplementation improved postoperative wound healing following dental implant surgery in patients with chronic periodontitis and in those treated with GBR or Bio-Oss collagen grafts. However, vitamin C supplementation was ineffective in decreasing the postoperative pain associated with dental implant surgery.
4. Discussion
To the best of our knowledge, this is the first scoping review to investigate the putative role of dietary supplements in affecting bone structural and mechanical properties involved in dental implant osseointegration, as well as in improving clinical outcomes, such as the maintenance of peri-implant tissue health and implant success rate.
The Federal Food, Drug, and Cosmetic Act defines a dietary supplement as a product that is intended to supplement the diet, which bears or contains one or more ingredients including a vitamin, mineral, herb, and amino acid, or a concentrate, metabolite, constituent, extract, or combinations of these [50]. The term “nutraceutical” was coined by Stephen De Felice to define “food (or parts of a food) that provides medical or health benefits, including the prevention and/or treatment of a disease”, by the fusion of the words “nutrition” and “pharmaceutical”, commonly used in marketing with no regulatory legal definition [51]. Ten years later, nutraceuticals are defined as dietary supplements that include a concentrated form of a presumed bioactive substance, originally derived from a food, but present in a non-food matrix, and used to maintain or improve health status in dosages exceeding those obtainable from conventional foods [52].
It should be stressed, however, that there is no consensus with regard to “nutraceutical” definition or similar terms. Aronson recently considered that the term “nutraceuticals” is too vague and should be abandoned, even if he did not propose any robust alternatives [53].
According to the recent data of the United States (US) Centers for Disease Control and Prevention’s National Health and Nutrition Examination Survey (NHANES), more than 25% of the US population had an insufficient intake of vitamins A, C, D, and E, as well as calcium, magnesium, and potassium in their diet; thus, the modern diet of Western countries does not seem to have an adequate intake of micronutrients. It was reported that micronutrient deficiencies affect around two billion people worldwide [54]. However, a consensus about the use of these substances, particularly concerning the adequate amount and safety, is not yet reached, even if they are supposed to have multiple physiological beneficial effects.
Several micronutrients are hypothesized to have an influence on skeletal system, particularly on jaw bone and alveolar bone [9] and on dental implant osseointegration. However, according to our findings, very few elements (i.e., vitamin D, magnesium, resveratrol, and vitamin C) were the matter of previous investigations on their role in dental implant osseointegration. Available data suggest that severe vitamin D deficiency or even the presence of established osteoporosis led to a higher implant failure rate [29,31] or to a worse BIC [34,35]. In osteoporotic rats, vitamin D depletion led to a significant decrease in BIC in the cortical area. Moreover, rats that received vitamin D showed a similar BIC to the control group [34]. Animal studies on vitamin D and osseointegration confirmed that the early stages of bone healing could be significantly influenced by vitamin D status [35,36,37,38,39,40]. In humans, Mangano et al. [29,31] reported a clear trend toward an increased incidence of early implant failures within the group with lower serum 25(OH)D levels. In particular, the authors reported 11.1% EDIF in patients with serum 25(OH)D < 10 ng/mL (severe vitamin D deficiency), 4.4% for those with 25(OH)D between 10 and 30 ng/mL, and 2.9% in patients with normal vitamin D status.
Moreover, Wagner et al. [30] showed that osteoporosis has a significant negative influence on marginal bone loss around implants and that vitamin D supplementation counteracts the marginal bone loss, with overall results of beneficial effects on the peri-implant bone formation.
Vitamin D deficiency commonly occurs in the general population. This hormone has a crucial function in skeletal mineralization, but also plays an important role in immunity and inflammatory response, increasing anti-inflammatory cytokines and decreasing pro-inflammatory ones [55].
Bashutski et al. [56] showed that, in vitamin D-deficient individuals, minimal benefits could be obtained from periodontal surgery along with an impaired post-surgical healing. Vitamin D could have other effects on osseointegration that are more related to soft tissue healing and marginal seals around implants, together with an effect on resistance against bacterial infections of the peri-implant sulcus. Also, topical applications of vitamin D were used for implant coating, showing some beneficial effects in animals, such as a reduction in crestal bone loss and an increase of BIC [57]. However, several critical issues persist regarding the use of vitamin D in enhancing osseointegration, particularly concerning its mechanism(s) of action, the influence of different serum 25(OH)D levels, and the recommended dosages required to significantly improve dental implant success rate.
Also, vitamin C deficiency may have a role in tissue healing and stability around dental implants. This micronutrient plays an important role in the biosynthesis of collagen, which is an important component of connective tissue of the gingiva, peri-implant mucosa, and alveolar bone [58]. These effects were confirmed by Li et al. [47], who found that vitamin C supplementation improved postoperative wound healing following dental implant surgery. Moreover, protective effects of this intervention on bone health could be expected, as vitamin C could hinder the effects of oxidative stress in promoting bone resorption and consequently reducing bone strength [59], although this hypothesis is not yet confirmed. However, the role of vitamin C supplementation in the general population, as well as in patients receiving dental implants, might be significantly affected by lifestyle, including smoking habits and diet, two factors that affect wound healing times. Furthermore, plasma ascorbic acid concentrations are not reported in clinical practice [60].
With regard to resveratrol, Casarin et al. [43] investigated its role on bone healing of calvarial defects in rats through messenger RNA (mRNA) quantification of bone morphogenetic protein (BMP)-2, BMP-7, osteopontin (OPN), bone sialoprotein (BSP), osteoprotegerin (OPG), and receptor activator of nuclear factor kappa B (NF-κB) ligand (RANKL). Gene expression analysis showed a higher expression of BMP-2 (p = 0.011), BMP-7 (p = 0.049), and OPN (p = 0.002) genes in the resveratrol-fed group than in the control group.
Ribeiro et al. [42] reported encouraging data about biomechanical retention and peri-implant bone formation in resveratrol-fed rats exposed to cigarette smoking inhalation, supporting a positive role of this substance in controlling different osteogenic mechanisms. Their gene expression analysis demonstrated that lower RANKL/OPG levels were detected in rats receiving resveratrol, as well as in non-smoking animals, when compared to animals exposed to smoking and receiving placebo. Both studies on resveratrol confirmed the substantial improvement in implant stability, by modulating the expression of genes involved in bone regulatory processes. However, the main limitation of findings supporting resveratrol, as well as magnesium, is the availability of animal studies only.
However, considering the results of our research, several micronutrients are non-authorized or even not considered by the “EU Register on nutrition and health claims” on the basis of current scientific evidence.
Major nutrients involved in skeletal health include calcium, phosphorus, vitamin D, magnesium, and potassium, but other micronutrients and trace elements such as boron, selenium, iron, zinc, and copper also impact bone metabolism. Information on the influence of such “minor” elements coming from studies on nutrient depletion and studies on osseointegration is still lacking.
5. Conclusions
Our scoping review overall demonstrated a lack of data about the effects of micronutrients and nutraceuticals on osseointegration of dental implants, although, for some of them, such as vitamin D, there was a clear association among their deficit, reduced osseointegration, and increased early implant failure incidence in both animal and human studies.
Some micronutrient deficiencies are supposed to increase oxidative stress and inflammation and to affect collagen structure and bone mineralization. For these reasons, it would be desirable that further studies investigate the hypothesis of an influence of micronutrients and nutraceuticals on dental implant osseointegration and long-term success, as well as the opportunity of a diet integration to enhance peri-implant wound healing, bone healing, and peri-implant tissue stability. However, data for many micronutrients that might modulate bone metabolism are lacking, and dosing regimens for dietary supplements that improve dental implant osseointegration are not defined according to available findings; furthermore, safety issues remain to be carefully investigated. In conclusion, our findings support an ancillary role of vitamin D, in patients with vitamin D deficiency, as well as vitamin C supplementation, in facilitating the success of the dental implant surgery.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/12/1/268/s1, Table S1: Search strategy.
Author Contributions
Conceptualization, L.N., A.M., S.M., L.G., and G.I.; methodology, L.N., A.M., S.M., M.P., M.A., S.L., G.T., M.B., and G.I.; writing—original draft preparation, L.N., A.M., M.P., M.A., G.C., and G.I.; writing—review and editing, L.N., A.M., M.P., M.A., S.L., G.T., M.B., G.C., L.G., and G.I.; funding acquisition, L.G. and G.I. All authors read and agreed to the published version of the manuscript.
Funding
The authors would like to acknowledge the Vanvitelli per la Ricerca (VALERE) program for the allocation of funding that aims to publish University of Campania “Luigi Vanvitelli” research products.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Zarb, G.A.; Albrektsson, T. Osseointegration—A requiem for the periodontal ligament? Int. J. Periodontol. Restor. Dent. 1991, 11, 88–91. [Google Scholar]
- Goiato, M.C.; Dos Santos, D.M.; Santiago, J.F., Jr.; Moreno, A.; Pellizzer, E.P. Longevity of dental implants in type IV bone: A systematic review. Int. J. Oral Maxillofac. Surg. 2014, 43, 1108–1116. [Google Scholar] [CrossRef]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur. J. Oral Sci. 1998, 106, 527–551. [Google Scholar] [CrossRef]
- Esposito, M.; Thomsen, P.; Ericson, L.E.; Lekholm, U. Histopathologic observations on early oral implant failures. Int. J. Oral Maxillofac. Implants 1999, 14, 798–810. [Google Scholar]
- Huynh-Ba, G.; Friedberg, J.R.; Vogiatzi, D.; Ioannidou, E. Implant failure predictors in the posterior maxilla: A retrospective study of 273 consecutive implants. J. Periodontol. 2008, 79, 2256–2261. [Google Scholar] [CrossRef] [PubMed]
- Sverzut, A.T.; Stabile, G.A.; de Moraes, M.; Mazzonetto, R.; Moreira, R.W. The influence of tobacco on early dental implant failure. J. Oral Maxillofac. Surg. 2008, 66, 1004–1009. [Google Scholar] [CrossRef] [PubMed]
- Urban, T.; Kostopoulos, L.; Wenzel, A. Immediate implant placement in molar regions: Risk factors for early failure. Clin. Oral Implants Res. 2012, 23, 220–227. [Google Scholar] [CrossRef] [PubMed]
- WHO Micronutrients. Available online: https://www.who.int/nutrition/topics/micronutrients/en/ (accessed on 27 December 2019).
- Iolascon, G.; Gimigliano, R.; Bianco, M.; De Sire, A.; Moretti, A.; Giusti, A.; Malavolta, N.; Migliaccio, S.; Migliore, A.; Napoli, N.; et al. Are Dietary Supplements and Nutraceuticals Effective for Musculoskeletal Health and Cognitive Function? A Scoping Review. J. Nutr. Health Aging 2017, 21, 527–538. [Google Scholar] [CrossRef]
- Montalvany-Antonucci, C.C.; Zicker, M.C.; Oliveira, M.C.; Macari, S.; Madeira, M.F.M.; Andrade IJr Ferreira, A.V.; Silva, T.A. Diet versus jaw bones: Lessons from experimental models and potential clinical implications. Nutrition 2018, 45, 59–67. [Google Scholar] [CrossRef]
- Aguirre, J.I.; Akhter, M.P.; Kimmel, D.B.; Pingel, J.; Xia, X.; Williams, A.; Jorgensen, M.; Edmonds, K.; Lee, J.Y.; Reinhard, M.K.; et al. Enhanced alveolar bone loss in a model of non-invasive periodontitis in rice rats. Oral Dis. 2012, 18, 459–468. [Google Scholar] [CrossRef]
- Kametaka, S.; Miyazaki, T.; Inoue, Y.; Hayashi, S.I.; Takamori, A.; Miyake, Y.; Suginaka, H. The effect of ofloxacin on experimental periodontitis in hamsters infected with Actinomyces viscosus. J. Periodontol. 1989, 60, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Fujita, Y.; Maki, K. High-fat diet induced periodontitis in mice through lipopolysaccharides (LPS) receptor signaling: Protective action of estrogens. BMC Obes. 2016, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- De Albuquerque Taddei, S.R.; Madeira, M.F.M.; de Abreu Lima, I.L.; Queiroz-Junior, C.M.; Moura, A.P.; Oliveira, D.D.; Andrade, I., Jr.; da Glória Souza, D.; Teixeira, M.M.; da Silva, T.A. Effect of Lithothamnium sp and calcium supplements in strain- and infection-induced bone resorption. Angle Orthod. 2014, 84, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Barò, M.A.; Rocamundi, M.R.; Viotto, O.J.; Ferreyra, R.S. Alveolar wound healing in rats fed on high sucrose diet. Acta Odontol. Latinoam. 2013, 26, 97–103. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Dermience, M.; Lognay, G.; Mathieu, F.; Goyens, P. Effects of thirty elements on bone metabolism. J. Trace Elem. Med. Biol. 2015, 32, 86–106. [Google Scholar] [CrossRef]
- Farley, J.R.; Wergedal, J.E.; Baylink, D.J. Fluoride directly stimulates proliferation and alkaline phosphatase activity of bone-forming cells. Science 1983, 222, 330–332. [Google Scholar] [CrossRef]
- Dommisch, H.; Kuzmanova, D.; Jönsson, D.; Grant, M.; Chapple, I. Effect of micronutrient malnutrition on periodontal disease and periodontal therapy. Periodontology 2000 2018, 78, 129–153. [Google Scholar] [CrossRef]
- Bushinsky, D.A.; Riordon, D.R.; Chan, J.S.; Krieger, N.S. Decreased potassium stimulates bone resorption. Am. J. Physiol. Ren. Physiol. 1997, 272, F774–F780. [Google Scholar] [CrossRef]
- Ornstrup, M.J.; Harsløf, T.; Sørensen, L.; Stenkjær, L.; Langdahl, B.L.; Pedersen, S.B. Resveratrol Increases Osteoblast Differentiation in Vitro Independently of Inflammation. Calcif. Tissue Int. 2016, 99, 155–163. [Google Scholar] [CrossRef]
- Choi, H.K.; Kim, G.J.; Yoo, H.S.; Song, D.H.; Chung, K.H.; Lee, K.J.; Koo, Y.T.; An, J.H. Vitamin C Activates Osteoblastogenesis and Inhibits Osteoclastogenesis via Wnt/β-Catenin/ATF4 Signaling Pathways. Nutrients 2019, 11, 506. [Google Scholar] [CrossRef]
- Kim, H.-N.; Lee, J.-H.; Jin, W.J.; Lee, Z.H. α-Tocopheryl Succinate Inhibits Osteoclast Formation by Suppressing Receptor Activator of Nuclear Factor-kappaB Ligand (RANKL) Expression and Bone Resorption. J. Bone Metab. 2012, 19, 111–120. [Google Scholar] [CrossRef]
- Myneni, V.D.; Mezey, E. Regulation of bone remodeling by vitamin K2. Oral Dis. 2017, 23, 1021–1028. [Google Scholar] [CrossRef]
- Yamaguchi, M. Nutritional factors and bone homeostasis: Synergistic effect with zinc and genistein in osteogenesis. Mol. Cell. Biochem. 2012, 366, 201–221. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M. Role of nutritional zinc in the prevention of osteoporosis. Mol. Cell. Biochem. 2010, 338, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Cruz, A.C.C.; Cardozo, F.T.G.S.; Magini, R.S.; Simões, C.M.O. Retinoic acid increases the effect of bone morphogenetic protein type 2 on osteogenic differentiation of human adipose-derived stem cells. J. Appl. Oral Sci. 2019, 27, e20180317. [Google Scholar] [CrossRef]
- Fratoni, V.; Brandi, M.L. B vitamins, homocysteine and bone health. Nutrients 2015, 7, 2176–2192. [Google Scholar] [CrossRef]
- Mangano, F.; Ghertasi Oskouei, S.; Paz, A.; Mangano, N.; Mangano, C. Low serum vitamin D and early dental implant failure: Is there a connection? A retrospective clinical study on 1740 implants placed in 885 patients. J. Dent. Res. Dent. Clin. Dent. Prospects 2018, 12, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Wagner, F.; Schuder, K.; Hof, M.; Heuberer, S.; Seemann, R.; Dvorak, G. Does osteoporosis influence the marginal peri-implant bone level in female patients? A cross-sectional study in a matched collective. Clin. Implant Dent. Relat. Res. 2017, 19, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Mortellaro, C.; Mangano, N.; Mangano, C. Is Low Serum Vitamin D Associated with Early Dental Implant Failure? A Retrospective Evaluation on 1625 Implants Placed in 822 Patients. Mediat. Inflamm. 2016, 2016, 5319718. [Google Scholar] [CrossRef] [PubMed]
- Fretwurst, T.; Grunert, S.; Woelber, J.P.; Nelson, K.; Semper-Hogg, W. Vitamin D deficiency in early implant failure: Two case reports. Int. J. Implant Dent. 2016, 2, 24. [Google Scholar] [CrossRef] [PubMed]
- Bryce, G.; MacBeth, N. Vitamin D deficiency as a suspected causative factor in the failure of an immediately placed dental implant: A case report. J. R. Naval Med. Serv. 2014, 100, 328–332. [Google Scholar]
- Liu, W.; Zhang, S.; Zhao, D.; Zou, H.; Sun, N.; Liang, X.; Dard, M.; Lanske, B.; Yuan, Q. Vitamin D supplementation enhances the fixation of titanium implants in chronic kidney disease mice. PLoS ONE 2014, 9, e95689. [Google Scholar] [CrossRef]
- Zhou, C.; Li, Y.; Wang, X.; Shui, X.; Hu, J. 1,25Dihydroxy vitamin D3 improves titanium implant osseointegration in osteoporotic rats. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, S174–S178. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.Y.; Yu, T.; Yang, X.Y.; Li, F.; Ma, L.; Yang, Y.; Liu, X.G.; Wang, Y.Y.; Gong, P. Vitamin D3 and insulin combined treatment promotes titanium implant osseointegration in diabetes mellitus rats. Bone 2013, 52, 1–8. [Google Scholar] [CrossRef]
- Akhavan, A.; Noroozi, Z.; Shafiei, A.A.; Haghighat, A.; Jahanshahi, G.R.; Mousavi, S.B. The effect of vitamin D supplementation on bone formation around titanium implants in diabetic rats. Dent. Res. J. 2012, 9, 582–587. [Google Scholar] [CrossRef]
- Dvorak, G.; Fügl, A.; Watzek, G.; Tangl, S.; Pokorny, P.; Gruber, R. Impact of dietary vitamin D on osseointegration in the ovariectomized rat. Clin. Oral Implants Res. 2012, 23, 1308–1313. [Google Scholar] [CrossRef]
- Kelly, J.; Lin, A.; Wang, C.J.; Park, S.; Nishimura, I. Vitamin D and bone physiology: Demonstration of vitamin D deficiency in an implant osseointegration rat model. J. Prosthodont. Implant Esthet. Reconstr. Dent. 2009, 18, 473–478. [Google Scholar] [CrossRef]
- Belluci, M.M.; Giro, G.; Del Barrio, R.A.L.; Pereira, R.M.R.; Marcantonio, E., Jr.; Orrico, S.R.P. Effects of magnesium intake deficiency on bone metabolism and bone tissue around osseointegrated implants. Clin. Oral Implants Res. 2011, 22, 716–721. [Google Scholar] [CrossRef]
- Del Barrio, R.A.; Giro, G.; Belluci, M.M.; Pereira, R.M.; Orrico, S.R. Effect of severe dietary magnesium deficiency on systemic bone density and removal torque of osseointegrated implants. Int. J. Oral Maxillofac. Implants 2010, 25, 1125–1130. [Google Scholar]
- Ribeiro, F.V.; Pimentel, S.P.; Corrêa, M.G.; Bortoli, J.P.; Messora, M.R.; Casati, M.Z. Resveratrol reverses the negative effect of smoking on peri-implant repair in the tibia of rats. Clin. Oral Implants Res. 2019, 30, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Casarin, R.C.; Casati, M.Z.; Pimentel, S.P.; Cirano, F.R.; Algayer, M.; Pires, P.R.; Ghiraldini, B.; Duarte, P.M.; Ribeiro, F.V. Resveratrol improves bone repair by modulation of bone morphogenetic proteins and osteopontin gene expression in rats. Int. J. Oral Maxillofac. Surg. 2014, 43, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, S.P.; Casarin, R.C.; Ribeiro, F.V.; Cirano, F.R.; Rovaris, K.; Haiter Neto, F.; Casati, M.Z. Impact of micronutrients supplementation on bone repair around implants: microCT and counter-torque analysis in rats. J. Appl. Oral Sci. 2016, 24, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Watanabe, T.; Nakada, H.; Sato, H.; Tanimoto, Y.; Sakae, T.; Kimoto, S.; Mijares, D.; Zhang, Y.; Kawai, Y. Improved Bone Micro Architecture Healing Time after Implant Surgery in an Ovariectomized Rat. J. Hard Tissue Biol. 2016, 25, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Nakada, H.; Takahashi, T.; Fujita, K.; Tanimoto, Y.; Sakae, T.; Kimoto, S.; Kawai, Y. Potential for acceleration of bone formation after implant surgery by using a dietary supplement: An animal study. J. Oral Rehabil. 2015, 42, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Tang, L.; Lin, Y.F.; Xie, G.F. Role of vitamin C in wound healing after dental implant surgery in patients treated with bone grafts and patients with chronic periodontitis. Clin. Implant Dent. Relat. Res. 2018, 20, 793–798. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Smoking and dental implants, a systematic review and meta-analysis. J. Dent. 2015, 43, 487–498. [Google Scholar] [CrossRef]
- Arora, M.; Schwarz, E.; Sivaneswaran, S.; Banks, E. Cigarette smoking and tooth loss in a cohort of older Australians, the 45 and Up Study. J. Am. Dent. Assoc. 2010, 141, 1242–1249. [Google Scholar] [CrossRef]
- Dietary Supplement Products & Ingredients. FDA. Available online: https://www.fda.gov/food/dietary-supplements/dietary-supplement-products-ingredients (accessed on 27 December 2019).
- DeFelice, S. The NutraCeutical Revolution: Fueling a Powerful, New International Market. Presented at the Harvard University Advanced Program in Biomedical Research Management and Development, Como, Italy; 1989. Available online: https://fimdefelice.org/library/the-nutraceutical-revolution-fueling-a-powerful-new-international-market/ (accessed on 27 December 2019).
- Zeisel, S.H. Regulation of “nutraceuticals”. Science 1999, 285, 1853–1855. [Google Scholar] [CrossRef]
- Aronson, J.K. Defining ‘nutraceuticals’: Neither nutritious nor pharmaceutical. Br. J. Clin. Pharmacol. 2017, 83, 8–19. [Google Scholar] [CrossRef]
- Fulgoni, V.L., III; Keast, D.R.; Auestad, N.; Quann, E.E. Nutrients from dairy foods are difficult to replace in diets of Americans: Food pattern modeling and an analyses of the National Health and Nutrition Examination Survey 2003–2006. Nutr. Res. 2011, 31, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Nastri, L.; Guida, L.; Annunziata, M.; Ruggiero, N.; Rizzo, A. Vitamin D modulatory effect on cytokines expression by human gingival fibroblasts and periodontal ligament cells. Minerva Stomatol. 2018, 67, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Bashutski, J.D.; Eber, R.M.; Kinney, J.S.; Benavides, E.; Maitra, S.; Braun, T.M.; Giannobile, W.V.; McCauley, L.K. The impact of vitamin D status on periodontal surgery outcomes. J. Dent. Res. 2011, 90, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Salomó-Coll, O.; Maté-Sánchez de Val, J.E.; Ramírez-Fernandez, M.P.; Hernández-Alfaro, F.; Gargallo-Albiol, J.; Calvo-Guirado, J.L. Topical applications of vitamin D on implant surface for bone-to-implant contact enhance: A pilot study in dogs part II. Clin. Oral Implants Res. 2016, 27, 896–903. [Google Scholar] [CrossRef]
- Boyera, N.; Galey, I.; Bernard, B.A. Effect of vitamin C and its derivatives on collagen synthesis and cross-linking by normal human fibroblasts. Int. J. Cosmet. Sci. 1998, 20, 151–158. [Google Scholar] [CrossRef] [PubMed]
- DePhillipo, N.N.; Aman, Z.S.; Kennedy, M.I.; Begley, J.P.; Moatshe, G.; LaPrade, R.F. Efficacy of Vitamin C Supplementation on Collagen Synthesis and Oxidative Stress After Musculoskeletal Injuries: A Systematic Review. Orthop. J. Sports Med. 2018, 6, 2325967118804544. [Google Scholar] [CrossRef]
- DiPietro, S.G.L.A. Factors affecting wound healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).