2. Materials and Methods
2.1. Design, Setting and Ethical Issues
This single-center, observational, longitudinal study was conducted for 18 months (July 2017 to December 2018) in the Neonatal Intensive Care Unit and the Nutrition Lab of Hospital Dona Estefânia, Centro Hospitalar Universitário de Lisboa Central. Institutional ethical committee approval (Nr 475/2017, dated 12th July 2018) and parental-informed consent were obtained.
2.2. Eligibility, Recruitment, Inclusion and Exclusion Criteria
Neonates subject to corrective surgery of major congenital gastrointestinal tract anomalies early after birth were eligible. Infants were recruited consecutively as soon as they were not dependent on supplemental oxygen. Only infants undergoing indirect calorimetry measurements during at least two consecutive weeks were included and followed up to discharge. Infants with associated conditions that increase metabolic rates, such as congenital heart disease complicated with a hyperdynamic circulatory state, or decrease metabolic rates, such as hypothyroidism, were excluded. The size of the convenience sample was determined by the observer’s availability (SB).
2.3. Nutritional Intake and Body Weight Records
Daily energy and macronutrient intakes by parenteral and enteral nutrition, type of feeding (fortified or non-fortified human milk, type of formula), and mode of administration (continuous or intermittent) were recorded from birth to discharge by the same investigator (SB). Following the unit protocol, if vomiting was considered excessive or daily gastric residuals were more than 50% of the intake in the previous 24 h, energy and macronutrients administered by enteral route were not took into account. Routine body weight, daily measured by nurses using scales incorporated in incubators or external automatic scales, was daily recorded.
2.4. Indirect Calorimetry Measurements
As previously described [
16], REE and RQ were assessed using the portable open-circuit continuous indirect calorimetry Deltatrac II Metabolic Monitor (Datex-Ohmeda, Instrumentarium Corp, Helsinki, Finland). Oxygen consumption (VO
2) and carbon dioxide production (VCO
2) were measured and REE calculated using the abbreviated Weir formula, REE = [3.9 (VO
2) + 1.1 (VCO
2)] 1.44 [
2,
25]. Measurements were started as soon as infants were not dependent on supplemental oxygen, scheduled twice a week (Tuesdays and Fridays), and performed by the same investigator (SB). Recommended procedures for instrument calibration and measurement technique in small infants were followed [
25,
32]. Infants were housed either in open cribs or in convective incubators with a servocontrol mechanism regulated by abdominal skin temperature at 36.4 °C to 36.5 °C [
4]. The chamber was carefully adapted to prevent air leaks. The activity of the infants was visually assigned every minute during REE measurements using a validated scale [
4,
33]. In infants receiving intermittent feeding, measurements were undertaken 1-h after bolus meal to avoid the postprandial thermogenesis effect [
34]. In infants receiving continuous tube feeding, measurements were performed with no temporal restrictions. Every REE measurement was undertaken during quiet or active sleep, or exceptionally in quiet awake status that has a slightly higher mean REE [
4]. Whenever the infant became physically active or agitated, measurements were stopped and repeated later on the same day under resting or sleeping conditions [
35]. Measurements were postponed to a subsequent day if axillary temperature was equal to or greater than 37 °C [
4]. Each measurement lasted about 40-min, including 10-min for adaptation of the infant to the environment and face chamber [
33]. For each 30-min assessment, the continuous period of 20-min of highest quality, without interference of infant movements, was recorded for subsequent analysis.
Measurements were not performed or were temporarily interrupted whenever the infant was unstable on manipulation, in acute phases of sepsis, or if any acute pathological event occurred that might have had a negative impact on the infant’s metabolic condition. Infants were removed from follow-up if they needed further major surgery, transferred to another hospital, or discharged before two-week calorimetry measurements were completed.
The difference between the estimated total energy intake on the day before the indirect calorimetry measurements and the measured REE was considered the energy balance.
2.5. Body Composition Assessment
Body composition was assessed by air displacement plethysmography using the Pea Pod equipment (Cosmed, Concord, CA, USA), which measures body mass, and estimates FM and FFM with precision of 0.1 g. Before each body composition assessment, crown-heel length was accurately measured using a standard procedure [
36]. The FMI, expressed as FM (kg)/length (m
2) [
37], was used as an indicator of adiposity. For safety reasons, weekly body composition assessments were scheduled as soon as infants were not dependent on supplemental oxygen and only after removal of central venous lines.
2.6. Statistical Analysis
An exploratory data analysis was carried out for all variables. Continuous variables not changing over time were described with mean and standard deviation (SD) or median and inter-quantile ranges (IQR) or total ranges (minimum–maximum). Additionally, LOWESS (Locally Weighted Scatterplot Smoothers) plots were used to describe the association between each continuous variable (total energy intake, protein intake, carbohydrate intake, fat intake, and body weight) and postmenstrual age (PMA). For the chronologic record of repeated measurements and calculations, the age after birth (in days), the individual PMA (in complete weeks), and time after surgery (in days) were considered.
Considering that energy and macronutrient needs differ according to the degree of an infant’s maturity [
38,
39,
40,
41], and that nutrient support influences REE and RQ [
3,
7], profiles of total energy intake, macronutrient intakes, REE, RQ, and body weight gain were analyzed separately in infants born preterm (gestational age at birth lower than 37 weeks) and at term (gestational age at birth greater than or equal to 37 weeks). Cross-sectional data for each week PMA on energy and macronutrient intake, REE, energy balance, and RQ were considered only for those PMA weeks that include at least two infants.
To study the association between these variables and the three outcomes of REE, RQ and FMI, univariable and multivariable additive mixed effects regression models were used to consider the correlation structure between measures in time and to allow the modelling of non-linear associations between the outcomes and the independent variables by using spline smoothers. For statistical analysis, weekly total energy and macronutrient intakes on the day before the indirect calorimetry measurements were considered. Crude and adjusted regression coefficients with corresponding 95% confidence intervals were estimated. The level of significance was α = 0.05.
Data analysis was performed using the software Stata (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.) and R (R: A Language and Environment for Statistical Computing, R Core Team, R Foundation for Statistical Computing, Vienna, Austria, year = 2019,
http://www.R-project.org).
3. Results
Thirty-one neonates were initially recruited but two were excluded due to associated congenital heart anomalies complicated with heart failure. Thus, 29 neonates were included for analysis. This sample included 15 infants born preterm (7 females), with a median (minimum–maximum) gestational age of 35.3 (31.4–36.7) weeks and a median birth weight of 2304 (1470–2882) g, and 14 infants born at term (4 females), with a median gestational age of 38.1 (37.1–40.6) weeks and a median birth weight of 2935 (2542–3485) g. All neonates were appropriate for gestational age. The main diagnoses were esophageal atresia (n = 13), gastroschisis (n = 7), duodenal atresia (n = 5), and annular pancreas (n = 4).
No death occurred during or close to the study period and no infant received caffeine or metabolism stimulating drugs during the period of indirect calorimetry assessment.
The individual PMA at which body weight and energy and macronutrient intakes were recorded ranged between 31 weeks gestational age at birth and 47 weeks PMA at discharge.
Indirect calorimetry (REE and RQ) was measured between 34 and 47 weeks PMA, starting at a median (IQR) of 11.8 (7–15) days after surgery. A total of 317 longitudinal indirect calorimetry measurements were performed in the entire sample, 293 (92.4%) during sleep (mostly in deep sleep) and 24 (7.6%) while quietly awake. Forty-five (14.2%) measurements were performed in infants on exclusive parenteral nutrition, 192 (60.6%) 1-h after bolus meal, and 80 (25.2%) in infants on continuous enteral feeding.
The FMI was assessed in a subset of 15 infants, who underwent a total of 22 measurements between 37 and 45 weeks PMA. Calculated FMI is presented for all infants born preterm, but at term PMA, and at term.
Variations of weekly measured total energy intake, macronutrient intake, REE, energy balance, RQ, and body weight gain are presented separately for the cohorts of infants born preterm (n = 15), from 34 to 47 weeks PMA, and those born at term (n = 14), from 38 to 47 weeks PMA.
Data on weekly energy and macronutrient intake, REE, energy balance, and RQ, obtained at 34 weeks and after 42 weeks PMA in infants born preterm, and after 44 weeks PMA in those born at term, included at most two infants and may not be representative of their cohort. Therefore, only values recorded in postmenstrual weeks including more than two infants were considered in the descriptive analysis below.
The median daily total energy intake varied between 80.7 and 109.4 Kcal/kg in infants born preterm, and between 74.0 and 105.2 Kcal/kg in infants born at term. No significant differences were found in energy intake between infants born preterm and at term. Of note, in infants born preterm, during preterm postmenstrual weeks, the median daily total energy intake had been below 91.7 Kcal/kg (
Table 1,
Figure S1A).
The median daily protein intake varied between 3.0 and 4.0 g/kg in infants born preterm, and between 1.6 to 3.2 g/kg in infants born at term. Infants born preterm had received significantly higher protein intake than those born at term (
p = 0.049) (
Table 2,
Figure S1B).
The median daily carbohydrate intake varied between 12.9 and 16.1 g/kg in infants born preterm, and between 10.1 and 15.4 g/kg in infants born at term. No significant differences were found in carbohydrate intake between infants born preterm and at term (
Table 3,
Figure S1C).
The median daily fat intake varied between 0.8 and 5.2 g/kg in infants born preterm and between 1.1 and 3.8 g/kg in infants born at term. No significant differences were found in fat intake between infants born preterm and at term (
Table 4,
Figure S1D).
The median REE varied between 55.7 and 67.4 Kcal/kg/d in infants born preterm, and between 57.3 and 67.9 Kcal/kg/d in infants born at term (
Figure 1A and
Table 5). No significant differences were found in REE either between sexes or between preterm and term infants.
The median energy balance was usually positive and varied between 16.1 and 45.6 Kcal/kg/d in infants born preterm and between 19.8 and 45.0 Kcal/kg/d in infants born at term (
Figure 1B and
Table 6). No significant differences were found in energy balance either between sexes or between infants born preterm and at term.
The median RQ had been usually below 1. The RQ increased from 0.70 at 35 weeks PMA to 0.86–0.92 between 39 and 42 weeks PMA infants born preterm, and from 0.63 at 38 weeks PMA to 0.84–0.88 between 41 and 44 weeks PMA in infants born at term (
Figure 1C and
Table 7). No significant differences were found either between sexes or between infants born preterm and at term.
Based on daily body weight measurements, the median (IQR) weight gain velocities from birth to discharge was 13.8 (10.7–34.3) g/kg/d in infants born preterm and of 6.0 (2.7–12.9) g/kg/d in infants born at term, being significantly faster in infants born preterm (p = 0.037).
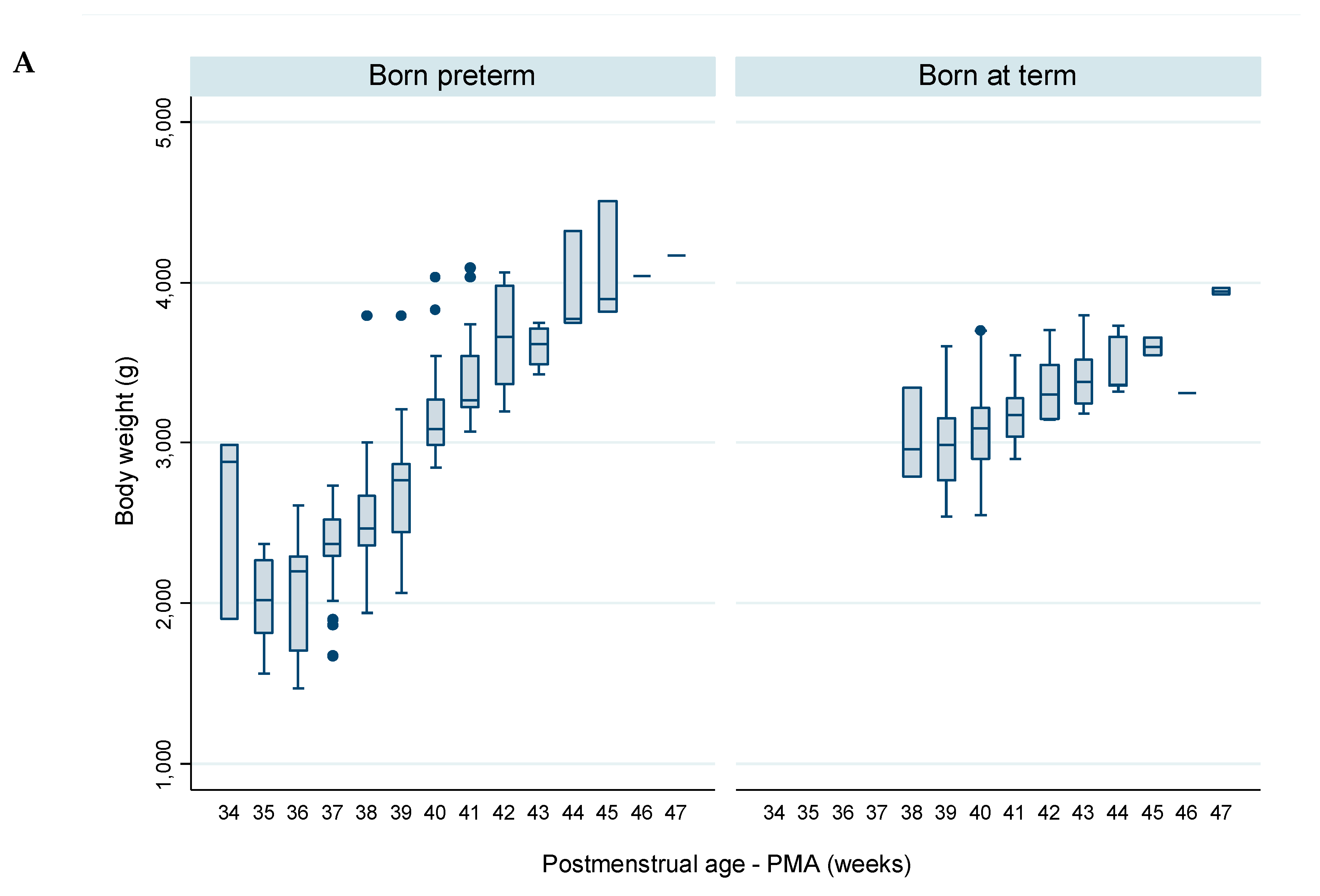
The variation of weekly body weight, measured on the same days of indirect calorimetry measurements (
Figure 2A and
Table 8), revealed that:
- -
In infants born preterm, the median body weight decreased from 2882 g at 34 weeks PMA to 2017 g at 35 weeks PMA, and subsequently a daily increase was observed, reaching 4170 g at 47 weeks PMA.
- -
In infants born at term, the median body weight increased a daily increase was observed from 2960 g at 38–39 weeks PMA, reaching 3943 g at 47 weeks PMA.
The FMI was assessed in a subset of 15 infants—8 were born preterm and 7 born at term. Following the safety criteria adopted, all infants were measured at or after term PMA. Infants born preterm and at term were analyzed together due to the homogeneity in PMA and the small dimension of the sample. A single measurement was undertaken in twelve infants and two measurements with one-week interval were undertaken in three infants (
Figure 2B and
Table 9). The median FMI increased from 1.0 kg/m
2 at 37 weeks PMA to 3.1 kg/m
2 at 45 weeks PMA.
Determinants of the Evolution of REE, RQ and Adiposity
Among all infants, preterm and term, no significant univariate associations were found between REE and sex, binary gestational age at birth (born preterm vs. born at term), PMA, weekly measured body weight, or daily total energy intake (
Table S1); therefore, no multivariate model was explored for REE as a dependent variable.
Models for determinants of RQ were explored. From univariate analysis (
Table S2), PMA, body weight, daily carbohydrate intake, and REE were selected for multivariate analysis, but only PMA, daily carbohydrate intake and REE remained significant in the final model. Accordingly, for each week increase in PMA, there was a mean increase of 0.013 (95% CI: 0.007 to 0.019) in RQ (
p < 0.001) for infants with the same levels of carbohydrate intake and REE. For each 1 g/kg increase in carbohydrate intake, there was a mean increase of 0.009 (95% CI: 0.004 to 0.014) in RQ (
p < 0.001) for infants with the same PMA and REE. For each Kcal/kg increase in REE there was a mean decrease of 0.006 (95% CI: −0.007 to −0.005) in RQ (
p < 0.001) for infants with the same PMA and carbohydrate intake level.
Univariate associations with FMI variation were explored (
Table S3). Postmenstrual age, weekly body weight, daily total energy intake, and carbohydrate and fat intakes were identified as candidates for multivariable analysis. Only PMA and daily carbohydrate and fat intakes remained significant in the final multivariate model. Accordingly, a mean increase in FMI of 0.32 kg/m
2 (95% CI: 0.23 to 0.41;
p < 0.001) for each additional week of PMA was estimated. A mean decrease in FMI of 0.21 g/m
2 (95% CI: −3.74 to −0.52;
p = 0.009) was observed for each additional g/kg in daily carbohydrate intake. A mean increase in FMI of 0.40 g/m
2 (95% CI: 0.06 to 0.74;
p = 0.022) was observed for each additional g/kg in daily fat intake.
5. Conclusions
This cohort study describes the evolution of REE and RQ in infants growing during the late anabolic phase, after corrective surgery of major congenital gastrointestinal tract anomalies. In infants born preterm, the median REE varied between 55.7 and 67.4 Kcal/kg/d and the median RQ increased from 0.70 to 0.86–0.92, from 34 to 42 weeks PMA. In those born at term, the median REE varied between 57.3 and 67.9 Kcal/kg/d and the median RQ increased from 0.63 to 0.84–0.88, from 38 to 44 weeks PMA. Despite some deficit in energy, continuous body weight gain was recorded, with satisfactory weight gain velocity in infants born preterm, but slower than reported for healthy infants in those born at term. Adiposity was measured at late PMA in approximately in half of the infants studied. At term PMA, the median FMI was between 1.7 and 1.8 kg/m2, lower than reported in non-surgical infants. This low adiposity is consistent with several study periods in which low intake of energy was observed, during which there was increased fat oxidation as indicated by the low RQ.
Data from this study indicate that after the early phase of corrective surgery of major congenital gastrointestinal tract anomalies, higher energy and fat intakes are needed to cover energy cost of growth and reduce fat oxidation, thus preventing lipolysis and promoting lipogenesis, particularly in term infants. Further studies are needed to confirm these results and improve the nutritional approach in this population.