Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey Questionnaire
2.2.1. Dietary Assessment
2.2.2. Physical Activity Assessment
2.2.3. Stress, Irritability and Sleep Assessment
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Source of Information
3.3. Eating Habits
3.4. Shopping
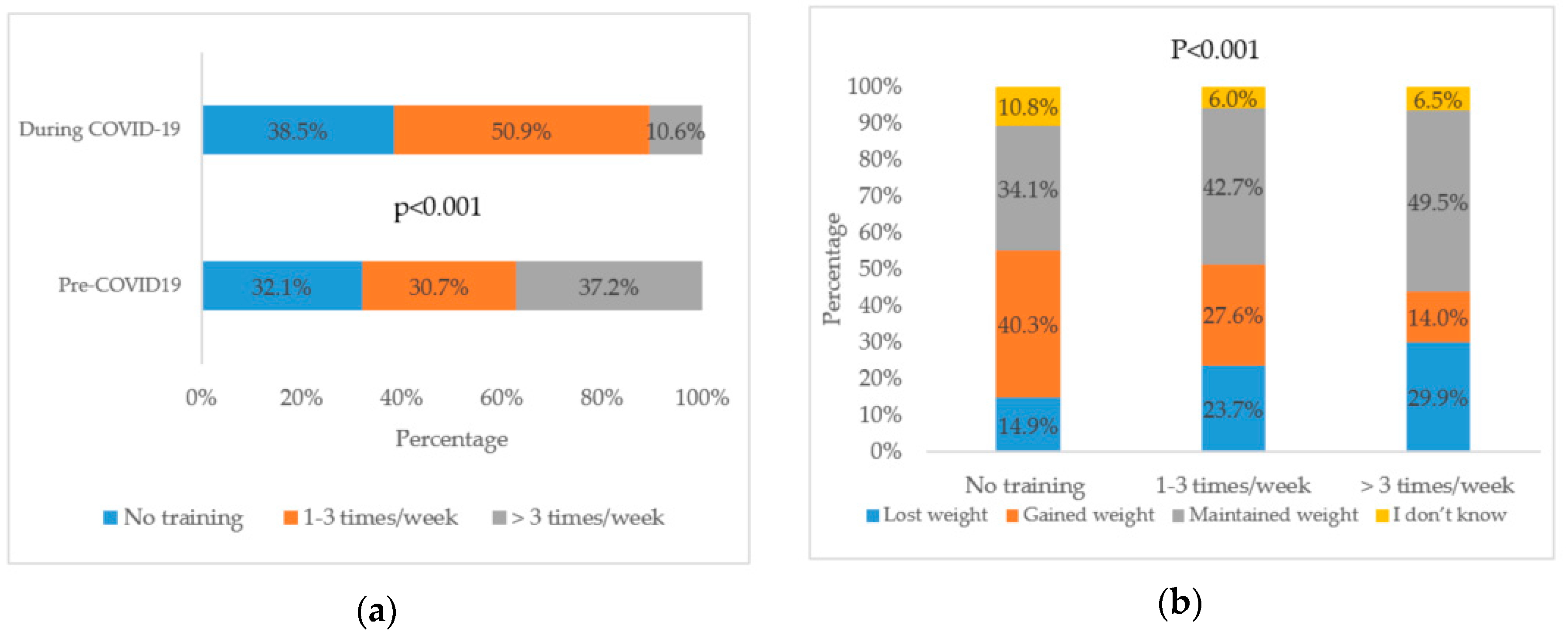
3.5. Physical Activity
3.6. Stress
3.7. Sleep
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Barro, R.J.; Ursúa, J.F.; Weng, J. The Coronavirus and the Great Influenza Pandemic: Lessons from the “Spanish flu” for the Coronavirus’s Potential Effects on Mortality and Economic Activity; 0898-2937; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 16 August 2020).
- WHO. Coronavirus Disease (COVID-19) Weekly Epidemiological and Operational Updates September 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200928-weekly-epi-update.pdf?sfvrsn=9e354665_6 (accessed on 29 September 2020).
- Wilder-Smith, A.; Freedman, D. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020, 27, taaa020. [Google Scholar] [CrossRef] [PubMed]
- Koh, D. COVID-19 lockdowns throughout the world. Occup. Med. 2020. [Google Scholar] [CrossRef]
- Bloukh, S.H.; Shaikh, A.; Pathan, H.M.; Edis, Z. Prevalence of COVID-19: A Look behind the Scenes from the UAE and India. Preprints 2020. [Google Scholar] [CrossRef]
- Bank, T.W. United Arab Emirates: Data Source: United Nations World Population Prospects. Available online: https://data.worldbank.org/country/AE (accessed on 16 August 2020).
- De Bel-Air, F. Demography, Migration, and the Labour Market in the UAE; Migration Policy Center, Gulf Labour Markets and Migration (GLMM): Firenze, Italy, 2015. [Google Scholar]
- Scarmozzino, F.; Visioli, F. Covid-19 and the Subsequent Lockdown Modified Dietary Habits of Almost Half the Population in an Italian Sample. Foods 2020, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; Szabo de Edelenyi, F.; Alles, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the COVID-19 lockdown period (March-May 2020): Results from the French NutriNet-Sante cohort study. medRxiv 2020. [Google Scholar] [CrossRef]
- Calder, P.C. Nutrition, immunity and COVID-19. BMJ Nutr. Prev. Health 2020, 3, 74. [Google Scholar] [CrossRef]
- Zachary, Z.; Brianna, F.; Brianna, L.; Garrett, P.; Jade, W.; Alyssa, D.; Mikayla, K. Self-quarantine and Weight Gain Related Risk Factors During the COVID-19 Pandemic. Obes. Res. Clin. Pract. 2020. [Google Scholar] [CrossRef]
- Musaiger, A.O. Diet and Prevention of Coronary Heart Disease in the Arab Middle East Countries. Med. Princ. Pract. 2002, 11, 9–16. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Lippi, G.; Henry, B.M.; Sanchis-Gomar, F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Yammine, K. The prevalence of physical activity among the young population of UAE: A meta-analysis. Perspect. Public Health 2017, 137, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Todisco, P.; Donini, L.M. Eating disorders and obesity (ED&O) in the COVID-19 storm. Eat. Weight Disord. 2020, 1. [Google Scholar] [CrossRef]
- Touyz, S.; Lacey, H.; Hay, P. Eating disorders in the time of COVID-19. J. Eat. Disord. 2020, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020. [Google Scholar] [CrossRef]
- Ng, S.W.; Zaghloul, S.; Ali, H.; Harrison, G.; Yeatts, K.; El Sadig, M.; Popkin, B.M. Nutrition transition in the United Arab Emirates. Eur. J. Clin. Nutr. 2011, 65, 1328–1337. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Pejtersen, J.H.; Kristensen, T.S.; Borg, V.; Bjorner, J.B. The second version of the Copenhagen Psychosocial Questionnaire. Scand. J. Public Health 2010, 38, 8–24. [Google Scholar] [CrossRef]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Osler, M.; Heitmann, B.L. The Validity of a Short Food Frequency Questionnaire and its Ability to Measure Changes in Food Intake: A Longitudinal Study. Int. J. Epidemiol. 1996, 25, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.; Al-Alami, U. Food consumption patterns of female undergraduate students in the United Arab Emirates. West Afr. J. Med. 2011, 30, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.O.; Abuirmeileh, N.M. Food consumption patterns of adults in the United Arab Emirates. J. R. Soc. Promot. Health 1998, 118, 146–150. [Google Scholar] [CrossRef]
- Streiner, D.L. Starting at the Beginning: An Introduction to Coefficient Alpha and Internal Consistency. J. Personal. Assess. 2003, 80, 99–103. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef]
- Bhutani, S.; Cooper, J.A. COVID-19 related home confinement in adults: Weight gain risks and opportunities. Obesity 2020. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Husain, W.; Ashkanani, F. Does COVID-19 Change Dietary Habits and Lifestyle Behaviours in Kuwait? Environ. Health Prev. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- ALMughamis, N.S.; AlAsfour, S.; Mehmood, S. Poor Eating Habits and Predictors of Weight Gain During the COVID-19 Quarantine Measures in Kuwait: A Cross Sectional Study. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Moynihan, A.B.; Van Tilburg, W.A.; Igou, E.R.; Wisman, A.; Donnelly, A.E.; Mulcaire, J.B. Eaten up by boredom: Consuming food to escape awareness of the bored self. Front. Psychol. 2015, 6, 369. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.; Rebar, A.L. Habit Formation and Behavior Change. In Oxford Research Encyclopedia of Psychology; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Mattioli, A.V.; Puviani, M.B.; Nasi, M.; Farinetti, A. COVID-19 pandemic: The effects of quarantine on cardiovascular risk. Eur. J. Clin. Nutr. 2020. [Google Scholar] [CrossRef]
- Sulaiman, N.; Elbadawi, S.; Hussein, A.; Abusnana, S.; Madani, A.; Mairghani, M.; Alawadi, F.; Sulaiman, A.; Zimmet, P.; Huse, O. Prevalence of overweight and obesity in United Arab Emirates Expatriates: The UAE national diabetes and lifestyle study. Diabetol. Metab. Syndr. 2017, 9, 88. [Google Scholar] [CrossRef]
- Razzak, H.A.; El-Metwally, A.; Harbi, A.; Al-Shujairi, A.; Qawas, A. The prevalence and risk factors of obesity in the United Arab Emirates. Saudi J. Obes. 2017, 5, 57. [Google Scholar] [CrossRef]
- Belal, A.M. Nutrition-related chronic diseases Epidemic in UAE: Can we stand to STOP it? Sudan. J. Public Health 2009, 4, 383–392. [Google Scholar]
- Makansi, N.; Allison, P.; Awad, M.; Bedos, C. Fruit and vegetable intake among Emirati adolescents: A mixed methods study. East. Mediterr. Health J. 2018, 24. [Google Scholar] [CrossRef]
- Díez, J.; Bilal, U.; Franco, M. Unique features of the Mediterranean food environment: Implications for the prevention of chronic diseases Rh: Mediterranean food environments. Eur. J. Clin. Nutr. 2019, 72, 71–75. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean diet and cardiovascular health: A critical review. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Becerra-Tomás, N.; Blanco Mejía, S.; Viguiliouk, E.; Khan, T.; Kendall, C.W.; Kahleova, H.; Rahelić, D.; Sievenpiper, J.L.; Salas-Salvadó, J. Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 1207–1227. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Zappala, G.; Bernardini, S.; Giambini, I.; Bes-Rastrollo, M.; Martinez-Gonzalez, M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: A meta-analysis of observational studies. Int. J. Food Sci. Nutr. 2017, 68, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Germani, A.; Vitiello, V.; Giusti, A.M.; Pinto, A.; Donini, L.M.; del Balzo, V. Environmental and economic sustainability of the Mediterranean Diet. Int. J. Food Sci. Nutr. 2014, 65, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.; Esposito, K. Mediterranean diet and metabolic diseases. Curr. Opin. Lipidol. 2008, 19, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Hassapidou, M.; Tziomalos, K.; Lazaridou, S.; Pagkalos, I.; Papadimitriou, K.; Kokkinopoulou, A.; Tzotzas, T. The Nutrition Health Alliance (NutriHeAl) Study: A Randomized, Controlled, Nutritional Intervention Based on Mediterranean Diet in Greek Municipalities. J. Am. Coll. Nutr. 2020, 39, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Villegas, A.; Bes-Rastrollo, M.; Martínez-González, M.A.; Serra-Majem, L. Adherence to a Mediterranean dietary pattern and weight gain in a follow-up study: The SUN cohort. Int. J. Obes. 2006, 30, 350–358. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Roman-Vinas, B.; Sanchez-Villegas, A.; Guasch-Ferre, M.; Corella, D.; La Vecchia, C. Benefits of the Mediterranean diet: Epidemiological and molecular aspects. Mol. Asp. Med. 2019, 67, 1–55. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Salas-Salvadó, J.; Estruch, R.; Corella, D.; Fitó, M.; Ros, E. Benefits of the Mediterranean Diet: Insights From the PREDIMED Study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Sarrafzadegan, N.; Fadhil, I.; Taubert, K.; Sadeghi, M.; Wenger, N.K.; Tan, N.S.; Grace, S.L. Cardiovascular disease in the Eastern Mediterranean region: Epidemiology and risk factor burden. Nat. Rev. Cardiol. 2018, 15, 106–119. [Google Scholar] [CrossRef]
- Mahmoud, I.; Sulaiman, N. Dyslipidaemia prevalence and associated risk factors in the United Arab Emirates: A population-based study. BMJ Open 2019, 9, e031969. [Google Scholar] [CrossRef]
- Taha, Z.; Eltom, S.E. The Role of Diet and Lifestyle in Women with Breast Cancer: An Update Review of Related Research in the Middle East. Biores. Open Access 2018, 7, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.O.; Al-Hazzaa, H.M. Prevalence and risk factors associated with nutrition-related noncommunicable diseases in the Eastern Mediterranean region. Int. J. Gen. Med. 2012, 5, 199–217. [Google Scholar] [CrossRef]
- Galal, O. Nutrition-related health patterns in the Middle East. Asia Pac. J. Clin. Nutr. 2003, 12, 337–343. [Google Scholar]
- Gombart, A.F.; Pierre, A.; Maggini, S. A review of micronutrients and the immune System–Working in harmony to reduce the risk of infection. Nutrients 2020, 12, 236. [Google Scholar] [CrossRef] [PubMed]
- Ipsos. 5 Ways COVID-19 Has Impacted MENA’s Food Habits. Available online: https://www.ipsos.com/sites/default/files/ct/news/documents/2020-06/5_ways_covid-19_impacted_menas_food_habits_-_ipsos_mena_0.pdf (accessed on 16 August 2020).
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M. Effects of COVID-19 home confinement on physical activity and eating behaviour Preliminary results of the ECLB-COVID19 international online-survey. medRxiv 2020. [Google Scholar] [CrossRef]
- Abbas, A.M.; Fathy, S.K.; Fawzy, A.T.; Salem, A.S.; Shawky, M.S. The mutual effects of COVID-19 and obesity. Obes. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, J.; Burtscher, M.; Millet, G.P. (Indoor) isolation, stress and physical inactivity: Vicious circles accelerated by Covid-19? Scand. J. Med. Sci. Sports 2020. [Google Scholar] [CrossRef]
- Jiménez-Pavón, D.; Carbonell-Baeza, A.; Lavie, C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog. Cardiovasc. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Czosnek, L.; Lederman, O.; Cormie, P.; Zopf, E.; Stubbs, B.; Rosenbaum, S. Health benefits, safety and cost of physical activity interventions for mental health conditions: A meta-review to inform translation efforts. Ment. Health Phys. Act. 2019, 16, 140–151. [Google Scholar] [CrossRef]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Zandifar, A.; Badrfam, R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatry 2020, 51. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Schmidt, A.L.; Zola, P.; Zollo, F.; Scala, A. The covid-19 social media infodemic. arXiv 2020, arXiv:2003.05004. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e923549. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef]
- Salvatore, F.P.; Relja, A.; Filipčić, I.Š.; Polašek, O.; Kolčić, I. Mediterranean diet and mental distress:“10,001 Dalmatians” study. Br. Food J. 2019, 121, 1314–1326. [Google Scholar] [CrossRef]
- Godos, J.; Ferri, R.; Caraci, F.; Cosentino, F.I.I.; Castellano, S.; Galvano, F.; Grosso, G. Adherence to the mediterranean diet is associated with better sleep quality in Italian adults. Nutrients 2019, 11, 976. [Google Scholar] [CrossRef]
- Muñoz, M.A.; Fíto, M.; Marrugat, J.; Covas, M.I.; Schröder, H. Adherence to the Mediterranean diet is associated with better mental and physical health. Br. J. Nutr. 2008, 101, 1821–1827. [Google Scholar] [CrossRef]
- Smith, G. Does Gender Influence Online Survey Participation: A Record-Linkage Analysis of University Faculty Online Survey Response Behavior; ERIC Document Reproduction Service No. ED 501717; San Jose State University, ScholarWorks: San Jose, CA, USA, 2008. [Google Scholar]

| Characteristics | n | % |
|---|---|---|
| Gender | ||
| Male | 244 | 24.1 |
| Female | 768 | 75.9 |
| Age (years) | ||
| 18–25 | 280 | 27.7 |
| 26–35 | 294 | 29.1 |
| 36–45 | 240 | 23.7 |
| 46–55 | 154 | 15.2 |
| >55 | 44 | 4.3 |
| Marital status | ||
| Married | 571 | 56.4 |
| Single | 403 | 39.8 |
| Divorced | 30 | 3.0 |
| Widowed | 8 | 0.8 |
| Number of children | ||
| None | 506 | 50.0 |
| 1–2 | 230 | 22.7 |
| ≥ 3 | 276 | 27.3 |
| Education level | ||
| Less than high school | 8 | 0.8 |
| High school | 111 | 11.0 |
| College/Diploma | 102 | 10.1 |
| Bachelor’s degree | 547 | 54.1 |
| Higher than bachelor’s degree | 244 | 24.1 |
| Employment status | ||
| Full-time | 539 | 53.3 |
| Part-time | 44 | 4.3 |
| Self-employed | 31 | 3.1 |
| Student | 156 | 15.4 |
| Unemployed | 230 | 22.7 |
| Retired | 12 | 1.2 |
| Working/studying from home | ||
| Yes | 623 | 61.6 |
| No | 309 | 30.5 |
| Not applicable | 80 | 7.9 |
| Weight change during pandemic | ||
| Lost weight | 212 | 20.9 |
| Gained weight | 314 | 31.0 |
| Maintained weight | 406 | 40.1 |
| Do not know | 80 | 7.9 |
| Perceived health state during pandemic | ||
| Excellent | 217 | 21.4 |
| Very good | 402 | 39.7 |
| Good | 284 | 28.1 |
| Fair | 102 | 10.1 |
| Poor | 7 | 0.7 |
| Emirate of residence | ||
| Abu Dhabi | 343 | 33.9 |
| Dubai | 329 | 32.5 |
| Sharjah | 244 | 24.1 |
| Ajman | 52 | 5.1 |
| Ras al Khaimah | 20 | 2.0 |
| Fujairah | 16 | 1.6 |
| Umm al Quwain | 8 | 0.8 |
| Source of Information * | Health-Related Information, n (%) | Nutrition-Related Information, n (%) |
|---|---|---|
| Local and international health authorities | 662 (65.4) | 493 (48.7) |
| Social media | 699 (69.1) | 686 (67.8) |
| Healthcare professionals | 409 (40.4) | 462 (45.7) |
| Television | 231 (22.8) | 172 (17.0) |
| Newspapers | 75 (7.4) | 51 (5.0) |
| Friends and family | 339 (33.5) | 386 (38.1) |
| Variables | Pre-COVID-19 n (%) | During COVID-19 n (%) | p-Value (2-Sided) |
|---|---|---|---|
| Most consumed meals during the week * | |||
| Homemade | 838 (82.8) | 974 (96.2) | <0.001 |
| Frozen ready-to-eat meals | 119 (11.8) | 97 (9.6) | 0.032 |
| Fast food | 270 (26.7) | 80 (7.9) | <0.001 |
| Restaurants 1 | 289 (28.6) | 58 (5.7) | <0.001 |
| Healthy restaurants 2 | 98 (9.7) | 46 (4.5) | <0.001 |
| Number of meals per day | |||
| 1–2 meals | 470 (46.4) | 369 (36.5) | <0.001 |
| 3–4 meals | 521 (51.5) | 572 (56.5) | 0.009 |
| ≥5 meals | 21 (2.1) | 71 (7.0) | <0.001 |
| Eating breakfast on most days | |||
| Yes | 668 (66.0) | 751 (74.2) | <0.001 |
| No | 344 (34.0) | 261 (25.8) | |
| Skipping meals | |||
| Yes | 663 (65.5) | 468 (46.2) | <0.001 |
| No | 349 (34.5) | 544 (53.8) | |
| Reasons for skipping meals (If the answer was yes) * | |||
| To reduce food intake | 143 (21.7) | 136 (29.1) | 0.011 |
| Lack of time | 410 (62.3) | 143 (30.6) | <0.001 |
| To lose weight | 122 (18.5) | 110 (23.6) | 0.001 |
| Lack of appetite | 182 (27.7) | 168 (36.0) | 0.016 |
| Fasting | 68 (10.3) | 120 (25.7) | <0.001 |
| Amount of water consumed per day | |||
| 1–4 cups | 410 (40.5) | 337 (33.3) | <0.001 |
| 5–7 cups | 358 (35.4) | 394 (38.9) | 0.036 |
| ≥8 cups | 244 (24.1) | 281 (27.8) | 0.003 |
| Food Items | ≥4 Times/Day | 2–3 Times/Day | Once/Day | 1–4 Times/Week | Never |
|---|---|---|---|---|---|
| n (%) | |||||
| Fruits | 20 (2.0) | 133 (13.1) | 341 (33.7) | 462 (45.7) | 56 (5.5) |
| Vegetables | 32 (3.2) | 244 (24.1) | 362 (35.8) | 356 (35.2) | 18 (1.8) |
| Milk and milk products | 17 (1.7) | 167 (16.5) | 361 (35.7) | 374 (37.0) | 93 (9.2) |
| Meat/fish/chicken | 32 (3.2) | 133 (13.1) | 440 (43.5) | 383 (37.8) | 24 (2.4) |
| Bread/rice/pasta | 43 (4.2) | 263 (26.0) | 350 (34.6) | 311 (30.7) | 45 (4.4) |
| Sweets/desserts | 29 (2.9) | 106 (10.5) | 331 (32.7) | 437 (43.2) | 109 (10.8) |
| Salty snacks | 14 (1.4) | 85 (8.4) | 276 (27.3) | 500 (49.4) | 137 (13.5) |
| Coffee/tea | 80 (7.9) | 321 (31.7) | 300 (29.6) | 222 (21.9) | 89 (8.8) |
| Sweetened drinks | 18 (1.8) | 51 (5.0) | 156 (15.4) | 340 (33.6) | 447 (44.2) |
| Energy drinks | 4 (0.4) | 11 (1.1) | 35 (3.5) | 87 (8.6) | 875 (86.5) |
| Food Groups | Western | Free Sugars |
|---|---|---|
| Fruits | 0.2839 | −0.3807 |
| Vegetable | 0.3302 | −0.4219 |
| Milk | 0.3247 | −0.1932 |
| Meat | 0.3599 | −0.0732 |
| Carbs | 0.3975 | −0.0764 |
| Sweets | 0.3845 | 0.2917 |
| Salted Foods | 0.3356 | 0.2776 |
| Coffee/Tea | 0.2457 | −0.1641 |
| Sweet Drinks | 0.2678 | 0.4929 |
| Energy Drinks | 0.1575 | 0.4433 |
| KMO | 0.78 |
| Variables | n | % |
|---|---|---|
| Prepare shopping list | ||
| Yes | 813 | 80.3 |
| No | 199 | 19.7 |
| Start stocking up on foods | ||
| Yes | 444 | 43.9 |
| No | 412 | 40.7 |
| Already stocking up | 156 | 15.4 |
| Online grocery shopping | ||
| Yes | 425 | 42.0 |
| No | 587 | 58.0 |
| Reading food labels | ||
| Yes | 530 | 52.4 |
| No | 113 | 11.2 |
| Sometimes | 369 | 36.5 |
| Sanitizing/cleaning groceries | ||
| Yes | 728 | 71.9 |
| No | 113 | 11.2 |
| Sometimes | 171 | 16.9 |
| Variables | Pre-COVID-19 n (%) | During COVID-19 n (%) | p-Value (2-Sided) |
|---|---|---|---|
| Doing household chores | |||
| Never | 302 (29.8) | 207 (20.5) | <0.001 |
| 1–3 times/week | 404 (39.8) | 333 (32.9) | <0.001 |
| 4–5 times/week | 62 (6.1) | 114 (11.3) | <0.001 |
| Everyday | 244 (24.1) | 358 (35.4) | <0.001 |
| Screen time for study or work | |||
| None | 188 (18.6) | 160 (15.8) | 0.004 |
| 1–2 h/day | 282 (27.9) | 136 (13.4) | <0.001 |
| 3–5 h/day | 218 (21.5) | 234 (23.1) | 0.375 |
| >5 h/day | 324 (32.0) | 482 (47.6) | <0.001 |
| Screen time for entertainment | |||
| Less than 30 min/day | 113 (11.2) | 62 (6.1) | <0.001 |
| 1–2 h/day | 456 (45.1) | 231 (22.8) | <0.001 |
| 3–5 h/day | 312 (30.8) | 353 (34.9) | 0.053 |
| >5 h/day | 131 (12.9) | 366 (36.2) | <0.001 |
| Variables | Pre-COVID-19 n (%) | During COVID-19 n (%) | p-Value (2-Sided) |
|---|---|---|---|
| Hours of sleep per night | |||
| <7 h | 523 (51.7) | 395 (39.0) | <0.001 |
| 7–9 h | 459 (45.4) | 499 (49.3) | 0.057 |
| >9 h | 30 (3.0) | 118 (11.7) | <0.001 |
| How would you rate your sleep quality | |||
| Very good | 308 (30.4) | 282 (27.9) | 0.134 |
| Good | 529 (52.3) | 446 (44.1) | <0.001 |
| Poor | 175 (17.3) | 284 (28.1) | <0.001 |
| Did you experience any of the following * | |||
| Slept badly and restlessly | 251 (24.8) | 285 (28.2) | 0.057 |
| Hard to go to sleep | 199 (19.7) | 358 (35.4) | <0.001 |
| Woken up too early and not been able to get back to sleep | 232 (22.9) | 147 (14.5) | <0.001 |
| Woken up several times and found it difficult to get back to sleep | 187 (18.5) | 334 (33.0) | <0.001 |
| None | 477 (47.1) | 397 (39.2) | <0.001 |
| Describe your energy level | |||
| Energized | 369 (36.5) | 189 (18.7) | <0.001 |
| Neutral | 596 (58.9) | 510 (50.4) | <0.001 |
| Lazy | 47 (4.7) | 313 (30.9) | <0.001 |
| Variables | All n = 1012 | Gender | Age Group (Year) | Education Level | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female n = 768 | Male n = 244 | p Value | 18–35 n = 574 | ≥36 n = 438 | p Value | High School n = 119 | Higher Degree n = 893 | p Value | ||
| Weight, n, (%) | ||||||||||
| Decreased | 212 (20.9) | 166 (21.6) | 46 (18.9) | 0.143 | 131 (22.8) | 81 (18.5) | 0.042 | 19 (16.0) | 193 (21.6) | 0.350 |
| Same as before | 486 (48.0) | 376 (49.0) | 110 (45.1) | 273 (47.6) | 213 (48.6) | 62 (52.1) | 424 (47.5) | |||
| Increased | 314 (31.0) | 226 (29.4) | 88 (36.1) | 170 (29.6) | 144 (32.9) | 38 (31.9) | 276 (30.9) | |||
| Meals per day, n (%) | ||||||||||
| Decreased | 124 (12.3) | 96 (12.5) | 28 (11.5) | 0.140 | 84 (14.6) | 40 (9.1) | 0.024 | 13 (10.9) | 111 (12.4) | 0.352 |
| Same as before | 628 (62.1) | 464 (60.4) | 164 (67.2) | 342 (59.6) | 272 (61.9) | 69 (58.0) | 559 (62.6) | |||
| Increased | 260 (25.7) | 208 (27.1) | 52 (21.3) | 148 (25.8) | 127 (29.0) | 37 (31.1) | 223 (25.0) | |||
| Physical activity, n (%) | ||||||||||
| Decreased | 424 (41.9) | 302 (39.3) | 122 (50.0) | 0.013 | 226 (39.4) | 198 (45.2) | 0.171 | 42 (35.3) | 382 (42.8) | 0.169 |
| Same as before | 438 (43.3) | 346 (45.1) | 92 (37.7) | 258 (44.9) | 180 (41.1) | 61 (51.3) | 377 (42.2) | |||
| Increased | 150 (14.8) | 120 (15.6) | 30 (12.3) | 90 (15.7) | 60 (13.7) | 16 (13.4) | 134 (15.0) | |||
| Screen time (entertainment), n (%) | ||||||||||
| Decreased | 72 (7.1) | 67 (8.7) | 5 (2.0) | 0.002 | 46 (8.0) | 26 (5.9) | 0.150 | 8 (6.7) | 64 (7.2) | 0.984 |
| Same as before | 415 (41.0) | 309 (40.2) | 106 (43.4) | 222 (38.7) | 193 (44.1) | 49 (41.2) | 366 (41.0) | |||
| Increased | 525 (51.9) | 392 (51.0) | 133 (54.5) | 306 (53.3) | 219 (50.0) | 62 (52.1) | 463 (51.8) | |||
| Sleep (h), n (%) | ||||||||||
| Decreased | 148 (14.6) | 124 (16.1) | 24 (9.8) | 0.051 | 100 (17.4) | 48 (11.0) | <0.001 | 23 (19.3) | 125 (14.0) | 0.302 |
| Same as before | 534 (52.8) | 397 (51.7) | 137 (56.1) | 270 (47.0) | 264 (60.3) | 59 (49.6) | 475 (53.2) | |||
| Increased | 330 (32.6) | 247 (32.2) | 83 (34.0) | 204 (35.5) | 126 (28.8) | 37 (31.1) | 293 (32.8) | |||
| Sleep disturbances, n (%) | ||||||||||
| Decreased | 157 (15.5) | 119 (15.5) | 38 (15.6) | 0.011 | 90 (15.7) | 67 (15.3) | <0.001 | 16 (13.4) | 141 (15.8) | 0.135 |
| Same as before | 552 (54.5) | 401 (52.2) | 151 (61.9) | 285 (49.7) | 267 (61.0) | 58 (48.7) | 494 (55.3) | |||
| Increased | 303 (29.9) | 248 (32.3) | 55 (22.5) | 199 (34.7) | 104 (23.7) | 45 (37.8) | 258 (28.9) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Magriplis, E.; Ali, H.I.; Al Sabbah, H.; Hasan, H.; et al. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients 2020, 12, 3314. https://doi.org/10.3390/nu12113314
Cheikh Ismail L, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Abu Jamous DO, Magriplis E, Ali HI, Al Sabbah H, Hasan H, et al. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients. 2020; 12(11):3314. https://doi.org/10.3390/nu12113314
Chicago/Turabian StyleCheikh Ismail, Leila, Tareq M. Osaili, Maysm N. Mohamad, Amina Al Marzouqi, Amjad H. Jarrar, Dima O. Abu Jamous, Emmanuella Magriplis, Habiba I. Ali, Haleama Al Sabbah, Hayder Hasan, and et al. 2020. "Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study" Nutrients 12, no. 11: 3314. https://doi.org/10.3390/nu12113314
APA StyleCheikh Ismail, L., Osaili, T. M., Mohamad, M. N., Al Marzouqi, A., Jarrar, A. H., Abu Jamous, D. O., Magriplis, E., Ali, H. I., Al Sabbah, H., Hasan, H., AlMarzooqi, L. M. R., Stojanovska, L., Hashim, M., Shaker Obaid, R. R., Saleh, S. T., & Al Dhaheri, A. S. (2020). Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients, 12(11), 3314. https://doi.org/10.3390/nu12113314













