Factors Associated with Stunting among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
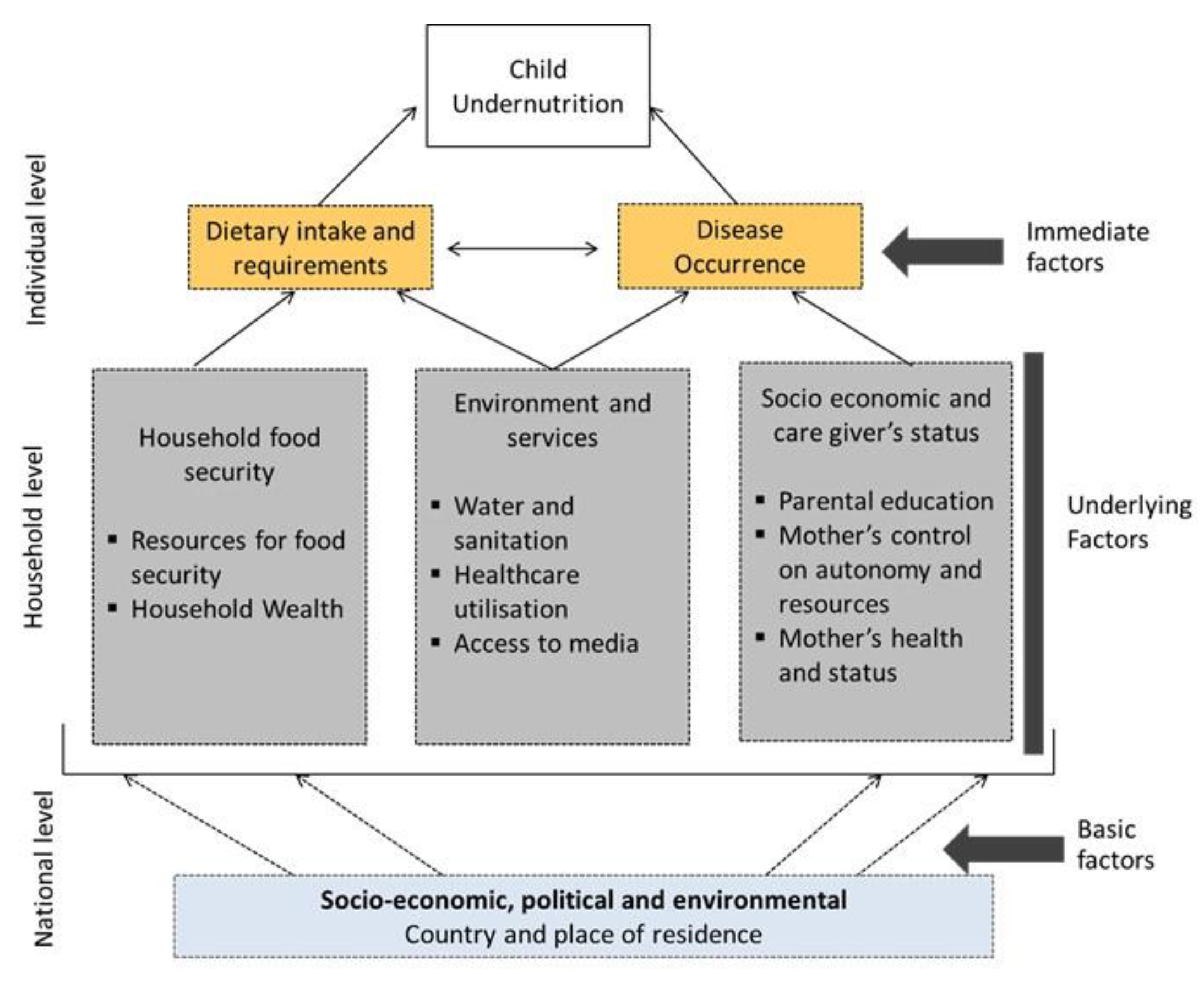
2.2. Study Variables
2.3. Potential Confounding Factors
2.4. Statistical Analysis
3. Results
3.1. Prevalence of Stunting in Children Aged 0–23 Months, 24–59 Months and 0–59 Months
3.2. Factors Associated with Child Stunting for Children Aged 0–23 Months
3.3. Factors Associated with Child Stunting for Children Aged 24–59 Months
3.4. Factors Associated with Child Stunting for Children Aged 0–59 Months
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations International Children’s Fund; World Health Organization; The World Bank. Joint Child Malnutrition Estimates-Levels and Trends; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Local Burden of Disease Child Growth Failure Collaborators. Mapping child growth failure across low- and middle-income countries. Nature 2020, 577, 231–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations Children Fund. Stop Stunting. Available online: http://www.unicefrosa-progressreport.org/stopstunting.html (accessed on 15 September 2020).
- De Onis, M.; Borghi, E.; Arimond, M.; Webb, P.; Croft, T.; Saha, K.; De-Regil, L.M.; Thuita, F.; Heidkamp, R.; Krasevec, J.; et al. Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Health Nutr. 2019, 22, 175–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, L.C.; Haddad, L. Reducing Child Undernutrition: Past Drivers and Priorities for the Post-MDG Era. World Dev. 2015, 68, 180–204. [Google Scholar] [CrossRef] [Green Version]
- Walker, S.; Chang, S.; Powell, C.; Simonoff, E.; Grantham-Mcgregor, S. Early Childhood Stunting Is Associated with Poor Psychological Functioning in Late Adolescence and Effects Are Reduced by Psychosocial Stimulation1,2. J. Nutr. 2007, 137, 2464–2469. [Google Scholar] [CrossRef] [PubMed]
- International Food and Policy Research Institute. Global Nutrition Report 2015: Actions and Accountability to Advance Nutrition and Sustainable Development; IFPRI: Washington, DC, USA, 2015. [Google Scholar]
- Ranjani, H.; Mehreen, T.; Pradeepa, R.; Anjana, R.; Garg, R.; Anand, K.; Mohan, V. Epidemiology of childhood overweight & obesity in India: A systematic review.(Systematic Review)(Report). Indian J. Med. Res. 2016, 143, 160. [Google Scholar] [CrossRef] [Green Version]
- United Nations International Children’s Fund. Multi-Sectoral Approaches to Nutrition: Nutrition-Specific and Nutrition-Sensitive Interventions to Accelerate Progress; UNICEF: New York, NY, USA, 2014. [Google Scholar]
- Headey, D.; Hoddinott, J.; Ali, D.; Tesfaye, R.; Dereje, M. The Other Asian Enigma: Explaining the Rapid Reduction of Undernutrition in Bangladesh. World Dev. 2015, 66, 749–761. [Google Scholar] [CrossRef] [Green Version]
- Rahman, M.S.; Howlader, T.; Masud, M.S.; Rahman, M.L. Association of Low-Birth Weight with Malnutrition in Children under Five Years in Bangladesh: Do Mother’s Education, Socio-Economic Status, and Birth Interval Matter? PLoS ONE 2016, 11, e0157814. [Google Scholar] [CrossRef] [Green Version]
- Akram, R.; Sultana, M.; Ali, N.; Sheikh, N.; Sarker, A.R. Prevalence and Determinants of Stunting Among Preschool Children and Its Urban–Rural Disparities in Bangladesh. Food Nutr. Bull. 2018, 39, 521–535. [Google Scholar] [CrossRef]
- Rannan-Eliya, R.P.; Hossain, S.M.; Anuranga, C.; Wickramasinghe, R.; Jayatissa, R.; Abeykoon, A.T. Trends and determinants of childhood stunting and underweight in Sri Lanka. Ceylon Med. J. 2013, 58, 10–18. [Google Scholar] [CrossRef] [Green Version]
- Srinivasan, C.S.; Zanello, G.; Shankar, B. Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC Public Health 2013, 13, 581. [Google Scholar] [CrossRef] [Green Version]
- Tiwari, R.; Ausman, L.M.; Agho, K.E. Determinants of stunting and severe stunting among under-fives: Evidence from the 2011 Nepal Demographic and Health Survey. BMC Pediatr. 2014, 14, 239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mal-Ed Network Investigators. Childhood stunting in relation to the pre- and postnatal environment during the first 2 years of life: The MAL-ED longitudinal birth cohort study. PLoS Med. 2017, 14, e1002408. [Google Scholar] [CrossRef]
- Girma, A.; Woldie, H.; Mekonnen, F.A.; Gonete, K.A.; Sisay, M. Undernutrition and associated factors among urban children aged 24–59 months in Northwest Ethiopia: A community based cross sectional study. BMC Pediatrics 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Aguayo, V.M.; Menon, P. Stop stunting: Improving child feeding, women’s nutrition and household sanitation in South Asia. Matern. Child Nutr. 2016, 12, 3–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aguayo, V.M.; Nair, R.; Badgaiyan, N.; Krishna, V. Determinants of stunting and poor linear growth in children under 2 years of age in India: An in-depth analysis of Maharashtra’s comprehensive nutrition survey. Matern. Child Nutr. 2016, 12 (Suppl. 1), 121–140. [Google Scholar] [CrossRef]
- Khan, S.; Zaheer, S.; Safdar, N.F. Determinants of stunting, underweight and wasting among children <5 years of age: Evidence from 2012–2013 Pakistan demographic and health survey. BMC Public Health 2019, 19, 358. [Google Scholar] [CrossRef] [Green Version]
- Hossain, F.B.; Shawon, M.S.R.; Al-Abid, M.S.U.; Mahmood, S.; Adhikary, G.; Bulbul, M.M.I. Double burden of malnutrition in children aged 24 to 59 months by socioeconomic status in five South Asian countries: Evidence from demographic and health surveys. BMJ Open 2020, 10, e032866. [Google Scholar] [CrossRef] [Green Version]
- Kang, Y.; Aguayo, V.M.; Campbell, R.K.; Dzed, L.; Joshi, V.; Waid, J.L.; Gupta, S.D.; Haselow, N.J.; West, K.P. Nutritional status and risk factors for stunting in preschool children in Bhutan. Matern. Child Nutr. 2018, 14, e12653. [Google Scholar] [CrossRef]
- Kim, R.; Mejía-Guevara, I.; Corsi, D.J.; Aguayo, V.M.; Subramanian, S.V. Relative importance of 13 correlates of child stunting in South Asia: Insights from nationally representative data from Afghanistan, Bangladesh, India, Nepal, and Pakistan. Soc. Sci. Med. 2017, 187, 144–154. [Google Scholar] [CrossRef]
- UNICEF. Children in South Asia. Available online: https://www.unicef.org/rosa/children-south-asia (accessed on 5 November 2020).
- Measure DHS. The Demographic and Health Survey Program. Available online: https://dhsprogram.com/publications/index.cfm (accessed on 27 February 2020).
- Corsi, D.J.; Neuman, M.; Finlay, J.E.; Subramanian, S.V. Demographic and health surveys: A profile. Int J Epidemiol. 2012, 41, 1602–1613. [Google Scholar] [CrossRef]
- WHO. Child Growth Standards Software. WHO Anthro (Version 3.2.2, January 2011) and Macros. Available online: http://www.who.int/childgrowth/software/en/ (accessed on 10 September 2020).
- Titaley, C.R.; Dibley, M.J.; Agho, K.; Roberts, C.L.; Hall, J. Determinants of neonatal mortality in Indonesia. BMC Public Health 2008, 8, 232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Z.; Kim, R.; Vollmer, S.; Subramanian, S.V. Factors Associated With Child Stunting, Wasting, and Underweight in 35 Low- and Middle-Income Countries. JAMA Netw. Open 2020, 3, e203386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Conclusions of a Consensus Meeting Held 6–8 November 2007; WHO: Washington, DC, USA, 2007. [Google Scholar]
- United Nations. Population. Available online: https://www.un.org/en/sections/issues-depth/population/index.html (accessed on 8 October 2020).
- United Nations Population Fund. Maldives Population Projections 2014–2054. Available online: http://statisticsmaldives.gov.mv/nbs/wp-content/uploads/2018/07/Maldives-Population-Projections-2014-2054.pdf (accessed on 25 October 2020).
- World Health Organisation. Global and Regional Trends by WHO REGIONS, 1990–2030. Available online: https://apps.who.int/gho/data/node.main-searo.NUTWHOREGIONS?lang=en (accessed on 30 August 2020).
- Krishna, A.; Mejía-Guevara, I.; McGovern, M.; Aguayo, V.M.; Subramanian, S.V. Trends in inequalities in child stunting in South Asia. Matern. Child Nutr. 2018, 14, e12517. [Google Scholar] [CrossRef] [PubMed]
- Marriott, B.P.; White, A.; Hadden, L.; Davies, J.C.; Wallingford, J.C. World Health Organization (WHO) infant and young child feeding indicators: Associations with growth measures in 14 low-income countries. Matern. Child Nutr. 2012, 8, 354–370. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walker, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 382, 452–477. [Google Scholar] [CrossRef]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Gribble, J.N.; Murray, N.J.; Menotti, E.P. Reconsidering childhood undernutrition: Can birth spacing make a difference? An analysis of the 2002–2003 El Salvador National Family Health Survey. Matern. Child Nutr. 2009, 5, 49–63. [Google Scholar] [CrossRef] [PubMed]
- Rutstein, S.O. Effects of preceding birth intervals on neonatal, infant and under-five years mortality andnutritional status in developing countries: Evidence from the demographic and health surveys. Int. J. Gynecol. Obstet. 2005, 89, S7–S24. [Google Scholar] [CrossRef] [PubMed]
- Olinto, M.T.; Victora, C.G.; Barros, F.C.; Tomasi, E. Determinants of malnutrition in a low-income population: Hierarchical analytical model. Cad. Saúde Pública 1993, 9 (Suppl. 1), 14–27. [Google Scholar] [CrossRef] [Green Version]
- United Nations. Sustainable Development Goals Indicators. Available online: https://unstats.un.org/sdgs/metadata/?Text=&Goal=2&Target= (accessed on 3 October 2020).
- Mushtaq, M.U.; Gull, S.; Khurshid, U.; Shahid, U.; Shad, M.A.; Siddiqui, A.M. Prevalence and socio-demographic correlates of stunting and thinness among Pakistani primary school children. BMC Public Health 2011, 11, 790. [Google Scholar] [CrossRef] [Green Version]
- Hasan, M.T.; Soares Magalhaes, R.J.; Williams, G.M.; Mamun, A.A. The role of maternal education in the 15-year trajectory of malnutrition in children under 5 years of age in Bangladesh. Matern. Child Nutr. 2016, 12, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Abuya, B.A.; Onsomu, E.O.; Kimani, J.K.; Moore, D. Influence of Maternal Education on Child Immunization and Stunting in Kenya. Matern. Child Health J. 2011, 15, 1389–1399. [Google Scholar] [CrossRef] [PubMed]
- Handayani, F.; Siagian, A.; Aritonang, E. Mother’s Education as A Determinant of Stunting among Children of Age 24 to 59 Months in North Sumatera Province of Indonesia. IOSR J. Humanit. Soc. Sci. 2017, 22, 58–64. [Google Scholar] [CrossRef]
- Benedict, R.K.; Craig, H.C.; Torlesse, H.; Stoltzfus, R.J. Trends and predictors of optimal breastfeeding among children 0–23 months, South Asia: Analysis of national survey data. Matern. Child Nutr. 2018, 14, e12698. [Google Scholar] [CrossRef]
- Barrera, A. The role of maternal schooling and its interaction with public health programs in child health production. J. Dev. Econ. 1990, 32, 69–91. [Google Scholar] [CrossRef] [Green Version]
- Buchmann, C. The Debt Crisis, Structural Adjustment and Women’s Education. Int. J. Comp. Sociol. 1996, 37, 5–30. [Google Scholar] [CrossRef]
- Paul Schultz, T. Why Governments Should Invest More to Educate Girls. World Dev. 2002, 30, 207–225. [Google Scholar] [CrossRef]
- Caldwell, J. Education as a factor in mortality decline: An examination of Nigerian data. Popul. Stud. 1979, 33, 395–413. [Google Scholar] [CrossRef]
- Caldwell, J.C. How is greater maternal education translated into lower child mortality? Health Transit. Rev. 1994, 4, 224–229. [Google Scholar]
- Özaltin, E.; Hill, K.; Subramanian, S.V. Association of Maternal Stature with Offspring Mortality, Underweight, and Stunting in Low- to Middle-Income Countries. JAMA 2010, 303, 1507–1516. [Google Scholar] [CrossRef] [Green Version]
- Hong, R.; Banta, J.E.; Betancourt, J.A. Relationship between household wealth inequality and chronic childhood under-nutrition in Bangladesh. Int. J. Equity Health 2006, 5, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalasani, S.; Rutstein, S. Household wealth and child health in India. Popul. Stud. 2014, 68, 15–41. [Google Scholar] [CrossRef] [PubMed]
- Ramli; Agho, K.E.; Inder, K.J.; Bowe, S.J.; Jacobs, J.; Dibley, M.J. Prevalence and risk factors for stunting and severe stunting among under-fives in North Maluku province of Indonesia. BMC Pediatrics 2009, 9, 64. [Google Scholar] [CrossRef] [Green Version]
- Bommer, C.; Vollmer, S.; Subramanian, S.V. How socioeconomic status moderates the stunting-age relationship in low-income and middle-income countries. BMJ Glob. Health 2019, 4, e001175. [Google Scholar] [CrossRef]
- Wamani, H.; Åstrøm, A.N.; Peterson, S.; Tumwine, J.K.; Tylleskär, T. Boys are more stunted than girls in Sub-Saharan Africa: A meta-analysis of 16 demographic and health surveys. BMC Pediatrics 2007, 7, 17. [Google Scholar] [CrossRef] [Green Version]
- Kavosi, E.; Hassanzadeh Rostami, Z.; Kavosi, Z.; Nasihatkon, A.; Moghadami, M.; Heidari, M. Prevalence and determinants of under-nutrition among children under six: A cross-sectional survey in Fars province, Iran. Int. J. Health Policy Manag. 2014, 3, 71–76. [Google Scholar] [CrossRef]
- Raj, A.; McDougal, L.P.; Silverman, J.G. Gendered Effects of Siblings on Child Malnutrition in South Asia: Cross-sectional Analysis of Demographic and Health Surveys from Bangladesh, India, and Nepal. Matern. Child Health J. 2015, 19, 217–226. [Google Scholar] [CrossRef] [Green Version]
- Edmeades, J.; Pande, R.; Macquarrie, K.; Falle, T.; Malhotra, A. TWO SONS AND A DAUGHTER: SEX COMPOSITION AND WOMEN’S REPRODUCTIVE BEHAVIOUR IN MADHYA PRADESH, INDIA. J. Biosoc. Sci. 2012, 44, 749–764. [Google Scholar] [CrossRef]
- Khatun, M.; Stenlund, H.; Hörnell, A. BRAC initiative towards promoting gender and social equity in health: A longitudinal study of child growth in Matlab, Bangladesh. Public Health Nutr. 2004, 7, 1071–1079. [Google Scholar] [CrossRef]
- Baker, P.; Friel, S. Processed foods and the nutrition transition: Evidence from Asia: Processed foods and nutrition transition in Asia. Obes. Rev. 2014, 15, 564–577. [Google Scholar] [CrossRef] [Green Version]
- Huffman, S.L.; Piwoz, E.G.; Vosti, S.A.; Dewey, K.G. Babies, soft drinks and snacks: A concern in low- and middle-income countries? Matern. Child Nutr. 2014, 10, 562–574. [Google Scholar] [CrossRef] [PubMed]
- Chirande, L.; Charwe, D.; Mbwana, H.; Victor, R.; Kimboka, S.; Issaka, A.I.; Baines, S.K.; Dibley, M.J.; Agho, K.E. Determinants of stunting and severe stunting among under-fives in Tanzania: Evidence from the 2010 cross-sectional household survey. BMC Pediatrics 2015, 15, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jehan, K.; Sidney, K.; Smith, H.; de Costa, A. Improving access to maternity services: An overview of cash transfer and voucher schemes in South Asia. Reprod. Health Matters 2012, 20, 142–154. [Google Scholar] [CrossRef] [Green Version]
- Buisman, L.R.; Van de Poel, E.; O’Donnell, O.; van Doorslaer, E.K.A. What explains the fall in child stunting in Sub-Saharan Africa? SSM Popul. Health 2019, 8, 100384. [Google Scholar] [CrossRef] [PubMed]
- Menon, P.; Headey, D.; Avula, R.; Nguyen, P.H. Understanding the geographical burden of stunting in India: A regression-decomposition analysis of district-level data from 2015–16. Matern. Child Nutr. 2018, 14, e12620. [Google Scholar] [CrossRef]
- Titaley, C.R.; Ariawan, I.; Hapsari, D.; Muasyaroh, A.; Dibley, M.J. Determinants of the Stunting of Children Under Two Years Old in Indonesia: A Multilevel Analysis of the 2013 Indonesia Basic Health Survey. Nutrients 2019, 11, 1106. [Google Scholar] [CrossRef] [Green Version]
- Ribeiro Sarmento, D. Traditional Birth Attendance (TBA) in a health system: What are the roles, benefits and challenges: A case study of incorporated TBA in Timor-Leste. Asia Pac. Fam. Med. 2014, 13, 12. [Google Scholar] [CrossRef] [Green Version]
- Falle, T.Y.; Mullany, L.C.; Thatte, N.; Khatry, S.K.; LeClerq, S.C.; Darmstadt, G.L.; Katz, J.; Tielsch, J.M. Potential Role of Traditional Birth Attendants in Neonatal Healthcare in Rural Southern Nepal. J. Health Popul. Nutr. 2009, 27, 53–61. [Google Scholar] [CrossRef] [Green Version]
- Campbell, O.M.R.; Graham, W.J. Strategies for reducing maternal mortality: Getting on with what works. Lancet 2006, 368, 1284–1299. [Google Scholar] [CrossRef]



| Variables | Model 1: Basic | Model 2: Basic and Underlying | Model 3: Basic, Underlying and Immediate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||
| Countries | ||||||||||||
| Maldives | 1.00 | 1.00 | 1.00 | |||||||||
| India | 1.83 | 1.11 | 3.02 | 0.018 | 1.74 | 0.99 | 3.08 | 0.055 | 1.41 | 0.78 | 2.57 | 0.250 |
| Bangladesh | 1.73 | 1.02 | 2.93 | 0.042 | 1.41 | 0.78 | 2.57 | 0.255 | 1.12 | 0.60 | 2.06 | 0.727 |
| Nepal | 1.74 | 0.99 | 3.09 | 0.056 | 1.14 | 0.62 | 2.11 | 0.678 | 0.87 | 0.46 | 1.66 | 0.682 |
| Pakistan | 1.51 | 0.85 | 2.67 | 0.160 | 1.50 | 0.80 | 2.82 | 0.207 | 1.29 | 0.67 | 2.50 | 0.447 |
| Type of place of residence | ||||||||||||
| Urban | 1.00 | 1.00 | 1.00 | |||||||||
| Rural | 1.34 | 1.12 | 1.61 | 0.001 | 1.02 | 0.86 | 1.22 | 0.808 | 1.01 | 0.86 | 1.19 | 0.891 |
| Working status | ||||||||||||
| Not working | 1.00 | 1.00 | ||||||||||
| Working | 1.35 | 1.00 | 1.82 | 0.052 | 1.15 | 0.87 | 1.53 | 0.331 | ||||
| Mother’s education | ||||||||||||
| Secondary or higher | 1.00 | 1.00 | ||||||||||
| Primary | 1.28 | 0.95 | 1.72 | 0.104 | 1.26 | 0.96 | 1.65 | 0.089 | ||||
| No education | 1.66 | 1.24 | 2.23 | 0.001 | 1.65 | 1.29 | 2.13 | <0.001 | ||||
| Maternal age at child’s birth | ||||||||||||
| less than 20 | 1.00 | 1.00 | ||||||||||
| 20–29 | 0.82 | 0.69 | 0.99 | 0.034 | 0.90 | 0.75 | 1.08 | 0.242 | ||||
| 30–39 | 0.76 | 0.58 | 0.99 | 0.040 | 0.92 | 0.70 | 1.21 | 0.561 | ||||
| 40+ | 0.56 | 0.35 | 0.90 | 0.016 | 0.81 | 0.48 | 1.37 | 0.429 | ||||
| Mother’s age | ||||||||||||
| 15–24 | 1.00 | 1.00 | ||||||||||
| 25–34 | 1.16 | 0.99 | 1.37 | 0.073 | 0.99 | 0.85 | 1.15 | 0.878 | ||||
| 35–49 | 1.64 | 1.17 | 2.30 | 0.004 | 1.18 | 0.84 | 1.65 | 0.339 | ||||
| Mother’s marital status | ||||||||||||
| Currently married | 1.00 | 1.00 | ||||||||||
| Formerly married $ | 0.48 | 0.21 | 1.09 | 0.079 | 0.37 | 0.15 | 0.92 | 0.032 | ||||
| Maternal height | ||||||||||||
| ≥160 cm | 1.00 | 1.00 | ||||||||||
| 155–159 | 1.09 | 0.83 | 1.42 | 0.549 | 1.10 | 0.82 | 1.48 | 0.531 | ||||
| 150–154 | 1.55 | 1.19 | 2.03 | 0.001 | 1.54 | 1.15 | 2.06 | 0.004 | ||||
| 145–149 | 1.92 | 1.49 | 2.47 | <0.001 | 2.00 | 1.51 | 2.65 | <0.001 | ||||
| <145 cm | 2.69 | 1.95 | 3.72 | <0.001 | 2.98 | 2.14 | 4.15 | <0.001 | ||||
| Maternal BMI (kg/m2) | ||||||||||||
| 25+ | 1.00 | 1.00 | ||||||||||
| 19–25 | 1.10 | 0.89 | 1.37 | 0.373 | 1.09 | 0.89 | 1.34 | 0.403 | ||||
| <= 18.5 | 1.29 | 1.00 | 1.68 | 0.053 | 1.25 | 0.97 | 1.61 | 0.088 | ||||
| Combined birth rank and birth interval | ||||||||||||
| 1st birth rank | 1.00 | 1.00 | ||||||||||
| 2nd/3rd birth rank, more than 2 years interval | 0.89 | 0.74 | 1.07 | 0.220 | 0.98 | 0.82 | 1.16 | 0.786 | ||||
| 2nd/3rd birth rank, less than or equal 2 | 1.19 | 0.99 | 1.44 | 0.071 | 1.24 | 1.02 | 1.51 | 0.031 | ||||
| 4th birth rank, more than 2 years interval | 0.91 | 0.69 | 1.18 | 0.469 | 1.00 | 0.79 | 1.28 | 0.984 | ||||
| 4th birth rank, less than or equal to 2 | 1.19 | 0.92 | 1.55 | 0.182 | 1.27 | 0.98 | 1.65 | 0.072 | ||||
| Paternal occupation | ||||||||||||
| Non-agriculture | 1.00 | 1.00 | ||||||||||
| Agriculture | 1.11 | 0.83 | 1.49 | 0.473 | 1.09 | 0.82 | 1.45 | 0.552 | ||||
| Not working | 1.00 | 0.75 | 1.33 | 0.980 | 0.94 | 0.68 | 1.29 | 0.688 | ||||
| Power over earnings (Woman has money autonomy) | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 1.12 | 0.82 | 1.55 | 0.471 | 1.10 | 0.79 | 1.51 | 0.579 | ||||
| Power over Household decision making | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 0.86 | 0.63 | 1.17 | 0.329 | 0.89 | 0.62 | 1.27 | 0.529 | ||||
| Woman has health care autonomy | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 0.95 | 0.70 | 1.28 | 0.717 | 0.90 | 0.65 | 1.24 | 0.526 | ||||
| Pooled Household wealth index | ||||||||||||
| Richest | 1.00 | 1.00 | ||||||||||
| Richer | 0.93 | 0.74 | 1.18 | 0.567 | 0.99 | 0.78 | 1.25 | 0.910 | ||||
| Middle | 1.05 | 0.82 | 1.33 | 0.714 | 1.07 | 0.85 | 1.37 | 0.558 | ||||
| Poorer | 1.05 | 0.77 | 1.42 | 0.773 | 1.05 | 0.77 | 1.44 | 0.744 | ||||
| Poorest | 1.11 | 0.81 | 1.52 | 0.515 | 1.12 | 0.82 | 1.52 | 0.487 | ||||
| Source of drinking water | ||||||||||||
| Not improved | 1.00 | 1.00 | ||||||||||
| Improved | 1.14 | 0.96 | 1.36 | 0.130 | 1.05 | 0.89 | 1.24 | 0.555 | ||||
| Type of toilet facility | ||||||||||||
| Improved | 1.00 | 1.00 | ||||||||||
| Unimproved | 1.04 | 0.85 | 1.26 | 0.725 | 1.11 | 0.92 | 1.33 | 0.273 | ||||
| Combined mode and place of delivery | ||||||||||||
| Caesarean and Health Facility | 1.00 | 1.00 | ||||||||||
| Vaginal and Health Facility | 1.52 | 1.19 | 1.94 | 0.001 | 1.61 | 1.30 | 2.00 | <0.001 | ||||
| Home | 1.69 | 1.31 | 2.18 | <0.001 | 1.81 | 1.42 | 2.31 | <0.001 | ||||
| Delivery Assistance | ||||||||||||
| Health professional | 1.00 | 1.00 | ||||||||||
| Traditional birth attendant | 0.81 | 0.66 | 1.00 | 0.050 | 0.79 | 0.65 | 0.97 | 0.021 | ||||
| Other untrained & | 0.93 | 0.80 | 1.09 | 0.385 | 0.92 | 0.79 | 1.08 | 0.316 | ||||
| Antenatal clinic visits | ||||||||||||
| ≥8 | 1.00 | 1.00 | ||||||||||
| 4 to 7 | 1.03 | 0.87 | 1.23 | 0.718 | 1.00 | 0.83 | 1.20 | 0.974 | ||||
| 1 to 3 | 1.32 | 1.04 | 1.67 | 0.021 | 1.21 | 0.99 | 1.50 | 0.070 | ||||
| None | 1.38 | 1.15 | 1.65 | <0.001 | 1.16 | 0.97 | 1.41 | 0.102 | ||||
| Media | ||||||||||||
| Reads newspaper | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 1.10 | 0.91 | 1.33 | 0.323 | 1.11 | 0.93 | 1.33 | 0.250 | ||||
| Listening radio | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 0.95 | 0.78 | 1.16 | 0.633 | 1.01 | 0.82 | 1.25 | 0.891 | ||||
| Watches television | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 1.05 | 0.91 | 1.22 | 0.505 | 1.00 | 0.87 | 1.14 | 0.957 | ||||
| Dietary diversity score | ||||||||||||
| <4 food Inadequate | 1.00 | |||||||||||
| 4+ foods Adequate | 0.80 | 0.66 | 0.96 | 0.015 | ||||||||
| Initiation of breastfeeding | ||||||||||||
| more than 1 h | 1.00 | |||||||||||
| within 1 h | 1.01 | 0.77 | 1.32 | 0.953 | ||||||||
| Currently breastfeeding | ||||||||||||
| Yes | 1.00 | |||||||||||
| No | 0.91 | 0.80 | 1.04 | 0.174 | ||||||||
| Duration of breastfeeding | ||||||||||||
| Up to 12 months | 1.00 | |||||||||||
| >12 months | 1.37 | 1.06 | 1.75 | 0.015 | ||||||||
| Vitamin A supplement | ||||||||||||
| Yes | 1.00 | |||||||||||
| No | 1.14 | 1.00 | 1.30 | 0.055 | ||||||||
| Child’s age in months | ||||||||||||
| 0 to 5 | 1.00 | |||||||||||
| 6 to 11 | 1.21 | 0.97 | 1.51 | 0.090 | ||||||||
| 12 to 17 | 2.32 | 1.61 | 3.36 | <0.001 | ||||||||
| 18 to 23 | 3.51 | 2.38 | 5.17 | <0.001 | ||||||||
| Sex of child | ||||||||||||
| Female | 1.00 | |||||||||||
| Male | 1.22 | 1.08 | 1.39 | 0.002 | ||||||||
| Vaccination | ||||||||||||
| No | 1.00 | |||||||||||
| Yes ** | 1.04 | 0.88 | 1.23 | 0.670 | ||||||||
| Had diarrhoea recently | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 1.10 | 0.90 | 1.33 | 0.352 | ||||||||
| Had fever in last two weeks | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 0.95 | 0.79 | 1.14 | 0.609 | ||||||||
| Variables | Model 1: Basic | Model 2: Basic and Underlying | Model 3: Basic, Underlying and Immediate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||
| Countries | ||||||||||||
| Maldives | 1.00 | 1.00 | 1.00 | |||||||||
| India | 3.73 | 2.63 | 5.30 | <0.001 | 2.65 | 1.74 | 4.02 | <0.001 | 2.69 | 1.77 | 4.08 | <0.001 |
| Bangladesh | 3.60 | 2.34 | 5.54 | <0.001 | 2.55 | 1.37 | 4.75 | 0.003 | 2.45 | 1.30 | 4.62 | 0.006 |
| Nepal | 4.32 | 2.97 | 6.31 | <0.001 | 2.61 | 1.71 | 3.96 | <0.001 | 2.62 | 1.71 | 4.02 | <0.001 |
| Pakistan | 3.79 | 2.54 | 5.64 | <0.001 | 3.37 | 2.17 | 5.23 | <0.001 | 3.28 | 2.09 | 5.15 | <0.001 |
| Type of place of residence | ||||||||||||
| Urban | 1.00 | 1.00 | 1.00 | |||||||||
| Rural | 1.86 | 1.62 | 2.14 | <0.001 | 1.18 | 1.04 | 1.33 | 0.008 | 1.17 | 1.04 | 1.31 | 0.011 |
| Working status | ||||||||||||
| Not working | 1.00 | 1.00 | ||||||||||
| Working | 0.87 | 0.69 | 1.08 | 0.199 | 0.86 | 0.69 | 1.08 | 0.196 | ||||
| Mother’s education | ||||||||||||
| Secondary or higher | 1.00 | 1.00 | ||||||||||
| Primary | 1.19 | 0.96 | 1.47 | 0.120 | 1.18 | 0.95 | 1.46 | 0.141 | ||||
| No education | 1.47 | 1.28 | 1.70 | <0.001 | 1.46 | 1.27 | 1.69 | <0.001 | ||||
| Maternal age at child’s birth | ||||||||||||
| Less than 20 | 1.00 | 1.00 | ||||||||||
| 20–29 | 0.98 | 0.81 | 1.18 | 0.812 | 0.98 | 0.81 | 1.18 | 0.810 | ||||
| 30–39 | 1.40 | 0.57 | 3.42 | 0.460 | 1.41 | 0.58 | 3.46 | 0.448 | ||||
| 40+ | 1.45 | 0.54 | 3.90 | 0.458 | 1.44 | 0.53 | 3.88 | 0.472 | ||||
| Mother’s age | ||||||||||||
| 15–24 | 1.00 | 1.00 | ||||||||||
| 25–34 | 0.89 | 0.77 | 1.03 | 0.119 | 0.89 | 0.77 | 1.03 | 0.118 | ||||
| 35–49 | 0.57 | 0.25 | 1.31 | 0.189 | 0.57 | 0.25 | 1.31 | 0.187 | ||||
| Mother’s marital status | ||||||||||||
| Currently married | 1.00 | 1.00 | ||||||||||
| Formerly married $ | 1.18 | 0.86 | 1.62 | 0.306 | 1.17 | 0.85 | 1.61 | 0.335 | ||||
| Maternal height | ||||||||||||
| ≥160 cm | 1.00 | 1.00 | ||||||||||
| 155–159 | 1.55 | 1.24 | 1.94 | <0.001 | 1.53 | 1.22 | 1.91 | <0.001 | ||||
| 150–154 | 2.40 | 1.99 | 2.90 | <0.001 | 2.38 | 1.97 | 2.87 | <0.001 | ||||
| 145–149 | 3.68 | 2.91 | 4.64 | <0.001 | 3.63 | 2.87 | 4.60 | <0.001 | ||||
| <145 cm | 4.81 | 3.75 | 6.18 | <0.001 | 4.76 | 3.71 | 6.11 | <0.001 | ||||
| Maternal BMI (kg/m2) | ||||||||||||
| 25+ | 1.00 | 1.00 | ||||||||||
| 19–25 | 1.08 | 0.86 | 1.37 | 0.498 | 1.08 | 0.85 | 1.37 | 0.529 | ||||
| <=18.5 | 1.43 | 1.17 | 1.74 | <0.001 | 1.42 | 1.16 | 1.73 | 0.001 | ||||
| Combined birth rank and birth interval | ||||||||||||
| 1st birth rank | 1.00 | 1.00 | ||||||||||
| 2nd/3rd birth rank, more than 2 years interval | 1.36 | 1.16 | 1.61 | <0.001 | 1.37 | 1.16 | 1.61 | <0.001 | ||||
| 2nd/3rd birth rank, less than or equal 2 | 1.95 | 1.61 | 2.35 | <0.001 | 1.95 | 1.61 | 2.36 | <0.001 | ||||
| 4th birth rank, more than 2 years interval | 1.70 | 1.37 | 2.12 | <0.001 | 1.70 | 1.37 | 2.11 | <0.001 | ||||
| 4th birth rank, less than or equal to 2 | 1.63 | 1.23 | 2.15 | 0.001 | 1.56 | 1.17 | 2.07 | 0.002 | ||||
| Paternal occupation | ||||||||||||
| Non-agriculture | 1.00 | 1.00 | ||||||||||
| Agriculture | 1.13 | 0.95 | 1.34 | 0.174 | 1.14 | 0.96 | 1.35 | 0.146 | ||||
| Not working | 1.08 | 0.89 | 1.32 | 0.412 | 1.09 | 0.90 | 1.32 | 0.401 | ||||
| Power over earnings (Woman has money autonomy) | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 1.27 | 1.01 | 1.59 | 0.043 | 1.28 | 1.02 | 1.60 | 0.035 | ||||
| Power over Household decision making | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 0.85 | 0.63 | 1.14 | 0.287 | 0.83 | 0.62 | 1.12 | 0.221 | ||||
| Woman has health care autonomy | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 0.91 | 0.70 | 1.20 | 0.512 | 0.93 | 0.71 | 1.21 | 0.572 | ||||
| Pooled Household wealth index | ||||||||||||
| Richest | 1.00 | 1.00 | ||||||||||
| Richer | 1.03 | 0.79 | 1.35 | 0.805 | 1.03 | 0.79 | 1.35 | 0.813 | ||||
| Middle | 1.37 | 1.13 | 1.66 | 0.002 | 1.36 | 1.12 | 1.66 | 0.002 | ||||
| Poorer | 1.43 | 1.18 | 1.75 | <0.001 | 1.43 | 1.17 | 1.74 | <0.001 | ||||
| Poorest | 1.65 | 1.31 | 2.06 | <0.001 | 1.64 | 1.31 | 2.05 | <0.001 | ||||
| Source of drinking water | ||||||||||||
| Not improved | 1.00 | 1.00 | ||||||||||
| Improved | 1.02 | 0.90 | 1.14 | 0.790 | 1.02 | 0.90 | 1.15 | 0.744 | ||||
| Type of toilet facility | ||||||||||||
| Improved | 1.00 | 1.00 | ||||||||||
| Unimproved | 1.00 | 0.86 | 1.16 | 0.950 | 1.00 | 0.86 | 1.15 | 0.963 | ||||
| Combined mode and place of delivery | ||||||||||||
| Caesarean and Health Facility | 1.00 | 1.00 | ||||||||||
| Non and Health Facility | 1.27 | 0.97 | 1.67 | 0.085 | 1.27 | 0.97 | 1.67 | 0.086 | ||||
| Non C and Home | 1.21 | 0.91 | 1.62 | 0.193 | 1.23 | 0.92 | 1.64 | 0.171 | ||||
| Delivery Assistance | ||||||||||||
| Health professional | 1.00 | 1.00 | ||||||||||
| Traditional birth attendant | 1.03 | 0.90 | 1.17 | 0.674 | 1.02 | 0.90 | 1.16 | 0.735 | ||||
| Other untrained & | 1.12 | 0.96 | 1.31 | 0.159 | 1.10 | 0.94 | 1.28 | 0.242 | ||||
| Antenatal clinic visits | ||||||||||||
| ≥8 | 1.00 | 1.00 | ||||||||||
| 4 to 7 | 1.09 | 0.86 | 1.39 | 0.482 | 1.09 | 0.86 | 1.39 | 0.479 | ||||
| 1 to 3 | 1.41 | 1.05 | 1.88 | 0.021 | 1.41 | 1.05 | 1.88 | 0.022 | ||||
| None | 1.17 | 0.95 | 1.45 | 0.141 | 1.20 | 0.97 | 1.49 | 0.096 | ||||
| Media | ||||||||||||
| Reads newspaper | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 1.18 | 0.98 | 1.43 | 0.085 | 1.18 | 0.98 | 1.43 | 0.087 | ||||
| Listening radio | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 1.23 | 0.96 | 1.57 | 0.107 | 1.22 | 0.95 | 1.58 | 0.120 | ||||
| Watches television | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 0.86 | 0.76 | 0.97 | 0.012 | 0.86 | 0.76 | 0.97 | 0.015 | ||||
| Dietary diversity score | ||||||||||||
| <4 food Inadequate | 1.00 | |||||||||||
| 4+ foods Adequate | 0.88 | 0.71 | 1.11 | 0.284 | ||||||||
| Vitamin A supplement | ||||||||||||
| Yes | 1.00 | |||||||||||
| No | 1.01 | 0.92 | 1.10 | 0.837 | ||||||||
| Sex of child | ||||||||||||
| Female | 1.00 | |||||||||||
| Male | 0.96 | 0.87 | 1.07 | 0.481 | ||||||||
| Vaccination | ||||||||||||
| No | 1.00 | |||||||||||
| Yes ** | 0.99 | 0.86 | 1.13 | 0.835 | ||||||||
| Had diarrhoea recently | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 1.21 | 1.03 | 1.42 | 0.018 | ||||||||
| Had fever in last two weeks | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 1.16 | 1.02 | 1.31 | 0.022 | ||||||||
| Variables | Model 1: Basic | Model 2: Basic and Underlying | Model 3: Basic, Underlying and Immediate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||
| Countries | ||||||||||||
| Maldives | 1.00 | 1.00 | 1.00 | |||||||||
| India | 2.78 | 1.97 | 3.93 | <0.001 | 2.29 | 1.58 | 3.32 | <0.001 | 2.07 | 1.44 | 2.98 | <0.001 |
| Bangladesh | 2.61 | 1.81 | 3.76 | <0.001 | 1.85 | 1.20 | 2.87 | 0.006 | 1.77 | 1.16 | 2.71 | 0.008 |
| Nepal | 2.96 | 2.06 | 4.25 | <0.001 | 1.91 | 1.36 | 2.70 | <0.001 | 1.77 | 1.25 | 2.51 | 0.001 |
| Pakistan | 2.61 | 1.77 | 3.85 | <0.001 | 2.47 | 1.71 | 3.57 | <0.001 | 2.28 | 1.57 | 3.31 | <0.001 |
| Type of place of residence | ||||||||||||
| Urban | 1.00 | 1.00 | 1.00 | |||||||||
| Rural | 1.64 | 1.45 | 1.85 | <0.001 | 1.13 | 1.01 | 1.25 | 0.028 | 1.11 | 1.00 | 1.23 | 0.056 |
| Working status | ||||||||||||
| Not working | 1.00 | 1.00 | ||||||||||
| Working | 1.02 | 0.86 | 1.21 | 0.851 | 0.97 | 0.80 | 1.17 | 0.756 | ||||
| Mother’s education | ||||||||||||
| Secondary or higher | 1.00 | 1.00 | ||||||||||
| Primary | 1.21 | 0.97 | 1.53 | 0.095 | 1.21 | 0.97 | 1.52 | 0.096 | ||||
| No education | 1.55 | 1.31 | 1.83 | <0.001 | 1.59 | 1.34 | 1.88 | <0.001 | ||||
| Maternal age at child’s birth | ||||||||||||
| Less than 20 | 1.00 | 1.00 | ||||||||||
| 20–29 | 0.80 | 0.69 | 0.93 | 0.004 | 0.89 | 0.77 | 1.02 | 0.091 | ||||
| 30–39 | 0.87 | 0.52 | 1.46 | 0.596 | 1.02 | 0.61 | 1.69 | 0.950 | ||||
| 40+ | 0.81 | 0.44 | 1.51 | 0.513 | 0.99 | 0.54 | 1.80 | 0.967 | ||||
| Mother’s age | ||||||||||||
| 15–24 | 1.00 | 1.00 | ||||||||||
| 25–34 | 1.14 | 1.02 | 1.26 | 0.018 | 1.01 | 0.91 | 1.12 | 0.877 | ||||
| 35–49 | 1.11 | 0.70 | 1.78 | 0.657 | 0.90 | 0.56 | 1.43 | 0.645 | ||||
| Mother’s marital status | ||||||||||||
| Currently married | 1.00 | 1.00 | ||||||||||
| Formerly married $ | 1.01 | 0.73 | 1.39 | 0.958 | 0.98 | 0.72 | 1.33 | 0.886 | ||||
| Maternal height | ||||||||||||
| ≥160 cm | 1.00 | 1.00 | ||||||||||
| 155–159 | 1.36 | 1.14 | 1.64 | 0.001 | 1.36 | 1.12 | 1.64 | 0.002 | ||||
| 150–154 | 2.03 | 1.73 | 2.38 | <0.001 | 2.03 | 1.72 | 2.40 | <0.001 | ||||
| 145–149 | 2.88 | 2.38 | 3.49 | <0.001 | 2.87 | 2.37 | 3.48 | <0.001 | ||||
| <145 cm | 3.73 | 2.95 | 4.72 | <0.001 | 3.80 | 2.99 | 4.82 | <0.001 | ||||
| Maternal BMI (kg/m2) | ||||||||||||
| 25+ | 1.00 | 1.00 | ||||||||||
| 19–25 | 1.06 | 0.85 | 1.32 | 0.615 | 1.09 | 0.89 | 1.34 | 0.405 | ||||
| <= 18.5 | 1.31 | 1.08 | 1.58 | 0.005 | 1.36 | 1.14 | 1.63 | 0.001 | ||||
| Combined birth rank and birth interval | ||||||||||||
| 1st birth rank | 1.00 | 1.00 | ||||||||||
| 2nd/3rd birth rank, more than 2 years interval | 1.16 | 1.05 | 1.27 | 0.003 | 1.19 | 1.07 | 1.31 | 0.001 | ||||
| 2nd/3rd birth rank, less than or equal 2 | 1.62 | 1.12 | 1.57 | <0.001 | 1.67 | 1.43 | 1.94 | <0.001 | ||||
| 4th birth rank, more than 2 yrs interval | 1.32 | 1.12 | 1.57 | 0.001 | 1.42 | 1.21 | 1.66 | <0.001 | ||||
| 4th birth rank, less than or equal to 2 | 1.44 | 1.17 | 1.76 | <0.001 | 1.50 | 1.23 | 1.84 | <0.001 | ||||
| Paternal occupation | ||||||||||||
| Non-agriculture | 1.00 | 1.00 | ||||||||||
| Agriculture | 1.13 | 0.97 | 1.32 | 0.114 | 1.14 | 0.97 | 1.33 | 0.101 | ||||
| Not working | 1.09 | 0.95 | 1.26 | 0.222 | 1.07 | 0.93 | 1.23 | 0.343 | ||||
| Power over earnings (Woman has money autonomy) | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 1.23 | 1.01 | 1.49 | 0.036 | 1.22 | 1.00 | 1.49 | 0.053 | ||||
| Power over Household decision making | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 0.87 | 0.70 | 1.07 | 0.185 | 0.85 | 0.69 | 1.06 | 0.151 | ||||
| Woman has health care autonomy | ||||||||||||
| By Husband alone | 1.00 | 1.00 | ||||||||||
| Woman alone or joint decision | 0.92 | 0.74 | 1.13 | 0.412 | 0.92 | 0.74 | 1.13 | 0.416 | ||||
| Pooled Household wealth index | ||||||||||||
| Richest | 1.00 | 1.00 | ||||||||||
| Richer | 0.99 | 0.78 | 1.24 | 0.899 | 0.99 | 0.78 | 1.24 | 0.899 | ||||
| Middle | 1.22 | 1.02 | 1.46 | 0.026 | 1.22 | 1.02 | 1.45 | 0.033 | ||||
| Poorer | 1.25 | 1.03 | 1.53 | 0.026 | 1.24 | 1.01 | 1.52 | 0.036 | ||||
| Poorest | 1.40 | 1.13 | 1.72 | 0.002 | 1.39 | 1.13 | 1.73 | 0.002 | ||||
| Source of drinking water | ||||||||||||
| Not improved | 1.00 | 1.00 | ||||||||||
| Improved | 1.08 | 0.98 | 1.20 | 0.127 | 1.04 | 0.93 | 1.16 | 0.521 | ||||
| Type of toilet facility | ||||||||||||
| Improved | 1.00 | 1.00 | ||||||||||
| Unimproved | 0.99 | 0.85 | 1.16 | 0.902 | 1.02 | 0.88 | 1.18 | 0.839 | ||||
| Combined mode and place of delivery | ||||||||||||
| Caesarean and Health Facility | 1.00 | 1.00 | ||||||||||
| Non and Health Facility | 1.39 | 1.08 | 1.80 | 0.011 | 1.37 | 1.08 | 1.75 | 0.011 | ||||
| Non C and Home | 1.43 | 1.10 | 1.86 | 0.008 | 1.43 | 1.11 | 1.84 | 0.006 | ||||
| Delivery Assistance | ||||||||||||
| Health professional | 1.00 | 1.00 | ||||||||||
| Traditional birth attendant | 0.94 | 0.83 | 1.06 | 0.313 | 0.94 | 0.83 | 1.06 | 0.321 | ||||
| Other untrained & | 1.04 | 0.93 | 1.16 | 0.468 | 1.04 | 0.93 | 1.17 | 0.446 | ||||
| Antenatal clinic visits | ||||||||||||
| ≥8 | 1.00 | 1.00 | ||||||||||
| 4 to 7 | 1.09 | 0.91 | 1.31 | 0.350 | 1.07 | 0.90 | 1.28 | 0.432 | ||||
| 1 to 3 | 1.34 | 1.08 | 1.66 | 0.008 | 1.35 | 1.09 | 1.67 | 0.005 | ||||
| None | 1.33 | 1.16 | 1.53 | <0.001 | 1.22 | 1.05 | 1.42 | 0.008 | ||||
| Media | ||||||||||||
| Reads newspaper | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 1.15 | 0.97 | 1.37 | 0.106 | 1.15 | 0.97 | 1.36 | 0.111 | ||||
| Listening radio | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 1.14 | 0.90 | 1.44 | 0.264 | 1.13 | 0.90 | 1.41 | 0.286 | ||||
| Watches television | ||||||||||||
| Not all | 1.00 | 1.00 | ||||||||||
| Yes ++ | 0.95 | 0.85 | 1.06 | 0.323 | 0.92 | 0.82 | 1.03 | 0.131 | ||||
| Dietary diversity score | ||||||||||||
| <4 food Inadequate | 1.00 | |||||||||||
| 4+ foods Adequate | 1.03 | 0.88 | 1.19 | 0.741 | ||||||||
| Vitamin A supplement | ||||||||||||
| Yes | 1.00 | |||||||||||
| No | 0.94 | 0.86 | 1.02 | 0.117 | ||||||||
| Child age in months | ||||||||||||
| 0–23 months | 1.00 | |||||||||||
| 24–59 months | 1.40 | 1.26 | 1.56 | <0.001 | ||||||||
| Sex of child | ||||||||||||
| Female | 1.00 | |||||||||||
| Male | 1.05 | 0.96 | 1.14 | 0.302 | ||||||||
| Vaccination | ||||||||||||
| No | 1.00 | |||||||||||
| Yes ** | 1.23 | 1.10 | 1.37 | <0.001 | ||||||||
| Had diarrhoea recently | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 1.12 | 0.99 | 1.27 | 0.060 | ||||||||
| Had fever in last two weeks | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 1.06 | 0.96 | 1.17 | 0.240 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wali, N.; Agho, K.E.; Renzaho, A.M.N. Factors Associated with Stunting among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys. Nutrients 2020, 12, 3875. https://doi.org/10.3390/nu12123875
Wali N, Agho KE, Renzaho AMN. Factors Associated with Stunting among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys. Nutrients. 2020; 12(12):3875. https://doi.org/10.3390/nu12123875
Chicago/Turabian StyleWali, Nidhi, Kingsley E. Agho, and Andre M.N. Renzaho. 2020. "Factors Associated with Stunting among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys" Nutrients 12, no. 12: 3875. https://doi.org/10.3390/nu12123875






