Meal Frequency and Skipping Breakfast Are Associated with Chronic Kidney Disease
Abstract
1. Introduction
2. Methods
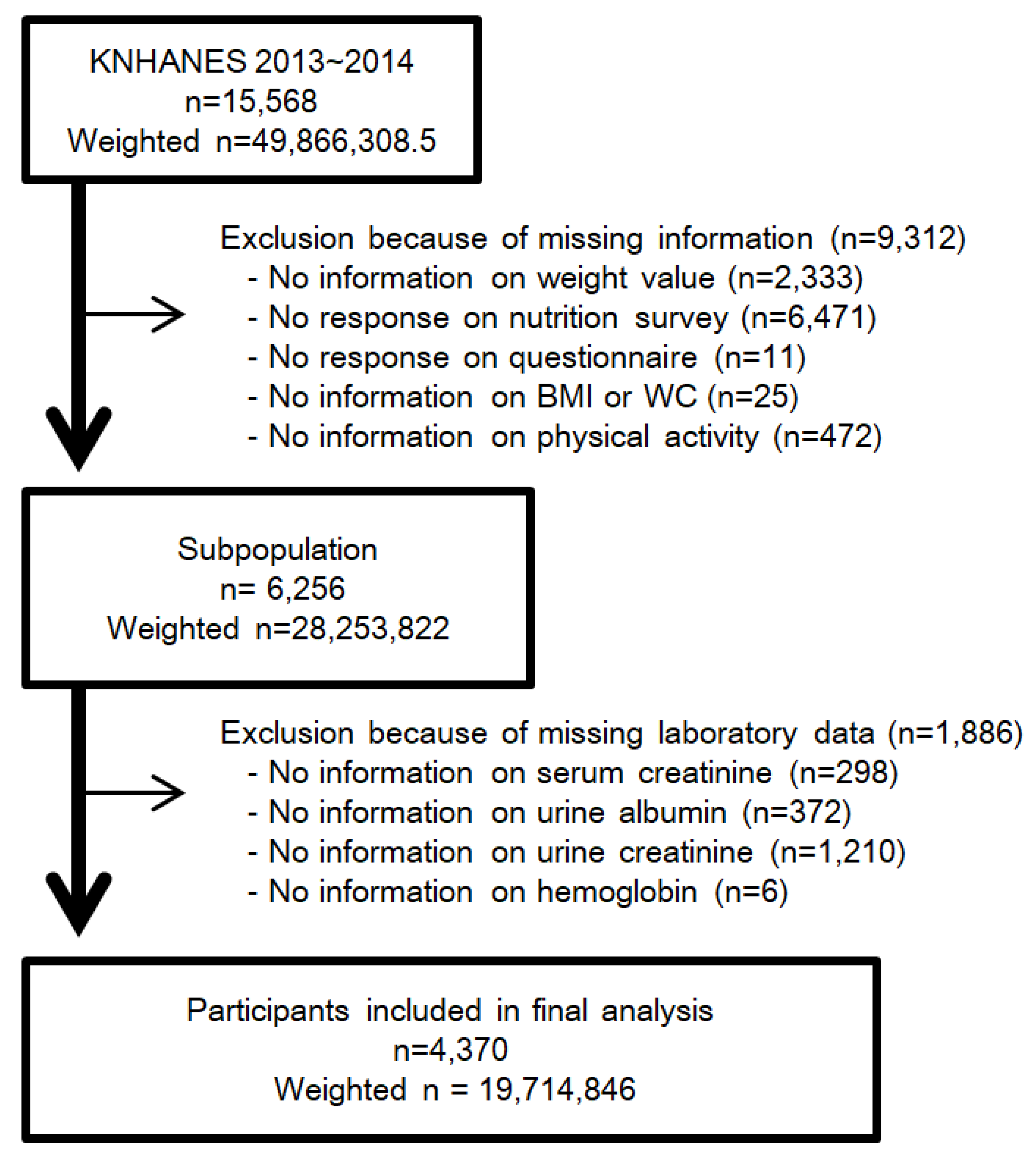
2.1. Study Population
2.2. Breakfast, Lunch, and Dinner Frequency and Meal Frequency
2.3. Definition of CKD and Other Covariates
2.4. Statistical Methods
3. Results
3.1. Baseline Characteristics
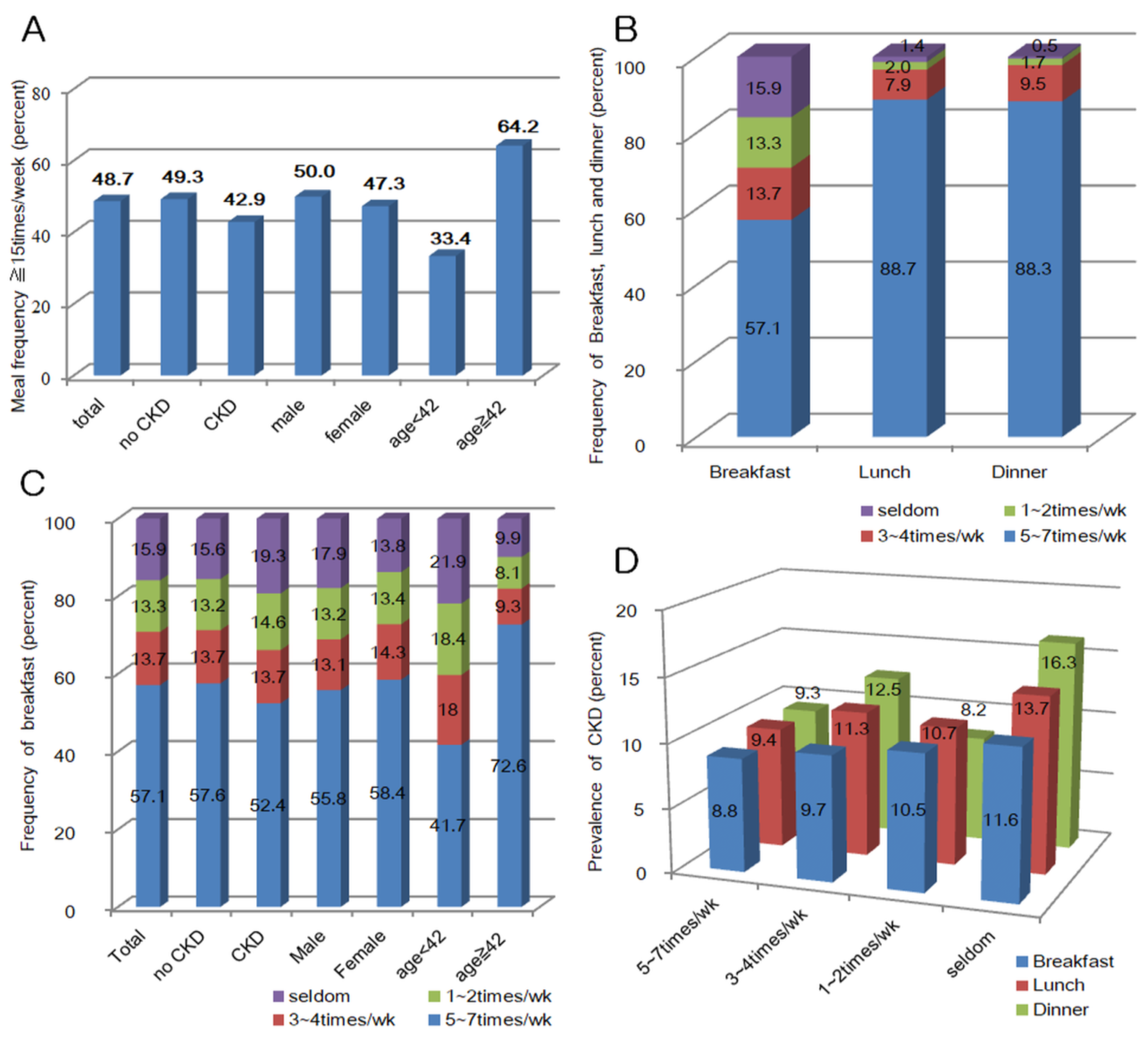
3.2. Association of CKD with Frequency of Meal
3.3. Association of CKD with Frequency of Meal Stratified by Gender and Age
3.4. Association of CKD with Frequency of Meal Stratified by eGFR and Urine ACR
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Eknoyan, G.; Lameire, N.; Eckardt, K.; Kasiske, B.; Wheeler, D.; Levin, A.; Stevens, P.; Bilous, R.; Lamb, E.; Coresh, J. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013, 3, 5–14. [Google Scholar]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic Kidney Disease. Lancet 2017, 389, 1238–1252. [Google Scholar] [CrossRef]
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.; Yang, C.W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D. Global Prevalence of Chronic Kidney Disease—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef] [PubMed]
- Eckardt, K.U.; Coresh, J.; Devuyst, O.; Johnson, R.J.; Kottgen, A.; Levey, A.S.; Levin, A. Evolving importance of kidney disease: From subspecialty to global health burden. Lancet 2013, 382, 158–169. [Google Scholar] [CrossRef]
- Kim, S.; Lim, C.S.; Han, D.C.; Kim, G.S.; Chin, H.J.; Kim, S.J.; Cho, W.Y.; Kim, Y.H.; Kim, Y.S. The prevalence of chronic kidney disease (CKD) and the associated factors to CKD in urban Korea: A population-based cross-sectional epidemiologic study. J. Korean Med. Sci. 2009, 24, S11–S21. [Google Scholar] [CrossRef]
- Ji, E.; Kim, Y.S. Prevalence of chronic kidney disease defined by using CKD-EPI equation and albumin-to-creatinine ratio in the Korean adult population. Korean J. Intern. Med. 2016, 31, 1120–1130. [Google Scholar] [CrossRef]
- Shin, S.Y.; Kwon, M.J.; Park, H.; Woo, H.Y. Comparison of chronic kidney disease prevalence examined by the chronic kidney disease epidemiology collaboration equation with that by the modification of diet in renal disease equation in Korean adult population. J. Clin. Lab Anal. 2014, 28, 320–327. [Google Scholar] [CrossRef]
- Park, J.I.; Baek, H.; Jung, H.H. Prevalence of Chronic Kidney Disease in Korea: The Korean National Health and Nutritional Examination Survey 2011–2013. J. Korean Med. Sci. 2016, 31, 915–923. [Google Scholar] [CrossRef]
- Wang, V.; Vilme, H.; Maciejewski, M.L.; Boulware, L.E. The Economic Burden of Chronic Kidney Disease and End-Stage Renal Disease. Semin. Nephrol. 2016, 36, 319–330. [Google Scholar] [CrossRef]
- Kim, S.H.; Jo, M.W.; Go, D.S.; Ryu, D.R.; Park, J. Economic burden of chronic kidney disease in Korea using national sample cohort. J. Nephrol. 2017, 30, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Feehally, J.; Khosravi, M. Effects of acute and chronic hypohydration on kidney health and function. Nutr. Rev. 2015, 73 (Suppl. 2), 110–119. [Google Scholar] [CrossRef]
- Clark, W.F.; Sontrop, J.M.; Huang, S.H.; Moist, L.; Bouby, N.; Bankir, L. Hydration and Chronic Kidney Disease Progression: A Critical Review of the Evidence. Am. J. Nephrol. 2016, 43, 281–292. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P.; Ard, J.; Baskin, M.L.; Chiuve, S.E.; Johnson, H.M.; Kris-Etherton, P.; Varady, K.; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; et al. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement from the American Heart Association. Circulation 2017, 135, e96–e121. [Google Scholar] [CrossRef] [PubMed]
- Cahill, L.E.; Chiuve, S.E.; Mekary, R.A.; Jensen, M.K.; Flint, A.J.; Hu, F.B.; Rimm, E.B. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 2013, 128, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Odegaard, A.O.; Jacobs, D.R., Jr.; Steffen, L.M.; Van Horn, L.; Ludwig, D.S.; Pereira, M.A. Breakfast frequency and development of metabolic risk. Diabetes Care 2013, 36, 3100–3106. [Google Scholar] [CrossRef]
- Smith, K.J.; Blizzard, L.; McNaughton, S.A.; Gall, S.L.; Dwyer, T.; Venn, A.J. Daily eating frequency and cardiometabolic risk factors in young Australian adults: Cross-sectional analyses. Br. J. Nutr. 2012, 108, 1086–1094. [Google Scholar] [CrossRef]
- Ballon, A.; Neuenschwander, M.; Schlesinger, S. Breakfast Skipping Is Associated with Increased Risk of Type 2 Diabetes among Adults: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J. Nutr. 2019, 149, 106–113. [Google Scholar] [CrossRef]
- Uemura, M.; Yatsuya, H.; Hilawe, E.H.; Li, Y.; Wang, C.; Chiang, C.; Otsuka, R.; Toyoshima, H.; Tamakoshi, K.; Aoyama, A. Breakfast Skipping is Positively Associated with Incidence of Type 2 Diabetes Mellitus: Evidence from the Aichi Workers’ Cohort Study. J. Epidemiol. 2015, 25, 351–358. [Google Scholar] [CrossRef]
- Ha, K.; Song, Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients 2019, 11, 2437. [Google Scholar] [CrossRef]
- Jung, C.H.; Lee, J.S.; Ahn, H.J.; Choi, J.S.; Noh, M.Y.; Lee, J.J.; Lee, E.Y.; Lim, J.H.; Lee, Y.R.; Yoon, S.Y.; et al. Association of meal frequency with metabolic syndrome in Korean adults: From the Korea National Health and Nutrition Examination Survey (KNHANES). Diabetol. Metab. Syndr. 2017, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Drummond, S.E.; Crombie, N.E.; Cursiter, M.C.; Kirk, T.R. Evidence that eating frequency is inversely related to body weight status in male, but not female, non-obese adults reporting valid dietary intakes. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Headland, M.; Clifton, P.M.; Carter, S.; Keogh, J.B. Weight-Loss Outcomes: A Systematic Review and Meta-Analysis of Intermittent Energy Restriction Trials Lasting a Minimum of 6 Months. Nutrients 2016, 8, 354. [Google Scholar] [CrossRef] [PubMed]
- Holmback, I.; Ericson, U.; Gullberg, B.; Wirfalt, E. A high eating frequency is associated with an overall healthy lifestyle in middle-aged men and women and reduced likelihood of general and central obesity in men. Br. J. Nutr. 2010, 104, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Horne, B.D.; Muhlestein, J.B.; Anderson, J.L. Health effects of intermittent fasting: Hormesis or harm? A systematic review. Am. J. Clin. Nutr. 2015, 102, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Trepanowski, J.F.; Kroeger, C.M.; Barnosky, A.; Klempel, M.C.; Bhutani, S.; Hoddy, K.K.; Gabel, K.; Freels, S.; Rigdon, J.; Rood, J.; et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern. Med. 2017, 177, 930–938. [Google Scholar] [CrossRef]
- Kent, P.S.; McCarthy, M.P.; Burrowes, J.D.; McCann, L.; Pavlinac, J.; Goeddeke-Merickel, C.M.; Wiesen, K.; Kruger, S.; Byham-Gray, L.; Pace, R.C.; et al. Academy of Nutrition and Dietetics and National Kidney Foundation: Revised 2014 Standards of Practice and Standards of Professional Performance for registered dietitian nutritionists (competent, proficient, and expert) in nephrology nutrition. J. Ren. Nutr. 2014, 24, 275–285.e45. [Google Scholar] [CrossRef]
- Kelly, J.T.; Palmer, S.C.; Wai, S.N.; Ruospo, M.; Carrero, J.J.; Campbell, K.L.; Strippoli, G.F. Healthy Dietary Patterns and Risk of Mortality and ESRD in CKD: A Meta-Analysis of Cohort Studies. Clin. J. Am. Soc. Nephrol. 2017, 12, 272–279. [Google Scholar] [CrossRef]
- Bach, K.E.; Kelly, J.T.; Palmer, S.C.; Khalesi, S.; Strippoli, G.F.M.; Campbell, K.L. Healthy Dietary Patterns and Incidence of CKD: A Meta-Analysis of Cohort Studies. Clin. J. Am. Soc. Nephrol. 2019, 14, 1441–1449. [Google Scholar] [CrossRef]
- Ajjarapu, A.S.; Hinkle, S.N.; Li, M.; Francis, E.C.; Zhang, C. Dietary Patterns and Renal Health Outcomes in the General Population: A Review Focusing on Prospective Studies. Nutrients 2019, 11, 1877. [Google Scholar] [CrossRef]
- Crews, D.C. Food as medicine for CKD: Implications for disadvantaged populations. Clin. Nephrol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Dunkler, D.; Dehghan, M.; Teo, K.K.; Heinze, G.; Gao, P.; Kohl, M.; Clase, C.M.; Mann, J.F.; Yusuf, S.; Oberbauer, R.; et al. Diet and kidney disease in high-risk individuals with type 2 diabetes mellitus. JAMA Intern. Med. 2013, 173, 1682–1692. [Google Scholar] [CrossRef] [PubMed]
- Michishita, R.; Matsuda, T.; Kawakami, S.; Kiyonaga, A.; Tanaka, H.; Morito, N.; Higaki, Y. The Association Between Unhealthy Lifestyle Behaviors and the Prevalence of Chronic Kidney Disease (CKD) in Middle-Aged and Older Men. J. Epidemiol. 2016, 26, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Wakasugi, M.; Kazama, J.J.; Yamamoto, S.; Kawamura, K.; Narita, I. A combination of healthy lifestyle factors is associated with a decreased incidence of chronic kidney disease: A population-based cohort study. Hypertens Res. 2013, 36, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Bragazzi, N.L. Ramadan fasting and chronic kidney disease: A systematic review. J. Res. Med. Sci. 2014, 19, 665–676. [Google Scholar] [PubMed]
- Hassan, S.; Hassan, F.; Abbas, N.; Hassan, K.; Khatib, N.; Edgim, R.; Fadol, R.; Khazim, K. Does Ramadan Fasting Affect Hydration Status and Kidney Function in CKD Patients? Ann. Nutr. Metab. 2018, 72, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, M.H.; Azadbakht, L. Is Ramadan fasting related to health outcomes? A review on the related evidence. J. Res. Med. Sci. 2014, 19, 987–992. [Google Scholar]
- Korea Centers for Disease Control & Prevention. Korea National Health & Nutrition Examination Survey. Available online: https://knhanes.cdc.go.kr/knhanes/eng/index.do (accessed on 26 January 2020).
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare of Korea; Korea Centers for Disease Control and Prevention. 2013 Korea Health Statistics. Available online: http://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7 (accessed on 21 January 2020).
- Ministry of Health and Welfare of Korea; Korea Centers for Disease Control and Prevention. 2014 Korea Health Statistics. Available online: http://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7 (accessed on 21 January 2020).
- Statistics Korea. Korean Statistical Information Service. Available online: https://kosis.kr/eng/ (accessed on 26 January 2020).
- Lee, H.J.; Jang, J.; Lee, S.A.; Choi, D.W.; Park, E.C. Association between Breakfast Frequency and Atherosclerotic Cardiovascular Disease Risk: A Cross-Sectional Study of KNHANES Data, 2014–2016. Int. J. Environ. Res. Public Health 2019, 16, 1853. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Rabin, R.; Gudex, C.; Selai, C.; Herdman, M. From translation to version management: A history and review of methods for the cultural adaptation of the EuroQol five-dimensional questionnaire. Value Health 2014, 17, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Korea Centers for Disease Control & Prevention. Korea National Health & Nutrition Examination Survey, 2013 & 2014, Guidelines for Nutrition Survey. Available online: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_02_02.do?classType=4 (accessed on 26 January 2020).
- Kurella, M.; Lo, J.C.; Chertow, G.M. Metabolic syndrome and the risk for chronic kidney disease among nondiabetic adults. J. Am. Soc. Nephrol. 2005, 16, 2134–2140. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Muntner, P.; Hamm, L.L.; Jones, D.W.; Batuman, V.; Fonseca, V.; Whelton, P.K.; He, J. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann. Intern. Med. 2004, 140, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Wolf, G. After all those fat years: Renal consequences of obesity. Nephrol. Dial. Transplant. 2003, 18, 2471–2474. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.M.; Chen, J.D. Inverse association between body mass index and chronic kidney disease in older diabetic adults. Ann. Epidemiol. 2013, 23, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.Y.L.; Wang, J.; Nikam, M.; Lai, B.C.; Yeoh, L.Y. Low, rather than High, Body Mass Index Is a Risk Factor for Acute Kidney Injury in Multiethnic Asian Patients: A Retrospective Observational Study. Int. J. Nephrol. 2018, 2018, 3284612. [Google Scholar] [CrossRef]
- Dittmann, K.; Hannemann, A.; Wallaschofski, H.; Rettig, R.; Stracke, S.; Volzke, H.; Nauck, M.; Friedrich, N. U-shaped association between central body fat and the urinary albumin-to-creatinine ratio and microalbuminuria. BMC Nephrol. 2013, 14, 87. [Google Scholar] [CrossRef]
- Speakman, J.R. Sex- and age-related mortality profiles during famine: Testing the ’body fat’ hypothesis. J. Biosoc. Sci. 2013, 45, 823–840. [Google Scholar] [CrossRef]
- Valencak, T.G.; Osterrieder, A.; Schulz, T.J. Sex matters: The effects of biological sex on adipose tissue biology and energy metabolism. Redox Biol. 2017, 12, 806–813. [Google Scholar] [CrossRef]
- Shi, H.; Clegg, D.J. Sex differences in the regulation of body weight. Physiol. Behav. 2009, 97, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Valle, A.; Catala-Niell, A.; Colom, B.; Garcia-Palmer, F.J.; Oliver, J.; Roca, P. Sex-related differences in energy balance in response to caloric restriction. Am. J. Physiol. Endocrinol. Metab. 2005, 289, E15–E22. [Google Scholar] [CrossRef][Green Version]
- Wang, S.Y.; Cai, G.Y.; Chen, X.M. Energy restriction in renal protection. Br. J. Nutr. 2018, 120, 1149–1158. [Google Scholar] [CrossRef] [PubMed]
- Hilliard, L.M.; Colafella, K.M.; Bulmer, L.L.; Puelles, V.G.; Singh, R.R.; Ow, C.P.; Gaspari, T.; Drummond, G.R.; Evans, R.G.; Vinh, A.; et al. Chronic recurrent dehydration associated with periodic water intake exacerbates hypertension and promotes renal damage in male spontaneously hypertensive rats. Sci. Rep. 2016, 6, 33855. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Arroyo, F.E.; Tapia, E.; Blas-Marron, M.G.; Gonzaga, G.; Silverio, O.; Cristobal, M.; Osorio, H.; Arellano-Buendia, A.S.; Zazueta, C.; Aparicio-Trejo, O.E.; et al. Vasopressin Mediates the Renal Damage Induced by Limited Fructose Rehydration in Recurrently Dehydrated Rats. Int. J. Biol. Sci. 2017, 13, 961–975. [Google Scholar] [CrossRef] [PubMed]

| Variables | MF < 15 | MF ≥ 15 | ||
|---|---|---|---|---|
| n † | Mean or % (95% CI) ‡ | n † | Mean or % (95% CI) ‡ | |
| Male sex (Yes or No) | 822 | 51.1 (48.8–53.5) | 982 | 53.9 (51.8–55.9) |
| Age (years) | 2076 | 37.1 (36.5–37.8) | 2294 | 45.6 (44.9–46.2) |
| Annual family income | ||||
| High | 657 | 32.4% (29.4–35.6) | 813 | 36.0 (32.8–39.4) |
| Medium high | 661 | 31.5% (28.8–34.3) | 710 | 31.9 (29.1–34.7) |
| Medium low | 578 | 28.0% (25.4–30.8) | 545 | 23.3 (20.8–26.1) |
| Low | 175 | 7.8% (6.4–9.6) | 221 | 8.5 (7.2–10.1) |
| Education | ||||
| More than college | 907 | 44.8 (42.0–47.6) | 830 | 38.9 (36.2–41.6) |
| High school | 860 | 43.2 (40.7–45.9) | 864 | 40.1 (37.7–42.6) |
| Middle school | 153 | 6.4 (5.3–7.6) | 268 | 10.7 (9.2–12.4) |
| Less than elementary school | 154 | 5.5 (4.5–6.7) | 330 | 10.3 (8.9–11.8) |
| Job status (Yes or No) | 1358 | 67.9 (65.5–70.1) | 1526 | 69.1 (66.8–71.3) |
| Marital status | ||||
| Married | 1379 | 60.4 (57.4–63.3) | 1887 | 78.0 (75.7–80.2) |
| Divorce or widowed | 145 | 5.1 (4.2–6.3) | 154 | 5.7 (4.7–6.9) |
| Not married | 549 | 34.3 (31.4–37.4) | 250 | 16.2 (14.2–18.4) |
| Smoking | ||||
| Never | 1235 | 53.2 (50.7–55.7) | 1489 | 58.7 (56.5–60.8) |
| Ex-smoker | 288 | 15.3 (13.6–17.2) | 428 | 20.7 (18.9–22.6) |
| Current | 553 | 31.5 (29.1–34.0) | 377 | 20.6 (18.4–23.0) |
| EuroQol-5D (n) | 2076 | 0.966 (0.963–0.970) | 2294 | 0.964 (0.959–0.968) |
| Systolic BP (mmHg) | 2074 | 113.5 (112.7–114.2) | 2294 | 115.8 (115.0–116.6) |
| Diastolic BP (mmHg) | 2074 | 75.3 (74.8–75.9) | 2294 | 76.2 (75.6–76.7) |
| Waist circumference (cm) | 2076 | 79.9 (79.4–80.4) | 2294 | 80.8 (80.3–81.3) |
| BMI (kg/㎡) | 2076 | 23.7 (23.5–23.9) | 2294 | 23.7 (23.6–23.9) |
| Physical activity (MET-minutes/week) | 2076 | 1884 (1734–2031) | 2294 | 1841 (1702–1981) |
| Serum creatinine (mg/dL) | 2076 | 0.848 (0.835–0.862) | 2294 | 0.850 (0.842–0.859) |
| CKD-EPI eGFR (mL/min/1.73 m2) | 2076 | 102.8 (102.0–103.6) | 2294 | 96.7 (95.9–97.5) |
| Random urine ACR (mg/gCr) | 2076 | 29.7 (12.4–47.0) | 2294 | 19.8 (12.8–26.7) |
| CKD (Yes or No) | 206 | 10.7 (9.2–12.3) | 206 | 8.5 (7.3–9.8) |
| Fasting glucose (mg/dL) | 2076 | 95.2 (94.3–96.0) | 2294 | 98.6 (97.6–99.6) |
| HbA1c (%) | 2076 | 5.598 (5.568–5.629) | 2294 | 5.784 (5.748–5.821) |
| HDL (mg/dL) | 2076 | 51.7 (51.1–52.3) | 2294 | 51.1 (50.5–51.6) |
| LDL (mg/dL) | 2076 | 111.4 (109.8–113.1) | 2294 | 112.5 (111.1–114.0) |
| Hemoglobin (g/dL) | 2076 | 14.36 (14.29–14.43) | 2294 | 14.36 (14.29–14.43) |
| Daily Calorie intake (kcal/day) | 2076 | 2195 (2145–2244) | 2294 | 2199 (2159–2238) |
| Hypertension (Yes or No) | 323 | 14.4 (12.7–16.4) | 582 | 23.8 (21.8–25.9) |
| Diabetes (Yes or No) | 123 | 5.1 (4.2–6.1) | 280 | 11.0 (9.6–12.5) |
| Old Coronary arterial disease (Yes or No) | 16 | 0.6 (0.3–1.0) | 34 | 1.1 (0.8–1.6) |
| Old cerebrovascular accident (Yes or No) | 15 | 0.7 (0.4–1.3) | 38 | 1.3 (0.8–2.0) |
| Dyslipidemia, (Yes or No) | 685 | 33.2 (31.0–35.5) | 880 | 37.4 (35.1–39.7) |
| Variables | Unadjusted OR (95% CI) | Model 1 (95% CI) | Model 2 (95% CI) | Model 3 (95% CI) |
|---|---|---|---|---|
| Meal frequency, <15/week (Ref.: ≥15 times/week) | 1.294 (1.038–1.612) | 1.531 (1.228–1.909) | 1.634 (1.297–2.060) | 1.531 (1.209–1.938) |
| Male gender (Yes or No) | 1.418 (1.128–1.783) | 1.370 (0.942–1.992) | 1.877 (1.229–2.866) | |
| Age (per year) | 1.019 (1.009–1.029) | 1.002 (0.991–1.013) | 0.994 (0.982–1.006) | |
| BMI (Ref.: normal, 18.5–25.0 Kg/m2) | ||||
| Obese (≥25.0 kg/m2) | 1.241 (0.956–1.611) | 1.258 (0.966–1.636) | ||
| Underweight (<18.5 kg/m2) | 1.934 (1.068–3.503) | 2.048 (1.120–3.745) | ||
| Physical activity (Ref.: high, ≥3000) | ||||
| Moderate (600–2999) | 1.250 (0.897–1.742) | 1.234 (0.884–1.722) | ||
| Low (<600) | 1.069 (0.764–1.497) | 1.021 (0.726–1.435) | ||
| Hypertension (Yes or No) | 1.996 (1.498–2.660) | 2.048 (1.536–2.730) | ||
| Diabetes (Yes or No) | 3.210 (2.314–4.451) | 1.924 (1.226–3.020) | ||
| Old CAD (Yes or No) | 1.400 (0.662–2.960) | 1.664 (0.793–3.492) | ||
| Old CVA (Yes or No) | 2.066 (1.128–3.783) | 2.199 (1.204–4.015) | ||
| Smoking (Ref.: never) | ||||
| Ex-smoker | 0.911 (0.607–1.370) | 0.906 (0.603–1.361) | ||
| Current smoker | 0.823 (0.547–1.240) | 0.846 (0.558–1.282) | ||
| Hemoglobin (g/dL) | 0.910 (0.810–1.023) | |||
| Fasting glucose (mg/dL) | 1.011 (1.005–1.017) | |||
| HDL (mg/dL) | 1.004 (0.993–1.015) | |||
| LDL (mg/dL) | 1.003 (1.000–1.007) | |||
| Daily calorie intake (g/day, log transformed) | 0.772 (0.618–0.965) |
| Variables | Unadjusted OR (95% CI) | Model 1 (95% CI) | Model 2 (95% CI) | Model 3 (95% CI) |
|---|---|---|---|---|
| Breakfast (Ref.: 5~7 times/week) | ||||
| 3~4 times/week | 1.106 (0.797–1.535) | 1.288 (0.928–1.788) | 1.353 (0.964–1.900) | 1.339 (0.951–1.885) |
| 1~2 times/week | 1.220 (0.876–1.699) | 1.438 (1.020–2.026) | 1.525 (1.067–2.178) | 1.413 (0.979–2.038) |
| Seldom | 1.360 (0.982–1.882) | 1.562 (1.114–2.191) | 1.695 (1.199–2.397) | 1.572 (1.108–2.231) |
| Male gender (Yes or No) | 1.379 (1.097–1.733) | 1.324 (0.912–1.920) | 1.837 (1.206–2.800) | |
| Age (per year) | 1.018 (1.008–1.029) | 1.001 (0.989–1.013) | 0.993 (0.981–1.006) | |
| BMI (Ref.: normal, 18.5–25.0 kg/m2) | ||||
| Obese (≥25.0 kg/m2) | 1.263 (0.974–1.637) | 1.278 (0.984–1.660) | ||
| Underweight (<18.5 kg/m2) | 1.899 (1.046–3.449) | 2.020 (1.102–3.703) | ||
| Physical activity (Ref.: high, ≥3000) | ||||
| Moderate (600–2999) | 1.242 (0.892–1.730) | 1.225 (0.878–1.708) | ||
| Low (<600) | 1.056 (0.756–1.474) | 1.007 (0.718–1.413) | ||
| Hypertension (Yes or No) | 1.994 (1.494–2.661) | 2.047 (1.533–2.734) | ||
| Diabetes (Yes or No) | 3.194 (2.306–4.423) | 1.913 (1.221–2.997) | ||
| Old CAD (Yes or No) | 1.371 (0.647–2.904) | 1.635 (0.778–3.437) | ||
| Old CVA (Yes or No) | 2.041 (1.112–3.745) | 2.173 (1.190–3.969) | ||
| Smoking (Ref.: never) | ||||
| Ex-smoker | 0.907 (0.605–1.362) | 0.902 (0.601–1.355) | ||
| Current smoker | 0.824 (0.548–1.239) | 0.849 (0.561–1.285) | ||
| Hemoglobin (g/dL) | 0.907 (0.807–1.019) | |||
| Fasting glucose (mg/dL) | 1.011 (1.005–1.017) | |||
| HDL (mg/dL) | 1.004 (0.993–1.015) | |||
| LDL (mg/dL) | 1.003 (1.000–1.007) | |||
| Daily calorie intake (g/day, log transformed) | 0.767 (0.613–0.959) |
| Variables | Unadjusted OR (95% CI) | Model 3 (95% CI) | Daily Calorie Intake (log Transformed) | p for Interaction ‡ | |
|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Model 3 (95% CI) | ||||
| Overall | |||||
| Meal < 15 times/week | 1.294 (1.038–1.612) | 1.531 (1.209–1.938) | 0.810 (0.659–0.996) | 0.772 (0.618–0.965) | 0.539 |
| Breakfast, seldom | 1.360 (0.982–1.882) | 1.572 (1.108–2.231) | 0.767 (0.613–0.959) | 0.502 | |
| Male gender | |||||
| Meal < 15 times/week | 1.229 (0.909–1.661) | 1.703 (1.241–2.336) | 0.712 (0.496–1.023) | 0.869 (0.596–1.265) | 0.621 |
| Breakfast, seldom | 1.388 (0.932–2.066) | 2.049 (1.314–3.195) | 0.880 (0.600–1.291) | 0.551 | |
| Female gender | |||||
| Meal < 15 times/week | 1.424 (1.042–1.945) | 1.294 (0.921–1.817) | 0.657 (0.491–0.880) | 0.673 (0.500–0.905) | 0.430 |
| Breakfast, seldom | 1.221 (0.731–2.039) | 1.036 (0.594–1.808) | 0.663 (0.493–0.891) | 0.246 | |
| Age, under 42 years | |||||
| Meal < 15 times/week | 1.633 (1.099–2.424) | 1.599 (1.066–2.400) † | 0.770 (0.553–1.073) | 0.728 (0.512–1.035) † | 0.987 |
| Breakfast, seldom | 1.391 (0.862–2.245) | 1.409 (0.868–2.286) † | 0.718 (0.506–1.020) † | 0.929 | |
| Age, above 42 years | |||||
| Meal < 15 times/week | 1.333 (1.020–1.743) | 1.593 (1.180–2.149) | 0.914 (0.695–1.202) | 0.830 (0.631–1.091) | 0.177 |
| Breakfast, seldom | 1.776 (1.133–2.784) | 1.976 (1.239–3.152) | 0.823 (0.623–1.088) | 0.842 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.J.; Yoon, J.H.; Choi, H.S.; Kim, C.S.; Bae, E.H.; Ma, S.K.; Kim, S.W. Meal Frequency and Skipping Breakfast Are Associated with Chronic Kidney Disease. Nutrients 2020, 12, 331. https://doi.org/10.3390/nu12020331
Kim YJ, Yoon JH, Choi HS, Kim CS, Bae EH, Ma SK, Kim SW. Meal Frequency and Skipping Breakfast Are Associated with Chronic Kidney Disease. Nutrients. 2020; 12(2):331. https://doi.org/10.3390/nu12020331
Chicago/Turabian StyleKim, Young Jin, Jung Hwan Yoon, Hong Sang Choi, Chang Seong Kim, Eun Hui Bae, Seong Kwon Ma, and Soo Wan Kim. 2020. "Meal Frequency and Skipping Breakfast Are Associated with Chronic Kidney Disease" Nutrients 12, no. 2: 331. https://doi.org/10.3390/nu12020331
APA StyleKim, Y. J., Yoon, J. H., Choi, H. S., Kim, C. S., Bae, E. H., Ma, S. K., & Kim, S. W. (2020). Meal Frequency and Skipping Breakfast Are Associated with Chronic Kidney Disease. Nutrients, 12(2), 331. https://doi.org/10.3390/nu12020331






