Lower Energy Intake among Advanced vs. Early Parkinson’s Disease Patients and Healthy Controls in a Clinical Lunch Setting: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
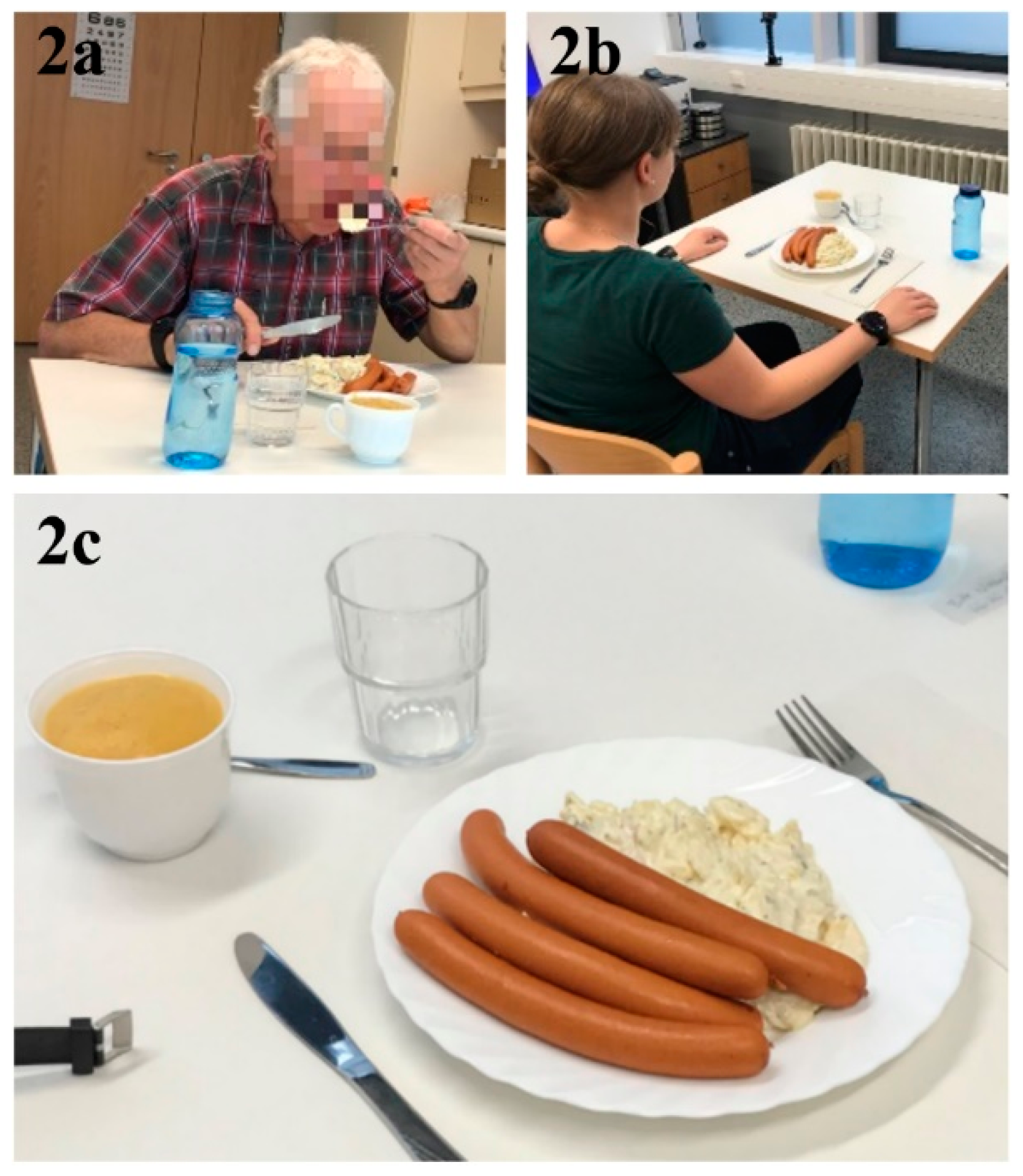
2.2. Setting
2.3. Participants
2.4. The Standardized Meal
2.5. Statistical Methods
2.6. Data Sources/Measurement
2.6.1. Weight and Height
2.6.2. Energy Intake (kcal)
2.6.3. Eating Behaviors
2.6.4. Baseline Characteristics and Parkinson’s Medication
2.6.5. Variables to Assess Motor Symptoms
2.6.6. Variables to Assess Non-Motor Symptoms (NMS)
2.7. Study Size
3. Results
3.1. Group Characteristics
3.2. Primary Outcome: Group Differences in Energy Intake
3.3. Secondary Outcome 1: Exploratory Analysis Explaining Group-Level Differences in Energy Intake
3.4. Secondary Outcome 2: Meal Component Intake Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Chaudhuri, K.R.; Martinez-Martin, P.; Schapira, A.H.V.; Stocchi, F.; Sethi, K.; Odin, P.; Brown, R.G.; Koller, W.; Barone, P.; MacPhee, G.; et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: The NMS Quest study. Mov. Disord. 2006, 21, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Tysnes, O.-B.; Storstein, A. Epidemiology of Parkinson’s disease. J. Neural. Transm. (Vienna) 2017, 124, 901–905. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A.; Visanji, N.P.; Liu, L.W.C.; Lang, A.E.; Pfeiffer, R.F. Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol. 2015, 14, 625–639. [Google Scholar] [CrossRef]
- Haehner, A.; Hummel, T.; Reichmann, H. Olfactory dysfunction as a diagnostic marker for Parkinson’s disease. Expert Rev. Neurother. 2009, 9, 1773–1779. [Google Scholar] [CrossRef]
- Reichmann, H.; Brandt, M.D.; Klingelhoefer, L. The nonmotor features of Parkinson’s disease: Pathophysiology and management advances. Curr. Opin. Neurol. 2016, 29, 467–473. [Google Scholar] [CrossRef]
- Sheard, J.M.; Ash, S.; Silburn, P.A.; Kerr, G.K. Prevalence of malnutrition in Parkinson’s disease: A systematic review. Nutr. Rev. 2011, 69, 520–532. [Google Scholar] [CrossRef]
- Athlin, E.; Norberg, A.; Axelsson, K.; Möller, A.; Nordström, G. Aberrant eating behavior in elderly parkinsonian patients with and without dementia: Analysis of video-recorded meals. Res. Nurs. Health 1989, 12, 41–51. [Google Scholar] [CrossRef]
- Abbott, R.A.; Cox, M.; Markus, H.; Tomkins, A. Diet, body size and micronutrient status in Parkinson’s disease. Eur. J. Clin. Nutr. 1992, 46, 879–884. [Google Scholar]
- Ma, K.; Xiong, N.; Shen, Y.; Han, C.; Liu, L.; Zhang, G.; Wang, L.; Guo, S.; Guo, X.; Xia, Y.; et al. Weight loss and malnutrition in patients with parkinson’s disease: Current knowledge and future prospects. Front. Aging Neurosci. 2018, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Lesourd, B.M. Nutrition and immunity in the elderly: Modification of immune responses with nutritional treatments. Am. J. Clin. Nutr. 1997, 66, 478S–484S. [Google Scholar] [CrossRef]
- Lorefält, B.; Toss, G.; Granérus, A.-K. Bone mass in elderly patients with Parkinson’s disease. Acta Neurol. Scand. 2007, 116, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, K.; Kadota, J.; Iida, K.; Shirai, R.; Abe, K.; Kohno, S. Reduced immune function and malnutrition in the elderly. Tohoku J. Exp. Med. 1999, 187, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.C.; Vassallo, M. Prognostic significance of weight changes in Parkinson’s disease: The Park-weight phenotype. Neurodegener. Dis. Manag. 2014, 4, 309–316. [Google Scholar] [CrossRef]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Kurtis, M.M.; Chaudhuri, K.R.; NMSS validation group. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov. Disord. 2011, 26, 399–406. [Google Scholar] [CrossRef]
- Steinhardt, J.; Münte, T.F.; Schmid, S.M.; Wilms, B.; Brüggemann, N. A systematic review of body mass gain after deep brain stimulation of the subthalamic nucleus in patients with Parkinson’s disease. Obes. Rev. 2019. [Google Scholar] [CrossRef]
- Kistner, A.; Lhommée, E.; Krack, P. Mechanisms of body weight fluctuations in Parkinson’s disease. Front. Neurol. 2014, 5. [Google Scholar] [CrossRef]
- Bachmann, C.G.; Zapf, A.; Brunner, E.; Trenkwalder, C. Dopaminergic treatment is associated with decreased body weight in patients with Parkinson’s disease and dyskinesias. Eur. J. Neurol. 2009, 16, 895–901. [Google Scholar] [CrossRef]
- Cersosimo, M.G.; Raina, G.B.; Pellene, L.A.; Micheli, F.E.; Calandra, C.R.; Maiola, R. Weight loss in Parkinson’s disease: The relationship with motor symptoms and disease progression. Biomed. Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Wang, L.; Xiong, N.; Huang, J.; Guo, S.; Liu, L.; Han, C.; Zhang, G.; Jiang, H.; Ma, K.; Xia, Y.; et al. Protein-restricted diets for ameliorating motor fluctuations in Parkinson’s disease. Front. Aging Neurosci. 2017, 9. [Google Scholar] [CrossRef]
- Barichella, M.; Cereda, E.; Cassani, E.; Pinelli, G.; Iorio, L.; Ferri, V.; Privitera, G.; Pasqua, M.; Valentino, A.; Monajemi, F.; et al. Dietary habits and neurological features of Parkinson’s disease patients: Implications for practice. Clin. Nutr. 2017, 36, 1054–1061. [Google Scholar] [CrossRef]
- Hall, K.D.; Sacks, G.; Chandramohan, D.; Chow, C.C.; Wang, Y.C.; Gortmaker, S.L.; Swinburn, B.A. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011, 378, 826–837. [Google Scholar] [CrossRef]
- Markus, H.S.; Cox, M.; Tomkins, A.M. Raised resting energy expenditure in Parkinson’s disease and its relationship to muscle rigidity. Clin. Sci. 1992, 83, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Levi, S.; Cox, M.; Lugon, M.; Hodkinson, M.; Tomkins, A. Increased energy expenditure in Parkinson’s disease. BMJ 1990, 301, 1256–1257. [Google Scholar] [CrossRef] [PubMed]
- Toth, M.J.; Fishman, P.S.; Poehlman, E.T. Free-living daily energy expenditure in patients with Parkinson’s disease. Neurology 1997, 48, 88–91. [Google Scholar] [CrossRef]
- Dhurandhar, N.V.; Schoeller, D.; Brown, A.W.; Heymsfield, S.B.; Thomas, D.; Sørensen, T.I.A.; Speakman, J.R.; Jeansonne, M.; Allison, D.B. Energy balance measurement working group energy balance measurement: When something is not better than nothing. Int. J. Obes. (Lond) 2015, 39, 1109–1113. [Google Scholar] [CrossRef]
- Klingelhoefer, L.; Reichmann, H. Dementia—The real problem for patients with Parkinson’s disease. Basal Ganglia 2014, 4, 9–13. [Google Scholar] [CrossRef]
- Titova, N.; Padmakumar, C.; Lewis, S.J.G.; Chaudhuri, K.R. Parkinson’s: A syndrome rather than a disease? J. Neural. Transm. (Vienna) 2017, 124, 907–914. [Google Scholar] [CrossRef]
- Sauerbier, A.; Jenner, P.; Todorova, A.; Chaudhuri, K.R. Non motor subtypes and Parkinson’s disease. Parkinsonism Relat. Disord. 2016, 22, S41–S46. [Google Scholar] [CrossRef]
- Erro, R.; Vitale, C.; Amboni, M.; Picillo, M.; Moccia, M.; Longo, K.; Santangelo, G.; De Rosa, A.; Allocca, R.; Giordano, F.; et al. The Heterogeneity of early Parkinson’s disease: A cluster analysis on newly diagnosed untreated patients. PLoS ONE 2013, 8, e70244. [Google Scholar] [CrossRef]
- Hughes, A.J.; Daniel, S.E.; Kilford, L.; Lees, A.J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 1992, 55, 181–184. [Google Scholar] [CrossRef] [PubMed]
- The World Medical Association. WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 15 July 2020).
- GoPro. The World’s Most Versatile Action Cameras. Available online: https://gopro.com/en/us/ (accessed on 7 February 2020).
- Kyritsis, K.; Diou, C.; Delopoulos, A. Modeling wrist micromovements to measure in-meal eating behavior from inertial sensor data. IEEE J. Biomed. Health Inform. 2019, 23, 2325–2334. [Google Scholar] [CrossRef] [PubMed]
- Kyritsis, K.; Diou, C.; Delopoulos, A. A data driven end-to-end approach for in-the-wild monitoring of eating behavior using smartwatches. IEEE J. Biomed. Health Inform. 2020. [Google Scholar] [CrossRef]
- Fagerberg, P.; Langlet, B.; Glossner, A.; Ioakimidis, I. Food intake during school lunch is better explained by objectively measured eating behaviors than by subjectively rated food taste and fullness: A cross-sectional study. Nutrients 2019, 11, 597. [Google Scholar] [CrossRef]
- Ioakimidis, I.; Zandian, M.; Eriksson-Marklund, L.; Bergh, C.; Grigoriadis, A.; Södersten, P. Description of chewing and food intake over the course of a meal. Physiol. Behav. 2011, 104, 761–769. [Google Scholar] [CrossRef]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef]
- Fahn, S.; David, C.M.; Peter, J. Recent Developments in Parkinson’s Disease; Raven Press: New York, NY, USA, 1986; ISBN 978-0-88167-132-2. [Google Scholar]
- Guy, W. ECDEU Assessment Manual for Psychopharmacology; U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs: Rockville, MD, USA, 1976. [Google Scholar]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef]
- Yamauchi, Y.; Endo, S.; Sakai, F.; Yoshimura, I. A new whole-mouth gustatory test procedure. 1. Thresholds and principal components analysis in healthy men and women. Acta Otolaryngol. Suppl. 2002, 39–48. [Google Scholar] [CrossRef]
- Hummel, T.; Sekinger, B.; Wolf, S.R.; Pauli, E.; Kobal, G. “Sniffin’ sticks”: Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem. Senses 1997, 22, 39–52. [Google Scholar] [CrossRef]
- Hummel, T.; Kobal, G.; Gudziol, H.; Mackay-Sim, A. Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: An upgrade based on a group of more than 3000 subjects. Eur. Arch. Otorhinolaryngol. 2007, 264, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Suiter, D.M.; Leder, S.B. Clinical utility of the 3-ounce water swallow test. Dysphagia 2008, 23, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Leder, S.B.; Suiter, D.M.; Green, B.G. Silent aspiration risk is volume-dependent. Dysphagia 2011, 26, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Hughes, T.A.; Wiles, C.M. Neurogenic dysphagia: The role of the neurologist. J. Neurol. Neurosurg. Psychiatry 1998, 64, 569–572. [Google Scholar] [CrossRef]
- Prosiegel, M.; Weber, S. Dysphagie: Diagnostik und Therapie: Ein Wegweiser für kompetentes Handeln; Springer: Berlin, Germany, 2013; ISBN 978-3-642-35104-4. [Google Scholar]
- Diener, H.-C. Leitlinien für Diagnostik und Therapie in der Neurologie; Thieme: Stuttgart, Germany, 2012; ISBN 978-3-13-132415-3. [Google Scholar]
- Höglinger, G.U.; Respondek, G.; Stamelou, M.; Kurz, C.; Josephs, K.A.; Lang, A.E.; Mollenhauer, B.; Müller, U.; Nilsson, C.; Whitwell, J.L.; et al. Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov. Disord. 2017, 32, 853–864. [Google Scholar] [CrossRef]
- Hawkes, C.H.; Del Tredici, K.; Braak, H. A timeline for Parkinson’s disease. Parkinsonism Relat. Disord. 2010, 16, 79–84. [Google Scholar] [CrossRef]
- Olanow, C.W.; Watts, R.L.; Koller, W.C. An algorithm (decision tree) for the management of Parkinson’s disease (2001): Treatment guidelines. Neurology 2001, 56, S1–S88. [Google Scholar] [CrossRef]
- Antonini, A.; Stoessl, A.J.; Kleinman, L.S.; Skalicky, A.M.; Marshall, T.S.; Sail, K.R.; Onuk, K.; Odin, P.L.A. Developing consensus among movement disorder specialists on clinical indicators for identification and management of advanced Parkinson’s disease: A multi-country Delphi-panel approach. Curr. Med. Res. Opin. 2018, 34, 2063–2073. [Google Scholar] [CrossRef]
- Stocchi, F.; Jenner, P.; Obeso, J.A. When do levodopa motor fluctuations first appear in Parkinson’s disease? Eur. Neurol. 2010, 63, 257–266. [Google Scholar] [CrossRef]
- Luquin, M.-R.; Kulisevsky, J.; Martinez-Martin, P.; Mir, P.; Tolosa, E.S. Consensus on the definition of advanced Parkinson’s disease: A neurologists-based Delphi study (CEPA study). Parkinsons. Dis. 2017, 2017, 4047392. [Google Scholar] [CrossRef]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-processed diets cause excess calorie intake and weight gain: An inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019, 30, 67–77.e3. [Google Scholar] [CrossRef] [PubMed]
- Kyritsis, K.; Diou, C.; Delopoulos, A. Detecting meals in the wild using the inertial data of a typical smartwatch. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 4229–4232. [Google Scholar]
- Kyritsis, K.; Fagerberg, P.; Ioakimidis, I.; Klingelhoefer, L.; Reichmann, H.; Delopoulos, A. Using imu sensors to assess motor degradation of pd patients by modeling in-meal plate-to-mouth movement elongation. Eng. Med. Biol. Conf. 2020. [Google Scholar]
- Konstantinidis, D.; Dimitropoulos, K.; Langlet, B.; Daras, P.; Ioakimidis, I. Validation of a deep learning system for the full automation of bite and meal duration analysis of experimental meal videos. Nutrients 2020, 12, 209. [Google Scholar] [CrossRef] [PubMed]
- Hermsen, S.; Mars, M.; Higgs, S.; Frost, J.H.; Hermans, R.C.J. Effects of eating with an augmented fork with vibrotactile feedback on eating rate and body weight: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 90. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, N.; Zheng, Z.K. Design and validation of a tremor stabilizing handle for patients with parkinson disease and essential tremor. In Proceedings of the Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management; Duffy, V.G., Ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 274–283. [Google Scholar]
- Dias, S.B.; Konstantinidis, E.; Diniz, J.A.; Bamidis, P.; Charisis, V.; Hadjidimitriou, S.; Stadtschnitzer, M.; Fagerberg, P.; Ioakeimidis, I.; Dimitropoulos, K.; et al. Serious games as a means for holistically supporting Parkinson’s disease patients: The i-prognosis personalized game suite framework. In Proceedings of the 2017 9th International Conference on Virtual Worlds and Games for Serious Applications (VS-Games), Athens, Greece, 6–8 September 2017; pp. 237–244. [Google Scholar]
- Chen, H.; Zhang, S.M.; Hernán, M.A.; Willett, W.C.; Ascherio, A. Weight loss in Parkinson’s disease. Ann. Neurol. 2003, 53, 676–679. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.C.; Turton, J. Olfaction, dyskinesia and profile of weight change in Parkinson’s disease: Identifying neurodegenerative phenotypes. Parkinsonism Relat. Disord. 2012, 18, 964–970. [Google Scholar] [CrossRef]
- Lorefält, B.; Granérus, A.-K.; Unosson, M. Avoidance of solid food in weight losing older patients with Parkinson’s disease. J. Clin. Nurs. 2006, 15, 1404–1412. [Google Scholar] [CrossRef] [PubMed]
- Klingelhoefer, L.; Reichmann, H. Pathogenesis of Parkinson disease—The gut-brain axis and environmental factors. Nat. Rev. Neurol. 2015, 11, 625–636. [Google Scholar] [CrossRef]
- Pedrosa Carrasco, A.J.; Timmermann, L.; Pedrosa, D.J. Management of constipation in patients with Parkinson’s disease. NPJ Parkinsons. Dis. 2018, 4. [Google Scholar] [CrossRef]
- Klingelhoefer, L.; Reichmann, H. Parkinson’s disease and gastrointestinal non motor symptoms: Diagnostic and therapeutic options—A practise guide. J. Parkinsons. Dis. 2015, 5, 647–658. [Google Scholar] [CrossRef]
- Lean, K.; Nawaz, R.F.; Jawad, S.; Vincent, C. Reducing urinary tract infections in care homes by improving hydration. BMJ Open Qual. 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, A.; Baba, T.; Hasegawa, T.; Kobayashi, M.; Sugeno, N.; Konno, M.; Miura, E.; Hosokai, Y.; Ishioka, T.; Nishio, Y.; et al. Hypometabolism in the supplementary and anterior cingulate cortices is related to dysphagia in Parkinson’s disease: A cross-sectional and 3-year longitudinal cohort study. BMJ Open 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Langlet, B.; Tang Bach, M.; Odegi, D.; Fagerberg, P.; Ioakimidis, I. The effect of food unit sizes and meal serving occasions on eating behaviour characteristics: Within person randomised crossover studies on healthy women. Nutrients 2018, 10, 880. [Google Scholar] [CrossRef] [PubMed]
- Sheen, F.; Hardman, C.A.; Robinson, E. Plate-clearing tendencies and portion size are independently associated with main meal food intake in women: A laboratory study. Appetite 2018, 127, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Uc, E.Y.; Struck, L.K.; Rodnitzky, R.L.; Zimmerman, B.; Dobson, J.; Evans, W.J. Predictors of weight loss in Parkinson’s disease. Mov. Disord. 2006, 21, 930–936. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.C.; Macnamara, L.; Hasoon, M.; Vassallo, M.; Ross, I. Cascade of levodopa dose and weight-related dyskinesia in Parkinson’s disease (LD-WD-PD cascade). Parkinsonism Relat. Disord. 2006, 12, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.C.; Ross, I.N.; Rascol, O.; Brooks, D. Relationship between weight, levodopa and dyskinesia: The significance of levodopa dose per kilogram body weight. Eur. J. Neurol. 2008, 15, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Rolls, B.J.; Fedoroff, I.C.; Guthrie, J.F. Gender differences in eating behavior and body weight regulation. Health Psychol. 1991, 10, 133–142. [Google Scholar] [CrossRef] [PubMed]



| Potato Salad | Sausages | Apple Puree | |
|---|---|---|---|
| Protein, g | 2.0 | 14 | <0.5 |
| Carbohydrate, g | 11 | 1.2 | 18 |
| Sugars, g | 1.2 | <0.5 | 18 |
| Fat, g | 9.4 | 26 | <0.5 |
| Energy, kcal | 140 | 295 | 84 |
| Healthy Controls | Early PD | Advanced PD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Females (n = 14) | Males (n = 9) | Total (n = 23) | Females (n = 7) | Males (n = 13) | Total (n = 20) | Females (n = 8) | Males (n = 13) | Total (n = 21) | |
| General characteristics | |||||||||
| Age, years | 61.2 (7.3) | 64.4 (8.4) | 62.5 (7.7) | 62.4 (4.6) | 59.9 (9.9) | 60.8 (8.3) | 64.0 (6.6) | 64.0 (8.2) | 64.0 (7.5) |
| Bodyweight, kg | 70.3 (9.0) | 87.0 (15.1) | 76.8 (14.1) | 79.5 (17.1) | 86.2 (13.0) | 83.8 (14.5) | 76.6 (14.4) | 85.8 (14.1) | 82.3 (14.6) |
| Height, m | 1.65 (0.06) | 1.79 (0.09) | 1.70 (0.10) | 1.67 (0.06) | 1.78 (0.06) | 1.74 (0.08) | 1.62 (0.06) | 1.78 (0.08) | 1.72 (0.11) |
| BMI, kg/m2 | 25.6 (3.4) | 27.1 (3.6) | 26.2 (3.5) | 28.3 (6.9) | 27.3 (4.3) | 27.6 (5.2) | 29.1 (5.4) | 27.0 (3.5) | 27.8 (4.3) |
| PD Status | |||||||||
| H&Y stage | 1.4 (0.9) | 1.3 (0.9) | 1.3 (0.9) | 1.9 (0.4) | 2.0 (0.0) | 2.0 (0.2) NA | 2.5 (0.8) | 2.2 (0.4) | 2.3 (0.6) NA |
| Disease duration | 0 (0) | 0 (0) | 0 (0) | 3.6 (1.5) | 2.9 (2.0) | 3.1 (1.8) NA | 10.9 (4.1) | 12.9 (4.9) | 12.1 (4.6) NA |
| PD Medications | |||||||||
| Levodopa Equivalent Daily Dose (mg/d) | 0 (0) | 0 (0) | 0 (0) | 431 (176) | 578 (279) | 527 (253) † | 1216 (525) | 1059 (559) | 1119 (538) *,† |
| Daily Levodopa dose (mg/d)/kg bodyweight | 0 (0) | 0 (0) | 0 (0) | 1.3 (1.7) | 2.8 (2.6) | 2.3 (2.4) † | 9.0 (4.5) | 6.0 (3.0) | 7.2 (3.9) *,† |
| Daily Levodopa Dose (mg/d) | 0 (0) | 0 (0) | 0 (0) | 107 (143) | 245 (222) | 197 (206) † | 669 (322) | 527 (282) | 581 (298) *,† |
| Motor features of PD | |||||||||
| Tremor UE | 0.1 (0.3) | 0.9 (1.1) | 0.4 (0.8) | 1.9 (1.6) | 1.8 (1.6) | 1.8 (1.5) † | 1.5 (1.2) | 2.5 (1.5) | 2.1 (1.4) † |
| Brady/Hypokinesia UE | 1.8 (1.4) | 0.7 (1.0) | 1.3 (1.3) | 6.3 (3.5) | 5.4 (2.0) | 5.7 (2.6) † | 6.1 (2.5) | 8.7 (4.0) | 7.7 (3.6) *,† |
| Rigidity UE | 0 (0) | 0 (0) | 0 (0) | 2.0 (1.5) | 2.3 (2.1) | 2.2 (1.9) † | 1.3 (0.7) | 1.5 (1.7) | 1.4 (1.4) † |
| Non motor features of PD | |||||||||
| Taste problems, N (%) | 2 (14.3) | 0 (0) | 2 (8.7) | 0 (0) | 2 (15.4) | 2 (10) | 0 (0) | 6 (46.2) | 6 (28.6) |
| Smell problems, N (%) | 3 (21.4) | 2 (22.2) | 5 (21.7) | 6 (85.7) | 13 (100) | 19 (95) † | 7 (88.8) | 13 (100) | 20 (95.2) † |
| Eating problems, N (%) | 2 (14.3) | 1 (11.1) | 3 (13) | 1 (14.3) | 3 (23.1) | 4 (20) | 3 (37.5) | 5 (41.7) | 8 (40) |
| Dysphagia, N (%) | 1 (7.1) | 1 (11.1) | 2 (8.7) | 0 (0) | 2 (15.4) | 2 (10) | 3 (37.5) | 5 (38.5) | 8 (38.1) † |
| Has depression diagnosis, N (%) | 5 (35.7) | 2 (22) | 7 (30.4) | 2 (28.6) | 3 (25.0) | 5 (26.3) | 2 (25.0) | 3 (23.1) | 5 (23.8) |
| Has constipation, N (%) | 0 (0) | 1 (11.1) | 1 (4.5) | 1 (14.3) | 2 (20.0) | 3 (17.6) | 1 (14.3) | 7 (53.8) | 8 (40) † |
| Primary Outcome Models | B | t | p | Lower Bound 95% Confidence Interval for B | Upper Bound 95% Confidence Interval for B |
|---|---|---|---|---|---|
| 1 * | |||||
| Sex | 297.729 | 5.738 | 0.000 | 193.862 | 401.596 |
| Early PD | 40.651 | 0.651 | 0.517 | −84.269 | 165.571 |
| Advanced PD | −162.063 | −2.623 | 0.011 | −285.731 | −38.394 |
| 2 * | |||||
| Sex | 297.729 | 5.738 | 0.000 | 193.862 | 401.596 |
| Healthy control | −40.651 | −0.651 | 0.517 | −165.571 | 84.269 |
| Advanced PD | −202.713 | −3.208 | 0.002 | −329.214 | −76.213 |
| Healthy Controls | Early PD | Advanced PD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Females (n = 14) | Males (n = 9) | Total (n = 23) | Females (n = 7) | Males (n = 13) | Total (n = 20) | Females (n = 8) | Males (n = 13) | Total (n = 21) | ||
| Meal component intake | ||||||||||
| Potato salad intake (g) | 214 (97) | 320 (71) | 255 (101) | 209 (63) | 339 (80) | 291 (97) | 161 (81) | 269 (67) | 232 (88) *,† | |
| Sausage intake (g) | 114 (25) | 171 (42) | 136 (42) | 123 (26) | 166 (40) | 150 (41) | 88 (21) | 138 (38) | 120 (41) *,† | |
| Apple mash intake (g) | 166 (54) | 142 (74) | 157 (63) | 187 (21) | 180 (35) | 183 (30) | 151 (46) | 153 (46) | 152 (45) | |
| Water intake (g) | 160 (113) | 172 (69) | 165 (97) | 147 (63) | 131 (49) | 137 (54) | 73 (48) | 95 (85) | 87 (73) † | |
| Eating behaviors | ||||||||||
| Energy eating rate (kcal/min) | 77 (21) | 94 (17) | 83 (21) | 80 (12) | 83 (26) | 82 (22) | 76 (23) | 82 (20) | 80 (21) | |
| Eating rate (g/min) | 49 (13) | 55 (10) | 51 (12) | 51 (7) | 51 (15) | 51 (13) | 49 (14) | 50 (13) | 50 (13) | |
| Meal duration (min) | 10.3 (2.1) | 11.5 (2.3) | 10.8 (2.2) | 10.2 (0.6) | 13.8 (4.7) | 12.5 (4.1) | 9.3 (3.2) | 12.1 (4.7) | 11.0 (4.4) | |
| Number of spoonfuls | 51 (12) | 59 (13) | 54 (13) | 49 (7) | 61 (17) | 57 (15) | 41 (8) | 56 (17) | 50 (16) * | |
| Number of chews | 543 (215) | 686 (202) | 599 (218) | 475 (75) | 903 (458) | 753 (422) | 448 (132) | 828 (475) | 683 (421) | |
| Chews/g of food eaten | 1.2 (0.7) | 1.1 (.4) | 1.2 (.6) | 0.9 (0.3) | 1.4 (0.6) | 1.2 (0.5) | 1.1 (0.5) | 1.5 (0.8) | 1.3 (0.7) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fagerberg, P.; Klingelhoefer, L.; Bottai, M.; Langlet, B.; Kyritsis, K.; Rotter, E.; Reichmann, H.; Falkenburger, B.; Delopoulos, A.; Ioakimidis, I. Lower Energy Intake among Advanced vs. Early Parkinson’s Disease Patients and Healthy Controls in a Clinical Lunch Setting: A Cross-Sectional Study. Nutrients 2020, 12, 2109. https://doi.org/10.3390/nu12072109
Fagerberg P, Klingelhoefer L, Bottai M, Langlet B, Kyritsis K, Rotter E, Reichmann H, Falkenburger B, Delopoulos A, Ioakimidis I. Lower Energy Intake among Advanced vs. Early Parkinson’s Disease Patients and Healthy Controls in a Clinical Lunch Setting: A Cross-Sectional Study. Nutrients. 2020; 12(7):2109. https://doi.org/10.3390/nu12072109
Chicago/Turabian StyleFagerberg, Petter, Lisa Klingelhoefer, Matteo Bottai, Billy Langlet, Konstantinos Kyritsis, Eva Rotter, Heinz Reichmann, Björn Falkenburger, Anastasios Delopoulos, and Ioannis Ioakimidis. 2020. "Lower Energy Intake among Advanced vs. Early Parkinson’s Disease Patients and Healthy Controls in a Clinical Lunch Setting: A Cross-Sectional Study" Nutrients 12, no. 7: 2109. https://doi.org/10.3390/nu12072109
APA StyleFagerberg, P., Klingelhoefer, L., Bottai, M., Langlet, B., Kyritsis, K., Rotter, E., Reichmann, H., Falkenburger, B., Delopoulos, A., & Ioakimidis, I. (2020). Lower Energy Intake among Advanced vs. Early Parkinson’s Disease Patients and Healthy Controls in a Clinical Lunch Setting: A Cross-Sectional Study. Nutrients, 12(7), 2109. https://doi.org/10.3390/nu12072109







