Where Do Adolescents Eat Less-Healthy Foods? Correspondence Analysis and Logistic Regression Results from the UK National Diet and Nutrition Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. The NDNS-RP 2008–2012 Sample
2.2. Dietary Data
2.3. Classification of Food Groups and Locations
2.4. Statistical Analysis
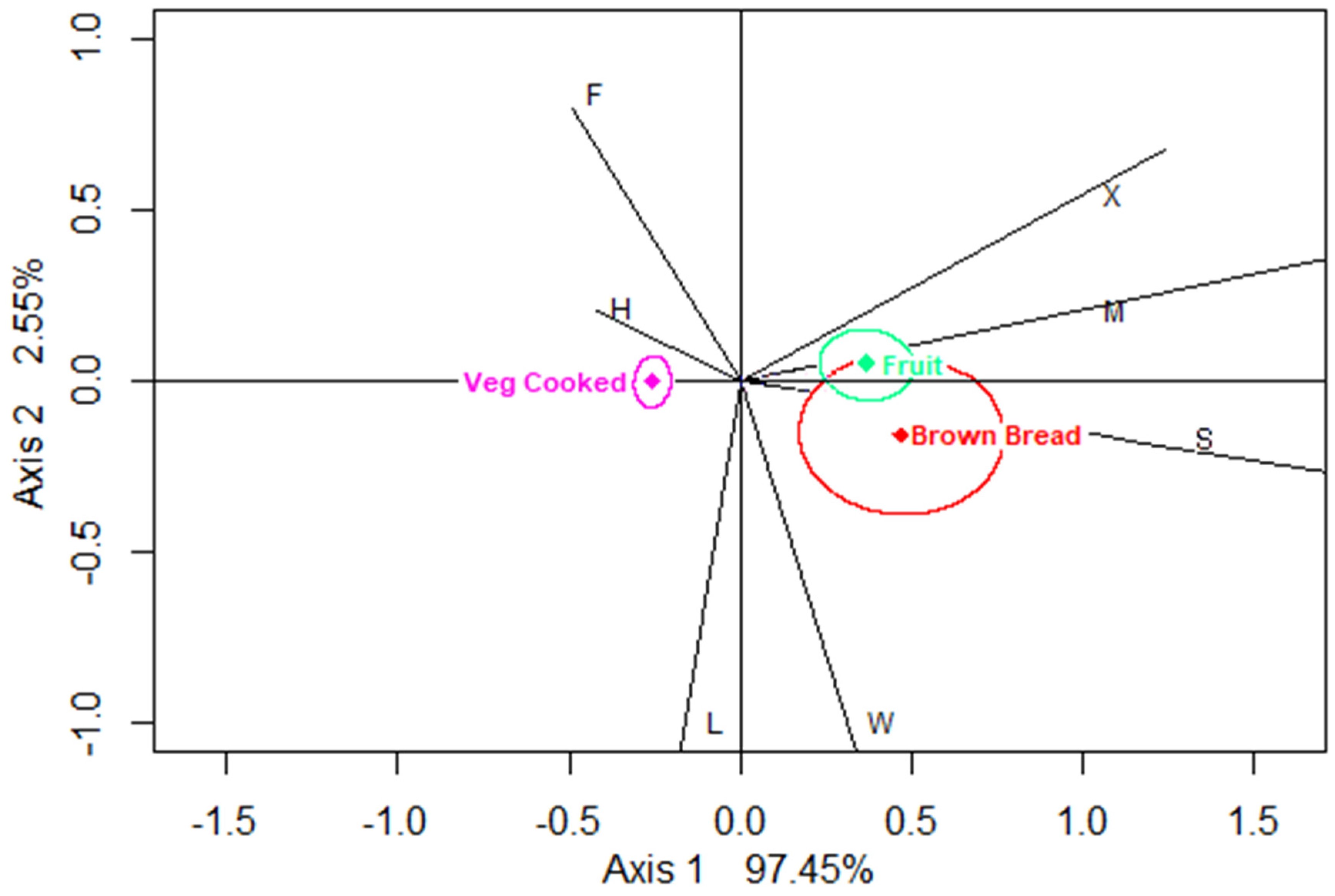
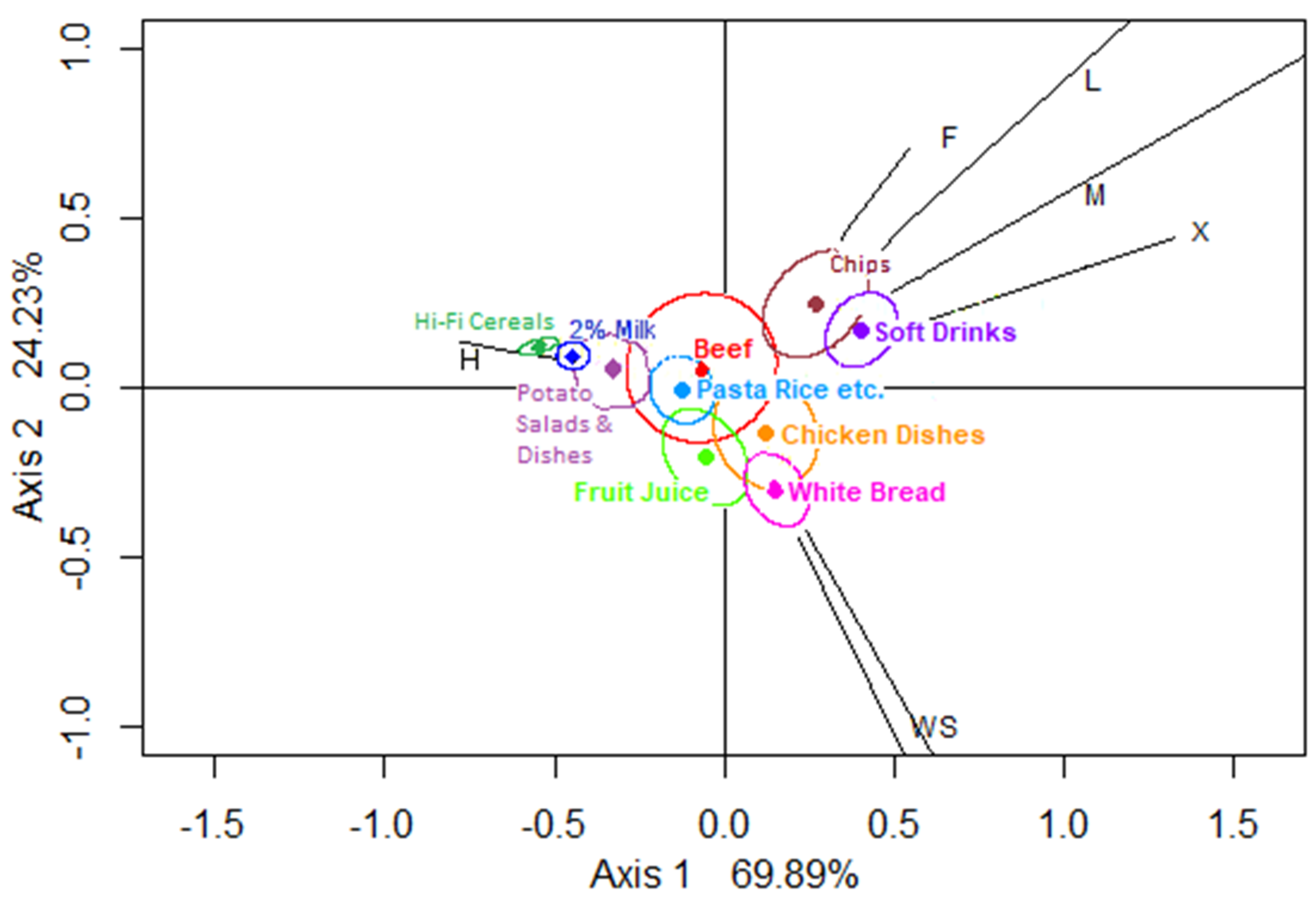
2.4.1. Step 1: Correspondence Analysis (CA)
2.4.2. Step 2: Logistic Regression with GEE
3. Results
3.1. Study Sample
3.2. Results from Correspondence Analysis (Step 1)
3.3. Overall Summary of Data Mining for Associations by Correspondence Analysis
3.4. Results of Logistic Regression Analyses (Step 2)
4. Discussion
4.1. Strengths and Weaknesses of the Study
4.2. Comparison with Previous Studies
4.3. Interpretation of the Findings and Implications for Public Health Policy
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; Naghavi, M.; et al. Health effects of overweight and obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [PubMed]
- Scarborough, P.; Rayner, M.; Stockley, L.; Black, A. Nutrition professionals’ perception of the “healthiness” of individual foods. Public Health Nutr. 2007, 10, 346–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, L.; Mander, A.; Jones, L.R.; Emmett, P.M.; A Jebb, S. Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. Am. J. Clin. Nutr. 2008, 87, 846–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NatCen Social Research. National Diet and Nutrition Survey Years 1 to 9 of the Rolling Programme (2008/2009–2016/2017): Time Trend and Income Analyses; NatCen Social Research: London, UK, 2019. [Google Scholar]
- Ambrosini, G.L.; Oddy, W.H.; Huang, R.C.; Mori, T.A.; Beilin, L.J.; Jebb, S.A. Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. Am. J. Clin. Nutr. 2013, 98, 327–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weichselbaum, E.; Buttriss, J.L. Diet, nutrition and schoolchildren: An update. Nutr. Bull. 2014, 39, 9–73. [Google Scholar] [CrossRef]
- Goffe, L.; Rushton, S.; White, M.; Adamson, A.; Adams, J. Relationship between mean daily energy intake and frequency of consumption of out-of-home meals in the UK National Diet and Nutrition Survey. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 131. [Google Scholar] [CrossRef]
- Burgoine, T.; Sarkar, C.; Webster, C.; Monsivais, P. Examining the interaction of fast-food outlet exposure and income on diet and obesity: Evidence from 51,361 UK Biobank participants. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 71. [Google Scholar] [CrossRef] [Green Version]
- Adams, J.; Goffe, L.; Brown, T.; Lake, A.A.; Summerbell, C.D.; White, M.; Wrieden, W.; Adamson, A. Frequency and socio-demographic correlates of eating meals out and take-away meals at home: Cross-sectional analysis of the UK national diet and nutrition survey, waves 1–4 (2008–12). Int. J. Behav. Nutr. Phys. Act. 2015, 12, 51. [Google Scholar] [CrossRef] [Green Version]
- Patterson, R.; Risby, A.; Chan, M.-Y. Consumption of takeaway and fast food in a deprived inner London Borough: Are they associated with childhood obesity? BMJ Open 2012, 2, e000402. [Google Scholar] [CrossRef] [Green Version]
- Venn, A.J.; Thomson, R.J.; Schmidt, M.D.; Cleland, V.J.; Curry, B.A.; Gennat, H.C.; Dwyer, T. Overweight and obesity from childhood to adulthood: A follow-up of participants in the 1985 Australian Schools Health and Fitness Survey. Med. J. Aust. 2007, 186, 458–460. [Google Scholar] [CrossRef]
- OECD—Organisation for Economic Co-operation and Development Obesity Update 2017. Available online: www.oecd.org/health/obesity-update.htm (accessed on 7 July 2020).
- Department of Health—Healthy Lives, Healthy People. Available online: https://www.gov.uk/government/publications/healthy-lives-healthy-people-our-strategy-for-public-health-in-england (accessed on 7 July 2020).
- Yang, W.; Kelly, T.; He, J. The Genetic Epidemiology of Obesity. Epidemiol. Rev. 2007, 29, 49–61. [Google Scholar] [CrossRef]
- Langenberg, C.; Sharp, S.J.; Franks, P.W.; Scott, R.A.; Deloukas, P.; Forouhi, N.G.; Froguel, P.; Groop, L.C.; Hansen, T.; Palla, L.; et al. Gene-lifestyle interaction and type 2 diabetes: The EPIC interact case-cohort study. PLoS Med. 2014, 11, e1001647. [Google Scholar] [CrossRef] [Green Version]
- Brownson, R.C.; Haire-Joshu, D.; Luke, D. Shaping the context of health: A review of environmental and policy approaches in the prevention of chronic diseases. Annu. Rev. Public Health 2006, 27, 341–370. [Google Scholar] [CrossRef] [Green Version]
- Allender, S. Policy change to create supportive environments for physical activity and healthy eating: Which options are the most realistic for local government? Health Promot. Int. 2012, 27, 261–274. [Google Scholar] [CrossRef] [Green Version]
- Ziauddeen, N.; Page, P.; Penney, T.L.; Nicholson, S.; Kirk, S.F.; Almiron-Roig, E. Eating at food outlets and leisure places and “on the go” is associated with less-healthy food choices than eating at home and in school in children: Cross-sectional data from the UK National Diet and Nutrition Survey Rolling Program (2008-2014). Am. J. Clin. Nutr. 2018, 107, 992–1003. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Nguyen, B.T. Fast-food and full-service restaurant consumption among children and adolescents: Effect on energy, beverage, and nutrient intake. Arch. Pediatr. Adolesc. Med. 2013, 167, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Penney, T.; Almiron-Roig, E.; Shearer, C.; McIsaac, J.-L.; Kirk, S.F. Modifying the food environment for childhood obesity prevention: Challenges and opportunities. Proc. Nutr. Soc. 2014, 73, 226–236. [Google Scholar] [CrossRef] [Green Version]
- National Health Service. Home-Change4Life. NHS. Published 2009. Available online: https://www.nhs.uk/change4life (accessed on 7 July 2020).
- Poti, J.M.; Slining, M.; Popkin, B.M.; Kenan, W. Where are kids getting their empty calories? Stores, schools, and fast-food restaurants each played an important role in empty calorie intake among US children during 2009–2010. J. Acad. Nutr. Diet. 2014, 114, 908–917. [Google Scholar] [CrossRef] [Green Version]
- Tyrrell-Smith, R.; Greenhalgh, F.; Hodgson, S.; Wills, W.J.; Mathers, J.C.; Adamson, A.J.; Lake, A. Food environments of young people: Linking individual behaviour to environmental context. J. Public Health 2017, 39, 95–104. [Google Scholar]
- Müller, K.; Libuda, L.; Diethelm, K.; Huybrechts, I.; Moreno, L.A.; Manios, Y.; Mistura, L.; Dallongeville, J.; Kafatos, A.; González-Gross, M.; et al. Lunch at school, at home or elsewhere: Where do adolescents usually get it and what do they eat? Results of the HELENA study. Appetite 2013, 71, 332–339. [Google Scholar] [CrossRef]
- Tugault-Lafleur, C.N.; Black, J.L. Lunch on School Days in Canada: Examining Contributions to Nutrient and Food Group Intake and Differences across Eating Locations. J. Acad. Nutr. Diet. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Francis, J.; Martin, K.; Costa, B.; Christian, H.; Kaur, S.; Harray, A.; Barblett, A.; Oddy, W.H.; Ambrosini, G.; Allen, K.; et al. Informing Intervention Strategies to Reduce Energy Drink Consumption in Young People: Findings From Qualitative Research. J. Nutr. Educ. Behav. 2017, 49, 724–733. [Google Scholar] [CrossRef] [Green Version]
- Burgoine, T.; Forouhi, N.G.; Griffin, S.J.; Wareham, N.J.; Monsivais, P. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: Population based, cross sectional study. BMJ 2014, 348, 1464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drewnowski, A.; Rehm, C.D. Energy intakes of US children and adults by food purchase location and by specific food source. Nutr. J. 2013, 12, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NatCen Social Research. National Diet and Nutrition Survey Results from Years 1, 2, 3 and 4 (Combined) of the Rolling Programme (2008/2009–2011/2012); NatCen Social Research: London, UK, 2014. [Google Scholar]
- NatCen Social Research. National Diet and Nutrition Survey Results from Years 7 and 8 (Combined) of the Rolling Programme (2014/2015 to 2015/2016); NatCen Social Research: London, UK, 2018. [Google Scholar]
- Fincham, J.E. Response rates and responsiveness for surveys, standards, and the Journal. Am. J. Pharm. Educ. 2008, 72, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NDNS_Appendix_B. Weighting the Core Sample. 2011. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216487/dh_130786.pdf (accessed on 30 May 2020).
- NDNS_Appendix_A. Dietary Data Collection and Editing. 2014. Available online: https://www.food.gov.uk/sites/default/files/media/document/ndns-appendix-a.pdf (accessed on 30 May 2020).
- Palla, L.; Almoosawi, S. Diurnal Patterns of Energy Intake Derived via Principal Component Analysis and Their Relationship with Adiposity Measures in Adolescents: Results from the National Diet and Nutrition Survey RP (2008–2012). Nutrients 2019, 11, 422. [Google Scholar] [CrossRef] [Green Version]
- Fitt, E.; Cole, D.; Ziauddeen, N.; Pell, D.; Stickley, E.; Harvey, A.; Stephen, A.M. DINO (Diet In Nutrients Out)—An integrated dietary assessment system. Public Health Nutr. 2015, 18, 234–241. [Google Scholar] [CrossRef] [Green Version]
- Food Standards Agency (FSA). Food Portion Sizes; The Stationery Office: London, UK, 2002.
- NDNS_Appendix_X. Mis-Reporting in the NDNS. 2011. Available online: https://www.food.gov.uk/sites/default/files/media/document/ndns-appendix-x.pdf (accessed on 30 May 2020).
- NDNS_Appendix_R. Main and Subsidiary Food Groups. 2011. Available online: https://fsa-catalogue2.s3.eu-west-2.amazonaws.com/ndns-appendix-r.pdf (accessed on 30 May 2020).
- Scarborough, P.; Rayner, M.; Stockley, L. Developing nutrient profile models: A systematic approach. Public Health Nutr. 2007, 10, 330–336. [Google Scholar] [CrossRef] [Green Version]
- Food Standard Agency. Nutrient Profiling Technical Guidance; 2011. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216094/dh_123492.pdf (accessed on 30 May 2020).
- Pechey, R.; Jebb, S.A.; Kelly, M.P.; Almiron-Roig, E.; Conde, S.; Nakamura, R.; Shemilt, I.; Suhrcke, M.; Marteau, T.M. Socioeconomic differences in purchases of more vs. less healthy foods and beverages: Analysis of over 25,000 British households in 2010. Soc. Sci. Med. 2013, 92, 22–26. [Google Scholar] [CrossRef]
- Scarborough, P.; Boxer, A.; Rayner, M.; Stockley, L. Testing nutrient profile models using data from a survey of nutrition professionals. Public Health Nutr. 2007, 10, 337–345. [Google Scholar] [CrossRef]
- Greenacre, M.J. Correspondence Analysis in Practice; Academic Press: London, UK, 1993. [Google Scholar]
- Beh, E.J.; Lombardo, R. Correspondence Analysis: Theory, Practice and New Strategies; Wiley: Chichester, UK, 2014. [Google Scholar]
- Ringrose, T.J. Bootstrap confidence regions for correspondence analysis. J. Stat. Comput. Simul. 2012, 82, 1397–1413. [Google Scholar] [CrossRef]
- Beh, E.J.; Lombardo, R. Confidence Regions and Approximate p-values for Classical and Non Symmetric Correspondence Analysis. Commun. Stat. Methods 2015, 44, 95–114. [Google Scholar] [CrossRef]
- Liang, K.Y.; Zeger, S.L. Longitudinal Data-Analysis Using Generalized Linear-Models. Biometrika 1986, 73, 13–22. [Google Scholar] [CrossRef]
- Gabriel, K.R.; Odoroff, C.L. Biplots in Biomedical-Research. Stat. Med. 1990, 9, 469–485. [Google Scholar] [CrossRef] [PubMed]
- Gower, S.; Lubbe, S.; Le Roux, N.J. Understanding Biplots; Wiley: Chichester, UK, 2010. [Google Scholar]
- Hanley, J.A.; Negassa, A.; Edwardes, M.D.D.; Forrester, J.E. Statistical Analysis of Correlated Data Using Generalized Estimating Equations: An Orientation. Am. J. Epidemiol. 2003, 157, 364–375. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Hardin, J.W.; Hilbe, J.M. Generalised Estimating Equations, 2nd ed.; Chapman and Hall: New York, NY, USA, 2013. [Google Scholar]
- SAS Customer Support. Generalized Estimating Equations. SAS Support Document. Available online: https://support.sas.com/rnd/app/stat/topics/gee/gee.pdf (accessed on 7 July 2020).
- Office for National Statistics. The National Statistics Socio-Economic Classification (NS-SEC). Available online: https://www.ons.gov.uk/methodology/classificationsandstandards/otherclassifications/thenationalstatisticssocioeconomicclassificationnssecrebasedonsoc2010#classes-and-collapses (accessed on 30 May 2020).
- Subar, A.F.; Freedman, L.S.; A Tooze, J.; I Kirkpatrick, S.; Boushey, C.; Neuhouser, M.L.; E Thompson, F.; Potischman, N.; Guenther, P.M.; Tarasuk, V.; et al. Addressing Current Criticism Regarding the Value of Self-Report Dietary Data. J. Nutr. 2015, 145, 2639–2645. [Google Scholar] [CrossRef] [Green Version]
- Kirwan, L.; Walsh, M.C.; Brennan, L.; Gibney, E.R.; A Drevon, C.; Daniel, H.; A Lovegrove, J.; Manios, Y.; A Martínez, J.; Saris, W.H.M.; et al. Comparison of the portion size and frequency of consumption of 156 foods across seven European countries: Insights from the Food4ME study. Eur. J. Clin. Nutr. 2016, 70, 642–644. [Google Scholar] [CrossRef]
- Lewis, H.B.; Ahern, A.L.; A Jebb, S. How much should I eat? A comparison of suggested portion sizes in the UK. Public Health Nutr. 2012, 15, 2110–2117. [Google Scholar] [CrossRef] [Green Version]
- Haskelberg, H.; Neal, B.; Dunford, E.; Flood, V.; Rangan, A.; Thomas, B.; Cleanthous, X.; Trevena, H.; Zheng, J.M.; Louie, J.C.Y.; et al. High variation in manufacturer-declared serving size of packaged discretionary foods in Australia. Br. J. Nutr. 2016, 115, 1810–1818. [Google Scholar] [CrossRef] [Green Version]
- Steyn, N.P.; Senekal, M.; Norris, S.A.; Whati, L.; Mackeown, J.M.; Nel, J.H. How well do adolescents determine portion sizes of foods and beverages? Asia. Pac. J. Clin. Nutr. 2006, 15, 35–42. [Google Scholar]
- Cleophas, T.J.; Zwinderman, A.H. Machine Learning in Medicine—A Complete Overview, 2nd ed.; Springer Nature: Cham, Switzerland, 2015. [Google Scholar]
- Chapman, A.; Beh, E.; Palla, L. Application of Correspondence Analysis to Graphically Investigate Associations Between Foods and Eating Locations. Stud. Health Technol. Inform. 2017, 235, 166–170. [Google Scholar] [PubMed]
- Cohen, D.A.; Ghosh-Dastidar, B.; Beckman, R.; Lytle, L.; Elder, J.; Pereira, M.A.; Mortenson, S.V.; Pickrel, J.; Conway, T.L. Adolescent girls’ most common source of junk food away from home. Health Place 2012, 18, 963–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mytton, O.T.; Forouhi, N.G.; Scarborough, P.; Lentjes, M.; Luben, R.; Rayner, M.; Khaw, K.T.; Wareham, N.J.; Monsivais, P. Association between intake of less-healthy foods defined by the United Kingdom’s nutrient profile model and cardiovascular disease: A population-based cohort study. Popkin BM, ed. PLoS Med. 2018, 15, e1002484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziauddeen, N.; Almiron-Roig, E.; Penney, T.; Nicholson, S.; Kirk, S.F.; Page, P. Eating at Food Outlets and “On the Go” Is Associated with Less Healthy Food Choices in Adults: Cross-Sectional Data from the UK National Diet and Nutrition Survey Rolling Programme (2008–2014). Nutrients 2017, 9, 1315. [Google Scholar] [CrossRef] [Green Version]
- Mak, T.N.; Prynne, C.J.; Cole, D.; Fitt, E.; Roberts, C.; Bates, B.; Stephen, A.M. Assessing eating context and fruit and vegetable consumption in children: New methods using food diaries in the UK National Diet and Nutrition Survey Rolling Programme. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 126. [Google Scholar] [CrossRef] [Green Version]
- Matthiessen, J.; Fagt, S.; Biltoft-Jensen, A.P.; Beck, A.M.; Ovesen, L. Size makes a difference. Public Health Nutr. 2003, 61, 65–72. [Google Scholar] [CrossRef]
- Rehm, C.D.; Drewnowski, A. Trends in consumption of solid fats, added sugars, sodium, sugar-sweetened beverages, and fruit from fast food restaurants and by fast food restaurant type among US children, 2003-2010. Nutrients 2016, 8, 804. [Google Scholar] [CrossRef] [Green Version]
- Drewnowski, A.; Aggarwal, A.; Cook, A.; Stewart, O.; Moudon, A.V. Geographic disparities in Healthy Eating Index scores (HEI-2005 and 2010) by residential property values: Findings from Seattle Obesity Study (SOS). Prev. Med. (Baltim.) 2016, 83, 46–55. [Google Scholar] [CrossRef] [Green Version]
- Lake, A.; Townshend, T. Obesogenic environments: Exploring the built and food environments. J. R. Soc. Promot. Health 2006, 1266, 262–267. [Google Scholar] [CrossRef]
- Department of Health. Childhood Obesity: A Plan for Action. Published 2016. Available online: https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action (accessed on 7 July 2020).
- Hollands, G.J.; Shemilt, I.; Marteau, T.; Jebb, S.A.; Kelly, M.P.; Nakamura, R.; Suhrcke, M.; Ogilvie, D.B. Altering micro-environments to change population health behaviour: Towards an evidence base for choice architecture interventions. BMC Public Health 2013, 13, 1218. [Google Scholar] [CrossRef]

| Calories Cumul % | Score | Healthiness Category | |||
|---|---|---|---|---|---|
| Healthier < −2 | Neutral | Less Healthy > 4 | |||
| Pasta and rice and other cereals | 10.05 | 2.0 | N | ||
| White Bread | 18.49 | 1.7 | N | ||
| Chips and potatoes | 24.54 | −0.3 | N | ||
| Soft drinks, not diet | 29.86 | 2.2 | N | ||
| Biscuits | 34.00 | 18.9 | L | ||
| Crisps, savoury snacks | 37.84 | 12.3 | L | ||
| Chocolate (incl. confectionary) | 41.50 | 25.2 | L | ||
| Buns, cakes, sweet pastries, fruit pies | 44.99 | 17.1 | L | ||
| Chicken dishes and turkey | 48.36 | −0.5 | N | ||
| Miscellaneous unclassified foods | 51.22 | 9.4 | L | ||
| Cheese | 53.88 | 22.0 | L | ||
| Semi-skimmed milk | 56.47 | −0.5 | N | ||
| Vegetables (not raw) | 58.93 | −6.3 | H | ||
| Low-fibre breakfast cereals | 61.20 | 11.8 | L | ||
| Sausages | 63.36 | 14.6 | L | ||
| Coated chicken and turkey manuf. | 65.37 | 5.6 | L | ||
| Potatoes other, potato salads and dishes | 67.24 | −1.7 | N | ||
| Beef, veal and dishes | 69.10 | 0.5 | N | ||
| Fruit | 70.93 | −3.3 | H | ||
| High fibre breakfast cereals | 72.76 | 2.1 | N | ||
| Fruit juice | 74.53 | 1.5 | N | ||
| Spreads, less fat | 76.27 | 22.9 | L | ||
| Meat pastries, rolls and pies (“meat pies”) | 77.92 | 15.1 | L | ||
| Brown Bread granary and wheat germ | 79.42 | −3.0 | H | ||
| Sugars, preserves and sweet spreads | 80.91 | 15.1 | L | ||
| N | % | % (Weighted Sample) | ||
|---|---|---|---|---|
| Age (years) | 11–15 | 543 | 61.4 | 60.8 |
| 16–18 | 341 | 38.6 | 39.2 | |
| Sex | Male | 445 | 50.3 | 51.3 |
| Female | 439 | 49.7 | 48.7 | |
| Ethnicity (%) | White | 778 | 88 | 86.2 |
| Non-white | 106 | 12 | 13.8 | |
| Occupational group (SES) * | 1. Higher managerial, administrative and professional occupations | 126 | 14.3 | 14.6 |
| 2. Lower managerial, administrative and professional occupations | 236 | 26.7 | 24.6 | |
| 3. Intermediate occupations | 73 | 8.3 | 7.4 | |
| 4. Small employers and own account workers | 94 | 10.6 | 11.2 | |
| 5. Lower supervisory and technical occupations | 90 | 10.2 | 9.7 | |
| 6. Semi-routine occupations | 125 | 14.1 | 14.6 | |
| 7. Routine occupations | 91 | 10.3 | 11.5 | |
| 8. Never worked and long-term unemployed | 29 | 3.3 | 4.3 | |
| Missing | 20 | 2.3 | 2.2 | |
| BMI (%) | Normal weight | 553 | 62.6 | 62.7 |
| Overweight | 124 | 14.0 | 14.5 | |
| Obese | 175 | 19.8 | 19.8 | |
| Missing | 32 | 3.6 | 3 | |
| Drinking (%) | Yes ** | 132 | 14.9 | 13.8 |
| No (once or twice a months or less) | 752 | 85.1 | 86.2 | |
| Smoking (%) | Yes *** | 91 | 10.3 | 10.4 |
| No | 793 | 89.7 | 89.6 | |
| Location | Frequency | % of Total | Cumulative % |
|---|---|---|---|
| Home (all home locations) | 44,271 | 70.8 | |
| Home living room | 15,552 | 24.9 | 24.9 |
| Home kitchen | 12,558 | 20.1 | 45.0 |
| Home dining room | 6207 | 9.9 | 54.9 |
| Home bedroom | 4100 | 6.6 | 61.5 |
| Home not given | 2703 | 4.3 | 65.8 |
| Home other | 2617 | 4.2 | 70.0 |
| Home garden | 534 | 0.9 | 70.8 |
| School | 7683 | 12.3 | 83.1 |
| Leisure clubs, cafes | 3190 | 5.1 | 88.2 |
| Friends’/Carers’/Relatives’ homes | 2769 | 4.4 | 92.6 |
| Other locations | 2161 | 3.5 | 96.1 |
| Mobile: car, bus, train, etc. | 1295 | 2.1 | 98.2 |
| Work | 1154 | 1.9 | 100 |
| All locations | 62,523 | 100 |
| Unadjusted Odds Ratio | Adjusted Odds Ratio | |||||||
|---|---|---|---|---|---|---|---|---|
| Other Location vs. Home | Other Location vs. School/Work | Other Location vs. Home | Other Location vs. School/Work | |||||
| Food | OR | 99% CI p-Value | OR | 99% CI p-Value | OR | 99% CI p-Value | OR | 99% CI p-Value |
| Sweetened soft drinks (N = 1678) | 2.78 | (2.07, 3.73) p < 0.0001 | 2.09 | (1.50, 2.93) p < 0.0001 | 2.79 | (2.08, 3.75) p < 0.0001 | 2.02 | (1.43, 2.84) p < 0.0001 |
| Chips (N = 664) | 2.81 | (2.17, 3.63) p < 0.0001 | 3.42 | (2.16, 5.40) p < 0.0001 | 2.82 | (2.17, 3.66) p < 0.0001 | 3.42 | (2.13, 5.50) p < 0.0001 |
| Chocolate (N = 574) | 2.49 | (1.81, 3.42) p < 0.0001 | 1.72 | (1.14, 2.60) p = 0.0007 | 2.56 | (1.85, 3.51) p < 0.0001 | 1.88 | (1.22, 2.91) p = 0.0002 |
| Meat pies (N = 124) | 2.61 | (1.42, 4.81) p < 0.0001 | 1.22 | (0.55, 2.71) p = 0.53 | 2.73 | (1.48, 5.06) p < 0.0001 | 1.28 | (0.53, 3.07) p = 0.47 |
| Unadjusted Odds Ratio | Adjusted Odds Ratio | |||||||
|---|---|---|---|---|---|---|---|---|
| Other Location vs. Home | Other Location vs. School/Work | Other Location vs. Home | Other Location vs. School/Work | |||||
| Food | OR | 99% CI p-Value | OR | 99% CI p-Value | OR | 99% CI p-Value | OR | 99% CI p-Value |
| Sweetened soft drinks (N = 2999) | 3.08 | (2.56, 3.70) p < 0.0001 | 2.59 | (1.96, 3.42) p < 0.0001 | 3.06 | (2.53, 3.71) p < 0.0001 | 2.50 | (1.84, 3.39) p < 0.0001 |
| Chips (N = 1546) | 2.92 | (2.39, 3.55) p < 0.0001 | 2.94 | (2.10, 4.12) p < 0.0001 | 2.91 | (2.36, 3.57) p < 0.0001 | 2.75 | (1.91, 3.95) p < 0.0001 |
| Chocolate (N = 1440) | 2.38 | (1.84, 3.07) p < 0.0001 | 1.30 | (0.94, 1.81) p = 0.0007 | 2.35 | (1.82, 3.03) p < 0.0001 | 1.31 | (0.93, 1.83) p = 0.04 |
| Meat pies (N = 306) | 1.96 | (1.23, 3.10) p = 0.0002 | 0.76 | (0.40, 1.45) p = 0.28 | 1.89 | (1.19, 3.01) p = 0.0004 | 0.74 | (0.39, 1.39) p = 0.21 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palla, L.; Chapman, A.; Beh, E.; Pot, G.; Almiron-Roig, E. Where Do Adolescents Eat Less-Healthy Foods? Correspondence Analysis and Logistic Regression Results from the UK National Diet and Nutrition Survey. Nutrients 2020, 12, 2235. https://doi.org/10.3390/nu12082235
Palla L, Chapman A, Beh E, Pot G, Almiron-Roig E. Where Do Adolescents Eat Less-Healthy Foods? Correspondence Analysis and Logistic Regression Results from the UK National Diet and Nutrition Survey. Nutrients. 2020; 12(8):2235. https://doi.org/10.3390/nu12082235
Chicago/Turabian StylePalla, Luigi, Andrew Chapman, Eric Beh, Gerda Pot, and Eva Almiron-Roig. 2020. "Where Do Adolescents Eat Less-Healthy Foods? Correspondence Analysis and Logistic Regression Results from the UK National Diet and Nutrition Survey" Nutrients 12, no. 8: 2235. https://doi.org/10.3390/nu12082235





