Assessing Adherence, Competence and Differentiation in a Stepped-Wedge Randomised Clinical Trial of a Complex Behaviour Change Intervention
Abstract
:1. Introduction
1.1. Objectives and Importance
1.2. The Aims of the Current Paper Are to
- Estimate the adherence to the EAT Intervention, including the degree to which intervention components were delivered during dietetic consultations conducted after training in the EAT Intervention.
- Estimate the competence with which the EAT Intervention was delivered, including the degree to which sessions conducted after training met apriori competence benchmarks.
- Examine the differentiation of the intervention period from the control period by comparing adherence and competence outcomes, non-specific factors (therapeutic alliance) and treatment dose (session number and duration). We expected that intervention sessions would be differentiated from control sessions with regard to adherence and competence outcomes (i.e., increased delivery of the intervention and greater skills). No specific hypotheses were made regarding therapeutic alliance or dose, as it is unknown whether and/or how these factors may be influenced by training in the EAT Intervention.
2. Materials and Methods
2.1. Setting and Trial Design
2.2. Intervention Providers
2.3. Interventions
Treatment as Usual
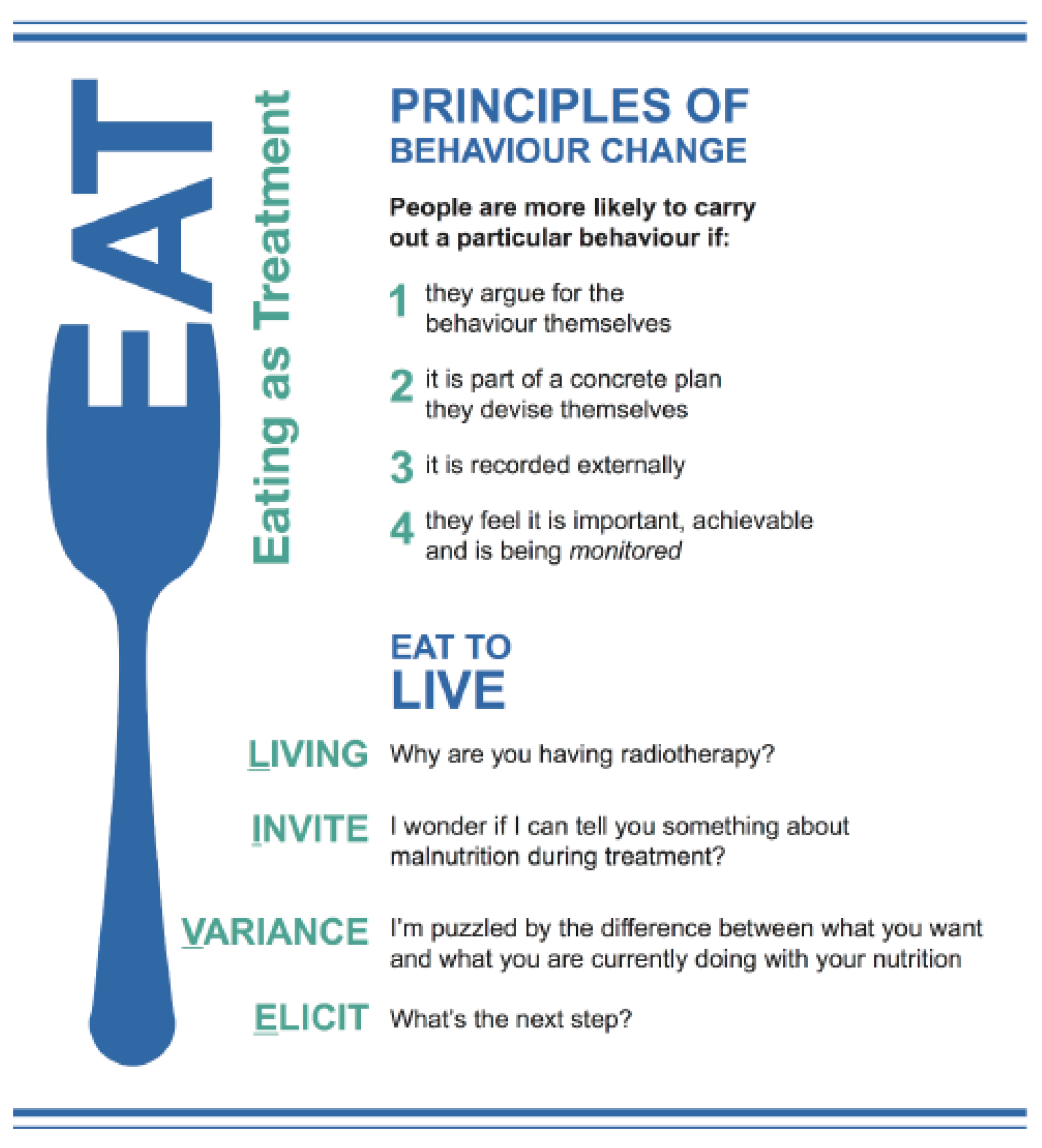
2.4. The EAT Intervention
Intervention
2.5. Procedure
2.5.1. Training
2.5.2. Audio-Recordings
2.5.3. Sampling
2.5.4. Coding
2.5.5. Measures
Adherence
Competence
2.6. Non-specific Factors
2.7. Number and Duration of Dietetic Consultations
2.8. Statistical Analysis
2.8.1. Adherence
2.8.2. Competence
2.8.3. Differentiation
2.8.4. Non-specific Factors
3. Results
3.1. Intervention Adherence
3.2. Intervention Competence
3.3. Delivery of the EAT Intervention Across Time
3.3.1. Differentiation
3.3.2. Contamination
3.4. Non-Specific Factors
3.5. Dose
4. Discussion
4.1. Delivery of Study Checklist Skills
4.2. Behaviour Change Counselling
4.3. Implications for Research and Practice
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Van Bokhorst-de van der, S.; van Leeuwen, P.A.; Kuik, D.J.; Klop, W.M.; Sauerwein, H.P.; Snow, G.B.; Quak, J.J. The impact of nutritional status on the prognoses of patients with advanced head and neck cancer. Cancer 1999, 86, 519–527. [Google Scholar] [CrossRef]
- Bauer, J.; Isenring, E.; Ferguson, M. Dietary counseling: Evidence in chemotherapy patients. J. Support Oncol. 2008, 6, 354–355. [Google Scholar] [PubMed]
- Gorenc, M.; Kozjek, N.R.; Strojan, P. Malnutrition and cachexia in patients with head and neck cancer treated with (chemo)radiotherapy. Rep. Pract. Oncol. Radiother. 2015, 20, 249–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linden, W.; Vodermaier, A.; Mackenzie, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Fixsen, D.; Grimshaw, J.M.; Eccles, M.P. Specifying and reporting complex behaviour change interventions: The need for a scientific method. Implement. Sci. 2009, 4, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onken, L.S.; Carroll, K.M.; Shoham, V.; Cuthbert, B.N.; Riddle, M. Reenvisioning Clinical Science: Unifying the Discipline to Improve the Public Health. Clin. Psychol. Sci. 2014, 2, 22–34. [Google Scholar] [CrossRef] [Green Version]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [Green Version]
- Borrelli, B.; Sepinwall, D.; Ernst, D.; Bellg, A.J.; Czajkowski, S.; Breger, R.; DeFrancesco, C.; Levesque, C.; Sharp, D.L.; Ogedegbe, G.; et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J. Consult. Clin. Psychol. 2005, 73, 852–860. [Google Scholar] [CrossRef]
- Perepletchikova, F.; Treat, T.A.; Kazdin, A.E. Treatment integrity in psychotherapy research: Analysis of the studies and examination of the associated factors. J. Consult. Clin. Psychol. 2007, 75, 829–841. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. The effectiveness and ineffectiveness of complex behavioral interventions: Impact of treatment fidelity. Contemp. Clin. Trials 2014, 37, 234–241. [Google Scholar] [CrossRef]
- Walton, H.; Spector, A.; Tombor, I.; Michie, S. Measures of fidelity of delivery of, and engagement with, complex, face-to-face health behaviour change interventions: A systematic review of measure quality. Br. J. Health Psychol. 2017, 22, 872–903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rixon, L.; Baron, J.; McGale, N.; Lorencatto, F.; Francis, J.; Davies, A. Methods used to address fidelity of receipt in health intervention research: A citation analysis and systematic review. BMC Health Serv. Res. 2016, 16, 663. [Google Scholar] [CrossRef] [Green Version]
- Preyde, M.; Burnham, P.V. Intervention fidelity in psychosocial oncology. J. Evid. Based Soc. Work 2011, 8, 379–396. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, B. The Assessment, Monitoring, and Enhancement of Treatment Fidelity In Public Health Clinical Trials. J. Public Health Dent. 2011, 71, S52–S63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boutron, I.; Altman, D.G.; Moher, D.; Schulz, K.F.; Ravaud, P. CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann. Intern. Med. 2017, 167, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Britton, B.; McCarter, K.; Baker, A.; Wolfenden, L.; Wratten, C.; Bauer, J.; Beck, A.K.; McElduff, P.; Halpin, S.; Carter, G. Eating As Treatment (EAT) study protocol: A stepped-wedge, randomised controlled trial of a health behaviour change intervention provided by dietitians to improve nutrition in patients with head and neck cancer undergoing radiotherapy. BMJ Open 2015, 5. [Google Scholar] [CrossRef]
- Britton, B.; Baker, A.; Wolfenden, L.; Wratten, C.; Bauer, J.; Beck, A.K.; McCarter, K.; Harrowfield, J.; Isenring, E.; Tang, C.; et al. Eating As Treatment (EAT): A stepped-wedge, randomised controlled trial of a health behaviour change intervention provided by dietitians to improve nutrition in patients with head and neck cancer undergoing radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 353–362. [Google Scholar] [CrossRef] [Green Version]
- Britton, B.; Baker, A.; Clover, K.; McElduff, P.; Wratten, C.; Carter, G. Heads Up: A pilot trial of a psychological intervention to improve nutrition in head and neck cancer patients undergoing radiotherapy. Eur. J. Cancer Care 2016, 26. [Google Scholar] [CrossRef]
- Ottery, F.D. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 1996, 12 (Suppl. 1), S15–S19. [Google Scholar] [CrossRef]
- NHMRC. National Health and Medical Research Council National Statement on Ethical Conduct in Human Research (2007)-Updated May 2015; The National Health and Medical Research Council, the Australian Research Council and the Australian Vice-Chancellors’ Committee; Commonwealth of Australia: Canberra, Australia, 2015.
- Beck, A.K.; Baker, A.; Britton, B.; Wratten, C.; Bauer, J.; Wolfenden, L.; Carter, G. Fidelity considerations in translational research: Eating As Treatment—A stepped wedge, randomised controlled trial of a dietitian delivered behaviour change counselling intervention for head and neck cancer patients undergoing radiotherapy. Trials 2015, 16, 465. [Google Scholar] [CrossRef] [Green Version]
- Hussey, M.A.; Hughes, J.P. Design and analysis of stepped wedge cluster randomized trials. Contemp. Clin. Trials 2007, 28, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Head and Neck Guideline Steering Committee. Evidence-Based Practice Guidelines for the Nutritional Management of Adult Patients with Head and Neck Cancer; Cancer Council Australia: Sydney, Australia, 2015. [Google Scholar]
- McHugh, R.K.; Murray, H.W.; Barlow, D.H. Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behav. Res. Ther. 2009, 47, 946–953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rollnick, S.; Mason, P.; Butler, C. Health Behaviour Change: A Guide for Practitioners, 1st ed.; Churchill Livingstone: London, UK, 1999. [Google Scholar]
- McCarter, K.; Baker, A.; Britton, B.; Beck, A.K.; Carter, G.; Bauer, J.; Wratten, C.; Halpin, S.A.; Holliday, E.; Oldmeadow, C.; et al. Effectiveness of clinical practice change strategies in improving dietitian care for head and neck cancer patients according to evidence based clinical guidelines: A stepped wedge randomised controlled trial. Transl. Behav. Med. 2018, 8, 166–174. [Google Scholar] [CrossRef] [Green Version]
- Bellg, A.J.; Borrelli, B.; Resnick, B.; Hecht, J.; Minicucci, D.S.; Ory, M.; Ogedegbe, G.; Orwig, D.; Ernst, D.; Czajkowski, S. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004, 23, 443–451. [Google Scholar] [CrossRef]
- Lane, C.; Huws-Thomas, M.; Hood, K.; Rollnick, S.; Edwards, K.; Robling, M. Measuring adaptations of motivational interviewing: The development and validation of the behavior change counseling index (BECCI). Patient Educ. Couns. 2005, 56, 166–173. [Google Scholar] [CrossRef]
- Blackburn, I.-M.; James, I.; Milne, D.; Reichelt, F.K. Cognitive Therapy Scale-Revised (CTS-R). Newcastle upon Tyne, UK. 2000. Available online: https://ebbp.org/resources/CTS-R.pdf (accessed on 20 June 2020).
- Dreyfus, S.E. The Five-Stage Model of Adult Skill Acquisition. Bull. Sci. Technol. Soc. 2004, 24, 177–181. [Google Scholar] [CrossRef] [Green Version]
- Holdsworth, E.; Bowen, E.; Brown, S.; Howat, D. Client engagement in psychotherapeutic treatment and associations with client characteristics, therapist characteristics, and treatment factors. Clin. Psychol. Rev. 2014, 34, 428–450. [Google Scholar] [CrossRef] [Green Version]
- Copeland, L.; McNamara, R.; Kelson, M.; Simpson, S. Mechanisms of change within motivational interviewing in relation to health behaviors outcomes: A systematic review. Patient Educ. Couns. 2015, 98, 401–411. [Google Scholar] [CrossRef]
- Nienhuis, J.B.; Owen, J.; Valentine, J.C.; Winkeljohn Black, S.; Halford, T.C.; Parazak, S.E.; Budge, S.; Hilsenroth, M. Therapeutic alliance, empathy, and genuineness in individual adult psychotherapy: A meta-analytic review. Psychother. Res. 2018, 28, 593–605. [Google Scholar] [CrossRef]
- De Vries, A.M.M.; de Roten, Y.; Meystre, C.; Passchier, J.; Despland, J.N.; Stiefel, F. Clinician characteristics, communication, and patient outcome in oncology: A systematic review. Psycho-Oncology 2014, 23, 375–381. [Google Scholar] [CrossRef]
- Cahill, J.; Stiles, W.B.; Barkham, M.; Hardy, G.E.; Stone, G.; Agnew-Davies, R.; Unsworth, G. Two short forms of the Agnew Relationship Measure: The ARM-5 and ARM-12. Psychother. Res. 2012, 22, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Lane, C. The Behaviour Change Counselling Index (BECCI): Manual for Coding Behaviour Change Counselling; University of Wales College of Medicine: Wales, UK, 2002. [Google Scholar]
- Beck, A.K.; Britton, B.; Baker, A.; Odelli, C.; Wratten, C.; Bauer, J.; Wolfenden, L.; Carter, G. Preliminary report: Training head and neck cancer dietitians in behaviour change counselling. PPsycho-Oncology 2017, 26, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, J.; Kuerbis, A.; Amrhein, P.; Hail, L.; Lynch, K.; McKay, J.R. Motivational interviewing: A pilot test of active ingredients and mechanisms of change. Psychol. Addict. Behav. 2012, 26, 859–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spahn, J.M.; Reeves, R.S.; Keim, K.S.; Laquatra, I.; Kellogg, M.; Jortberg, B.; Clark, N.A. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet. Assoc. 2010, 110, 879–891. [Google Scholar] [CrossRef]
- Charuhas Macris, P.; Schilling, K.; Palko, R. Academy of Nutrition and Dietetics: Revised 2017 Standards of Practice and Standards of Professional Performance for Registered Dietitian Nutritionists (Competent, Proficient, and Expert) in Oncology Nutrition. J. Acad. Nutr. Diet. 2018, 118, 736–748.e42. [Google Scholar] [CrossRef] [Green Version]
- Michie, S.; Abraham, C.; Whittington, C.; McAteer, J.; Gupta, S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychol. 2009, 28, 690–701. [Google Scholar] [CrossRef] [Green Version]
- Bailey, R.R. Goal Setting and Action Planning for Health Behavior Change. Am. J. Lifestyle Med. 2017, 13, 615–618. [Google Scholar] [CrossRef]
- Effective Public Health Practice Project. Dictionary for the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies. 1998. Available online: https://epoc.cochrane.org/epoc-taxonomy (accessed on 20 June 2020).
- Kendall, P.; Gosch, E.; Furr, J.; Sood, E. Flexibility Within Fidelity. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 987–993. [Google Scholar] [CrossRef]
- Wiltsey Stirman, S.; Gutner, C.A.; Crits-Christoph, P.; Edmunds, J.; Evans, A.C.; Beidas, R.S. Relationships between clinician-level attributes and fidelity-consistent and fidelity-inconsistent modifications to an evidence-based psychotherapy. Implement. Sci. 2015, 10, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Aarons, G.A. Mental Health Provider Attitudes toward Adoption of Evidence-Based Practice: The Evidence-Based Practice Attitude Scale (EBPAS). Ment. Health Serv. Res. 2004, 6, 61–74. [Google Scholar] [CrossRef]
- Spollen, J.J.; Thrush, C.R.; Mui, D.V.; Woods, M.B.; Tariq, S.G.; Hicks, E. A randomized controlled trial of behavior change counseling education for medical students. Med. Teach. 2010, 32, e170–e177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, C.C.; Simpson, S.A.; Hood, K.; Cohen, D.; Pickles, T.; Spanou, C.; McCambridge, J.; Moore, L.; Randell, E.; Alam, M.F.; et al. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: A cluster randomised trial. BMJ 2013, 346, f1191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jansink, R.; Braspenning, J.; Laurant, M.; Keizer, E.; Elwyn, G.; Weijden, T.v.d.; Grol, R. Minimal improvement of nurses’ motivational interviewing skills in routine diabetes care one year after training: A cluster randomized trial. BMC Fam. Pract. 2013, 14, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soderlund, L.L.; Madson, M.B.; Rubak, S.; Nilsen, P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ. Couns. 2011, 84, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.; Staiger, P.K.; Simpson, A.; Best, D.; Lubman, D.I. After 30 years of dissemination, have we achieved sustained practice change in motivational interviewing? Addiction 2016, 111, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Moyers, T.B. Eight Stages in Learning Motivational Interviewing. J. Teach. Addict. 2006, 5, 3–17. [Google Scholar] [CrossRef]
- Miller, W.R.; Yahne, C.E.; Moyers, T.B.; Martinez, J.; Pirritano, M. A randomized trial of methods to help clinicians learn motivational interviewing. J. Consult. Clin. Psychol. 2004, 72, 1050–1062. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehane, E.; Leahy-Warren, P.; O’Riordan, C.; Savage, E.; Drennan, J.; O’Tuathaigh, C.; O’Connor, M.; Corrigan, M.; Burke, F.; Hayes, M.; et al. Evidence-based practice education for healthcare professions: An expert view. BMJ Evid. Based Med. 2019, 24, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rapoport, L.; Perry, K.N. Do dietitians feel that they have had adequate training in behaviour change methods? J. Hum. Nutr. Diet. 2000, 13, 287–298. [Google Scholar] [CrossRef]
- Cant, R.P.; Aroni, R.A. Exploring dietitians’ verbal and nonverbal communication skills for effective dietitian-patient communication. J. Hum. Nutr. Diet. 2008, 21, 502–511. [Google Scholar] [CrossRef]
- Ashenden, R.; Silagy, C.; Weller, D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam. Pract. 1997, 14, 160–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sladdin, I.; Ball, L.; Bull, C.; Chaboyer, W. Patient-centred care to improve dietetic practice: An integrative review. J. Hum. Nutr. Diet. 2017, 30, 453–470. [Google Scholar] [CrossRef] [PubMed]
- Hallgren, K.A.; Dembe, A.; Pace, B.T.; Imel, Z.E.; Lee, C.M.; Atkins, D.C. Variability in motivational interviewing adherence across sessions, providers, sites, and research contexts. J. Subst. Abuse Treat. 2018, 84, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; West, R.; Sheals, K.; Godinho, C.A. Evaluating the effectiveness of behavior change techniques in health-related behavior: A scoping review of methods used. Transl. Behav. Med. 2018, 8, 212–224. [Google Scholar] [CrossRef] [Green Version]
- Mowbray, C.T.; Holter, M.C.; Teague, G.B.; Bybee, D. Fidelity Criteria: Development, Measurement, and Validation. Am. J. Eval. 2003, 24, 315–340. [Google Scholar] [CrossRef]
- Collyer, H.; Eisler, I.; Woolgar, M. Systematic literature review and meta-analysis of the relationship between adherence, competence and outcome in psychotherapy for children and adolescents. Eur. Child Adolesc. Psychiatry 2018, 29, 417–431. [Google Scholar] [CrossRef]
- Whitehead, K.A.; Langley-Evans, S.C.; Tischler, V.A.; Swift, J.A. Communication skills for behaviour change in dietetic consultations. J. Hum. Nutr. Diet. 2009, 22, 493–500. [Google Scholar] [CrossRef]
- Whitehead, K.A.; Langley-Evans, S.C.; Tischler, V.A.; Swift, J.A. Assessing communication skills in dietetic consultations: The development of the reliable and valid DIET-COMMS tool. J. Hum. Nutr. Diet. 2014, 27, 321–332. [Google Scholar] [CrossRef]
- Gearing, R.E.; El-Bassel, N.; Ghesquiere, A.; Baldwin, S.; Gillies, J.; Ngeow, E. Major ingredients of fidelity: A review and scientific guide to improving quality of intervention research implementation. Clin. Psychol. Rev. 2011, 31, 79–88. [Google Scholar] [CrossRef]
- Shah, S.; Rodolfa, E. Peer Supervision and Support. In APA Handbook of Clinical Psychology: Education and Profession; Norcross, J.C., VandenBos, G.R., Freedheim, D.K., Campbell, L.F., Eds.; American Psychological Association: Washington, DC, USA, 2016; pp. 197–207. [Google Scholar]
- Frank, H.E.; Becker-Haimes, E.M.; Kendall, P.C. Therapist training in evidence-based interventions for mental health: A systematic review of training approaches and outcomes. Clin. Psychol. Sci. Pract. 2020, e12330. [Google Scholar] [CrossRef]

| YES | NO | |
|---|---|---|
| Practitioner discusses the adequacy of the patient’s energy intake | ||
| Practitioner conducts a formal/standardised assessment to measure patient nutrition | ||
| Practitioner discusses how eating/nutrition is an integral part of “radiotherapy” treatment | ||
| Practitioner encourages the patient to discuss their reason(s) for undergoing radiotherapy | ||
| Practitioner collaboratively develops a formal, written nutrition plan with the patient | ||
| Practitioner encourages the patient to discuss their progress towards the goals outlined on their written nutrition plan |
| Control (n = 196) | Intervention (n = 194) | Odds ratio, Beta, or z Score † | Confidence Interval † | p† | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| ADHERENCE | ||||||
| Study Specific Checklist | ||||||
| Reasons for RT | 2 (1.2%) | 43 (22.1%) | OR = 24.087 | 3.408 | 170.247 | 0.001 ** |
| Eating as Integral to Radiotherapy | 49 (25%) | 88 (45.3%) | OR = 7.083 | 2.582 | 19.431 | <0.001 *** |
| Nutrition Plan | 8 (4%) | 61 (31.4%) | OR = 55.171 | 10.875 | 279.893 | <0.001 *** |
| Review Plan | 2 (1.2%) | 30 (18.5%) | OR = 4.086 | 0.446 | 37.406 | 0.213 |
| Validated Nutrition Assessment | 112 (57.1%) | 144 (73.4%) | OR = 0.674 | 0.299 | 1.522 | 0.342 |
| Adequacy of Intake | 173 (88.2%) | 187 (96.3%) | OR = 0.917 | 0.211 | 3.987 | 0.908 |
| Behaviour Change Counselling Index | ||||||
| Threshold of 2.57 attained | 12 (6.1%) | 30 (15.5%) | OR = 11.819 | 2.617 | 53.382 | 0.001 ** |
| Overall Practitioner Score | 2.01 (0.39) | 2.14 (0.42) | β = 0.315 | 0.121 | 0.393 | <0.001 *** |
| “Spirit” of Intervention Delivery | ||||||
| Meets Dreyfus Threshold (i.e., “Competent”) | 196 (100%) | 194 (100%) | ||||
| Mean CTS-R Interpersonal Effectiveness Score | 5.51 (0.73) | 5.69 (0.67) | β = −0.023 | −0.246 | 0.180 | 0.762 |
| COMPETENCE | ||||||
| CTS-R Application of Behaviour Change Counselling Item | ||||||
| Meets Dreyfus Threshold (i.e., “Competent”) | 69 (35.2%) | 109 (56.2%) | OR = 4.176 | 1.905 | 9.153 | <0.001 *** |
| Mean CTS-R Application of BCC Competence Score | 2.21 (1.08) | 2.72 (1.34) | β = 0.386 | 0.540 | 1.386 | <0.001 *** |
| NON-SPECIFIC EFFECTS | ||||||
| Therapeutic Alliance | ||||||
| Patient Rated | 33.01 (4.02) | 33.38 (3.07) | z = −0.61 | −6.76 | 3.55 | 0.542 |
| Dietitian Rated | 29.69 (4.60) | 31.6 3 (4.34) | z = −0.63 | −7.29 | 3.74 | 0.528 |
| DOSE | ||||||
| Number of Dietetic Consultations Attended | 10.34 (3.59) | 10.05 (2.86) | β = −0.042 | −1.026 | 0.485 | 0.482 |
| Session Duration (mins) | 19:11 (08:11) | 19:39 (10:42) | β = 28.55 | −85.27 | 142.37 | 0.622 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beck, A.K.; Baker, A.L.; Carter, G.; Wratten, C.; Bauer, J.; Wolfenden, L.; McCarter, K.; Britton, B. Assessing Adherence, Competence and Differentiation in a Stepped-Wedge Randomised Clinical Trial of a Complex Behaviour Change Intervention. Nutrients 2020, 12, 2332. https://doi.org/10.3390/nu12082332
Beck AK, Baker AL, Carter G, Wratten C, Bauer J, Wolfenden L, McCarter K, Britton B. Assessing Adherence, Competence and Differentiation in a Stepped-Wedge Randomised Clinical Trial of a Complex Behaviour Change Intervention. Nutrients. 2020; 12(8):2332. https://doi.org/10.3390/nu12082332
Chicago/Turabian StyleBeck, Alison Kate, Amanda L. Baker, Gregory Carter, Chris Wratten, Judith Bauer, Luke Wolfenden, Kristen McCarter, and Ben Britton. 2020. "Assessing Adherence, Competence and Differentiation in a Stepped-Wedge Randomised Clinical Trial of a Complex Behaviour Change Intervention" Nutrients 12, no. 8: 2332. https://doi.org/10.3390/nu12082332
APA StyleBeck, A. K., Baker, A. L., Carter, G., Wratten, C., Bauer, J., Wolfenden, L., McCarter, K., & Britton, B. (2020). Assessing Adherence, Competence and Differentiation in a Stepped-Wedge Randomised Clinical Trial of a Complex Behaviour Change Intervention. Nutrients, 12(8), 2332. https://doi.org/10.3390/nu12082332





