A Traditional Korean Diet Alters the Expression of Circulating MicroRNAs Linked to Diabetes Mellitus in a Pilot Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Dietary Intervention
2.3. Blood Chemistry
2.4. Dietary Glycemic Index (DGI) and Dietary Glycemic Load (DGL)
2.5. MiR Array for Screening Circulating miR
2.6. Real Time Quantitative PCR (RT-qPCR) for Validation
2.7. Statistics
3. Results
3.1. Baseline Characteristics and Changes in Clinical Parameters
3.2. Comparison of Macronutrient Intake and Food Consumption between the Two Diet Groups
3.3. DGI and DGL
3.4. MiR Screening
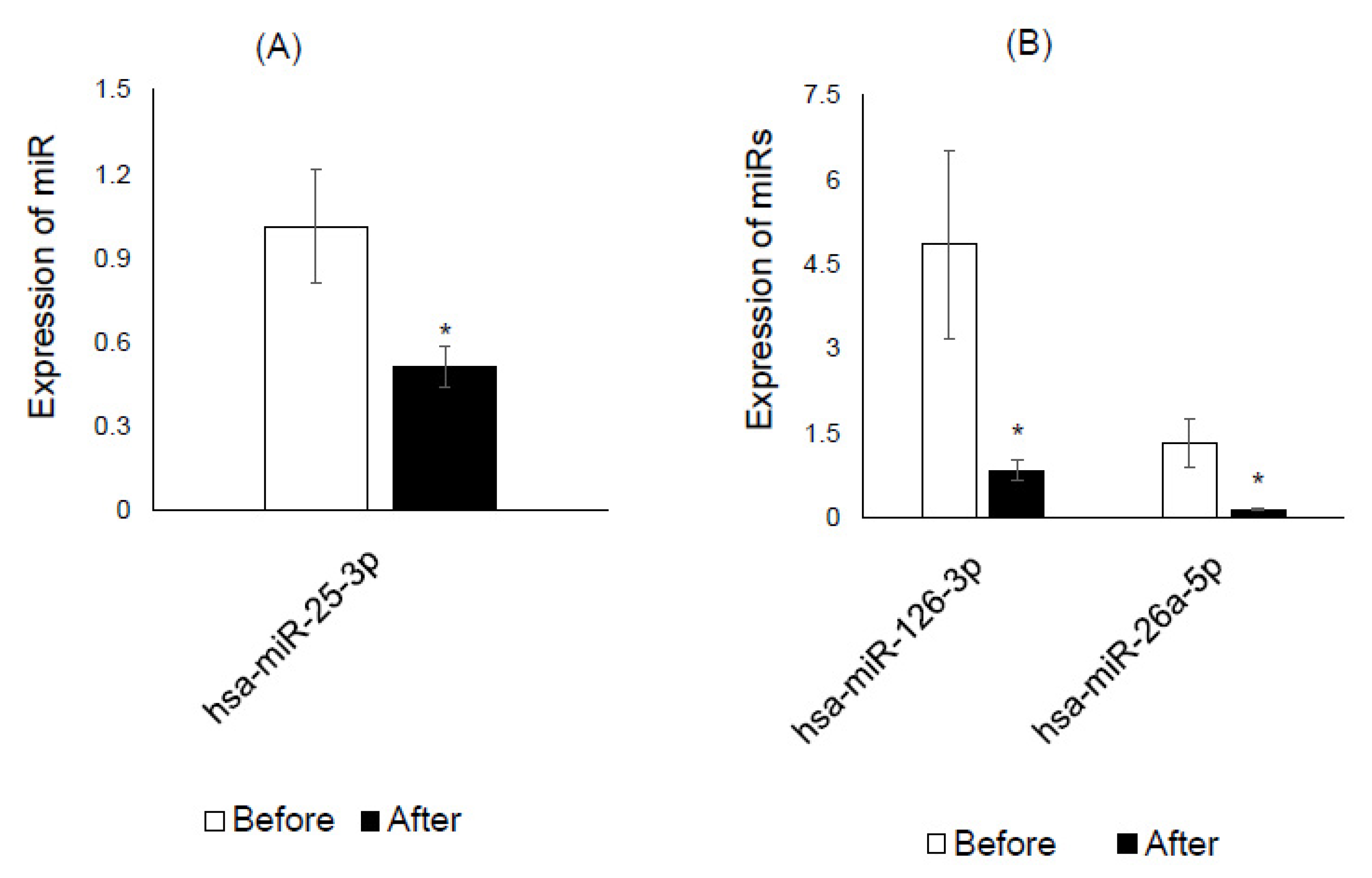
3.5. Validation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Kim, S.H.; Kim, M.S.; Lee, M.S.; Park, Y.S.; Lee, H.J.; Kang, S.A.; Lee, S.H.; Lee, K.E.; Yang, H.J.; Kim, H.J.; et al. Korean diet: Characteristics and historical background. J. Ethn. Foods 2016, 3, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.A.; Shin, S.; Ha, K.; Hwang, Y.; Park, Y.H.; Kang, M.S.; Joung, H. Effect of a balanced Korean diet on metabolic risk factors among overweight/obese Korean adults: A randomized controlled trial. Eur. J. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Jo, I. Grains, vegetables, and fish dietary pattern is inversely associated with the risk of metabolic syndrome in South korean adults. J. Am. Diet. Assoc. 2011, 111, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.J.; Park, S.H.; Choi, E.K.; Cha, Y.S.; Cho, B.H.; Kim, Y.G.; Kim, M.G.; Song, W.O.; Park, T.S.; Ko, J.K.; et al. Beneficial effects of Korean traditional diets in hypertensive and type 2 diabetic patients. J. Med. Food 2014, 17, 161–171. [Google Scholar] [CrossRef] [Green Version]
- Shin, J.H.; Jung, S.; Kim, S.A.; Kang, M.S.; Kim, M.S.; Joung, H.; Hwang, G.S.; Shin, D.M. Differential Effects of Typical Korean Versus American-Style Diets on Gut Microbial Composition and Metabolic Profile in Healthy Overweight Koreans: A Randomized Crossover Trial. Nutrients 2019, 11, 2450. [Google Scholar] [CrossRef] [Green Version]
- Schroeder, N.; Park, Y.H.; Kang, M.S.; Kim, Y.; Ha, G.K.; Kim, H.R.; Yates, A.A.; Caballero, B. A randomized trial on the effects of 2010 Dietary Guidelines for Americans and Korean diet patterns on cardiovascular risk factors in overweight and obese adults. J. Acad. Nutr. Diet. 2015, 115, 1083–1092. [Google Scholar] [CrossRef]
- Salmanidis, M.; Pillman, K.; Goodall, G.; Bracken, C. Direct transcriptional regulation by nuclear microRNAs. Int. J. Biochem. Cell Biol. 2014, 54, 304–311. [Google Scholar] [CrossRef]
- Lynn, F.C. Meta-regulation: MicroRNA regulation of glucose and lipid metabolism. Trends Endocrinol. Metab. 2009, 20, 452–459. [Google Scholar] [CrossRef]
- Lee, J.H.; Friso, S.; Choi, S.W. Epigenetic mechanisms underlying the link between non-alcoholic fatty liver diseases and nutrition. Nutrients 2014, 6, 3303–3325. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Xiao, Y.; Wu, X.; Jiang, L.; Yang, S.; Ding, Z.; Fang, Z.; Hua, H.; Kirby, M.S.; Shou, J. A circulating microRNA signature as noninvasive diagnostic and prognostic biomarkers for nonalcoholic steatohepatitis. BMC Genom. 2018, 19, 188. [Google Scholar] [CrossRef] [Green Version]
- Parr, E.B.; Camera, D.M.; Burke, L.M.; Phillips, S.M.; Coffey, V.G.; Hawley, J.A. Circulating MicroRNA Responses between ‘High’ and ‘Low’ Responders to a 16-Wk Diet and Exercise Weight Loss Intervention. PLoS ONE 2016, 11, e0152545. [Google Scholar] [CrossRef] [PubMed]
- Assmann, T.S.; Riezu-Boj, J.I.; Milagro, F.I.; Martinez, J.A. Circulating adiposity-related microRNAs as predictors of the response to a low-fat diet in subjects with obesity. J. Cell Mol. Med. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ben-Moshe, N.B.; Avraham, R.; Kedmi, M.; Zeisel, A.; Yitzhaky, A.; Yarden, Y.; Domany, E. Context-specific microRNA analysis: Identification of functional microRNAs and their mRNA targets. Nucleic. Acids. Res. 2012, 40, 10614–10627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mantilla-Escalante, D.C.; de Las Hazas, M.C.L.; Gil-Zamorano, J.; Del Pozo-Acebo, L.; Crespo, M.C.; Martin-Hernandez, R.; Del Saz, A.; Tome-Carneiro, J.; Cardona, F.; Cornejo-Pareja, I.; et al. Postprandial Circulating miRNAs in Response to a Dietary Fat Challenge. Nutrients 2019, 11, 1326. [Google Scholar] [CrossRef] [Green Version]
- Soda, N.; Rehm, B.H.A.; Sonar, P.; Nguyen, N.T.; Shiddiky, M.J.A. Advanced liquid biopsy technologies for circulating biomarker detection. J. Mater. Chem. B 2019, 7, 6670–6704. [Google Scholar] [CrossRef]
- Setti, G.; Pezzi, M.E.; Viani, M.V.; Pertinhez, T.A.; Cassi, D.; Magnoni, C.; Bellini, P.; Musolino, A.; Vescovi, P.; Meleti, M. Salivary MicroRNA for Diagnosis of Cancer and Systemic Diseases: A Systematic Review. Int. J. Mol. Sci. 2020, 21, 907. [Google Scholar] [CrossRef] [Green Version]
- Rapado-Gonzalez, O.; Majem, B.; Muinelo-Romay, L.; Alvarez-Castro, A.; Santamaria, A.; Gil-Moreno, A.; Lopez-Lopez, R.; Suarez-Cunqueiro, M.M. Human salivary microRNAs in Cancer. J. Cancer 2018, 9, 638–649. [Google Scholar] [CrossRef] [Green Version]
- Wong, D.T. Salivary extracellular noncoding RNA: Emerging biomarkers for molecular diagnostics. Clin. Ther. 2015, 37, 540–551. [Google Scholar] [CrossRef] [Green Version]
- KR, O.L.; Glynn, C.L. Investigating the Isolation and Amplification of microRNAs for Forensic Body Fluid Identification. Microrna 2018, 7, 187–194. [Google Scholar] [CrossRef] [Green Version]
- Shin, P.-K.; Chun, S.; Kim, M.S.; Park, S.-J.; Kim, M.J.; Kwon, D.Y.; Kim, K.; Lee, H.-J.; Choi, S.-W. Traditional Korean diet can alter the urine organic acid profile, which may reflect the metabolic influence of the diet. J. Nutr. Health 2020, 53, 231–243. [Google Scholar] [CrossRef]
- Du, H.; van der Daphne, A.L.; van Bakel, M.M.; van der Kallen, C.J.; Blaak, E.E.; van Greevenbroek, M.M.; Jansen, E.H.; Nijpels, G.; Stehouwer, C.D.; Dekker, J.M.; et al. Glycemic index and glycemic load in relation to food and nutrient intake and metabolic risk factors in a Dutch population. Am. J. Clin. Nutr. 2008, 87, 655–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murakami, K.; Sasaki, S.; Takahashi, Y.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Reproducibility and relative validity of dietary glycaemic index and load assessed with a self-administered diet-history questionnaire in Japanese adults. Br. J. Nutr. 2008, 99, 639–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, S.; Choi, H.; Lee, S.; Park, J.M.; Kim, B.R.; Paik, H.Y.; Song, Y. Establishing a table of glycemic index values for common Korean foods and an evaluation of the dietary glycemic index among the Korean adult population. Korean J. Nutr. 2012, 45, 80–93. [Google Scholar] [CrossRef]
- Nielsen, L.B.; Wang, C.; Sorensen, K.; Bang-Berthelsen, C.H.; Hansen, L.; Andersen, M.L.; Hougaard, P.; Juul, A.; Zhang, C.Y.; Pociot, F.; et al. Circulating levels of microRNA from children with newly diagnosed type 1 diabetes and healthy controls: Evidence that miR-25 associates to residual beta-cell function and glycaemic control during disease progression. Exp. Diabetes Res. 2012, 2012, 896362. [Google Scholar] [CrossRef] [Green Version]
- Demirsoy, I.H.; Ertural, D.Y.; Balci, S.; Cinkir, U.; Sezer, K.; Tamer, L.; Aras, N. Profiles of Circulating MiRNAs Following Metformin Treatment in Patients with Type 2 Diabetes. J. Med. Biochem. 2018, 37, 499–506. [Google Scholar] [CrossRef]
- de Candia, P.; Spinetti, G.; Specchia, C.; Sangalli, E.; La Sala, L.; Uccellatore, A.; Lupini, S.; Genovese, S.; Matarese, G.; Ceriello, A. A unique plasma microRNA profile defines type 2 diabetes progression. PLoS ONE 2017, 12, e0188980. [Google Scholar] [CrossRef] [Green Version]
- Zhang, T.; Li, L.; Shang, Q.; Lv, C.; Wang, C.; Su, B. Circulating miR-126 is a potential biomarker to predict the onset of type 2 diabetes mellitus in susceptible individuals. Biochem. Biophys. Res. Commun. 2015, 463, 60–63. [Google Scholar] [CrossRef]
- DiMarco, D.M.; Fernandez, M.L. The Regulation of Reverse Cholesterol Transport and Cellular Cholesterol Homeostasis by MicroRNAs. Biology 2015, 4, 494–511. [Google Scholar] [CrossRef] [Green Version]
- Lv, Y.C.; Tang, Y.Y.; Peng, J.; Zhao, G.J.; Yang, J.; Yao, F.; Ouyang, X.P.; He, P.P.; Xie, W.; Tan, Y.L.; et al. MicroRNA-19b promotes macrophage cholesterol accumulation and aortic atherosclerosis by targeting ATP-binding cassette transporter A1. Atherosclerosis 2014, 236, 215–226. [Google Scholar] [CrossRef]
- Foley, N.H.; O’Neill, L.A. miR-107: A toll-like receptor-regulated miRNA dysregulated in obesity and type II diabetes. J. Leukoc Biol. 2012, 92, 521–527. [Google Scholar] [CrossRef]
- Prabu, P.; Rome, S.; Sathishkumar, C.; Aravind, S.; Mahalingam, B.; Shanthirani, C.S.; Gastebois, C.; Villard, A.; Mohan, V.; Balasubramanyam, M. Circulating MiRNAs of ‘Asian Indian Phenotype’ Identified in Subjects with Impaired Glucose Tolerance and Patients with Type 2 Diabetes. PLoS ONE 2015, 10, e0128372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGregor, R.A.; Choi, M.S. microRNAs in the regulation of adipogenesis and obesity. Curr. Mol. Med. 2011, 11, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Li, Z.; Zheng, Y.; Yan, M.; Cui, Y.; Jiang, J. Circulating microRNA-92a level predicts acute coronary syndrome in diabetic patients with coronary heart disease. Lipids Health Dis. 2019, 18, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, A.; Dougal, D.M.; Jenkins, W.; Greene, N.; Williams-DeVane, C.; Kimbro, K.S. Serum miR-17 levels are downregulated in obese, African American women with elevated HbA1c. J. Diabetes Metab. Disord. 2019, 18, 173–179. [Google Scholar] [CrossRef]
- Ye, D.; Zhang, T.; Lou, G.; Xu, W.; Dong, F.; Chen, G.; Liu, Y. Plasma miR-17, miR-20a, miR-20b and miR-122 as potential biomarkers for diagnosis of NAFLD in type 2 diabetes mellitus patients. Life Sci. 2018, 208, 201–207. [Google Scholar] [CrossRef]
- He, Y.; Ding, Y.; Liang, B.; Lin, J.; Kim, T.K.; Yu, H.; Hang, H.; Wang, K. A Systematic Study of Dysregulated MicroRNA in Type 2 Diabetes Mellitus. Int. J. Mol. Sci. 2017, 18, 456. [Google Scholar] [CrossRef] [PubMed]
- Cione, E.; La Torre, C.; Cannataro, R.; Caroleo, M.C.; Plastina, P.; Gallelli, L. Quercetin, Epigallocatechin Gallate, Curcumin, and Resveratrol: From Dietary Sources to Human MicroRNA Modulation. Molecules 2019, 25, 63. [Google Scholar] [CrossRef] [Green Version]
- Casabonne, D.; Benavente, Y.; Seifert, J.; Costas, L.; Armesto, M.; Arestin, M.; Besson, C.; Saberi Hosnijeh, F.; Duell, E.J.; Weiderpass, E.; et al. Serum levels of hsa-miR-16-5p, -29a-3p, -150-5p, -155-5p and -223-3p and subsequent risk of chronic lymphocytic leukemia in the EPIC study. Int. J. Cancer 2020. [Google Scholar] [CrossRef]
- Zhang, L.; Valencia, C.A.; Dong, B.; Chen, M.; Guan, P.J.; Pan, L. Transfer of microRNAs by extracellular membrane microvesicles: A nascent crosstalk model in tumor pathogenesis, especially tumor cell-microenvironment interactions. J. Hematol. Oncol. 2015, 8, 14. [Google Scholar] [CrossRef] [Green Version]
- Mononen, N.; Lyytikainen, L.P.; Seppala, I.; Mishra, P.P.; Juonala, M.; Waldenberger, M.; Klopp, N.; Illig, T.; Leiviska, J.; Loo, B.M.; et al. Whole blood microRNA levels associate with glycemic status and correlate with target mRNAs in pathways important to type 2 diabetes. Sci. Rep. 2019, 9, 8887. [Google Scholar] [CrossRef]
- Yoshizawa, J.M.; Schafer, C.A.; Schafer, J.J.; Farrell, J.J.; Paster, B.J.; Wong, D.T. Salivary biomarkers: Toward future clinical and diagnostic utilities. Clin. Microbiol. Rev. 2013, 26, 781–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiu, X.; Zhang, J.; Shi, W.; Liu, S.; Kang, M.; Chu, H.; Wu, D.; Tong, N.; Gong, W.; Tao, G.; et al. Circulating MicroRNA-26a in Plasma and Its Potential Diagnostic Value in Gastric Cancer. PLoS ONE 2016, 11, e0151345. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Chen, M.; Wu, W. Analysis of microRNA (miRNA) expression profiles reveals 11 key biomarkers associated with non-small cell lung cancer. World J. Surg. Oncol. 2017, 15, 175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salazar-Ruales, C.; Arguello, J.V.; Lopez-Cortes, A.; Cabrera-Andrade, A.; Garcia-Cardenas, J.M.; Guevara-Ramirez, P.; Peralta, P.; Leone, P.E.; Paz, Y.M.C. Salivary MicroRNAs for Early Detection of Head and Neck Squamous Cell Carcinoma: A Case-Control Study in the High Altitude Mestizo Ecuadorian Population. Biomed. Res. Int. 2018, 2018, 9792730. [Google Scholar] [CrossRef] [Green Version]
- Yamada, N.O.; Heishima, K.; Akao, Y.; Senda, T. Extracellular Vesicles Containing MicroRNA-92a-3p Facilitate Partial Endothelial-Mesenchymal Transition and Angiogenesis in Endothelial Cells. Int. J. Mol. Sci. 2019, 20, 4406. [Google Scholar] [CrossRef] [Green Version]
- Pothiwala, P.; Jain, S.K.; Yaturu, S. Metabolic syndrome and cancer. Metab. Syndr. Relat. Disord. 2009, 7, 279–288. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, E.J.; LeRoith, D. Obesity and Diabetes: The Increased Risk of Cancer and Cancer-Related Mortality. Physiol. Rev. 2015, 95, 727–748. [Google Scholar] [CrossRef] [Green Version]
- Kweon, S.S. Updates on Cancer Epidemiology in Korea, 2018. Chonnam. Med. J. 2018, 54, 90–100. [Google Scholar] [CrossRef] [Green Version]
- Zhou, K.; Liu, M.; Cao, Y. New Insight into microRNA Functions in Cancer: Oncogene-microRNA-Tumor Suppressor Gene Network. Front. Mol. Biosci. 2017, 4, 46. [Google Scholar] [CrossRef] [Green Version]

| Variable | Control Diet (n = 5) | K-Diet (n = 5) | p Value |
|---|---|---|---|
| Age (years) | 54.60 ± 0.87 | 52.80 ± 1.02 | 0.2165 |
| Weight (kg) | 66.48 ± 2.02 | 64.36 ± 2.12 | 0.4901 |
| Waist circumference (cm) | 90.60 ± 1.54 | 85.40 ± 3.64 | 0.2247 |
| Systolic BP (mmHg) | 130.80 ± 6.46 | 119.80 ± 4.00 | 0.1859 |
| Diastolic BP (mmHg) | 87.60 ± 4.08 | 78.20 ± 1.74 | 0.0670 |
| Heart rate (bpm) | 81.60 ± 2.84 | 74.80 ± 3.47 | 0.1673 |
| Total Cholesterol (mg/dL) | 209.40 ± 4.74 | 239.40 ± 15.14 | 0.1199 |
| LDL-Cholesterol (mg/dL) | 142.20 ± 5.40 | 138.40 ± 24.91 | 0.8881 |
| HDL-Cholesterol (mg/dL) | 46.56 ± 4.05 | 57.65 ± 3.40 | 0.3125 |
| Triglyceride (mg/dL) | 103.20 ± 12.99 | 237.80 ± 116.24 | 0.2165 |
| Fasting glucose (mg/dL) | 92.40 ± 4.15 | 93.40 ± 3.31 | 0.8554 |
| Insulin (mU/L) | 6.64 ± 1.05 | 10.46 ± 2.09 | 0.1415 |
| HOMA-IR | 1.48 ± 0.18 | 2.47 ± 0.55 | 0.143 |
| Variable | Control Diet | K-Diet | ||||
|---|---|---|---|---|---|---|
| Baseline | 2-Week | p Value | Baseline | 2-Week | p Value | |
| Weight (kg) | 66.48 ± 2.02 | 65.68 ± 1.97 | 0.9444 | 64.36 ± 2.12 | 63.36 ± 1.82 | 0.1481 |
| Waist circumference (cm) | 90.60 ± 1.54 | 88.20 ± 0.85 | 0.3224 | 85.40 ± 3.64 | 83.80 ± 2.05 | 0.5565 |
| Total cholesterol (mg/dL) | 209.40 ± 4.74 | 229.80 ± 8.12 | 0.1953 | 239.40 ± 15.14 | 198.20 ± 13.25 | 0.0163 |
| LDL-cholesterol (mg/dL) | 142.20 ± 5.40 | 146.60 ± 7.09 | 0.7568 | 138.40 ± 24.91 | 123.60 ± 13.05 | 0.5053 |
| HDL-cholesterol (mg/dL) | 46.56 ± 4.05 | 55.12 ± 5.53 | 0.0717 | 57.65 ± 3.40 | 49.52 ± 9.03 | 0.8180 |
| Triglyceride (mg/dL) | 103.20 ± 12.99 | 140.40 ± 16.10 | 0.1452 | 237.80 ± 116.24 | 125.40 ± 16.36 | 0.3600 |
| Fasting glucose (mg/dL) | 92.40 ± 4.15 | 89.60 ± 3.39 | 0.3719 | 93.40 ± 3.31 | 82.20 ± 3.92 | 0.1396 |
| Insulin (mU/L) | 6.64 ± 1.05 | 9.00 ± 1.20 | 0.5413 | 10.46 ± 2.09 | 7.40 ± 1.34 | 0.1023 |
| HOMA-IR | 1.48 ± 0.18 | 1.98 ± 0.24 | 0.129 | 2.47 ± 0.55 | 1.46 ± 0.20 | 0.143 |
| Nutrients | Control Diet (n = 5) | K-Diet (n = 5) | p Value |
|---|---|---|---|
| Energy (kcal) | 1775.5 ± 25.5 | 1740.2 ± 12.7 | NS |
| Carbohydrate (% of energy) | 57 ± 0.6 | 63.7 ± 0.4 | <0.0001 |
| Dietary glycemic index | 54.35 ± 0.53 | 49.81 ± 0.24 | <0.0001 |
| Dietary glycemic load | 139.17 ± 2.82 | 149.98 ± 1.60 | 0.0012 |
| Protein (% of energy) | 15.7 ± 0.2 | 17.1 ± 0.3 | <0.0001 |
| Animal based protein (% of energy) | 7.3 ± 0.3 | 4.9 ± 0.3 | <0.0001 |
| Plant based protein | 8.4 ± 0.1 | 12.2 ± 0.1 | <0.0001 |
| Fat (% of energy) | 27.4 ± 0.4 | 19.2 ± 0.3 | <0.0001 |
| Animal based fat (% of energy) | 10.4 ± 0.5 | 2.3 ± 0.2 | <0.0001 |
| Plant based fat (% of energy) | 17.1 ± 0.3 | 16.9 ± 0.3 | NS |
| Cholesterol (mg) | 447.3 ± 30 | 182.9 ± 11 | <0.0001 |
| Food Groups | Control Diet (n = 5) | K-Diet (n = 5) | p Value |
|---|---|---|---|
| Total grains | 217.4 ± 5.1 | 277.7 ± 3.9 | <0.0001 |
| Whole grains | 0.4 ± 0.1 | 267.9 ± 4.9 | <0.0001 |
| Vegetables and fruits | 405.1 ± 7 | 543.2 ± 10.3 | <0.0001 |
| Kimchi | 132.2 ± 4.3 | 160.9 ± 5.1 | <0.0001 |
| Legumes and tofu | 40 ± 4.6 | 63.4 ± 4.6 | 0.0004 |
| Nuts | 2.6 ± 0.6 | 21.4 ± 3.8 | <0.0001 |
| Fishes and shell | 35.4 ± 3.9 | 53.2 ± 5.3 | 0.0073 |
| Seaweeds | 15.7 ± 2.8 | 24.5 ± 3.9 | 0.0708 |
| Meats | 57.3 ± 4.6 | 10 ± 2.2 | <0.0001 |
| Red meats | 48.8 ± 4.2 | 5.4 ± 1.3 | <0.0001 |
| Eggs | 40.5 ± 4.1 | 7 ± 1.5 | <0.0001 |
| Processed foods | 21.9 ± 3.4 | 0 ± 0 | <0.0001 |
| Salad dressing including mayonnaise | 11.7 ± 0.6 | 0 ± 0 | <0.0001 |
| Diet Group | miRNA | Expression Change | Associated Conditions | References |
|---|---|---|---|---|
| Control diet | hsa-miR-25-3p | Down | Type 1 diabetes | [24] |
| hsa-miR-148a-3p | Up | Type 1 diabetes Type 2 diabetes | [24,25,26] | |
| K-diet | hsa-miR-126-3p | Down | Prediabetes Type 2 diabetes | [27] |
| hsa-miR-18a-5p | Down | Type 2 diabetes | [26] | |
| hsa-miR-19b-3p | Down | Gestational diabetes Cholesterol metabolism | [28,29] | |
| hsa-miR-107 | Down | Type 2 diabetes Obesity | [30] | |
| hsa-miR-148a-3p | Down | Type 1 diabetes Type 2 diabetes | [24,25,26] | |
| hsa-miR-26b-5p | Down | Type 2 diabetes | [25] | |
| hsa-miR-374a-5p | Down | Type 2 diabetes | [31] | |
| hsa-miR-26a-5p | Down | Type 1 diabetes | [24] |
| Diet Group | miRNA | Expression Change | Associated Disorders | References |
|---|---|---|---|---|
| Control diet | hsa-miR-25-3p | Down | Type 1 diabetes | [24] |
| hsa-miR-31-5p | Down | Adipogenesis Obesity | [32] | |
| hsa-miR-200a-3p | Up | Type 1 diabetes | [24] | |
| K-diet | hsa-miR-92-3p | Down | Type 2 diabetes Acute coronary syndrome | [33] |
| hsa-miR-17-3p | Down | Type 2 diabetes Obesity | [34] | |
| hsa-miR-25b-3p | Down | Type 1 diabetes | [24] | |
| hsa-miR-122a-5p | Down | Type 2 diabetes NAFLD | [35] | |
| hsa-miR-193a-5p | Down | Type 2 diabetes | [36] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, P.-K.; Kim, M.S.; Park, S.-J.; Kwon, D.Y.; Kim, M.J.; Yang, H.J.; Kim, S.-H.; Kim, K.; Chun, S.; Lee, H.-J.; et al. A Traditional Korean Diet Alters the Expression of Circulating MicroRNAs Linked to Diabetes Mellitus in a Pilot Trial. Nutrients 2020, 12, 2558. https://doi.org/10.3390/nu12092558
Shin P-K, Kim MS, Park S-J, Kwon DY, Kim MJ, Yang HJ, Kim S-H, Kim K, Chun S, Lee H-J, et al. A Traditional Korean Diet Alters the Expression of Circulating MicroRNAs Linked to Diabetes Mellitus in a Pilot Trial. Nutrients. 2020; 12(9):2558. https://doi.org/10.3390/nu12092558
Chicago/Turabian StyleShin, Phil-Kyung, Myung Sunny Kim, Seon-Joo Park, Dae Young Kwon, Min Jung Kim, Hye Jeong Yang, Soon-Hee Kim, KyongChol Kim, Sukyung Chun, Hae-Jeung Lee, and et al. 2020. "A Traditional Korean Diet Alters the Expression of Circulating MicroRNAs Linked to Diabetes Mellitus in a Pilot Trial" Nutrients 12, no. 9: 2558. https://doi.org/10.3390/nu12092558
APA StyleShin, P.-K., Kim, M. S., Park, S.-J., Kwon, D. Y., Kim, M. J., Yang, H. J., Kim, S.-H., Kim, K., Chun, S., Lee, H.-J., & Choi, S.-W. (2020). A Traditional Korean Diet Alters the Expression of Circulating MicroRNAs Linked to Diabetes Mellitus in a Pilot Trial. Nutrients, 12(9), 2558. https://doi.org/10.3390/nu12092558






