Headaches and Magnesium: Mechanisms, Bioavailability, Therapeutic Efficacy and Potential Advantage of Magnesium Pidolate
Abstract
:1. Background
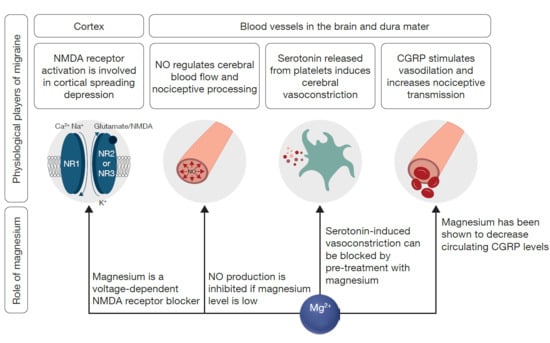
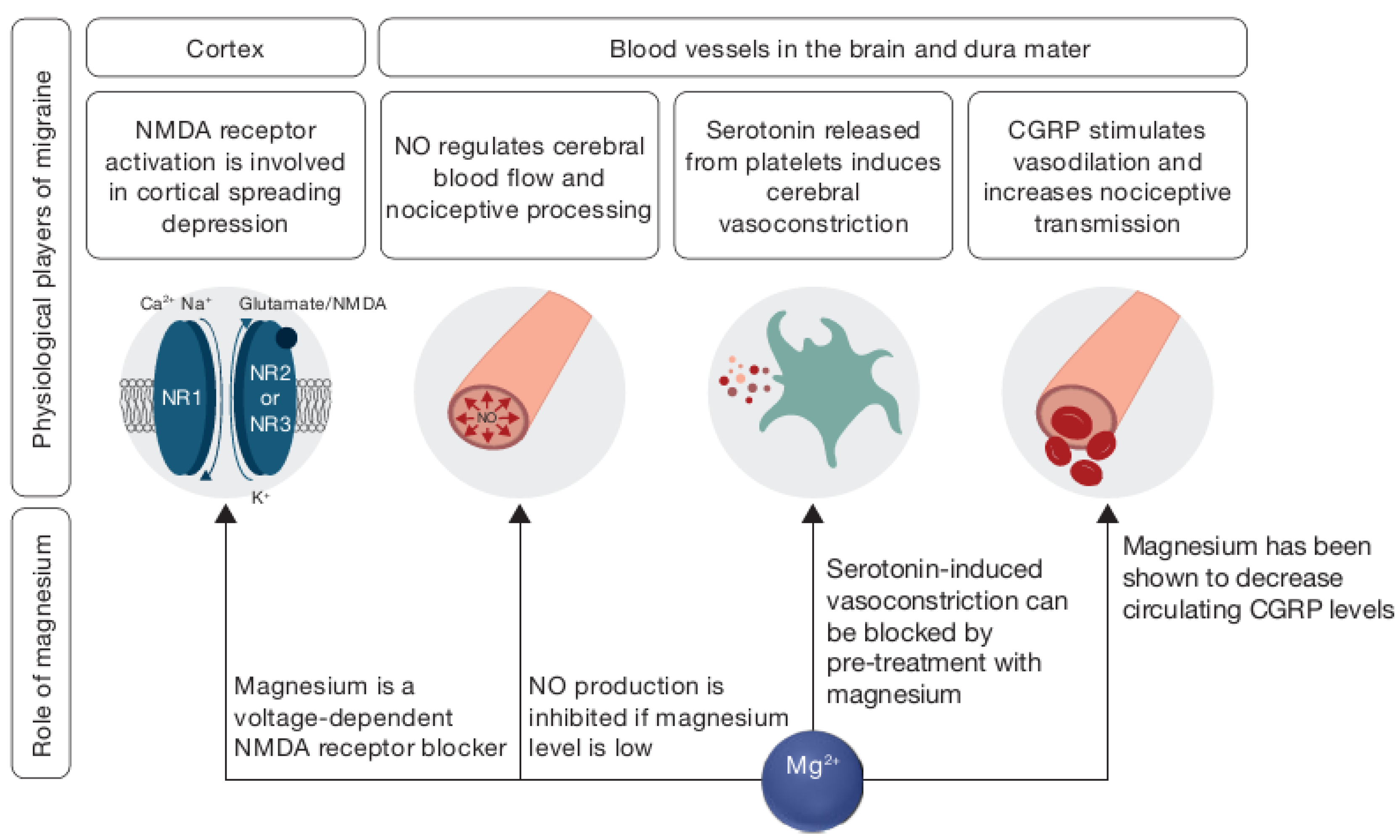
2. Why Should Magnesium Be Used to Treat Headaches?
3. Magnesium Supplementation—Therapeutic Efficacy
4. Magnesium Salt Biovailability—Pidolate Versus Other Salts
5. Magnesium Pidolate and Brain Penetration
6. Magnesium Pidolate and Headache: A Challenge for the Future
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jain, A.; Sethi, N.; Balbar, P. A clinical electroencephalographic and trace element study with special reference to zinc, copper and magnesium in serum and cerebrospinal fluid (CSF) in cases of migraine. J. Neurol. 1985, 232, S161. [Google Scholar]
- Ramadan, N.M.; Halvorson, H.; Vande-Linde, A.; Levine, S.R.; Helpern, J.A.; Welch, K.M. Low brain magnesium in migraine. Headache 1989, 29, 416–419. [Google Scholar] [CrossRef]
- Mauskop, A.; Altura, B.T.; Cracco, R.Q.; Altura, B.M. Intravenous magnesium sulfate relieves cluster headaches in patients with low serum ionized magnesium levels. Headache 1995, 35, 597–600. [Google Scholar] [CrossRef]
- Thomas, J.; Millot, J.M.; Sebille, S.; Delabroise, A.M.; Thomas, E.; Manfait, M.; Arnaud, M.J. Free and total magnesium in lymphocytes of migraine patients—Effect of magnesium-rich mineral water intake. Clin. Chim. Acta Int. J. Clin. Chem. 2000, 295, 63–75. [Google Scholar] [CrossRef]
- Sarchielli, P.; Coata, G.; Firenze, C.; Morucci, P.; Abbritti, G.; Gallai, V. Serum and Salivary Magnesium Levels in Migraine and Tension-Type Headache. Results in a Group of Adult Patients. Cephalalgia 1992, 12, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Trauninger, A.; Pfund, Z.; Koszegi, T.; Czopf, J. Oral magnesium load test in patients with migraine. Headache 2002, 42, 114–119. [Google Scholar] [CrossRef]
- Talebi, M.; Savadi-Oskouei, D.; Farhoudi, M.; Mohammadzade, S.; Ghaemmaghamihezaveh, S.; Hasani, A.; Hamdi, A. Relation between serum magnesium level and migraine attacks. Neuroscirnce 2011, 16, 320–323. [Google Scholar]
- Samaie, A.; Asghari, N.; Ghorbani, R.; Arda, J. Blood Magnesium levels in migraineurs within and between the headache attacks: A case control study. Pan Afr. Med. J. 2012, 11, 46. [Google Scholar]
- Assarzadegan, F.; Asgarzadeh, S.; Hatamabadi, H.R.; Shahrami, A.; Tabatabaey, A.; Asgarzadeh, M. Serum concentration of magnesium as an independent risk factor in migraine attacks: A matched case-control study and review of the literature. Int. Clin. Psychopharm. 2016, 31, 287–292. [Google Scholar] [CrossRef]
- The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia Int. J. Headache 2013, 33, 629–808. [CrossRef] [Green Version]
- Ravishankar, K. The art of history-taking in a headache patient. Ann. Indian Acad. Neurol. 2012, 15, S7–S14. [Google Scholar] [CrossRef] [PubMed]
- Maguire, M.E.; Cowan, J.A. Magnesium chemistry and biochemistry. Biometals 2002, 15, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Wacker, W. Magnesium and Man; Havard University Press: Cambridge, MA, USA, 1980; Volume 1. [Google Scholar]
- Whang, R.; Hampton, E.M.; Whang, D.D. Magnesium homeostasis and clinical disorders of magnesium deficiency. Ann. Pharmacother. 1994, 28, 220–226. [Google Scholar] [CrossRef]
- Elin, R.J. Assessment of magnesium status for diagnosis and therapy. Magnes. Res. 2010, 23, S194–S198. [Google Scholar] [CrossRef]
- Alfrey, A.C.; Miller, N.L. Bone magnesium pools in uremia. J. Clin. Investig. 1973, 52, 3019–3027. [Google Scholar] [CrossRef] [PubMed]
- Aikawa, J. Magnesium: Its Biological Significance; CRC Press: Boca Raton, FL, USA, 1981. [Google Scholar]
- Fine, K.D.; Ana, C.A.S.; Porter, J.L.; Fordtran, J.S. Intestinal absorption of magnesium from food and supplements. J. Clin. Investig. 1991, 88, 396–402. [Google Scholar] [CrossRef]
- Ayuk, J.; Gittoes, N.J. Contemporary view of the clinical relevance of magnesium homeostasis. Ann. Clin. Biochem. 2014, 51, 179–188. [Google Scholar] [CrossRef]
- Kolisek, M.; Sponder, G.; Pilchova, I.; Cibulka, M.; Tatarkova, Z.; Werner, T.; Racay, P. Magnesium Extravaganza: A Critical Compendium of Current Research into Cellular Mg(2+) Transporters Other than TRPM6/7. Rev. Physiol. Biochem. Pharmacol. 2019, 176, 65–105. [Google Scholar] [CrossRef]
- Botturi, A.; Ciappolino, V.; Delvecchio, G.; Boscutti, A.; Viscardi, B.; Brambilla, P. The Role and the Effect of Magnesium in Mental Disorders: A Systematic Review. Nutrients 2020, 12, 1661. [Google Scholar] [CrossRef]
- Boyle, N.B.; Lawton, C.; Dye, L. The Effects of Magnesium Supplementation on Subjective Anxiety and Stress-A Systematic Review. Nutrients 2017, 9, 429. [Google Scholar] [CrossRef] [Green Version]
- Witkowski, M.; Hubert, J.; Mazur, A. Methods of assessment of magnesium status in humans: A systematic review. Magnes. Res. 2011, 24, 163–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Workinger, J.; Doyle, R.; Bortz, J. Challenges in the Diagnosis of Magnesium Status. Nutrients 2018, 10, 1202. [Google Scholar] [CrossRef] [PubMed]
- Greenway, D.C.; Hindmarsh, J.T.; Wang, J.; Khodadeen, J.A.; Hébert, P.C. Reference interval for whole blood ionized magnesium in a healthy population and the stability of ionized magnesium under varied laboratory conditions. Clin. Biochem. 1996, 29, 515–520. [Google Scholar] [CrossRef]
- Lowenstein, F.W.; Stanton, M.F. Serum magnesium levels in the United States, 1971-1974. J. Am. Coll. Nutr. 1986, 5, 399–414. [Google Scholar] [CrossRef] [PubMed]
- Nicar, M.J.; Pak, C.Y. Oral magnesium load test for the assessment of intestinal magnesium absorption. Application in control subjects, absorptive hypercalciuria, primary hyperparathyroidism, and hypoparathyroidism. Min. Electrolyte Metab. 1982, 8, 44–51. [Google Scholar]
- Jahnen-Dechent, W.; Ketteler, M. Magnesium basics. Clin. Kidney J. 2012, 5, i3–i14. [Google Scholar] [CrossRef] [Green Version]
- Xiong, W.; Liang, Y.; Li, X.; Liu, G.; Wang, Z. Erythrocyte intracellular Mg(2+) concentration as an index of recognition and memory. Sci. Rep. 2016, 6, 26975. [Google Scholar] [CrossRef] [Green Version]
- Blancquaert, L.; Vervaet, C.; Derave, W. Predicting and Testing Bioavailability of Magnesium Supplements. Nutrients 2019, 11, 1663. [Google Scholar] [CrossRef] [Green Version]
- Facchinetti, F.; Sances, G.; Borella, P.; Genazzani, A.R.; Nappi, G. Magnesium prophylaxis of menstrual migraine: Effects on intracellular magnesium. Headache 1991, 31, 298–301. [Google Scholar] [CrossRef]
- Peikert, A.; Wilimzig, C.; Kohne-Volland, R. Prophylaxis of migraine with oral magnesium: Results from a prospective, multi-center, placebo-controlled and double-blind randomized study. Cephalalgia 1996, 16, 257–263. [Google Scholar] [CrossRef]
- Pfaffenrath, V.; Wessely, P.; Meyer, C.; Isler, H.R.; Evers, S.; Grotemeyer, K.H.; Taneri, Z.; Soyka, D.; Gobel, H.; Fischer, M. Magnesium in the prophylaxis of migraine—A double-blind placebo-controlled study. Cephalalgia 1996, 16, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Schuchardt, J.P.; Hahn, A. Intestinal Absorption and Factors Influencing Bioavailability of Magnesium—An Update. Curr. Nutr. Food Sci. 2017, 13, 260–278. [Google Scholar] [CrossRef] [PubMed]
- Coudray, C.; Rambeau, M.; Feillet-Coudray, C.; Gueux, E.; Tressol, J.C.; Mazur, A.; Rayssiguier, Y. Study of magnesium bioavailability from ten organic and inorganic Mg salts in Mg-depleted rats using a stable isotope approach. Magnes. Res. 2005, 18, 215–223. [Google Scholar] [PubMed]
- Decollogne, S.; Tomas, A.; Lecerf, C.; Adamowicz, E.; Seman, M. NMDA receptor complex blockade by oral administration of magnesium: Comparison with MK-801. Pharmacol. Biochem. Behav. 1997, 58, 261–268. [Google Scholar] [CrossRef]
- De Franceschi, L.; Bachir, D.; Galacteros, F.; Tchernia, G.; Cynober, T.; Alper, S.; Platt, O.; Beuzard, Y.; Brugnara, C. Oral magnesium supplements reduce erythrocyte dehydration in patients with sickle cell disease. J. Clin. Investig. 1997, 100, 1847–1852. [Google Scholar] [CrossRef] [Green Version]
- Grazzi, L.; Andrasik, F.; Usai, S.; Bussone, G. Magnesium as a preventive treatment for paediatric episodic tension-type headache: Results at 1-year follow-up. Neurol. Sci. 2007, 28, 148–150. [Google Scholar] [CrossRef]
- Mauskop, A.; Altura, B.T.; Cracco, R.Q.; Altura, B.M. Intravenous magnesium sulphate relieves migraine attacks in patients with low serum ionized magnesium levels: A pilot study. Clin. Sci. 1995, 89, 633–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, A.C.; Pfeffer, B.K.; Lawson, M.R.; Sewell, K.A.; King, A.R.; Zehtabchi, S. Intravenous Magnesium Sulfate to Treat Acute Headaches in the Emergency Department: A Systematic Review. Headache 2019, 59, 1674–1686. [Google Scholar] [CrossRef]
- Gertsch, E.; Loharuka, S.; Wolter-Warmerdam, K.; Tong, S.; Kempe, A.; Kedia, S. Intravenous magnesium as acute treatment for headaches: A pediatric case series. J. Emerg. Med. 2014, 46, 308–312. [Google Scholar] [CrossRef] [Green Version]
- Mauskop, A. Intravenous Magnesium Sulfate to Treat Acute Headaches in the Emergency Department: A Systematic Review—A Comment. Headache 2020, 60, 624. [Google Scholar] [CrossRef]
- Lingam, I.; Robertson, N.J. Magnesium as a Neuroprotective Agent: A Review of Its Use in the Fetus, Term Infant with Neonatal Encephalopathy, and the Adult Stroke Patient. Dev. Neurosci. 2018, 40, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, A.E.; Sarlo, G.L.; Holton, K.F. The Role of Magnesium in Neurological Disorders. Nutrients 2018, 10, 730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lodi, R.; Iotti, S.; Cortelli, P.; Pierangeli, G.; Cevoli, S.; Clementi, V.; Soriani, S.; Montagna, P.; Barbiroli, B. Deficient energy metabolism is associated with low free magnesium in the brains of patients with migraine and cluster headache. Brain Res. Bull. 2001, 54, 437–441. [Google Scholar] [CrossRef]
- Pouteau, E.; Kabir-Ahmadi, M.; Noah, L.; Mazur, A.; Dye, L.; Hellhammer, J.; Pickering, G.; Dubray, C. Superiority of magnesium and vitamin B6 over magnesium alone on severe stress in healthy adults with low magnesemia: A randomized, single-blind clinical trial. PLoS ONE 2018, 13, e0208454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sartori, S.B.; Whittle, N.; Hetzenauer, A.; Singewald, N. Magnesium deficiency induces anxiety and HPA axis dysregulation: Modulation by therapeutic drug treatment. Neuropharmacology 2012, 62, 304–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun-Edelstein, C.; Mauskop, A. Role of magnesium in the pathogenesis and treatment of migraine. Expert Rev. Neurother. 2009, 9, 369–379. [Google Scholar] [CrossRef]
- Coan, E.J.; Collingridge, G.L. Magnesium ions block an N-methyl-D-aspartate receptor-mediated component of synaptic transmission in rat hippocampus. Neurosci. Lett. 1985, 53, 21–26. [Google Scholar] [CrossRef]
- Baudouin-Legros, M.; Dard, B.; Guicheney, P. Hyperreactivity of platelets from spontaneously hypertensive rats. Role of external magnesium. Hypertension 1986, 8, 694–699. [Google Scholar] [CrossRef] [Green Version]
- Altura, B.M.; Altura, B.T. Factors Affecting Responsiveness of Blood Vessels to Prostaglandins and Other Chemical Mediators of Injury and Shock; Raven Press: New York, NY, USA, 1982. [Google Scholar]
- Innerarity, S. Hypomagnesemia in acute and chronic illness. Crit. Care Nurs. Q. 2000, 23, 1–19. [Google Scholar] [CrossRef]
- Myrdal, U.; Leppert, J.; Edvinsson, L.; Ekman, R.; Hedner, T.; Nilsson, H.; Ringqvist, I. Magnesium sulphate infusion decreases circulating calcitonin gene-related peptide (CGRP) in women with primary Raynaud’s phenomenon. Clin. Physiol. 1994, 14, 539–546. [Google Scholar] [CrossRef]
- Foster, A.C.; Fagg, G.E. Neurobiology. Taking apart NMDA receptors. Nature 1987, 329, 395–396. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.F.; Gebrewold, A.; Zhang, A.; Altura, B.T.; Altura, B.M. Role of excitatory amino acids in regulation of rat pial microvasculature. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1994, 266, R158–R163. [Google Scholar] [CrossRef] [PubMed]
- Mody, I.; Lambert, J.D.; Heinemann, U. Low extracellular magnesium induces epileptiform activity and spreading depression in rat hippocampal slices. J. Neurophysiol. 1987, 57, 869–888. [Google Scholar] [CrossRef] [PubMed]
- Hou, H.; Wang, L.; Fu, T.; Papasergi, M.; Yule, D.I.; Xia, H. Magnesium Acts as a Second Messenger in the Regulation of NMDA Receptor-Mediated CREB Signaling in Neurons. Mol. Neurobiol. 2020. [Google Scholar] [CrossRef]
- Chiarello, D.I.; Marin, R.; Proverbio, F.; Coronado, P.; Toledo, F.; Salsoso, R.; Gutierrez, J.; Sobrevia, L. Mechanisms of the effect of magnesium salts in preeclampsia. Placenta 2018, 69, 134–139. [Google Scholar] [CrossRef]
- Murata, T.; Dietrich, H.H.; Horiuchi, T.; Hongo, K.; Dacey, R.G. Mechanisms of magnesium-induced vasodilation in cerebral penetrating arterioles. Neurosci. Res. 2016, 107, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Bigal, M.E.; Bordini, C.A.; Tepper, S.J.; Speciali, J.G. Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. Cephalalgia 2002, 22, 345–353. [Google Scholar] [CrossRef]
- Choi, H.; Parmar, N. The use of intravenous magnesium sulphate for acute migraine: Meta-analysis of randomized controlled trials. Eur. J. Emerg. Med. 2014, 21, 2–9. [Google Scholar] [CrossRef]
- Peters, J.A.; Hales, T.G.; Lambert, J.J. Divalent cations modulate 5-HT3 receptor-induced currents in N1E-115 neuroblastoma cells. Eur. J. Pharmacol. 1988, 151, 491–495. [Google Scholar] [CrossRef]
- Goldstein, S.; Zsotér, T.T. The effect of magnesium on the response of smooth muscle to 5-hydroxytryptamine. Br. J. Pharmacol. 1978, 62, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Salamat, S.; Ismail, K.M.K.; O’ Brien, S. Premenstrual syndrome. Obstet. Gynaecol. Reprod. Med. 2008, 18, 29–32. [Google Scholar] [CrossRef]
- Quaranta, S.; Buscaglia, M.A.; Meroni, M.G.; Colombo, E.; Cella, S. Pilot study of the efficacy and safety of a modified-release magnesium 250 mg tablet (Sincromag) for the treatment of premenstrual syndrome. Clin. Drug Investig. 2007, 27, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.F.; De Souza, M.C.; Vickers, M.F.; Abeyasekera, S.; Collins, M.L.; Trinca, L.A. Magnesium supplementation alleviates premenstrual symptoms of fluid retention. J. Women Health 1998, 7, 1157–1165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Van Den Eeden, S.K.; Ackerson, L.M.; Salk, S.E.; Reince, R.H.; Elin, R.J. Oral magnesium oxide prophylaxis of frequent migrainous headache in children: A randomized, double-blind, placebo-controlled trial. Headache 2003, 43, 601–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aloisi, P.; Marrelli, A.; Porto, C.; Tozzi, E.; Cerone, G. Visual evoked potentials and serum magnesium levels in juvenile migraine patients. Headache 1997, 37, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Koseoglu, E.; Talaslioglu, A.; Gonul, A.S.; Kula, M. The effects of magnesium prophylaxis in migraine without aura. Magnes. Res. 2008, 21, 101–108. [Google Scholar] [PubMed]
- Karimi, N.; Razian, A.; Heidari, M. The efficacy of magnesium oxide and sodium valproate in prevention of migraine headache: A randomized, controlled, double-blind, crossover study. Acta Neurol. Belg. 2019. [Google Scholar] [CrossRef]
- Von Luckner, A.; Riederer, F. Magnesium in Migraine Prophylaxis-Is There an Evidence-Based Rationale? A Systematic Review. Headache 2018, 58, 199–209. [Google Scholar] [CrossRef]
- Antonaci, F.; Dumitrache, C.; De Cillis, I.; Allena, M. A review of current European treatment guidelines for migraine. J. Headache Pain 2010, 11, 13–19. [Google Scholar] [CrossRef] [Green Version]
- Holland, S.; Silberstein, S.D.; Freitag, F.; Dodick, D.W.; Argoff, C.; Ashman, E. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 2012, 78, 1346–1353. [Google Scholar] [CrossRef] [Green Version]
- Sarchielli, P.; Granella, F.; Prudenzano, M.P.; Pini, L.A.; Guidetti, V.; Bono, G.; Pinessi, L.; Alessandri, M.; Antonaci, F.; Fanciullacci, M.; et al. Italian guidelines for primary headaches: 2012 revised version. J. Headache Pain 2012, 13, S31–S70. [Google Scholar] [CrossRef] [Green Version]
- Taubert, K. Magnesium in migraine. Results of a multicenter pilot study. Fortschr. Der Med. 1994, 112, 328–330. [Google Scholar]
- Bøhmer, T.; Røseth, A.; Holm, H.; Weberg-Teigen, S.; Wahl, L. Bioavailability of oral magnesium supplementation in female students evaluated from elimination of magnesium in 24-h urine. Magnes. Trace Elem. 1990, 9, 272–278. [Google Scholar] [PubMed]
- Koenig, K.; Padalino, P.; Alexandrides, G.; Pak, C.Y. Bioavailability of potassium and magnesium, and citraturic response from potassium-magnesium citrate. J. Urol. 1991, 145, 330–334. [Google Scholar] [CrossRef]
- Altura, B.T.; Wilimzig, C.; Trnovec, T.; Nyulassy, S.; Altura, B.M. Comparative effects of a Mg-enriched diet and different orally administered magnesium oxide preparations on ionized Mg, Mg metabolism and electrolytes in serum of human volunteers. J. Am. Coll. Nutr. 1994, 13, 447–454. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Massey, L.; Gales, S.K.; Dittus, K.; Campbell, K. Blood and urinary magnesium kinetics after oral magnesium supplements. Clin. Ther. 1992, 14, 678–687. [Google Scholar] [PubMed]
- Lindberg, J.S.; Zobitz, M.M.; Poindexter, J.R.; Pak, C.Y. Magnesium bioavailability from magnesium citrate and magnesium oxide. J. Am. Coll. Nutr. 1990, 9, 48–55. [Google Scholar] [CrossRef]
- Mühlbauer, B.; Schwenk, M.; Coram, W.M.; Antonin, K.H.; Etienne, P.; Bieck, P.R.; Douglas, F.L. Magnesium-L-aspartate-HCl and magnesium-oxide: Bioavailability in healthy volunteers. Eur. J. Clin. Pharmacol. 1991, 40, 437–438. [Google Scholar] [CrossRef]
- Firoz, M.; Graber, M. Bioavailability of US commercial magnesium preparations. Magnes. Res. 2001, 14, 257–262. [Google Scholar]
- Walker, A.F.; Marakis, G.; Christie, S.; Byng, M. Mg citrate found more bioavailable than other Mg preparations in a randomised, double-blind study. Magnes. Res. 2003, 16, 183–191. [Google Scholar]
- Zhang, X.; Del Gobbo, L.C.; Hruby, A.; Rosanoff, A.; He, K.; Dai, Q.; Costello, R.B.; Zhang, W.; Song, Y. The Circulating Concentration and 24-h Urine Excretion of Magnesium Dose- and Time-Dependently Respond to Oral Magnesium Supplementation in a Meta-Analysis of Randomized Controlled Trials. J. Nutr. 2016, 146, 595–602. [Google Scholar] [CrossRef] [Green Version]
- Farruggia, G.; Castiglioni, S.; Sargenti, A.; Marraccini, C.; Cazzaniga, A.; Merolle, L.; Iotti, S.; Cappadone, C.; Maier, J.A. Effects of supplementation with different Mg salts in cells: Is there a clue? Magnes. Res. 2014, 27, 25–34. [Google Scholar] [CrossRef] [Green Version]
- Montagne, A.; Barnes, S.R.; Sweeney, M.D.; Halliday, M.R.; Sagare, A.P.; Zhao, Z.; Toga, A.W.; Jacobs, R.E.; Liu, C.Y.; Amezcua, L.; et al. Blood-brain barrier breakdown in the aging human hippocampus. Neuron 2015, 85, 296–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandoval, K.E.; Witt, K.A. Blood-brain barrier tight junction permeability and ischemic stroke. Neurobiol. Dis. 2008, 32, 200–219. [Google Scholar] [CrossRef] [PubMed]
- Amin, F.M.; Hougaard, A.; Cramer, S.P.; Christensen, C.E.; Wolfram, F.; Larsson, H.B.W.; Ashina, M. Intact blood-brain barrier during spontaneous attacks of migraine without aura: A 3T DCE-MRI study. Eur. J. Neurol. 2017, 24, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Kim, M.; Choi, S.H.; You, S.H.; Yoo, R.E.; Kang, K.M.; Yun, T.J.; Lee, S.T.; Moon, J.; Shin, Y.W. Altered Vascular Permeability in Migraine-associated Brain Regions: Evaluation with Dynamic Contrast-enhanced MRI. Radiology 2019, 292, 713–720. [Google Scholar] [CrossRef]
- Mi, X.; Ran, L.; Chen, L.; Qin, G. Recurrent Headache Increases Blood-Brain Barrier Permeability and VEGF Expression in Rats. Pain Physician 2018, 21, E633–E642. [Google Scholar]
- Kaya, M.; Ahishali, B. The role of magnesium in edema and blood brain barrier disruption. In Magnesium in the Central Nervous System; Vink, R., Nechifor, M., Eds.; University of Adelaide Press: Adelaide, Australia, 2011. [Google Scholar]
- Maier, J.A.; Bernardini, D.; Rayssiguier, Y.; Mazur, A. High concentrations of magnesium modulate vascular endothelial cell behaviour in vitro. Biochim. Biophys. Acta 2004, 1689, 6–12. [Google Scholar] [CrossRef]
- Esen, F.; Erdem, T.; Aktan, D.; Orhan, M.; Kaya, M.; Eraksoy, H.; Cakar, N.; Telci, L. Effect of magnesium sulfate administration on blood-brain barrier in a rat model of intraperitoneal sepsis: A randomized controlled experimental study. Crit. Care 2005, 9, R18–R23. [Google Scholar] [CrossRef] [Green Version]
- Johnson, A.C.; Tremble, S.M.; Chan, S.L.; Moseley, J.; LaMarca, B.; Nagle, K.J.; Cipolla, M.J. Magnesium sulfate treatment reverses seizure susceptibility and decreases neuroinflammation in a rat model of severe preeclampsia. PLoS ONE 2014, 9, e113670. [Google Scholar] [CrossRef]
- Romeo, V.; Cazzaniga, A.; Maier, J.A.M. Magnesium and the blood-brain barrier in vitro: Effects on permeability and magnesium transport. Magnes. Res. 2019, 32, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; You, J.; Zhao, N.; Xu, H. Magnesium Regulates Endothelial Barrier Functions through TRPM7, MagT1, and S1P1. Adv. Sci. 2019, 6, 1901166. [Google Scholar] [CrossRef] [Green Version]
- Euser, A.G.; Cipolla, M.J. Magnesium sulfate for the treatment of eclampsia: A brief review. Stroke 2009, 40, 1169–1175. [Google Scholar] [CrossRef] [PubMed]
- Allena, M.; Steiner, T.J.; Sances, G.; Carugno, B.; Balsamo, F.; Nappi, G.; Andree, C.; Tassorelli, C. Impact of headache disorders in Italy and the public-health and policy implications: A population-based study within the Eurolight Project. J. Headache Pain 2015, 16, 100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, L.; Kitzes, R. Infrared spectroscopy and magnesium content of bone mineral in osteoporotic women. Isr. J. Med. Sci. 1981, 17, 1123–1125. [Google Scholar]
- Vormann, J. Magnesium: Nutrition and metabolism. Mol. Asp. Med. 2003, 24, 27–37. [Google Scholar] [CrossRef]

| Inorganic Magnesium Salts | Organic Magnesium Salts | Combinations/Different Formulations |
|---|---|---|
| Carbonate | Acetate | Citrate + hydrogen-l-glutamate |
| Chloride | Aspartate | Dicitrate |
| Oxide | Citrate | Glycinate lysinate chelate |
| Sulfate | Gluconate | Oxide + glycerophosphate |
| Lactate | Pyrrolidone carboxylic acid | |
| Pidolate | Trimagnesium dicitrate | |
| U-aspartate-hydrochloride-trihydrate |
| Year | Type of Headache | Number of Patients | Outcome | Reference |
|---|---|---|---|---|
| 1985 | Migraine | 57 adults | Reduced magnesium levels in cerebrospinal fluid | [1] |
| 1989 | Migraine | 11 adults | Reduced magnesium levels in the brain | [2] |
| 1995 | Cluster | 22 adults | Up to 50% of migraine patients were found to be magnesium-deficient | [3] |
| 2000 | Migraine | 29 adults plus 18 healthy controls | Total magnesium in erythrocytes significantly increased compared with healthy controls | [4] |
| 2002 | Tension/migraine | 25 adults plus 20 healthy controls | Reduced magnesium levels in serum and saliva | [5] |
| 2002 | Migraine | 20 adults plus 20 healthy controls | Increased systemic retention of magnesium vs. controls | [6] |
| 2011 | Migraine | 140 adults plus 140 healthy controls | Total serum magnesium levels significantly lower vs. controls | [7] |
| 2012 | Migraine | 50 adults plus 50 healthy controls | Total serum magnesium levels significantly lower vs. controls | [8] |
| 2016 | Acute migraine | 40 adults plus 40 healthy controls | Decreased magnesium indicates a 35-fold increased risk of acute migraine | [9] |
| Type of Study | Author/Year | Study Length | Country | Type of Headache | Number of Patients | Magnesium Salt | Efficacy Outcome | Safety Outcome | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Children | |||||||||
| Multi-arm | Aloisi, 1997 | 20 days | Italy | Tension, migraine | 60 male and female children 6–13 years | 1500 mg daily oral magnesium pidolate | 20 days treatment sufficiently normalizes serum Magnesium levels in 90% of migraine patients | NR | [68] |
| Double-blind, placebo-controlled randomized trial | Wang, 2003 | 16 weeks | USA | Migraine | 118 male and female children 3–17 years (n = 60, placebo) | 9 mg/kg daily oral magnesium oxide | Significant reduction in headache days | NR | [67] |
| Open label trial | Grazzi, 2007 | 3 months | Italy | Tension | 45 male and female children 8–16 years | 2250 mg x2 daily oral magnesium pidolate | Headache days decreased by 69.9% | No significant side effects | [38] |
| Adults | |||||||||
| Double-blind, controlled, randomized, crossover trial | Karimi, 2019 | 24 weeks | Iran | Migraine | 63 adult male and females | 500 mg daily oral magnesium oxide (800 mg sodium valproate) | Magnesium oxide appears to be as effective as valproate in migraine prophylaxis without significant adverse effects | No side effects on top of headache symptoms | [70] |
| Systematic review (five clinical trials below) | Von Luckner, 2018 | 2–4 months | Various countries | Migraine | Five clinical trials of adult male and females | Different salts different doses | Possibly effective in preventing migraine. Safe and cost efficient | NA | [71] |
| 1. Double-blind, placebo-controlled randomized trial | Facchinetti, 1991 | 2 months | Italy | Menstrual migraine | 20 females | 360 mg daily oral magnesium pyrrolidone carboxylic acid | Significant reduction in the frequency of headache and total pain index | NR | [31] |
| 2. Double-blind, placebo-controlled randomized trial | Peikert, 1996 | 12 weeks | Germany | Migraine | 81 male and female adults (n = 38, placebo) | 600 mg daily oral trimagnesium dicitrate | Significant improvement in patients on active therapy | Diarrhoea and gastric complaints (mild and tolerable) | [32] |
| 3. Double-blind, placebo-controlled randomized trial | Pfaffenrath, 1996 | 12 weeks | Germany | Migraine | 69 male and female adults (n = 34, placebo) | 242 mg daily oral magnesium-u-aspartate-hydrochloride-trihydrate | No effect | Soft stool, diarrhoea (mild) | [33] |
| 4. Double-blind, placebo-controlled randomized trial | Koseoglu, 2008 | 3 months | Turkey | Migraine | 40 male and female adults (n = 10, placebo) | 600 mg daily oral magnesium citrate | Migraine attack frequency, severity, and P1 amplitude decreased | Diarrhoea, soft stools, gastric irritation (mild) | [69] |
| 5. Multicenter, crossover trial | Taubert, 1994 | 2 × 2 months | Germany | Migraine | 63 adult male and females | 600 mg daily oral trimagnesium dicitrate or placebo | Statistically significant reduction in the frequency of attacks compared with placebo | Diarrhoea | [75] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maier, J.A.; Pickering, G.; Giacomoni, E.; Cazzaniga, A.; Pellegrino, P. Headaches and Magnesium: Mechanisms, Bioavailability, Therapeutic Efficacy and Potential Advantage of Magnesium Pidolate. Nutrients 2020, 12, 2660. https://doi.org/10.3390/nu12092660
Maier JA, Pickering G, Giacomoni E, Cazzaniga A, Pellegrino P. Headaches and Magnesium: Mechanisms, Bioavailability, Therapeutic Efficacy and Potential Advantage of Magnesium Pidolate. Nutrients. 2020; 12(9):2660. https://doi.org/10.3390/nu12092660
Chicago/Turabian StyleMaier, Jeanette A., Gisele Pickering, Elena Giacomoni, Alessandra Cazzaniga, and Paolo Pellegrino. 2020. "Headaches and Magnesium: Mechanisms, Bioavailability, Therapeutic Efficacy and Potential Advantage of Magnesium Pidolate" Nutrients 12, no. 9: 2660. https://doi.org/10.3390/nu12092660
APA StyleMaier, J. A., Pickering, G., Giacomoni, E., Cazzaniga, A., & Pellegrino, P. (2020). Headaches and Magnesium: Mechanisms, Bioavailability, Therapeutic Efficacy and Potential Advantage of Magnesium Pidolate. Nutrients, 12(9), 2660. https://doi.org/10.3390/nu12092660