A Definition of “Regular Meals” Driven by Dietary Quality Supports a Pragmatic Schedule
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment
2.3. Data Collection
2.4. Instruments
2.5. Data Analyses
Development of Mealtime Regularity Score (mReg)
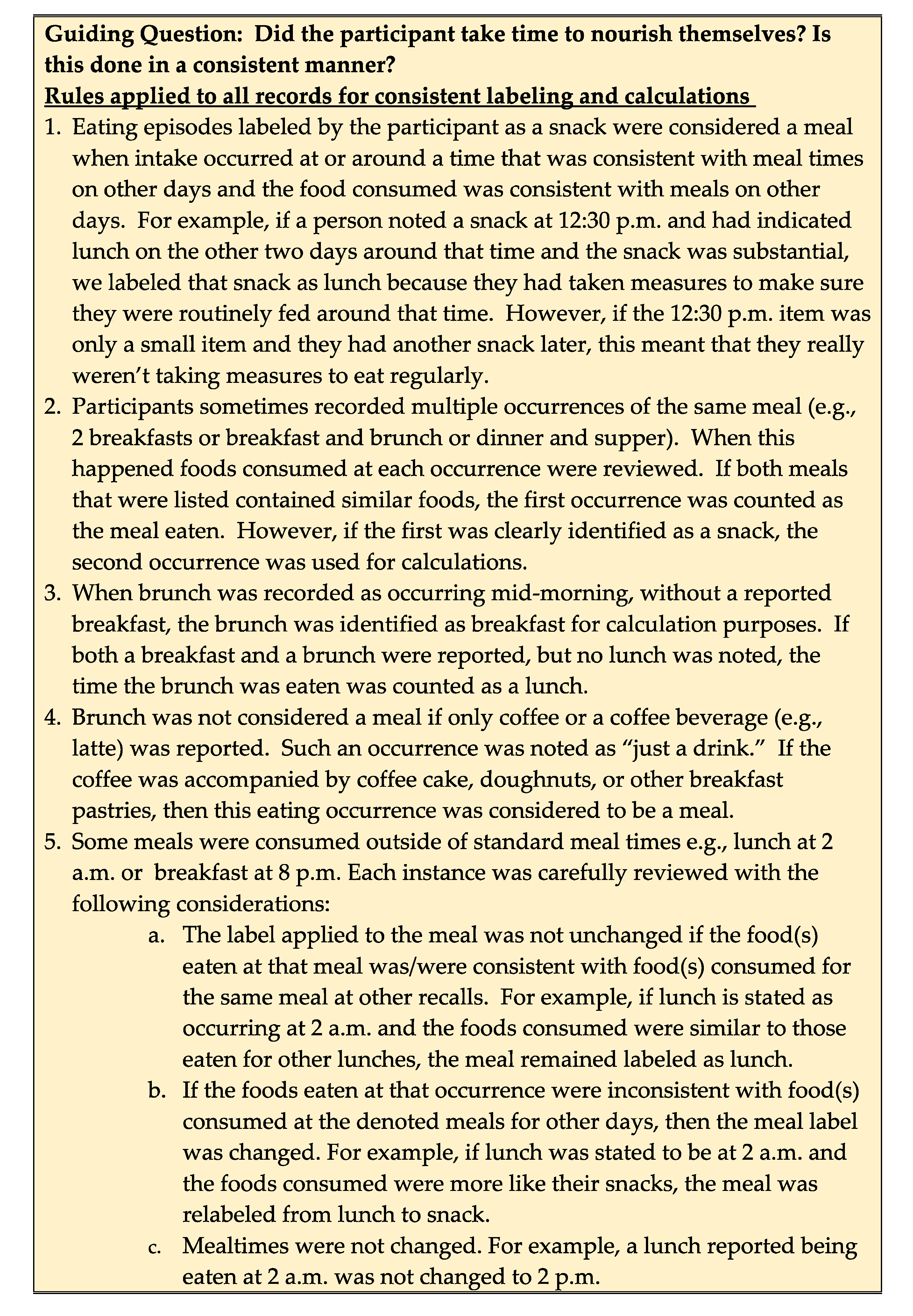
- For each meal, the time interval between first, second and third recalls was calculated and recorded. For nearly all participants, listing of meals and times was straightforward, e.g., recall 1 breakfast 8:00 a.m., recall 2 breakfast 8:30 a.m.; and recall 3 breakfast 3 8:30 a.m. However, a small number of participants provided unclear or conflicting entries, e.g., Recall 1 breakfast 6 a.m., Brunch 9 a.m., Lunch 12 p.m. For these and other ambiguous entries, a decision guide was developed to assure uniform decisions were applied across similar situations (Figure 1).
- An interval-driven scoring system was developed that provided higher scores to smaller intervals, i.e., greater regularity. One, two or three points were allocated to descriptors of rarely/never, often/sometimes and always, respectively. In all, three scoring schemes were developed. The first scoring scheme (version 1) allocated points based on meal-specific day-to-day intervals derived from informal interviews with project personnel about mealtime practices. This scheme resulted in a disproportionately high number of always designations for lunch and dinner. To facilitate a more proportionate distribution among the descriptors, a second scoring algorithm (version 2) was developed that more narrowly defined the descriptors for meals. For example, in version one, an interval of 0 to 60 min between the three breakfasts was denoted as always; this was changed to 0 to 30 min in version 2. However, several breakfast intervals were just a few minutes over the 30 min cutoff for version 2 breakfast, prompting concern that version 2 was too rigid for breakfast. Therefore, a third scoring version was included that differed from version 2 only in having a slightly expanded interval for breakfast to be denoted as always regular. The frequency-driven descriptors of mealtime intervals for the three temporally specific scoring versions are detailed in Table 1.
- For each scoring version, based on the descriptor applied to the day-to-day time difference for each meal, participants received a score (from 1 to 3) each for breakfast, lunch and dinner. Meal-specific regularity scores were summed to produce a mealtime regularity score for each version (i.e., mReg1, mReg2, mReg3) that could range from 3 (least regular) to 9 (most regular).
3. Results
3.1. Description of Participants
3.2. Recall Day Patterns
3.3. mReg Characteristics and Association with Dietary Quality and BMI
3.4. Test–Retest Reliability
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 11 July 2020).
- Weight Concern. Fighting Obesity with Knowledge. Available online: http://www.weightconcern.com/?q=node/ (accessed on 11 July 2020).
- Food and Agriculture Organization of the United Nations. Food-Based Dietary Guidelines-Japan. Available online: http://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/Japan/en (accessed on 11 July 2020).
- Sowa, A.; Tobiasz-Adamczyk, B.; Topór-Madry, R.; Poscia, A.; La Milia, D.I. Predictors of healthy ageing: Public health policy targets. BMC Health Serv. Res. 2016, 16, 289. [Google Scholar] [CrossRef]
- Turer, C.B.; Stroo, M.; Brouwer, R.J.; Krause, K.M.; Lovelady, C.A.; Bastian, L.A.; Peterson, B.; Østbye, T. Do high-risk preschoolers or overweight mothers meet AAP-recommended behavioral goals for reducing obesity? Acad. Pediatr. 2013, 13, 243–250. [Google Scholar] [CrossRef] [Green Version]
- Lehto, R.; Ray, C.; Lahti-Koski, M.; Roos, E. Meal pattern and BMI in 9–11-year-old children in Finland. Public Health Nutr. 2010, 14, 1245–1250. [Google Scholar] [CrossRef] [Green Version]
- Larsen, S.C.; Heitmann, B.L. More Frequent Intake of Regular Meals and Less Frequent Snacking Are Weakly Associated with Lower Long-Term Gains in Body Mass Index and Fat Mass in Middle-Aged Men and Women. J. Nutr. 2019, 149, 824–830. [Google Scholar] [CrossRef]
- Eisenberg, M.E.; Neumark-Sztainer, D.; Fulkerson, J.A.; Story, M. Family Meals and Substance Use: Is There a Long-Term Protective Association? J. Adolesc. Health 2008, 43, 151–156. [Google Scholar] [CrossRef]
- Rijlaarsdam, J.; Tiemeier, H.; Ringoot, A.P.; Ivanova, M.Y.; Jaddoe, V.W.V.; Verhulst, F.C.; Roza, S.J. Early family regularity protects against later disruptive behavior. Eur. Child Adolesc. Psychiatry 2015, 25, 781–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pot, G.K.; Almoosawi, S.; Stephen, A.M. Meal irregularity and cardiometabolic consequences: Results from observational and intervention studies. Proc. Nutr. Soc. 2016, 75, 475–486. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.-P.; Ard, J.; Baskin, M.L.; Chiuve, S.E.; Johnson, H.M.; Kris-Etherton, P.; Varady, K. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation 2017, 135, e96–e121. [Google Scholar] [CrossRef] [PubMed]
- Esmaillzadeh, A.; Keshteli, A.H.; Feizi, A.; Zaribaf, F.; Feinle-Bisset, C.; Adibi, P. Patterns of diet-related practices and prevalence of gastroesophageal reflux disease. Neurogastroenterol. Motil. 2013, 25, 831-e638. [Google Scholar] [CrossRef]
- Keshteli, A.H.; Feizi, A.; Esmaillzadeh, A.; Zaribaf, F.; Feinle-Bisset, C.; Talley, N.J.; Adibi, P. Patterns of dietary behaviours identified by latent class analysis are associated with chronic uninvestigated dyspepsia. Br. J. Nutr. 2015, 113, 803–812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paoli, A.; Tinsley, G.M.; Bianco, A.; Moro, T. The Influence of Meal Frequency and Timing on Health in Humans: The Role of Fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagata, C.; Tamura, T.; Wada, K.; Konishi, K.; Goto, Y.; Nagao, Y.; Ishihara, K.; Yamamoto, S. Sleep duration, nightshift work, and the timing of meals and urinary levels of 8-isoprostane and 6-sulfatoxymelatonin in Japanese women. Chrono-Int. 2017, 34, 1187–1196. [Google Scholar] [CrossRef] [PubMed]
- Beyer-Westendorf, J.; Siegert, G. Of men and meals. J. Thromb. Haemost. 2015, 13, 943–945. [Google Scholar] [CrossRef]
- Medical Research Council. How Eating Feeds into the Body Clock. Available online: http://www.sciencedaily.com/releases/2019/04/190425143607.htm (accessed on 11 July 2020).
- Roßbach, S.; Diederichs, T.; Nöthlings, U.; Buyken, A.; Alexy, U. Relevance of chronotype for eating patterns in adolescents. Chrono-Int. 2017, 35, 336–347. [Google Scholar] [CrossRef]
- Dashti, H.S.; Merino, J.; Lane, J.M.; Song, Y.; Smith, C.E.; Tanaka, T.; McKeown, N.M.; Tucker, C.; Sun, D.; Bartz, T.M.; et al. Genome-wide association study of breakfast skipping links clock regulation with food timing. Am. J. Clin. Nutr. 2019, 110, 473–484. [Google Scholar] [CrossRef]
- Jääskeläinen, A.; Schwab, U.; Kolehmainen, M.; Kaakinen, M.; Savolainen, M.J.; Froguel, P.; Cauchi, S.; Järvelin, M.-R.; Laitinen, J. Meal Frequencies Modify the Effect of Common Genetic Variants on Body Mass Index in Adolescents of the Northern Finland Birth Cohort. PLoS ONE 2013, 8, e73802. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Hannan, P.J.; Story, M.; Croll, J.; Perry, C. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. J. Am. Diet. Assoc. 2003, 103, 317–322. [Google Scholar] [CrossRef]
- Leech, R.M.; Worsley, A.; Timperio, A.; McNaughton, S.A. Understanding meal patterns: Definitions, methodology and impact on nutrient intake and diet quality. Nutr. Res. Rev. 2015, 28, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Berg, M.C.; Forslund, H.B. The Influence of Portion Size and Timing of Meals on Weight Balance and Obesity. Curr. Obes. Rep. 2015, 4, 11–18. [Google Scholar] [CrossRef]
- Miller, D.P.; Waldfogel, J.; Han, W.-J. Family Meals and Child Academic and Behavioral Outcomes. Child Dev. 2012, 83, 2104–2120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmerman, A.R.; Johnson, L.A.; Brunstrom, J.M. Assessing “chaotic eating” using self-report and the UK Adult National Diet and Nutrition Survey: No association between BMI and variability in meal or snack timings. Physiol. Behav. 2018, 192, 64–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lennernäs, M.; Andersson, I. Food-based Classification of Eating Episodes (FBCE). Appetite 1999, 32, 53–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham-Sabo, L.; Lohse, B.; Smith, S.; Browning, R.; Strutz, E.; Nigg, C.R.; Balgopal, M.; Kelly, K.; Ruder, E. Fuel for Fun: A cluster-randomized controlled study of cooking skills, eating behaviors, and physical activity of 4th graders and their families. BMC Public Health 2016, 16, 444. [Google Scholar] [CrossRef] [Green Version]
- National Cancer Institute. Automated Self-Administered 24-Hour Dietary Assessment Tool. Available online: https://epi.grants.cancer.gov/asa24/ (accessed on 11 July 2020).
- Krall, J.S.; Lohse, B. Validation of a measure of the Satter eating competence model with low-income females. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 26. [Google Scholar] [CrossRef] [Green Version]
- Lohse, B. The Satter Eating Competence Inventory for Low-income persons is a valid measure of eating competence for persons of higher socioeconomic position. Appetite 2015, 87, 223–228. [Google Scholar] [CrossRef]
- Godleski, S.; Lohse, B.; Krall, J. Confirmatory factor analyses support a 4-factor structure of the Satter Eating Competence InventoryTM and migration of an internal regulation item to the eating attitudes subscale. J. Nutr. Educ. Behav. 2019, 51, 1003–1010. [Google Scholar] [CrossRef]
- Hughes, S.O.; Cross, M.B.; Hennessy, E.; Tovar, A.; Economos, C.D.; Power, T.G. Caregiver’s Feeding Styles Questionnaire. Establishing cutoff points. Appetite 2012, 58, 393–395. [Google Scholar] [CrossRef] [Green Version]
- Parks, E.P.; Kumanyika, S.; Moore, R.H.; Stettler, N.; Wrotniak, B.H.; Kazak, A. Influence of Stress in Parents on Child Obesity and Related Behaviors. Pediatrics 2012, 130, e1096–e1104. [Google Scholar] [CrossRef] [Green Version]
- Lohse, B.; Satter, E.; Horacek, T.; Gebreselassie, T.; Oakland, M.J. Measuring Eating Competence: Psychometric Properties and Validity of the ecSatter Inventory. J. Nutr. Educ. Behav. 2007, 39, S154–S166. [Google Scholar] [CrossRef]
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kant, A.K.; Graubard, B.I. Within-person comparison of eating behaviors, time of eating, and dietary intake on days with and without breakfast: NHANES 2005–2010. Am. J. Clin. Nutr. 2015, 102, 661–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uzhova, I.; Mullally, D.; Peñalvo, J.L.; Gibney, E.R. Regularity of Breakfast Consumption and Diet: Insights from National Adult Nutrition Survey. Nutrients 2018, 10, 1578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Cancer Institute. Division of Cancer Control and Population Sciences. ASA24Ⓡ Evaluation and Validation. Available online: https://epi.grants.cancer.gov/asa24/respondent/validation.html (accessed on 12 July 2020.).
- Pursey, K.; Burrows, T.; Stanwell, P.; Collins, C.E.; Bonn, S.; Kim, J.; Sarkin, A. How Accurate is Web-Based Self-Reported Height, Weight, and Body Mass Index in Young Adults? J. Med. Internet Res. 2014, 16, e4. [Google Scholar] [CrossRef]
- Maukonen, M.; Mannisto, S.; Tolonen, H. A comparison of measured versus self-reported anthropometrics for assessing obesity in adults: A literature review. Scand. J. Public Health 2018, 46, 565–579. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Olendzki, B.; Pagoto, S.; Hurley, T.G.; Magner, R.P.; Ockene, I.S.; Schneider, K.L.; Merriam, P.A.; Hébert, J.R. Number of 24-Hour Diet Recalls Needed to Estimate Energy Intake. Ann. Epidemiol. 2009, 19, 553–559. [Google Scholar] [CrossRef] [Green Version]

| Version | Meal | Frequency | Score | Frequency-Driven Description of Mealtime Intervals | Frequency n (%) | Mealtime Regularity Score |
|---|---|---|---|---|---|---|
| One (1) | Breakfast | always | 3 | 0–60 min between the three breakfasts, no exceptions. Cannot skip breakfasts and get this score. | 67 (47) | Mean (SD) 7.26 (1.60) Median 7.00 Range 3–9 Score Frequency 3 4 4 4 5 16 6 10 7 46 8 17 9 45 |
| often/sometimes | 2 | 0–90 min between the three breakfasts and no breakfasts skipped OR 60 min between two breakfasts and skipped one breakfast | 21 (15) | |||
| rarely/never | 1 | 60–90 min between two breakfasts, but the third breakfast was >90 min from the other two OR was skipped; OR >90 min between two or more breakfasts (regardless of what the third breakfast was); OR two or more breakfasts were skipped. | 54 (38) | |||
| Lunch | always | 3 | 0–60 min between all lunches OR 60 min between two lunches and 120 min for the third meal. Cannot skip lunches and get this score. | 95 (67) | ||
| often/sometimes | 2 | Two lunches were 0–60 min apart, but one lunch was skipped OR 60–120 min between two or more lunches with no lunches skipped. | 15 (11) | |||
| rarely/never | 1 | 60–120 min between two lunches, but one lunch was > 120 min from the others or was skipped; OR if any lunches were >120 min apart from the rest; OR if two lunches were skipped. | 32 (23) | |||
| Dinner | always | 3 | 0–60 min between all dinners OR 60 min between two dinners and 120 min for the third meal. Cannot skip dinners and get this score. | 118 (83) | ||
| often/sometimes | 2 | Two dinners were 0–60 min apart, but one dinner was skipped OR 60–120 min between two dinners with no meals skipped. | 9 (6) | |||
| rarely/never | 1 | 60–120 min between two dinners, but one dinner was > 120 min from the others or was skipped; OR if any dinners were >120 min apart from the rest; OR if two dinners were skipped. | 15 (11) | |||
| Two (2) | Breakfast | always | 3 | 0–30 min between all breakfasts. Cannot skip breakfasts and get this score. | 37 (26) | Mean (SD) 5.54 (1.74) Median 6.00 Range 3–9 Score Frequency 3 21 4 28 5 21 6 23 7 30 8 13 9 6 |
| often/sometimes | 2 | 0–60 min between all breakfasts and no breakfasts were skipped; OR 0–30 min between two breakfasts and one breakfast skipped. | 35 (25) | |||
| rarely/never | 1 | One breakfast is >60 min from the rest OR if 0–60 min between two breakfasts and a third breakfast was skipped; OR if two breakfasts were skipped. | 70 (49) | |||
| Lunch | always | 3 | 0–30 min between all lunches. Cannot skip lunches and get this score. | 47 (33) | ||
| often/sometimes | 2 | 0–60 min between all lunches and no lunches were skipped; OR 0–30 min between two lunches and one lunch was skipped. | 38 (27) | |||
| rarely/never | 1 | One lunch is > 60 min from the rest OR if 0–60 min between two lunches and a third lunch was skipped; OR if two lunches were skipped. | 57 (40) | |||
| Dinner | always | 3 | 0–30 min between all dinners. Cannot skip dinners and get this score. | 42 (30) | ||
| often/sometimes | 2 | 0–60 min between all dinners and no dinners were skipped; OR 0–30 min between two dinners and one dinner was skipped. | 35 (25) | |||
| rarely/never | 1 | One dinner is >60 min from the rest OR if 0–60 min between two dinners and a third dinner was skipped; OR if two dinners were skipped. | 65 (46) | |||
| Three (3) | Breakfast | always | 3 | 0–45 min between all breakfasts. Cannot skip breakfasts and get this score | 42 (30) | Mean (SD) 5.57 (1.74) Median 6.00 Range 3–9 Score Frequency 3 21 4 26 5 22 6 23 7 30 8 14 9 6 |
| often/sometimes | 2 | 0–60 min between all breakfasts and no breakfasts were skipped; OR 0–45 min between two breakfasts and one breakfast skipped. | 30 (21) | |||
| rarely/never | 1 | If any meal is more than 60 min from the other two meals (skipping is not applied here); OR if 0–60 min between two meals, but one was skipped; OR if two or more meals were skipped. | 70 (49) | |||
| Lunch | always | 3 | 0–30 min between all lunches. Cannot skip lunches and get this score. | 47 (33) | ||
| often/sometimes | 2 | 0–60 min between all lunches and no lunches were skipped; OR 0–30 min between two lunches and one lunch was skipped | 38 (27) | |||
| rarely/never | 1 | One lunch is >60 min from the rest OR if 0–60 min between two lunches and a third lunch was skipped; OR if two lunches were skipped. | 57 (40) | |||
| Dinner | always | 3 | 0–30 min between all dinners. Cannot skip dinners and get this score. | 42 (30) | ||
| often/sometimes | 2 | 0–60 min between all dinners and no dinners were skipped; OR 0–30 min between two dinners and one dinner was skipped. | 35 (25) | |||
| rarely/never | 1 | One dinner is >60 min from the rest OR if 0–60 min between two dinners and a third dinner was skipped; OR if two dinners were skipped. | 65 (46) |
| Plans meals ahead of time | |
| Never | 1 (1) |
| Seldom | 5 (4) |
| Sometimes | 44 (31) |
| Most of the time | 66 (47) |
| Almost always | 26 (18) |
| Amount of time spent preparing a meal | |
| Do not prepare own meals | 2 (1) |
| <15 min | 4 (3) |
| 15–45 min | 121 (85) |
| >45 min | 15 (11) |
| Number of times/week prepared food at home | |
| 1–3 times | 7 (5) |
| 4–6 times | 74 (52) |
| Every day | 61 (43) |
| Reports eating regular meals | |
| Rarely/never | 2 (1) |
| Sometimes | 12 (9) |
| Often | 54 (38) |
| Always | 73 (52) |
| Reports eating a variety of foods | |
| Rarely/never | 5 (4) |
| Sometimes | 28 (20) |
| Often | 67 (48) |
| Always | 41 (29) |
| Feeling toward cooking | |
| I like to cook | 72 (51) |
| I do not mind cooking | 54 (38) |
| I do not like to cook | 15 (11) |
| Frequency of worrying about money for food | |
| Never | 46 (32) |
| Rarely | 54 (38) |
| Sometimes | 19 (13) |
| Often | 12 (9) |
| Always | 11 (8) |
| Parent feeding style 2 | |
| Uninvolved | 29 (22) |
| Indulgent | 40 (30) |
| Authoritarian | 40 (30) |
| Authoritative | 23 (17) |
| Eating competence (ecSI 2.0TM scores) 3,4 | |
| Total score (n = 135) Subscales Eating attitudes (n = 141) | 32.4 ± 8.1 (6–48) 12.9 ± 3.6 (0–18) |
| Internal regulation (n = 141) | 3.9 ± 1.4 (0–6) |
| Food acceptance (n = 139) | 5.3 ± 2.0 (1–9) |
| Contextual skills (n = 139) | 10.4 ± 2.8 (2–15) |
| Healthy eating index 4,5 | |
| Total | 58.6 ± 13.1. (22.0–89.1) |
| Energy (Kcal) | 1818.2 ± 573.7 (608.2–4422.5) |
| Total vegetable | 4.1 ± 1.2 (0.8–5.0) |
| Green beans | 3.0 ± 2.2 (0–5) |
| Total fruit | 2.7 ± 1.9 (0–5) |
| Whole fruit | 3.1 ± 2.1 (0–5) |
| Whole grain | 3.1 ± 3.0 (0–10) |
| Refined grain | 6.9 ± 3.0 (0–10) |
| Dairy | 6.5 ± 2.8 (0–10) |
| Total protein foods | 4.6 ± 0.8 (1.2–5) |
| Seafood and plants | 3.7 ± 1.8 (0–5) |
| Sodium | 2.9 ± 2.8 (0–10) |
| Fatty acids | 4.5 ± 3.1 (0–10) |
| Recall Pattern | Mealtime Regularity Score 1 | ||
|---|---|---|---|
| Version 1 | Version 2 | Version 3 | |
| Three weekdays (n = 32) | 8.03 (1.47) | 6.44 (1.70) | 6.50 (1.67) |
| Two weekdays/1 weekend day (n = 95) | 7.15 (1.52) | 5.29 (1.68) | 5.33 (1.69) |
| 1 weekday/2 weekend days (n = 15) | 6.33 (1.76) | 5.13 (1.64) | 5.13 (1.64) |
| p2 | 0.001 | 0.003 | 0.002 |
| Retest Mealtime Regularity Scores | |||
| Three weekdays (n = 11) | 8.27 (0.79) | 6.09 (1.70) | 6.18 (1.72) |
| Two weekdays/1 weekend day (n = 12) | 6.75 (2.26) | 4.92 (1.56) | 5.00 (1.65) |
| 1 weekday/2 weekend days (n = 5) | 6.20 (1.30) | 4.80 (1.30) | 4.80 (1.30) |
| p | 0.042 | NS | NS |
| Healthy Eating Index 3 | Mealtime Regularity Score 2 | ||
|---|---|---|---|
| Version 1 | Version 2 | Version 3 | |
| Total score | 0.26; 0.002 | 0.12; NS | 0.12; NS |
| Energy (Kcal) | 0.03; NS | −0.04; NS | −0.04; NS |
| Total vegetables | 0.04; NS | −0.03; NS | −0.02; NS |
| Green beans | 0.06; NS | −0.12; NS | −0.11; NS |
| Total fruit | 0.18; 0.035 | 0.12; NS | 0.13; NS |
| Whole fruit | 0.17; 0.040 | 0.09; NS | 0.10; NS |
| Whole grain | 0.13; NS | 0.009; NS | 0.001; NS |
| Dairy | 0.02; NS | 0.09; NS | 0.09; NS |
| Total protein | 0.15; NS 4 | 0.19; 0.027 | 0.18; 0.03 |
| Seafood plant | 0.15; NS 4 | 0.16; NS 4 | 0.15; NS 4 |
| Refined grain | 0.06; NS | −0.03; NS | −0.03; NS |
| Sodium | 0.03; NS | −0.05; NS | −0.05; NS |
| Fatty acids | 0.12; NS | 0.07; NS | 0.07; NS |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lohse, B.; Faulring, K.; Mitchell, D.C.; Cunningham-Sabo, L. A Definition of “Regular Meals” Driven by Dietary Quality Supports a Pragmatic Schedule. Nutrients 2020, 12, 2667. https://doi.org/10.3390/nu12092667
Lohse B, Faulring K, Mitchell DC, Cunningham-Sabo L. A Definition of “Regular Meals” Driven by Dietary Quality Supports a Pragmatic Schedule. Nutrients. 2020; 12(9):2667. https://doi.org/10.3390/nu12092667
Chicago/Turabian StyleLohse, Barbara, Kathryn Faulring, Diane C. Mitchell, and Leslie Cunningham-Sabo. 2020. "A Definition of “Regular Meals” Driven by Dietary Quality Supports a Pragmatic Schedule" Nutrients 12, no. 9: 2667. https://doi.org/10.3390/nu12092667






