Caregivers’ Role in the Effectiveness of Two Dutch School-Based Nutrition Education Programmes for Children Aged 7–12 Years Old
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measures
2.1.1. Primary Outcome Measures
Nutrition Knowledge
Fruit and Vegetable Intake
Health Promotion Behaviour
2.1.2. Other Measures
2.2. Statistical Analysis
3. Results
3.1. Caregivers’ HPB and Children’s FV Intake and Nutrition Knowledge
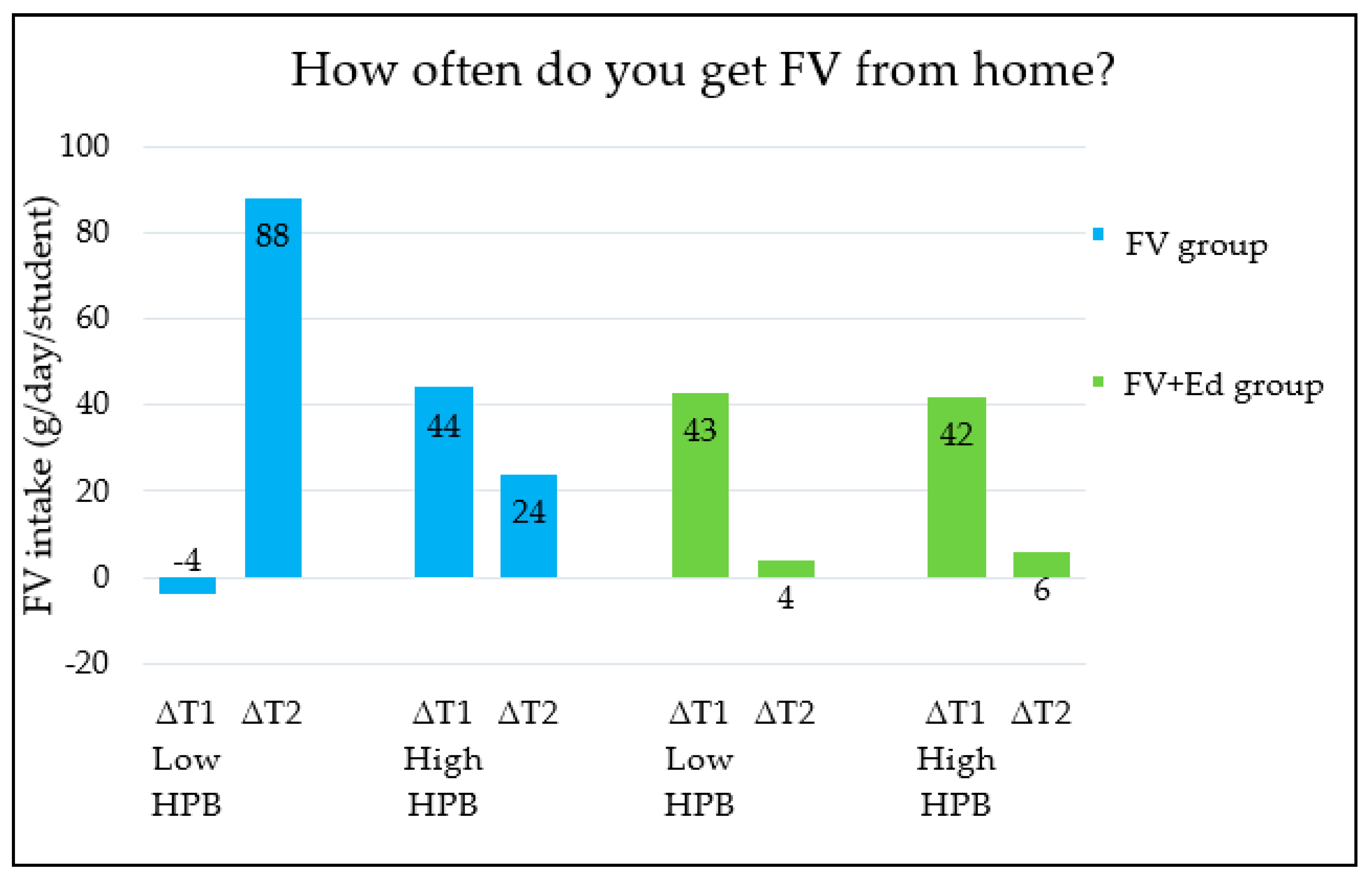
3.2. Contribution of Caregivers’ HPB to the Effectiveness of the Programmes
4. Discussion
4.1. The Association between Caregivers’ HPB and Children’s Healthy Eating Behaviour
4.2. The Contribution of Caregivers’ HPB to the Effectiveness of the Programmes
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Description of FV Provision Programme and Education Programme
References
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Increasing Fruit and Vegetable Consumption to Reduce the Risk of Noncommunicable Diseases 2019. Available online: who.int/elena/titles/fruit_vegetables_ncds/en/ (accessed on 23 June 2020).
- Boeing, H.; Bechthold, A.; Bub, A.; Ellinger, S.; Haller, D.; Kroke, A.; Leschik-Bonnet, E.; Müller, M.J.; Oberritter, H.; Schulze, M. Critical review: Vegetables and fruit in the prevention of chronic diseases. Eur. J. Nutr. 2012, 51, 637–663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Cauwenberghe, E.; Maes, L.; Spittaels, H.; van Lenthe, F.J.; Brug, J.; Oppert, J.-M.; De Bourdeaudhuij, I. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: Systematic review of published and ‘grey’ literature. Br. J. Nutr. 2010, 103, 781–797. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.; Christian, M.S.; Cleghorn, C.L.; Greenwood, D.C.; Cade, J.E. Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am. J. Clin. Nutr. 2012, 96, 889–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birch, L.L.; Fisher, J.A. Appetite and eating behavior in children. Pediatr. Clin. N. Am. 1995, 42, 931–953. [Google Scholar] [CrossRef]
- Fisher, J.O.; Birch, L.L. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. Am. J. Clin. Nutr. 1999, 69, 1264–1272. [Google Scholar] [CrossRef] [Green Version]
- Wind, M.; Bobelijn, K.; De Bourdeaudhuij, I.; Klepp, K.-I.; Brug, J. A qualitative exploration of determinants of fruit and vegetable intake among 10-and 11-year-old schoolchildren in the low countries. Ann. Nutr. Metab. 2005, 49, 228–235. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.; Gorely, T. Family correlates of fruit and vegetable consumption in children and adolescents: A systematic review. Public Health Nutr. 2009, 12, 267–283. [Google Scholar] [CrossRef]
- Hearn, M.D.; Baranowski, T.; Baranowski, J.; Doyle, C.; Smith, M.; Lin, L.S.; Resnicow, K. Environmental influences on dietary behavior among children: Availability and accessibility of fruits and vegetables enable consumption. J. Health Educ. 1998, 29, 26–32. [Google Scholar] [CrossRef]
- Hayman, L.L. The Dietary Intervention Study in Children (DISC): Progress and prospects for primary prevention. Prog. Cardiovasc. Nurs. 2003, 18, 4. [Google Scholar] [CrossRef]
- Fisher, J.O.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. J. Am. Diet. Assoc. 2002, 102, 58–64. [Google Scholar] [CrossRef]
- Stanek, K.; Abbott, D.; Cramer, S. Diet. quality and the eating environment of preschool children. J. Am. Diet. Assoc. 1990, 90, 1582–1584. [Google Scholar] [PubMed]
- Neumark-Sztainer, D.; Hannan, P.J.; Story, M.; Croll, J.; Perry, C. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. J. Am. Diet. Assoc. 2003, 103, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Quelly, S.B. Helping with meal preparation and children’s dietary intake: A literature review. J. School Nurs. 2019, 35, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Baumrind, D. The development of instrumental competence through socialisation. In Minnesota Symposium on Child Psychology; University of Minnesota Press: Minneapolis, MN, USA, 1973; Volume 7, 224p. [Google Scholar]
- Maccoby, E.; Martin, A. Socialization in the Context of the Family: Parent-Child Interaction; Handbook of Child Psychology Socialisation, Personality and Social Development; Wiley: Chichester, UK, 1983; pp. 1–102. [Google Scholar]
- Fisher, J.O.; Birch, L. Fat preferences and fat consumption of 3-to 5-year-old children are related to parental adiposity. J. Am. Diet. Assoc. 1995, 95, 759–764. [Google Scholar] [CrossRef]
- Darling, N.; Steinberg, L. Parenting style as context: An. integrative model. Psychol. Bull. 1993, 113, 487. [Google Scholar] [CrossRef]
- Martínez, I.; Garcia, F.; Fuentes, M.C.; Veiga, F.; Garcia, O.F.; Rodrigues, Y.; Cruise, E.; Serra, E. Researching parental socialisation styles across three cultural contexts: Scale ESPA29 bi-dimensional validity in Spain, Portugal, and Brazil. Int. J. Environ. Res. Public Health 2019, 16, 197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, C.; Duncanson, K.; Burrows, T. A systematic review investigating associations between parenting style and child feeding behaviours. J. Hum. Nutr. Diet. 2014, 27, 557–568. [Google Scholar] [CrossRef]
- Patrick, H.; Nicklas, T.; Hughes, S.O.; Morales, M. The benefits of authoritative feeding style: Caregiver feeding styles and children’s food consumption patterns. Appetite 2005, 44, 243–249. [Google Scholar] [CrossRef]
- Cullen, K.W.; Baranowski, T.; Rittenberry, L.; Cosart, C.; Owens, E.; Hebert, D.; de Moor, C. Socioenvironmental influences on children’s fruit, juice and vegetable consumption as reported by parents: Reliability and validity of measures. Public Health Nutr. 2000, 3, 345–356. [Google Scholar] [CrossRef] [Green Version]
- Anliker, J.A.; Laus, M.J.; Samonds, K.W.; Beal, V.A. Mothers‘ reports of their three-year-old children’s control over foods and involvement in food-related activities. J. Nutr. Educ. 1992, 24, 285–291. [Google Scholar] [CrossRef]
- Eppright, E.S.; Fox, H.; Fryer, B.; Lamkin, G.H.; Vivian, V.M. The North Central Regional Study of diets of preschool children. 2. Nutrition knowledge and attitudes of mothers. J. Home Econ. 1970, 62, 327–332. [Google Scholar]
- Gable, S.; Lutz, S. Household, parent, and child contributions to childhood obesity. Fam. Relat. 2000, 49, 293–300. [Google Scholar] [CrossRef]
- Zeinstra, G.G.; Koelen, M.A.; Kok, F.J.; van der Laan, N.; de Graaf, C. Parental child-feeding strategies in relation to Dutch children’s fruit and vegetable intake. Public Health Nutr. 2010, 13, 787–796. [Google Scholar] [CrossRef] [Green Version]
- Bucher, T.; Siegrist, M.; Van der Horst, K. Vegetable variety: An effective strategy to increase vegetable choice in children. Public Health Nutr. 2014, 17, 1232–1236. [Google Scholar] [CrossRef]
- Kremers, S.P.; Brug, J.; de Vries, H.; Engels, R.C. Parenting style and adolescent fruit consumption. Appetite 2003, 41, 43–50. [Google Scholar] [CrossRef]
- Morgan, E.H.; Schoonees, A.; Sriram, U.; Faure, M.; Seguin-Fowler, R.A. Caregiver involvement in interventions for improving children’s dietary intake and physical activity behaviors. Cochrane Database Syst. Rev. 2020, 1. [Google Scholar] [CrossRef] [Green Version]
- Racey, M.; O’Brien, C.; Douglas, S.; Marquez, O.; Hendrie, G.; Newton, G. Systematic review of school-based interventions to modify dietary behavior: Does intervention intensity impact effectiveness? J. School Health 2016, 86, 452–463. [Google Scholar] [CrossRef]
- Steunpunt Smaaklessen & EU-Schoolfruit. Smaaklessen. Available online: https://smaaklessen.nl/ (accessed on 7 September 2020).
- Steunpunt Smaaklessen & EU-Schoolfruit. EU-Schoolfruit. Available online: https://www.euschoolfruit.nl/ (accessed on 7 September 2020).
- Fries, M.; Velwijk, J.; Haveman-Nies, A.; Bemelmans, W.; Wijga, A. Onderzoek naar de inhoud van lunchtrommels. Voed. Nu 2011, 3, 14–16. [Google Scholar]
- Verdonschot, A.; de Vet, E.; van Rossum, J.; Mesch, A.; Collins, C.E.; Bucher, T.; Haveman-Nies, A. Education or Provision? A Comparison of Two School-Based Fruit and Vegetable Nutrition Education Programs in the Netherlands. Nutrients 2020, 12, 3280. [Google Scholar] [CrossRef]
- Battjes-Fries, M.C.; Haveman-Nies, A.; Renes, R.-J.; Meester, H.J.; van’t Veer, P. Effect of the Dutch school-based education programme ‘Taste Lessons’ on behavioural determinants of taste acceptance and healthy eating: A quasi-experimental study. Public Health Nutr. 2015, 18, 2231–2241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vereecken, C.; De Pauw, A.; Van Cauwenbergh, S.; Maes, L. Development and test–retest reliability of a nutrition knowledge questionnaire for primary-school children. Public Health Nutr. 2012, 15, 1630–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haraldsdóttir, J.; Thórsdóttir, I.; de Almeida, M.D.V.; Maes, L.; Rodrigo, C.P.; Elmadfa, I.; Andersen, L.F. Validity and reproducibility of a precoded questionnaire to assess fruit and vegetable intake in European 11-to 12-year-old schoolchildren. Ann. Nutr. Metab. 2005, 49, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Poelman, M.P.; Dijkstra, S.C.; Sponselee, H.; Kamphuis, C.B.; Battjes-Fries, M.C.; Gillebaart, M.; Seidell, J.C. Towards the measurement of food literacy with respect to healthy eating: The development and validation of the self perceived food literacy scale among an adult sample in the Netherlands. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 54. [Google Scholar] [CrossRef] [Green Version]
- Voedingscentrum. Gezond Eten. Available online: https://www.voedingscentrum.nl/nl/gezond-eten-met-de-schijf-van-vijf.aspx (accessed on 16 December 2020).
- Donders-Engelen, M.; Van der Heijden, L.; Hulshof, K. Maten, Gewichten en Codenummers 2003; Division of Human Nutrition; Wageningen University and TNO Nutrition: Zeist, The Netherlands, 2003. [Google Scholar]
- Van Rossum, C.T.; Fransen, H.P.; Verkaik-Kloosterman, J.; Buurma-Rethans, E.J.; Ocke, M.C. Dutch National Food Consumption Survey 2007-2010: Diet of Children and Adults Aged 7 to 69 years; RIVM: Utrecht, The Netherlands, 2011. [Google Scholar]
- RIVM. Overzicht recepten. Available online: https://docplayer.nl/25034497-Overzicht-recepten-nevo-online-2016-list-of-recipes-nevo-online-2016.html (accessed on 23 June 2020).
- Field, A.P.; Miles, J.; Field, Z. Discovering Statistics Using R; Sage: London, UK; Thousand Oaks, CA, USA; New Delhi, India; Singapore, 2012. [Google Scholar]
- Reinaerts, E.; de Nooijer, J.; van de Kar, A.; de Vries, N. Development of a school-based intervention to promote fruit and vegetable consumption. Health Educ. 2006, 106, 345–356. [Google Scholar] [CrossRef]
- Haddad, J.; Ullah, S.; Bell, L.; Leslie, E.; Magarey, A. The influence of home and school environments on children’s diet and physical activity, and body mass index: A structural equation modelling approach. Matern. Child Health J. 2018, 22, 364–375. [Google Scholar] [CrossRef]
- Blanchette, L.; Brug, J. Determinants of fruit and vegetable consumption among 6–12-year-old children and effective interventions to increase consumption. J. Hum. Nutr. Diet. 2005, 18, 431–443. [Google Scholar] [CrossRef]
- Van Der Horst, K.; Oenema, A.; Ferreira, I.; Wendel-Vos, W.; Giskes, K.; van Lenthe, F.; Brug, J. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ. Res. 2007, 22, 203–226. [Google Scholar] [CrossRef] [Green Version]
- Zarnowiecki, D.; Sinn, N.; Petkov, J.; Dollman, J. Parental nutrition knowledge and attitudes as predictors of 5–6-year-old children’s healthy food knowledge. Public Health Nutr. 2012, 15, 1284–1290. [Google Scholar] [CrossRef] [Green Version]
- Variyam, J.N.; Blaylock, J.; Lin, B.H.; Ralston, K.; Smallwood, D. Mother’s nutrition knowledge and children’s dietary intakes. Am. J. Agric. Econ. 1999, 81, 373–384. [Google Scholar] [CrossRef]
- Gibson, E.L.; Wardle, J.; Watts, C.J. Fruit and vegetable consumption, nutritional knowledge and beliefs in mothers and children. Appetite 1998, 31, 205–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cullen, K.W.; Ash, D.M.; Warneke, C.; De Moor, C. Intake of soft drinks, fruit-flavored beverages, and fruits and vegetables by children in grades 4 through 6. Am. J. Public Health 2002, 92, 1475–1477. [Google Scholar] [CrossRef] [PubMed]
- Marshall, T.A.; Eichenberger Gilmore, J.M.; Broffitt, B.; Stumbo, P.J.; Levy, S.M. Diet. quality in young children is influenced by beverage consumption. J. Am. Coll. Nutr. 2005, 24, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, L.R.; Schwartz, M.B.; Brownell, K.D. Effects of soft drink consumption on nutrition and health: A systematic review and meta-analysis. Am. J. Public Health 2007, 97, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—A systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; MacLehose, R.F.; Larson, N.; Laska, M.; Neumark-Sztainer, D. Family food preparation and its effects on adolescent dietary quality and eating patterns. J. Adolesc. Health 2016, 59, 530–536. [Google Scholar] [CrossRef] [Green Version]
- Chu, Y.L.; Storey, K.E.; Veugelers, P.J. Involvement in meal preparation at home is associated with better diet quality among Canadian children. J. Nutr. Educ. Behav. 2014, 46, 304–308. [Google Scholar] [CrossRef]
- De Jong, E.; Visscher, T.; HiraSing, R.; Seidell, J.; Renders, C. Home environmental determinants of children’s fruit and vegetable consumption across different SES backgrounds. Pediatr. Obes. 2015, 10, 134–140. [Google Scholar] [CrossRef]
- Vereecken, C.A.; Keukelier, E.; Maes, L. Influence of mother’s educational level on food parenting practices and food habits of young children. Appetite 2004, 43, 93–103. [Google Scholar] [CrossRef]
- Verjans-Janssen, S.; Van Kann, D.; Kremers, S.; Vos, S.; Jansen, M.; Gerards, S. A cross-sectional study on the relationship between the Family Nutrition Climate and children’s nutrition behavior. Nutrients 2019, 11, 2344. [Google Scholar] [CrossRef] [Green Version]
- Wright, K.; Norris, K.; Newman Giger, J.; Suro, Z. Improving healthy dietary behaviors, nutrition knowledge, and self-efficacy among underserved school children with parent and community involvement. Child. Obes. 2012, 8, 347–356. [Google Scholar] [CrossRef] [PubMed]




| Variables | Number of Items | Example Question | Answer Options |
|---|---|---|---|
| Children’s nutrition knowledge | 24 | ‘What is most healthy to drink?’ (images of the products) | (1) Flavored milk, (2) Chocolate, (3) Milk, (4) I don’t know |
| Children’s FV intake | 6 | ‘What type of vegetable/fruit, and how much did you eat yesterday morning?’ | Precoded table with the most common eaten FV and open space to write FV that are not listed |
| Caregivers’ health promotion behaviour | 5 | ‘How often do you get FV from home to take to school?’ | (1) Every day, (2) 3–4 times a week, (3) 2–3 times a week, (4) Once a week, (5) Never |
| ‘How often do you get sweets from home to take to school?’ | (1) Every day, (2) 3–4 times a week, (3) 2–3 times a week, (4) Once a week, (5) Never | ||
| ‘How often do you get SSBs from home to take to school?’ | (1) Every day, (2) 3–4 times a week, (3) 2–3 times a week, (4) Once a week, (5) Never | ||
| ‘How often do you help with cooking at home?’ | (1) Every day, (2) 3–4 times a week, (3) 2–3 times a week, (4) Once a week, (5) Sometimes, (6) Never | ||
| ‘Do you talk about healthy eating at home?’ | (1) Yes, (2) Sometimes, (3) No |
| Total FV Intake, g/Day/Student | Nutrition Knowledge, Score | ||||
|---|---|---|---|---|---|
| Caregivers’ HPB | Na (%) | Mean (SD) | B b | Mean (SD) | B b |
| FV provision | 1382 | ||||
| Never | 164 (12) | 214 (220) | ref | 2.79 (0.829) | ref |
| 1/week | 138 (10) | 307 (266) | 93 ** | 2.94 (0.735) | 0.15 ** |
| 2–3/week | 177 (13) | 357 (291) | 143 ** | 2.90 (0.818) | 0.11 ** |
| 3–4/week | 269 (19) | 333 (272) | 119 ** | 3.10 (0.773) | 0.31 ** |
| Every day | 634 (46) | 357 (257) | 143 ** | 3.04 (0.825) | 0.25 ** |
| SSBs provision | 1367 | ||||
| Never | 552 (40) | 343 (283) | ref | 3.03 (0.798) | ref |
| 1/week | 156 (12) | 402 (249) | 59 ** | 3.01 (0.815) | −0.02 |
| 2–3/week | 139 (10) | 383 (278) | 40 | 3.01 (0.727) | −0.02 |
| 3–4/week | 110 (8) | 350 (274) | 7 | 3.05 (0.827) | 0.02 |
| Every day | 410 (30) | 268 (228) | −75 ** | 2.91 (0.857) | −0.12 ** |
| Sweets provision | 1373 | ||||
| Never | 455 (33) | 334 (254) | ref | 3.08 (0.816) | ref |
| 1/week | 340 (25) | 364 (285) | 30 * | 2.95 (0.781) | −0.13 ** |
| 2–3/week | 253 (18) | 357 (260) | 23 | 2.99 (0.792) | −0.09 * |
| 3–4/week | 147 (11) | 299 (253) | −35 | 3.03 (0.789) | −0.05 |
| Every day | 178 (13) | 255 (262) | −79 ** | 2.80 (0.876) | −0.28 ** |
| Help with cooking | 1374 | ||||
| Never | 157 (11) | 261 (231) | ref | 2.77 (0.832) | ref |
| Sometimes | 746 (54) | 304 (243) | 43 * | 2.98 (0.833) | 0.21 ** |
| 1/week | 106 (8) | 374 (280) | 113 ** | 3.17 (0.663) | 0.40 ** |
| 2–3/week | 130 (10) | 414 (303) | 153 ** | 3.31 (0.718) | 0.54 ** |
| 3–4/week | 78 (6) | 370 (285) | 109 ** | 3.03 (0.796) | 0.26 * |
| Every day | 157 (11) | 396 (307) | 135 ** | 2.85 (0.755) | 0.08 |
| Talking about food | 1377 | ||||
| No | 300 (22) | 270 (244) | ref | 2.76 (0.818) | ref |
| Sometimes | 747 (54) | 326 (264) | 56 ** | 3.00 (0.800) | 0.24 ** |
| Yes | 330 (24) | 396 (275) | 126 ** | 3.16 (0.793) | 0.40 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verdonschot, A.; de Vet, E.; van Seeters, N.; Warmer, J.; Collins, C.E.; Bucher, T.; Haveman-Nies, A. Caregivers’ Role in the Effectiveness of Two Dutch School-Based Nutrition Education Programmes for Children Aged 7–12 Years Old. Nutrients 2021, 13, 140. https://doi.org/10.3390/nu13010140
Verdonschot A, de Vet E, van Seeters N, Warmer J, Collins CE, Bucher T, Haveman-Nies A. Caregivers’ Role in the Effectiveness of Two Dutch School-Based Nutrition Education Programmes for Children Aged 7–12 Years Old. Nutrients. 2021; 13(1):140. https://doi.org/10.3390/nu13010140
Chicago/Turabian StyleVerdonschot, Angeliek, Emely de Vet, Natalie van Seeters, Jolieke Warmer, Clare E. Collins, Tamara Bucher, and Annemien Haveman-Nies. 2021. "Caregivers’ Role in the Effectiveness of Two Dutch School-Based Nutrition Education Programmes for Children Aged 7–12 Years Old" Nutrients 13, no. 1: 140. https://doi.org/10.3390/nu13010140





