Micronutrients and Markers of Oxidative Stress and Inflammation Related to Cardiometabolic Health: Results from the EHES-LUX Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Metabolic Syndrome
2.3. Micronutrients, Markers of Oxidative Stress, and Inflammation
2.4. Covariates
2.5. Statistical Data Analysis
3. Results
3.1. Participants’ Characteristics
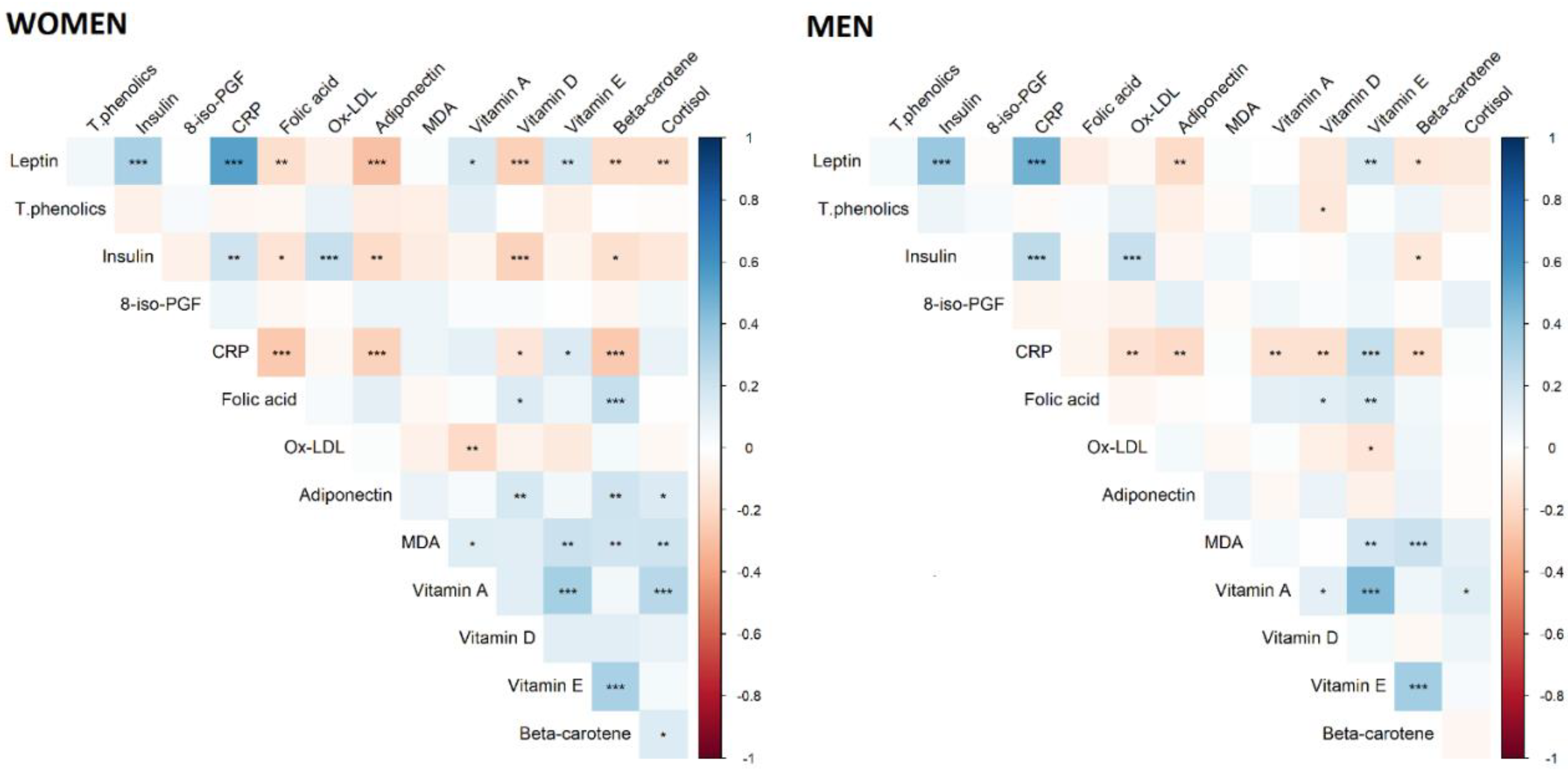
3.2. Association between MetS and Markers of Inflammation, Oxidative Stress, and Micronutrients
3.3. MetS Components and Markers of Inflammation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rani, V.; Deep, G.; Singh, R.K.; Palle, K.; Yadav, U.C. Oxidative stress and metabolic disorders: Pathogenesis and therapeutic strategies. Life Sci. 2016, 148, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Joshipura, K.J.; Hu, F.B.; Manson, J.E.; Stampfer, M.J.; Rimm, E.B.; Speizer, F.E.; Colditz, G.; Ascherio, A.; Rosner, B.; Spiegelman, D.; et al. The Effect of Fruit and Vegetable Intake on Risk for Coronary Heart Disease. Ann. Intern. Med. 2001, 134, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Rees, K.; Hartley, L.; Flowers, N.; Clarke, A.; Hooper, L.; Thorogood, M.; Stranges, S. ‘Mediterranean’ dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2013, CD009825. [Google Scholar] [CrossRef] [Green Version]
- Tian, Y.; Su, L.; Wang, J.; Duan, X.; Jiang, X. Fruit and vegetable consumption and risk of the metabolic syndrome: A meta-analysis. Public Health Nutr. 2018, 21, 756–765. [Google Scholar] [CrossRef]
- Lee, M.; Lim, M.; Kim, J. Fruit and vegetable consumption and the metabolic syndrome: A systematic review and dose–response meta-analysis. Br. J. Nutr. 2019, 122, 723–733. [Google Scholar] [CrossRef]
- Alissa, E.M.; Ferns, G.A. Dietary Fruits and Vegetables and Cardiovascular Diseases Risk. Crit. Rev. Food Sci. Nutr. 2015, 57, 1950–1962. [Google Scholar] [CrossRef] [Green Version]
- Galan, P.; Viteri, F.E.; Bertrais, S.; Czernichow, S.; Faure, H.; Arnaud, J.; Ruffieux, D.; Chenal, S.; Arnault, N.; Favier, A.; et al. Serum concentrations of β-carotene, vitamins C and E, zinc and selenium are influenced by sex, age, diet, smoking status, alcohol consumption and corpulence in a general French adult population. Eur. J. Clin. Nutr. 2005, 59, 1181–1190. [Google Scholar] [CrossRef] [Green Version]
- Godala, M.; Materek-Kuśmierkiewicz, I.; Moczulski, D.; Rutkowski, M.; Szatko, F.; Gaszyńska, E.; Tokarski, S.; Kowalski, J. The risk of plasma vitamin A, C, E and D deficiency in patients with metabolic syndrome: A case-control study. Adv. Clin. Exp. Med. 2017, 26, 581–586. [Google Scholar] [CrossRef] [Green Version]
- Ford, E.S.; Mokdad, A.H.; Giles, W.H.; Brown, D.W. The Metabolic Syndrome and Antioxidant Concentrations: Findings from the Third National Health and Nutrition Examination Survey. Diabetes 2003, 52, 2346–2352. [Google Scholar] [CrossRef] [Green Version]
- Samouda, H.; De Beaufort, C.E.; Gilson, G.; Schritz, A.; Vaillant, M.; Ghaddhab, C.; Ruiz-Castell, M.; Huiart, L.; Dohet, F.; Weber, B.; et al. Relationship of oxidative stress to visceral adiposity in youth and role played by vitamin D. Pediatr. Diabetes 2020, 21, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Landrier, J.-F.; Marcotorchino, J.; Tourniaire, F. Lipophilic Micronutrients and Adipose Tissue Biology. Nutrients 2012, 4, 1622–1649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, L.F.; Jacobs, D.R., Jr.; Gross, M.D.; Schreiner, P.J.; Williams, O.D.; Lee, D.-H. Longitudinal associations between body mass index and serum carotenoids: The CARDIA study. Br. J. Nutr. 2006, 95, 358–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallström, P.; Wirfält, E.; Lahmann, P.H.; Gullberg, B.; Janzon, L.; Berglund, G. Serum concentrations of β-carotene and α-tocopherol are associated with diet, smoking, and general and central adiposity. Am. J. Clin. Nutr. 2001, 73, 777–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamer, M.; Chida, Y. Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: Systematic review and meta-analysis. J. Hypertens. 2007, 25, 2361–2369. [Google Scholar] [CrossRef]
- Buijsse, B.; Feskens, E.; Schlettwein-Gsell, D.; Ferry, M.; Kok, F.J.; Kromhout, D.; De Groot, L. Plasma carotene and α-tocopherol in relation to 10-y all-cause and cause-specific mortality in European elderly: The Survey in Europe on Nutrition and the Elderly, a Concerted Action (SENECA). Am. J. Clin. Nutr. 2005, 82, 879–886. [Google Scholar] [CrossRef] [Green Version]
- Tresserra-Rimbau, A.; Rimm, E.B.; Remon, A.M.; Martínez-González, M.Á.; López-Sabater, M.C.; Covas, M.-I.; Corella, D.; Salas-Salvadó, J.; Gómez-Gracia, E.; Lapetra, J.; et al. Polyphenol intake and mortality risk: A re-analysis of the PREDIMED trial. BMC Med. 2014, 12, 77. [Google Scholar] [CrossRef] [Green Version]
- Kaulmann, A.; Bohn, T. Carotenoids, inflammation, and oxidative stress—Implications of cellular signaling pathways and relation to chronic disease prevention. Nutr. Res. 2014, 34, 907–929. [Google Scholar] [CrossRef]
- Beydoun, M.A.; Chen, X.; Jha, K.; Beydoun, H.A.; Zonderman, A.B.; Canas, J.A. Carotenoids, vitamin A, and their association with the metabolic syndrome: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 32–45. [Google Scholar] [CrossRef]
- Park, S.; Ham, J.-O.; Lee, B.-K. Effects of total vitamin A, vitamin C, and fruit intake on risk for metabolic syndrome in Korean women and men. Nutrition 2015, 31, 111–118. [Google Scholar] [CrossRef]
- Lee, I.-M.; Cook, N.R.; Gaziano, J.M.; Gordon, D.; Ridker, P.M.; Manson, J.E.; Hennekens, C.H.; Buring, J.E. Vitamin E in the primary prevention of cardiovascular disease and cancer: The Women’s Health Study: A randomized controlled trial. JAMA 2005, 294, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Khansari, N.; Shakiba, Y.; Mahmoudi, M. Chronic Inflammation and Oxidative Stress as a Major Cause of Age-Related Diseases and Cancer. Recent Pat. Inflamm. Allergy Drug Discov. 2009, 3, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Biswas, S.K. Does the Interdependence between Oxidative Stress and Inflammation Explain the Antioxidant Paradox? Oxidative Med. Cell. Longev. 2016, 2016, 5698931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef]
- Hajer, G.R.; Van Haeften, T.W.; Visseren, F.L.J. Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur. Heart J. 2008, 29, 2959–2971. [Google Scholar] [CrossRef] [Green Version]
- Bocquet, V.; Barré, J.; Couffignal, S.; D’Incau, M.; Delagardelle, C.; Michel, G.; Schlesser, M.; Stranges, S.; Kuemmerle, A.; Ruiz-Castell, M. Study design and characteristics of the Luxembourg European Health Examination Survey (EHES-LUX). BMC Public Health 2018, 18, 1169. [Google Scholar] [CrossRef]
- Zimmet, P.; Alberti, K.G.M.; Ríos, M.S. A New International Diabetes Federation (IDF) Worldwide Definition of the Metabolic Syndrome: The Rationale and the Results. Rev. Esp. Cardiol. 2005, 58, 1371–1375. [Google Scholar] [CrossRef]
- Donaldson, M. Development of a rapid, simple assay of plasma total carotenoids. BMC Res. Notes 2012, 5, 521. [Google Scholar] [CrossRef] [Green Version]
- Tibshirani, R. Regression Shrinkage and Selection via the Lasso. R. Stat. Soc. 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Rauma, A.L.; Törrönen, R.; Hänninen, O.; Verhagen, H.; Mykkänen, H. Antioxidant status in long-term adherents to a strict uncooked vegan diet. Am. J. Clin. Nutr. 1995, 62, 1221–1227. [Google Scholar] [CrossRef] [Green Version]
- Booth, S.L.; Johns, T.; Kuhnlein, H.V. Natural Food Sources of Vitamin A and Provitamin A. Food Nutr. Bull. 1992, 14, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Beydoun, M.A.; Shroff, M.R.; Chen, X.; Beydoun, H.A.; Wang, Y.; Zonderman, A.B. Serum Antioxidant Status Is Associated with Metabolic Syndrome among U.S. Adults in Recent National Surveys. J. Nutr. 2011, 141, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Del Bo, C.; Bernardi, S.; Marino, M.; Porrini, M.; Tucci, M.; Guglielmetti, S.; Cherubini, A.; Carrieri, B.; Kirkup, B.; Kroon, P.A.; et al. Systematic Review on Polyphenol Intake and Health Outcomes: Is there Sufficient Evidence to Define a Health-Promoting Polyphenol-Rich Dietary Pattern? Nutrients 2019, 11, 1355. [Google Scholar] [CrossRef] [Green Version]
- Pai, J.K.; Pischon, T.; Ma, J.; Manson, J.E.; Hankinson, S.E.; Joshipura, K.; Curhan, G.C.; Rifai, N.; Cannuscio, C.C.; Stampfer, M.J.; et al. Inflammatory Markers and the Risk of Coronary Heart Disease in Men and Women. N. Engl. J. Med. 2004, 351, 2599–2610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouchi, N.; Walsh, K. A Novel Role for Adiponectin in the Regulation of Inflammation. Arter. Thromb. Vasc. Biol. 2008, 28, 1219–1221. [Google Scholar] [CrossRef] [Green Version]
- Lew, J.; Sanghavi, M.; Ayers, C.R.; McGuire, D.K.; Omland, T.; Atzler, D.; Gore, M.O.; Neeland, I.; Berry, J.D.; Khera, A.; et al. Sex-Based Differences in Cardiometabolic Biomarkers. Circulation 2017, 135, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Kumari, R.; Kumar, S.; Kant, R. An update on metabolic syndrome: Metabolic risk markers and adipokines in the development of metabolic syndrome. Diabetes Metab. Syndr. 2019, 13, 2409–2417. [Google Scholar] [CrossRef] [PubMed]
- Franks, P.W.; Brage, S.; Luan, J.; Ekelund, U.; Rahman, M.; Farooqi, I.S.; Halsall, I.; O’Rahilly, S.; Wareham, N.J. Leptin Predicts a Worsening of the Features of the Metabolic Syndrome Independently of Obesity. Obes. Res. 2005, 13, 1476–1484. [Google Scholar] [CrossRef] [PubMed]
- Frühbeck, G.; Catalán, V.; Rodríguez, A.; Ramírez, B.; Becerril, S.; Salvador, J.; Portincasa, P.; Colina, I.; Gómez-Ambrosi, J. Involvement of the leptin-adiponectin axis in inflammation and oxidative stress in the metabolic syndrome. Sci. Rep. 2017, 7, 6619. [Google Scholar] [CrossRef] [PubMed]
- Charchour, R.; Dufour-Rainfray, D.; Morineau, G.; Vatier, C.; Fellahi, S.; Vigouroux, C.; Genoux, A.; Capeau, J.; Lacorte, J.-M.; Collet, C.; et al. Mutltifaceted biological roles of leptin. Ann. Biol. Clin. 2020, 78, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Könner, A.C.; Brüning, J.C. Selective Insulin and Leptin Resistance in Metabolic Disorders. Cell Metab. 2012, 16, 144–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, T.S.; Lean, M.E. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc. Dis. 2016, 5, 2048004016633371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurtado-Roca, Y.; Bueno, H.; Fernández-Ortiz, A.; Ordovas, J.M.; Ibanez, B.; Fuster, V.; Rodriguez-Artalejo, F.; Laclaustra, M. Oxidized LDL is associated with metabolic syndrome traits independently of central obesity and insulin resistance. Diabetes 2017, 66, 474–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van’t Erve, T.J.; Kadiiska, M.B.; London, S.J.; Mason, R.P. Classifying oxidative stress by F(2)-isoprostane levels across human diseases: A meta-analysis. Redox Biol. 2017, 12, 582–599. [Google Scholar] [CrossRef] [PubMed]


| Total (N = 504) | Men (N = 272) | Women (N = 232) | p-Value 1 | |
|---|---|---|---|---|
| Mean ± SD, N (%) | Mean ± SD, N (%) | Mean ± SD, N (%) | ||
| Anthropometric characteristics | ||||
| Weight, kg | 81.61 ± 18.47 | 88.37 ± 17.10 | 73.67 ± 16.83 | <0.0001 |
| BMI, kg/m2 | 28.34 ± 5.670 | 28.71 ± 4.830 | 27.90 ± 6.510 | 0.12 |
| Waist, cm | 96.24 ± 15.19 | 101.0 ± 13.32 | 90.62 ± 15.36 | <0.0001 |
| Hip size, cm | 104.3 ± 11.06 | 102.8 ± 9.130 | 106.0 ± 12.78 | <0.01 |
| Cardiometabolic risk factors | ||||
| Systolic blood pressure, mm Hg | 127.1 ± 16.63 | 132.3 ± 14.41 | 121.0 ± 17.02 | <0.0001 |
| Diastolic blood pressure, mm Hg | 81.89 ± 11.14 | 84.10 ± 10.93 | 79.28 ± 10.83 | <0.0001 |
| Triglycerides, mg/dL | 134.8 ± 81.65 | 160.9 ± 91.56 | 104.1 ± 54.18 | <0.0001 |
| HDL-C, mg/dL | 48.22 ± 13.53 | 42.81 ± 10.58 | 54.56 ± 13.86 | <0.0001 |
| Total cholesterol, mg/dL | 203.6 ± 38.53 | 204.6 ± 40.43 | 202.3 ± 36.24 | 0.50 |
| Glucose, mg/dL | 101.5 ± 21.28 | 104.8 ± 25.73 | 97.53 ± 13.45 | <0.0001 |
| HbA1c, mol/mol | 38.51 ± 6.840 | 38.72 ± 7.960 | 38.27 ± 5.250 | 0.45 |
| Metabolic syndrome | 280 (55.56) | 169 (62.13) | 111 (47.84) | <0.01 |
| Metabolic syndrome components | ||||
| Abdominal obesity 2 | 350 (69.44) | 185 (52.86) | 165 (47.14) | 0.45 |
| Hypertriglyceridemia 3 | 230 (45.63) | 153 (66.52) | 77 (33.48) | <0.0001 |
| Low HDL-C 4 | 219 (43.35) | 148 (67.58) | 71 (32.42) | <0.0001 |
| High blood pressure 5 | 265 (52.68) | 145 (54.72) | 120 (45.28) | 0.76 |
| Hyperglycemia 6 | 289 (57.46) | 182 (62.98) | 107 (37.02) | <0.0001 |
| Metabolic Syndrome (N = 280) | Non Metabolic Syndrome (N = 224) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | Q25 | Q75 | Min | Max | Median | Q25 | Q75 | Min | Max | p-Value 1 | |
| Markers of dietary intake | |||||||||||
| Vitamin D, µg/dL | 0.213 | 0.147 | 0.273 | 0.046 | 0.710 | 0.224 | 0.156 | 0.282 | 0.062 | 0.536 | 0.32 |
| Vitamin E, μg/dL | 1274 | 1087 | 1538 | 657.0 | 3100 | 1154 | 993.0 | 1327 | 587.0 | 2487 | <0.0001 |
| Vitamin A, μg/dL | 71.50 | 59.50 | 82.00 | 26.00 | 142.0 | 65.00 | 53.00 | 75.00 | 27.00 | 125.0 | <0.0001 |
| Folic acid, nmol/dL | 122.0 | 89.50 | 178.0 | 29.00 | 546.0 | 132.0 | 93.50 | 180.0 | 26.00 | 686.0 | 0.36 |
| Beta-carotene, nmol/dL | 1078 | 751.0 | 1510 | 28.00 | 5459 | 1220 | 851.0 | 1822 | 284.0 | 4268 | <0.01 |
| Total phenolics, mmol/dL | 1072 | 1006 | 1144 | 785.3 | 1384 | 1065 | 1014 | 1125 | 781.2 | 1351 | 0.66 |
| Markers of oxidative stress | |||||||||||
| MDA, μM | 1.101 | 0.847 | 1.389 | 0.171 | 2.605 | 1.102 | 0.807 | 1.343 | 0.132 | 2.520 | 0.49 |
| Ox-LDL, U/dL | 0.157 | 0.067 | 0.374 | 0.014 | 1.368 | 0.231 | 0.100 | 0.647 | 0.012 | 1.453 | <0.001 |
| 8-Iso-prostaglandin-F2α, µg/dL | 0.019 | 0.009 | 0.086 | 0.002 | 0.412 | 0.017 | 0.009 | 0.067 | 0.001 | 0.317 | 0.34 |
| Marker of stress | |||||||||||
| Cortisol, nmol/dL | 4153 | 3243 | 5150 | 112.0 | 12980 | 4152 | 3346 | 5202 | 1025 | 16240 | 0.95 |
| Markers of inflammation | |||||||||||
| CRP, µg/dL | 0.016 | 0.008 | 0.028 | 0.001 | 0.138 | 0.007 | 0.003 | 0.014 | 0.000 | 0.070 | <0.0001 |
| Adiponectin, µg/dL | 0.027 | 0.020 | 0.036 | 0.007 | 0.117 | 0.034 | 0.025 | 0.047 | 0.008 | 0.132 | <0.001 |
| Markers of energy metabolism and hormones | |||||||||||
| Leptin, µg/dL | 0.176 | 0.112 | 0.268 | 0.010 | 1.365 | 0.096 | 0.045 | 0.192 | 0.004 | 0.667 | <0.0001 |
| Insulin, nmol/dL | 1.148 | 0.760 | 1.761 | 0.180 | 17.97 | 0.919 | 0.540 | 1.228 | 0.157 | 18.00 | <0.0001 |
| Metabolic Syndrome | |||
|---|---|---|---|
| Men | Women | Total | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Vitamin A, μg/dL | - | 1.03 (1.01, 1.05) | 1.02 (1.01, 1.03) |
| CRP, μg/dL | 1.71 (1.19, 2.51) | 1.38 (0.94, 2.06) | 1.51 (1.16, 1.98) |
| Adiponectin, μg/dL | - | 0.18 (0.07, 0.46) | 0.24 (0.13, 0.46) |
| Leptin, μg/dL | 3.34 (2.15, 5.42) | 3.31 (1.63, 7.22) | 3.10 (2.10, 4.72) |
| Insulin, nmol/dL | - | - | 1.24 (0.90, 1.73) |
| Age, years | 1.08 (1.04, 1.12) | 1.13 (1.09, 1.18) | 1.10 (1.08, 1.14) |
| Aerobic Physical activity (≥150 min/week vs. <150 min/week) | 0.41 (0.21, 0.77) | 0.28 (0.11, 0.63) | 0.32 (0.19, 0.54) |
| Sex (women vs. men) | - | - | 0.26 (0.13, 0.51) |
| Men, N = 272 | Women, N = 231 | Total, N = 503 | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Abdominal obesity1 | |||
| Vitamin A, μg/dL | - | 1.01 (0.98, 1.03) | 1.00 (0.98, 1.01) |
| CRP, μg/dL | 2.14 (1.33, 3.45) | 1.13 (0.74, 1.73) | 1.43 (1.06, 1.94) |
| Adiponectin, μg/dL | - | 0.23 (0.07, 0.70) | 0.29 (0.13, 0.64) |
| Leptin, μg/dL | 15.2 (7.04, 32.8) | 15.1 (5.64, 40.6) | 13.5 (7.44, 24.6) |
| Insulin, nmol/dL | - | - | 1.15 (0.77, 1.73) |
| Age, years | 1.07 (1.03, 1.12) | 1.12 (1.07, 1.18) | 1.10 (1.06, 1.14) |
| Aerobic Physical activity (≥150 min/week vs. <150 min/week) | 0.66 (0.29, 1.52) | 0.38 (0.15, 0.99) | 0.48 (0.26, 0.89) |
| Sex (women vs. men) | - | - | 0.18 (0.07, 0.47) |
| Hypertriglyceridemia 2 | |||
| Vitamin A, μg/dL | - | 1.04 (1.02, 1.06) | 1.04 (1.02, 1.05) |
| CRP, μg/dL | 1.27 (0.95, 1.70) | 1.26 (0.84, 1.87) | 1.33 (1.04, 1.70) |
| Adiponectin, μg/dL | - | 0.21 (0.09, 0.53) | 0.26 (0.15, 0.47) |
| Leptin, μg/dL | 1.33 (0.95, 1.86) | 1.64 (0.83, 3.27) | 1.27 (0.92, 1.76) |
| Insulin, nmol/dL | - | - | 1.14 (0.87, 1.51) |
| Age, years | 1.05 (1.02, 1.07) | 1.10 (1.06, 1.15) | 1.06 (1.04, 1.09) |
| Aerobic Physical activity (≥150 min/week vs. <150 min/week) | 0.75 (0.44, 1.29) | 0.61 (0.26, 1.45) | 0.64 (0.40, 1.04) |
| Sex (women vs. men) | - | - | 0.51 (0.28, 0.93) |
| Low HDL-C 1 | |||
| Vitamin A, μg/dL | - | 1.00 (0.98, 1.02) | 1.00 (0.99, 1.01) |
| CRP, μg/dL | 1.34 (0.98, 1.84) | 0.87 (0.62, 1.23) | 1.08 (0.86, 1.37) |
| Adiponectin, μg/dL | - | 0.27 (0.11, 0.67) | 0.33 (0.19, 0.59) |
| Leptin, μg/dL | 1.08 (0.75, 1.55) | 1.70 (0.95, 3.04) | 1.17 (0.85, 1.61) |
| Insulin, nmol/dL | - | - | 1.07 (0.82, 1.41) |
| Age, years | 1.00 (0.97, 1.03) | 1.08 (1.04. 1.12) | 1.03 (1.01, 1.06) |
| Aerobic Physical activity (≥150 min/week vs. <150 min/week) | 0.78 (0.43, 1.39) | 0.50 (0.24, 1.05) | 0.66 (0.42, 1.04) |
| Sex (women vs men) | - | - | 2.13 (1.14, 3.98) |
| High blood pressure 1 | |||
| Vitamin A, μg/dL | - | 1.03 (1.01, 1.05) | 1.02 (1.01, 1.04) |
| CRP, μg/dL | 1.37 (0.98, 1.90) | 1.47 (1.01, 2.14) | 1.30 (1.02, 1.65) |
| Adiponectin, μg/dL | - | 0.31 (0.13, 0.74) | 0.45 (0.25, 0.81) |
| Leptin, μg/dL | 1.57 (1.08, 2.27) | 1.07 (0.59, 1.94) | 1.28 (0.93, 1.78) |
| Insulin, nmol/dL | - | - | 1.52 (1.13, 2.05) |
| Age, years | 1.07 (1.03, 1.10) | 1.11 (1.07, 1.16) | 1.09 (1.07, 1.12) |
| Aerobic Physical activity (≥150 min/week vs. <150 min/week) | 0.47 (0.26, 0.85) | 0.57 (0.26, 1.22) | 0.50 (0.31, 0.80) |
| Sex (women vs. men) | - | - | 0.41 (0.21, 0.79) |
| Hyperglycemia 1 | |||
| Vitamin A, μg/dL | - | 1.02 (1.00, 1.04) | 1.01 (1.00, 1.03) |
| CRP, μg/dL | 0.93 (0.69, 1.25) | 1.08 (0.74, 1.60) | 1.02 (0.81, 1.28) |
| Adiponectin, μg/dL | - | 0.44 (0.18, 1.05) | 0.73 (0.43, 1.25) |
| Leptin, μg/dL | 2.08 (1.45, 2.98) | 1.97 (1.01, 3.82) | 1.97 (1.42, 2.73) |
| Insulin, nmol/dL | - | - | 1.14 (0.87, 1.50) |
| Age, years | 1.04 (1.01, 1.07) | 1.10 (1.06, 1.14) | 1.06 (1.04, 1.08) |
| Aerobic Physical activity (≥150 min/week vs. <150 min/week) | 0.84 (0.48, 1.46) | 0.51 (0.23, 1.15) | 0.72 (0.46, 1.13) |
| Sex (women vs. men) | - | - | 0.23 (0.13, 0.43) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Castell, M.; Le Coroller, G.; Landrier, J.-F.; Kerkour, D.; Weber, B.; Fagherazzi, G.; Appenzeller, B.M.R.; Vaillant, M.; Bohn, T. Micronutrients and Markers of Oxidative Stress and Inflammation Related to Cardiometabolic Health: Results from the EHES-LUX Study. Nutrients 2021, 13, 5. https://doi.org/10.3390/nu13010005
Ruiz-Castell M, Le Coroller G, Landrier J-F, Kerkour D, Weber B, Fagherazzi G, Appenzeller BMR, Vaillant M, Bohn T. Micronutrients and Markers of Oxidative Stress and Inflammation Related to Cardiometabolic Health: Results from the EHES-LUX Study. Nutrients. 2021; 13(1):5. https://doi.org/10.3390/nu13010005
Chicago/Turabian StyleRuiz-Castell, Maria, Gwenaëlle Le Coroller, Jean-Francois Landrier, Djedgiga Kerkour, Bernard Weber, Guy Fagherazzi, Brice M. R. Appenzeller, Michel Vaillant, and Torsten Bohn. 2021. "Micronutrients and Markers of Oxidative Stress and Inflammation Related to Cardiometabolic Health: Results from the EHES-LUX Study" Nutrients 13, no. 1: 5. https://doi.org/10.3390/nu13010005





