Total, Bioavailable, and Free 25-Hydroxyvitamin D Equally Associate with Adiposity Markers and Metabolic Traits in Mexican Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Biochemical, Clinical and Anthropometric Measures
2.3. Genotyping of GC Gene Variants
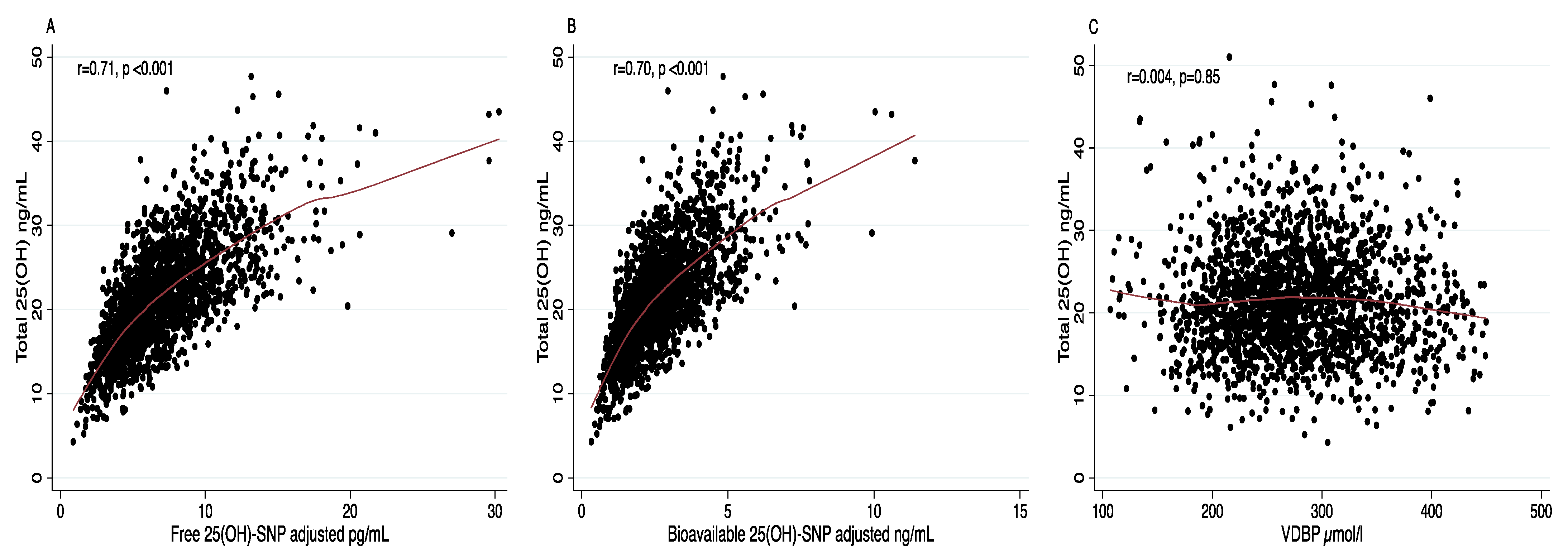
2.4. Estimation of Free and Bioavailable 25(OH)D
2.5. Outcome Measures
2.6. Measurement of Other Covariates
2.7. Statistical Analyses
3. Results
3.1. Demographic Characteristics of the Study Population
3.2. Levels of Total, Free and Bioavailable 25-Hydroxyvitamin D According to Clinical Data
3.3. Association between Vitamin D Levels, Adiposity Markers and Metabolic Traits
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khazai, N.; Judd, S.E.; Tangpricha, V. Calcium and vitamin D: Skeletal and extraskeletal health. Curr. Rheumatol. Rep. 2008, 10, 110–117. [Google Scholar] [CrossRef] [Green Version]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Holick, M.F.; Chen, T.C. Vitamin D deficiency: A worldwide problem with health consequences. Am. J. Clin. Nutr. 2008, 87, 1080S–1086S. [Google Scholar] [CrossRef] [Green Version]
- Bikle, D.D.; Gee, E.; Halloran, B.; Kowalski, M.A.; Ryzen, E.; Haddad, J.G. Assessment of the free fraction of 25-hydroxyvitamin d in serum and its regulation by albumin and the vitamin d-binding protein. J. Clin. Endocrinol. Metab. 1986, 63, 954–959. [Google Scholar] [CrossRef]
- Li, C.; Chen, P.; Duan, X.; Wang, J.; Shu, B.; Li, X.; Ba, Q.; Li, J.; Wang, Y.; Wang, H. Bioavailable 25(OH)D but Not Total 25(OH)D Is an Independent Determinant for Bone Mineral Density in Chinese Postmenopausal Women. EBioMedicine 2017, 15, 184–192. [Google Scholar] [CrossRef] [Green Version]
- Chun, R.F.; Peercy, B.E.; Orwoll, E.S.; Nielson, C.M.; Adams, J.S.; Hewison, M. Vitamin D and DBP: The free hormone hypothesis revisited. J. Steroid Biochem. Mol. Biol. 2014, 144 Pt A, 132–137. [Google Scholar] [CrossRef] [Green Version]
- Arnaud, J.; Constans, J. Affinity differences for vitamin D metabolites associated with the genetic isoforms of the human serum carrier protein (DBP). Hum. Genet. 1993, 92, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Larcombe, L.; Mookherjee, N.; Slater, J.; Slivinski, C.; Singer, M.; Whaley, C.; Denechezhe, L.; Matyas, S.; Turner-Brannen, E.; Nickerson, P.; et al. Vitamin D in a northern Canadian first nation population: Dietary intake, serum concentrations and functional gene polymorphisms. PLoS ONE 2012, 7, e49872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauridsen, A.L.; Vestergaard, P.; Nexo, E. Mean serum concentration of vitamin D-binding protein (Gc globulin) is related to the Gc phenotype in women. Clin. Chem. 2001, 47, 753–756. [Google Scholar] [CrossRef] [PubMed]
- Chun, R.F.; Lauridsen, A.L.; Suon, L.; Zella, L.A.; Pike, J.W.; Modlin, R.L.; Martineau, A.R.; Wilkinson, R.J.; Adams, J.; Hewison, M. Vitamin D-binding protein directs monocyte responses to 25-hydroxy- and 1,25-dihydroxyvitamin D. J. Clin. Endocrinol. Metab. 2010, 95, 3368–3376. [Google Scholar] [CrossRef] [Green Version]
- Khan, A.H.; Jafri, L.; Siddiqui, A.; Naureen, G.; Morris, H.; Moatter, T. Polymorphisms in the GC Gene for Vitamin D Binding Protein and Their Association with Vitamin D and Bone Mass in Young Adults. J. Coll. Physicians Surg. Pak. 2019, 29, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Johnsen, M.S.; Grimnes, G.; Figenschau, Y.; Torjesen, P.A.; Almås, B.; Jorde, R. Serum free and bio-available 25-hydroxyvitamin D correlate better with bone density than serum total 25-hydroxyvitamin D. Scand. J. Clin. Lab. Investig. 2014, 74, 177–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rivera-Paredez, B.; Hidalgo-Bravo, A.; de la Cruz-Montoya, A.; Martínez-Aguilar, M.M.; Ramírez-Salazar, E.G.; Flores, M.; Quezada-Sánchez, A.D.; Ramírez-Palacios, P.; Cid, M.; Martínez-Hernández, A.; et al. Association between vitamin D deficiency and common variants of Vitamin D binding protein gene among Mexican Mestizo and indigenous postmenopausal women. J. Endocrinol. Investig. 2020, 43, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Wimalawansa, S.J. Non-musculoskeletal benefits of vitamin D. J. Steroid Biochem. Mol. Biol. 2018, 175, 60–81. [Google Scholar] [CrossRef] [PubMed]
- Berridge, M.J. Vitamin D deficiency and diabetes. Biochem. J. 2017, 474, 1321–1332. [Google Scholar] [CrossRef] [PubMed]
- Afzal, S.; Bojesen, S.E.; Nordestgaard, B.G. Low 25-hydroxyvitamin D and risk of type 2 diabetes: A prospective cohort study and metaanalysis. Clin. Chem. 2013, 59, 381–391. [Google Scholar] [CrossRef] [Green Version]
- Szymczak-Pajor, I.; Śliwińska, A. Analysis of association between vitamin d deficiency and insulin resistance. Nutrients 2019, 11, 794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, L.; Zhai, Y.; Shen, S.; Wane, D. Association between Vitamin D and prediabetes: A PRISMA-compliant meta-analysis. Med. 2020, 99, e19034. [Google Scholar] [CrossRef]
- Ding, C.; Gao, D.; Wilding, J.; Trayhurn, P.; Bing, C. Vitamin D signalling in adipose tissue. Br. J. Nutr. 2012, 108, 1915–1923. [Google Scholar] [CrossRef] [Green Version]
- Koszowska, A.U.; Nowak, J.; Dittfeld, A.; Brończyk-Puzoń, A.; Kulpok, A.; Zubelewicz-Szkodzińska, B. Obesity, adipose tissue function and the role of vitamin D. Central Eur. J. Immunol. 2014, 39, 260–264. [Google Scholar] [CrossRef]
- Pereira-Santos, M.; Costa, P.R.F.; Assis, A.M.O.; Santos, C.A.S.T.; Santos, D.B. Obesity and vitamin D deficiency: A systematic review and meta-analysis. Obes. Rev. 2015, 16, 341–349. [Google Scholar] [CrossRef]
- Bikle, D.D.; Schwartz, J. Vitamin D binding protein, total and free Vitamin D levels in different physiological and pathophysiological conditions. Front. Endocrinol. 2019, 10, 317. [Google Scholar] [CrossRef] [Green Version]
- Denova-Gutiérrez, E.; Flores, Y.N.; Gallegos-Carrillo, K.; Ramírez-Palacios, P.; Rivera-Paredez, B.; Muñoz-Aguirre, P.; Velázquez-Cruz, R.; Torres-Ibarra, L.; Meneses-León, J.; Méndez-Hernández, P.; et al. Health workers cohort study: Methods and study design. Salud Publica Mex. 2016, 58, 708–716. [Google Scholar] [CrossRef]
- Freeman, J.; Wilson, K.; Spears, R.; Shalhoub, V.; Sibley, P. Performance evaluation of four 25-hydroxyvitamin D assays to measure 25-hydroxyvitamin D2. Clin. Biochem. 2015, 48, 1097–1104. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Aguilar, M.M.; Aparicio-Bautista, D.I.; Ramírez-Salazar, E.G.; Reyes-Grajeda, J.P.; De la Cruz-Montoya, A.H.; Antuna-Puente, B.; Hidalgo-Bravo, A.; Rivera-Paredez, B.; Ramírez-Palacios, P.; Quiterio, M.; et al. Serum proteomic analysis reveals vitamin d-binding protein (Vdbp) as a potential biomarker for low bone mineral density in mexican postmenopausal women. Nutrients 2019, 11, 2853. [Google Scholar] [CrossRef] [Green Version]
- Beckman Coulter. SYNCRON System(s). Albumin, REF 467858. Chemistry Information Sheet A18449 AF; Beckman Coulter, Inc.: Pasadena, CA, USA, 2015. [Google Scholar]
- Tate, J.R.; Berg, K.; Couderc, R.; Dati, F.; Kostner, G.M.; Marcovina, S.M.; Rifai, N.; Sakurabayashi, I.; Steinmetz, A. International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) Standardization Project for the Measurement of Lipoprotein(a). Phase 2: Selection and properties of a proposed secondary reference material for lipoprotein(a). Clin. Chem. Lab. Med. 1999, 37, 949–958. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Vermeulen, A.; Verdonck, L.; Kaufman, J.M. A critical evaluation of simple methods for the estimation of free testosterone in serum. J. Clin. Endocrinol. Metab. 1999, 84, 3666–3672. [Google Scholar] [CrossRef]
- Powe, C.E.; Evans, M.K.; Wenger, J.; Zonderman, A.B.; Berg, A.H.; Nalls, M.; Tamez, H.; Zhang, D.; Bhan, I.; Karumanchi, S.A.; et al. Vitamin D–Binding Protein and Vitamin D Status of Black Americans and White Americans. N. Engl. J. Med. 2013, 369, 1991–2000. [Google Scholar] [CrossRef] [Green Version]
- Rojas, R.; Aguilar-Salinas, C.A.; Jiménez-Corona, A.; Shamah-Levy, T.; Rauda, J.; Ávila-Burgos, L.; Villalpando, S.; Lazcano Ponce, E. Metabolic syndrome in Mexican adults: Results from the National Health and Nutrition Survey 2006. Salud Publica Mex. 2010, 52, S11–S18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of medical care in Diabetes-2018. Diabetes Care 2018, 41 (Suppl. 1), S13–S27. [Google Scholar] [CrossRef] [Green Version]
- Simental-Mendía, L.E.; Rodríguez-Morán, M.; Guerrero-Romero, F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab. Syndr. Relat. Disord. 2008, 6, 299–304. [Google Scholar] [CrossRef]
- Babic, N.; Valjevac, A.; Zaciragic, A.; Avdagic, N.; Zukic, S.; Hasic, S. The Triglyceride/HDL Ratio and Triglyceride Glucose Index as Predictors of Glycemic Control in Patients with Diabetes Mellitus Type 2. Med. Arch. 2019, 73, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A. Visceral adiposity index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef] [Green Version]
- Méndez-Hernández, P.; Dosamantes-Carrasco, L.D.; Siani, C.; Pierlot, R.; Martínez-Gómez, M.; Rivera-Paredez, B.; Cervantes-Popoca, L.; Rojas-Lima, E.; Salazar-Martínez, E.; Flores, Y.N.; et al. Mealtime habits and risk of developing the metabolic syndrome or insulin resistance among Mexican adults. Br. J. Nutr. 2016, 116, 1824–1833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernández-Avila, M.; Resoles, M.; Parra, S.; Romieu, I. Sistema de Evaluación de Hábitos Nutricionales y Consumo de Nutrimentos (SNUT); INSP Mexico: Cuernavaca, Mexico, 2000. [Google Scholar]
- Martínez-González, M.A.; López-Fontana, C.; Varo, J.J.; Sánchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses Health Study and the Health Professionals Follow-up Study. Public Health Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef]
- Powe, C.E.; Ricciardi, C.; Berg, A.H.; Erdenesanaa, D.; Collerone, G.; Ankers, E.; Wenger, J.; Karumanchi, S.A.; Thadhani, R.; Bhan, I. Vitamin D-binding protein modifies the vitamin D-bone mineral density relationship. J. Bone Miner. Res. 2011, 26, 1609–1616. [Google Scholar] [CrossRef]
- Thambiah, S.C.; Wong, T.H.; Gupta, E.D.; Radhakrishnan, A.K.; Gun, S.C.; Chembalingam, G.; Lai, L.C.; Yeap, S.S. Calculation of free and bioavailable vitamin D and its association with bone mineral density in Malaysian women. Malays. J. Pathol. 2018, 40, 287–294. [Google Scholar] [CrossRef]
- Rosen, C.J.; Adams, J.S.; Bikle, D.D.; Black, D.M.; Demay, M.B.; Manson, J.E.; Murad, M.H.; Kovacs, C.S. The nonskeletal effects of vitamin D: An Endocrine Society scientific statement. Endocr. Rev. 2012, 33, 456–492. [Google Scholar] [CrossRef] [Green Version]
- Pelczyńska, M.; Grzelak, T.; Sperling, M.; Bogdański, P.; Pupek-Musialik, D.; Czyzewska, K. Impact of 25-hydroxyVitamin D, free & bioavailable fractions of Vitamin D, & Vitamin D binding protein levels on metabolic syndrome components. Arch. Med. Sci. 2017. [Google Scholar] [CrossRef]
- Wang, J.; Eliassen, A.H.; Spiegelman, D.; Willett, W.C.; Hankinson, S.E. Plasma free 25-hydroxyvitamin D, vitamin D binding protein, and risk of breast cancer in the Nurses’ Health Study II. Cancer Causes Control 2014, 25, 819–827. [Google Scholar] [CrossRef] [Green Version]
- Oleröd, G.; Hultén, L.M.; Hammarsten, O.; Klingberg, E. The variation in free 25-hydroxy vitamin D and vitamin D-binding protein with season and vitamin D status. Endocr. Connect. 2017, 6, 111–120. [Google Scholar] [CrossRef] [Green Version]
- Karlsson, T.; Osmancevic, A.; Jansson, N.; Hulthén, L.; Holmäng, A.; Larsson, I. Increased vitamin D-binding protein and decreased free 25(OH)D in obese women of reproductive age. Eur. J. Nutr. 2014, 53, 259–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walsh, J.S.; Evans, A.L.; Bowles, S.; Naylor, K.E.; Jones, K.S.; Schoenmakers, I.; Jacques, R.M.; Eastell, R. Free 25-hydroxyvitamin D is low in obesity, but there are no adverse associations with bone health. Am. J. Clin. Nutr. 2016, 103, 1465–1471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, J.B.; Gallagher, J.C.; Jorde, R.; Berg, V.; Walsh, J.; Eastell, R.; Evans, A.L.; Bowles, S.; Naylor, K.E.; Jones, K.S.; et al. Determination of Free 25(OH)D Concentrations and Their Relationships to Total 25(OH)D in Multiple Clinical Populations. J. Clin. Endocrinol. Metab. 2018, 103, 3278–3288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Sabeh, M.; Ghanem, P.; Al-Shaar, L.; Rahme, M.; Baddoura, R.; Halaby, G.; Singh, R.J.; Vanderschueren, D.; Bouillon, R.; El-Hajj Fuleihan, G. Total, Bioavailable, and Free 25(OH)D Relationship with Indices of Bone Health in Elderly: A Randomized Controlled Trial. J. Clin. Endocrinol. Metab. 2021, 106, e990–e1001. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Ajani, U.A.; McGuire, L.C.; Liu, S. Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care 2005, 28, 1228–1230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chacko, S.A.; Song, Y.; Manson, J.A.E.; Van Horn, L.; Eaton, C.; Martin, L.W.; McTiernan, A.; Curb, J.D.; Wylie-Rosett, J.; Phillips, L.S.; et al. Serum 25-hydroxyvitamin D concentrations in relation to cardiometabolic risk factors and metabolic syndrome in postmenopausal women. Am. J. Clin. Nutr. 2011, 94, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Kayaniyil, S.; Harris, S.B.; Retnakaran, R.; Vieth, R.; Knight, J.A.; Gerstein, H.C.; Perkins, B.A.; Zinman, B.; Hanley, A.J. Prospective association of 25(OH)D with metabolic syndrome. Clin. Endocrinol. 2014, 80, 502–507. [Google Scholar] [CrossRef] [Green Version]
- Ju, S.Y.; Jeong, H.S.; Kim, D.H. Blood vitamin D status and metabolic syndrome in the general adult population: A dose-response meta-analysis. J. Clin. Endocrinol. Metab. 2014, 99, 1053–1063. [Google Scholar] [CrossRef]
- Chen, C.; Chen, Y.; Weng, P.; Xia, F.; Li, Q.; Zhai, H.; Wang, N.; Lu, Y. Association of 25-hydroxyvitamin D with cardiometabolic risk factors and metabolic syndrome: A mendelian randomization study. Nutr. J. 2019, 18, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naderpoor, N.; Shorakae, S.; Abell, S.K.; Mousa, A.; Joham, A.E.; Moran, L.J.; Stepto, N.K.; Spritzer, P.M.; Teede, H.J.; de Courten, B. Bioavailable and free 25-hydroxyvitamin D and vitamin D binding protein in polycystic ovary syndrome: Relationships with obesity and insulin resistance. J. Steroid Biochem. Mol. Biol. 2018, 177, 209–215. [Google Scholar] [CrossRef]
- Lee, C.C.; Young, K.A.; Norris, J.M.; Rotter, J.I.; Liu, Y.; Lorenzo, C.; Wagenknecht, L.E.; Cole, D.E.; Haffner, S.M.; Chen, Y.D.I.; et al. Association of directly measured plasma free 25(OH)D with insulin sensitivity and secretion: The IRAS Family Study. J. Clin. Endocrinol. Metab. 2017, 102, 2781–2788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bacha, F.; Bartz, S.K.; Tomsa, A.; Sharma, S. Free Vitamin D: Relationship to Insulin Sensitivity and Vascular Health in Youth. J. Pediatr. 2019, 212, 28–34. [Google Scholar] [CrossRef]
- Peris, P.; Filella, X.; Monegal, A.; Guañabens, N.; Foj, L.; Bonet, M.; Boquet, D.; Casado, E.; Cerdá, D.; Erra, A.; et al. Comparison of total, free and bioavailable 25-OH vitamin D determinations to evaluate its biological activity in healthy adults: The LabOscat study. Osteoporos. Int. 2017, 28, 2457–2464. [Google Scholar] [CrossRef] [PubMed]
- Mejía-Rodríguez, F.; Camacho-Cisneros, M.; García-Guerra, A.; Monterrubio-Flores, E.; Shamah-Levy, T.; Villalpando Hernández, S. Factors associated with nutritional supplement consumption in Mexican women aged 12 to 49 years. Arch. Latinoam. Nutr. 2008, 58, 164–173. [Google Scholar] [PubMed]
- Bikle, D.D.; Malmstroem, S.; Schwartz, J. Current Controversies: Are Free Vitamin Metabolite Levels a More Accurate Assessment of Vitamin D Status than Total Levels? Endocrinol. Metab. Clin. N. Am. 2017, 46, 901–918. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D.; Bouillon, R.; Thadhani, R.; Schoenmakers, I. Vitamin D metabolites in captivity? Should we measure free or total 25(OH)D to assess vitamin D status? J. Steroid Biochem. Mol. Biol. 2017, 173, 105–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Parameter | Men | Women | |
|---|---|---|---|
| n = 582 | n = 1322 | p Value | |
| Age (years) a | 46 (36–57) | 54 (43–63) | <0.001 |
| Leisure time physical activity (hour/week) a | 1.7 (0.4–5.0) | 1.1 (0.2–3.5) | <0.001 |
| Active (>150 min/week), % | 36.6 | 28.4 | 0.008 |
| Smoking status | |||
| Current, % | 21.0 | 8.6 | <0.001 |
| Past, % | 39.0 | 22.5 | <0.001 |
| BMI (kg/m2) a | 26.5 (24.1–29.0) | 26.8 (24.0–30.1) | 0.150 |
| Overweight, % | 48.9 | 40.3 | <0.001 |
| Obesity, % | 19.5 | 25.7 | 0.003 |
| Body fat proportion a | 31.5 (27.7–34.7) | 45.1 (40.7–49.1) | <0.001 |
| Metabolic syndrome (ATP III definition) b, % | 45.9 | 55.5 | <0.001 |
| Waist circumference (cm) a | 96 (90–102) | 92 (85–100) | <0.001 |
| Systolic blood pressure (mmHg) a | 122 (113–131) | 116 (106–129) | <0.001 |
| Diastolic blood pressure (mmHg) a | 77 (70–84) | 73 (66–79) | <0.001 |
| Elevated blood pressure, % | 43.0 | 37.0 | 0.010 |
| Fasting glucose(mg/dL) | 98 (92–107) | 96 (90–104) | <0.001 |
| Impaired glucose tolerance, % | 33.1 | 24.8 | <0.001 |
| Type 2 Diabetes, % | 15.0 | 14.3 | 0.680 |
| HDL-c(mg/dL) a | 39 (34–46) | 46 (39–54) | 0.007 |
| Triglycerides(mg/dL) a | 168 (118–247) | 151 (109–199) | <0.001 |
| HOMA-IR (>3.2) c, % | 35.1 | 32.4 | 0.370 |
| TyG index a,d | 4.3 (2.8–6.7) | 3.3 (2.1–4.8) | <0.001 |
| TG/HDL-c ratio a | 9.0 (8.7–9.5) | 8.9 (8.6–9.2) | <0.001 |
| Visceral adiposity index a | 2.6 (1.7–4.0) | 2.9 (1.8–4.1) | <0.001 |
| Total 25(OH)D (ng/mL) a | 22.1 (18.3–26.9) | 20.8 (16.7–24.8) | <0.001 |
| Free 25(OH)D-SNP adjusted (pg/mL) a,e | 7.1 (5.2–9.5) | 6.4 (4.6–8.6) | <0.001 |
| Bioavailable 25(OH)D-SNP adjusted (ng/mL) a,e | 2.7 (2.0–3.7) | 2.4 (1.7–3.2) | <0.001 |
| Albumin (g/dL) a | 4.3 (4.1–4.5) | 4.2 (4.0–4.4) | <0.001 |
| Vitamin D deficiency (<20 ng/mL), % | 36.3 | 44.6 | 0.0008 |
| Vitamin D-binding protein (µmol/L) a | 263.8 (229.6–303.8) | 275.3 (234.0–318.4) | 0.003 |
| Vitamin D intake (UI/day) a | 145.2 (75.8–259.3) | 144.5 (85.0–248.6) | 0.370 |
| Alcohol(g/day) a | 2.7 (0.6–7.4) | 0.6 (0.0–1.8) | <0.001 |
| Parameter | Total 25(OH)D (ng/mL) Median (95% CI) | p Value | Free 25(OH)D- SNP Adjusted a (pg/mL) Median (95% CI) | p Value | Bioavailable 25-(OH)D-SNP Adjusted a (ng/mL) Median (95% CI) | p Value |
|---|---|---|---|---|---|---|
| BMI b | ||||||
| Normal | 22.0 (21.4,22.6) | Ref. | 6.8 (6.5,7.0) | Ref. | 2.7 (2.5,2.8) | Ref. |
| Overweight | 20.8 (20.3,21.4) | 0.008 | 6.6 (6.4,6.9) | 0.260 | 2.5 (2.4,2.6) | 0.013 |
| Obesity | 20.4 (19.7,21.1) | 0.001 | 6.3 (6.0,6.6) | 0.023 | 2.3 (2.2,2.4) | <0.001 |
| Body fat proportion c,d | ||||||
| Low | 21.9 (21.4,22.7) | Ref. | 7.1 (6.9,7.4) | Ref. | 2.7 (2.6,2.9) | Ref. |
| Medium | 21.2 (20.6,21.7) | 0.220 | 6.4 (6.2,6.7) | 0.180 | 2.5 (2.3,2.6) | 0.130 |
| High | 20.2 (19.5,20.9) | 0.005 | 6.1 (5.9,6.4) | 0.038 | 2.3 (2.2,2.4) | 0.015 |
| Metabolic syndrome-ATP III c | ||||||
| No | 22.0 (21.5,22.4) | 6.9 (6.6,7.1) | 2.6 (2.5,2.7) | |||
| Yes | 20.3 (19.8,20.7) | <0.001 | 6.3 (6.1,6.5) | 0.001 | 2.4 (2.3,2.5) | <0.001 |
| High waist circumference c | ||||||
| No | 21.9 (21.4,22.4) | 6.8 (6.6,7.1) | 2.6 (2.5,2.7) | |||
| Yes | 20.4 (20.0,20.9) | <0.001 | 6.4 (6.2,6.6) | 0.060 | 2.4 (2.3,2.5) | 0.024 |
| Elevated blood pressure c | ||||||
| No | 21.3 (20.9,21.8) | 6.7 (6.5,6.9) | 2.6 (2.5,2.6) | |||
| Yes | 20.7 (20.1,21.2) | 0.070 | 6.3 (6.1,6.6) | 0.004 | 2.4 (2.3,2.5) | 0.003 |
| Type 2 diabetes c | ||||||
| No | 21.6 (21.1,22.1) | Ref. | 6.7 (6.5,6.9) | Ref. | 2.5 (2.4,2.6) | Ref. |
| Impaired glucose tolerance | 20.6 (20.3,21.3) | 0.010 | 6.8 (6.5,7.1) | 0.630 | 2.5 (2.4,2.7) | 0.710 |
| Yes | 19.8 (18.9,20.7) | <0.001 | 6.1 (5.6,6.5) | 0.020 | 2.3 (2.1,2.4) | 0.025 |
| HDL-c c | ||||||
| Normal | 21.5 (21.0,22.1) | Ref. | 6.8 (6.6,7.0) | Ref. | 2.6 (2.5,2.7) | Ref. |
| Low | 20.8 (20.4,21.3) | 0.05 | 6.5 (6.3,6.7) | 0.150 | 2.4 (2.3,2.5) | 0.025 |
| Triglycerides c | ||||||
| Normal | 22.5 (22.1,23.0) | Ref. | 7.1 (6.9,7.3) | Ref. | 2.7 (2.6,2.8) | Ref. |
| High | 20.0 (19.6,20.5) | <0.001 | 6.1 (5.9,6.3) | <0.001 | 2.3 (2.2,2.4) | <0.001 |
| TyG index c,d,e | ||||||
| Low | 22.9 (22.4,23.5) | Ref. | 7.2 (6.9,7.4) | Ref. | 2.7 (2.6,2.8) | Ref. |
| Medium | 21.0 (20.5,21.6) | <0.001 | 6.6 (6.4,6.9) | 0.001 | 2.5 (2.4,2.6) | 0.004 |
| High | 19.5 (18.9,20.0) | <0.001 | 6.1 (5.8,6.4) | <0.001 | 2.3 (2.2,2.4) | <0.001 |
| TG/HDL-c ratio c,d | ||||||
| Low | 22.9 (22.3,23.5) | Ref. | 7.2 (7.0,7.5) | Ref. | 2.7 (2.6,2.8) | Ref. |
| Medium | 20.8 (20.2,21.4) | <0.001 | 6.5 (6.3,6.8) | <0.001 | 2.5 (2.4,2.6) | 0.001 |
| High | 19.9 (19.3,20.5) | <0.001 | 6.2 (5.9,6.4) | <0.001 | 2.3 (2.2,2.4) | <0.001 |
| Visceral adiposity index (VAI) c,d | ||||||
| Low | 22.8 (22.3,23.4) | Ref. | 7.1 (6.9,7.4) | Ref. | 2.7 (2.6,2.8) | Ref. |
| Medium | 21.1 (20.5,21.6) | <0.001 | 6.7 (6.4,6.9) | 0.050 | 2.5 (2.4,2.6) | 0.045 |
| High | 19.7 (19.1,20.2) | <0.001 | 6.1 (5.8,6.3) | <0.001 | 2.3 (2.2,2.4) | <0.001 |
| HOMA-IR (>3.2) c,f | ||||||
| No | 21.4 (20.9,21.8) | 0.002 | 6.5 (6.3,6.8) | 0.080 | 2.5 (2.4,2.6) | 0.010 |
| Yes | 20.0 (19.4,20.7) | 6.3 (5.9,6.6) | 2.3 (2.1,2.4) | |||
| 25(OH)D (ng/mL) | p Value | Free 25(OH)D SNP Adjusted (pg/mL) a | p Value | Bioavailable 25(OH)D SNP Adjusted a (ng/mL) | p Value | |
|---|---|---|---|---|---|---|
| Outcome b | OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| BMI | ||||||
| Normal | Ref. | Ref. | Ref. | |||
| Overweight | 0.97 (0.95,0.99) | 0.001 | 0.98 (0.95,1.01) | 0.20 | 0.93 (0.85,1.00) | 0.07 |
| Obesity | 0.95 (0.93,0.97) | <0.001 | 0.69 (0.54,0.88) | 0.24 | 0.89 (0.86,0.99) | 0.031 |
| Body fat proportion | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.98 (0.97,1.00) | 0.09 | 0.98 (0.94,1.03) | 0.45 | 0.93 (0.82,1.05) | 0.23 |
| High | 0.96 (0.93,0.98) | 0.001 | 0.96 (0.92,1.01) | 0.15 | 0.86 (0.75,0.98) | 0.022 |
| Metabolic syndrome-ATP III | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.95 (0.94,0.97) | <0.001 | 0.96 (0.93,0.99) | 0.003 | 0.88 (0.81,0.95) | 0.001 |
| Metabolic syndrome-ATP III c | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.96 (0.95–0.98) | <0.001 | 0.95 (0.92–0.99) | 0.006 | 0.89 (0.81–0.97) | 0.007 |
| High waist circumference | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.96 (0.95,0.98) | <0.001 | 0.99 (0.96,1.02) | 0.55 | 0.94 (0.86,1.01) | 0.12 |
| Type 2 diabetes | ||||||
| No | Ref. | Ref. | Ref. | |||
| Impaired glucose tolerance | 0.98 (0.96,0.99) | 0.025 | 0.99 (0.95,1.02) | 0.41 | 0.98 (0.90,1.07) | 0.63 |
| Yes | 0.94 (0.92,0.97) | <0.001 | 0.95 (0.90,0.99) | 0.015 | 0.86 (0.77,0.97) | 0.016 |
| Type 2 diabetes c | ||||||
| No | Ref. | Ref. | Ref. | |||
| Impaired glucose tolerance | 0.99 (0.97–1.01) | 0.154 | 0.99 (0.96–1.02) | 0.497 | 0.99 (0.91–1.08) | 0.882 |
| Yes | 0.95 (0.93–0.97) | <0.001 | 0.95 (0.91–0.99) | 0.023 | 0.88 (0.78–0.99) | 0.036 |
| Elevated blood pressure | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.98 (0.97,0.99) | 0.042 | 0.96 (0.94,0.99) | 0.044 | 0.93 (0.85,1.00) | 0.060 |
| Elevated blood pressure c | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.99 (0.98–1.01) | 0.405 | 0.97 (0.94–1.00) | 0.065 | 0.94 (0.86–1.02) | 0.158 |
| Low HDL-c | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.98 (0.97,0.99) | 0.015 | 0.99 (0.96,1.02) | 0.440 | 0.94 (0.87,1.01) | 0.09 |
| Low HDL-c c | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.99 (0.97–1.00) | 0.133 | 0.99 (0.96–1.02) | 0.579 | 0.95 (0.88–1.02) | 0.179 |
| High triglycerides | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.93 (0.92,0.95) | <0.001 | 0.89 (0.87,0.92) | <0.001 | 0.75 (0.70,0.82) | <0.001 |
| High triglycerides c | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.94 (0.92–0.95) | <0.001 | 0.90 (0.87–0.92) | <0.001 | 0.76 (0.70–0.82) | <0.001 |
| TyG index d,e | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.95 (0.94,0.97) | <0.001 | 0.95 (0.92,0.98) | 0.002 | 0.85 (0.79,0.94) | 0.001 |
| High | 0.93 (0.91,0.95) | <0.001 | 0.88 (0.84,0.91) | <0.001 | 0.73 (0.66,0.80) | <0.001 |
| TyG index c,d,e | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.96 (0.94–0.98) | <0.001 | 0.95 (0.91–0.98) | 0.002 | 0.86 (0.79–0.95) | 0.002 |
| High | 0.91 (0.89–0.93) | <0.001 | 0.88 (0.84–0.91) | <0.001 | 0.73 (0.66–0.81) | <0.001 |
| TG/HDL ratio d | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.96 (0.94,0.98) | <0.001 | 0.94 (0.90,0.97) | <0.001 | 0.85 (0.75,0.90) | <0.001 |
| High | 0.91 (0.89,0.93) | <0.001 | 0.90 (0.86,0.93) | <0.001 | 0.74 (0.67,0.82) | <0.001 |
| TG/HDL ratio b,d | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.96 (0.94–0.97) | <0.001 | 0.93 (0.90–0.97) | <0.001 | 0.82 (0.75–0.90) | <0.001 |
| High | 0.58 (0.44–0.76) | <0.001 | 0.89 (0.86–0.93) | <0.001 | 0.75 (0.68–0.83) | <0.001 |
| Visceral adiposity index (VAI) d | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.96 (0.94,0.98) | <0.001 | 0.95 (0.92,0.99) | 0.005 | 0.86 (0.79,0.94) | 0.001 |
| High | 0.92 (0.90,0.94) | <0.001 | 0.90 (0.87,0.93) | <0.001 | 0.75 (0.68,0.83) | <0.001 |
| Visceral adiposity index (VAI) c,d | ||||||
| Low | Ref. | Ref. | Ref. | |||
| Medium | 0.96 (0.94–0.98) | <0.001 | 0.95 (0.92–0.99) | 0.006 | 0.87 (0.79–0.95) | 0.002 |
| High | 0.93 (0.91–0.95) | <0.001 | 0.90 (0.95–0.93) | <0.001 | 0.76 (0.69–0.84) | <0.001 |
| HOMA–IR (>3.2) f | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.96 (0.94,0.98) | <0.001 | 0.97 (0.94,1.01) | 0.18 | 0.92 (0.83,1.01) | 0.091 |
| HOMA–IR (>3.2) c,f | ||||||
| No | Ref. | Ref. | Ref. | |||
| Yes | 0.97 (0.95–0.99) | 0.006 | 0.98 (0.94–1.02) | 0.307 | 0.94 (0.84–1.05) | 0.294 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rivera-Paredez, B.; Hidalgo-Bravo, A.; León-Reyes, G.; León-Maldonado, L.S.; Aquino-Gálvez, A.; Castillejos-López, M.; Denova-Gutiérrez, E.; Flores, Y.N.; Salmerón, J.; Velázquez-Cruz, R. Total, Bioavailable, and Free 25-Hydroxyvitamin D Equally Associate with Adiposity Markers and Metabolic Traits in Mexican Adults. Nutrients 2021, 13, 3320. https://doi.org/10.3390/nu13103320
Rivera-Paredez B, Hidalgo-Bravo A, León-Reyes G, León-Maldonado LS, Aquino-Gálvez A, Castillejos-López M, Denova-Gutiérrez E, Flores YN, Salmerón J, Velázquez-Cruz R. Total, Bioavailable, and Free 25-Hydroxyvitamin D Equally Associate with Adiposity Markers and Metabolic Traits in Mexican Adults. Nutrients. 2021; 13(10):3320. https://doi.org/10.3390/nu13103320
Chicago/Turabian StyleRivera-Paredez, Berenice, Alberto Hidalgo-Bravo, Guadalupe León-Reyes, Leith S. León-Maldonado, Arnoldo Aquino-Gálvez, Manuel Castillejos-López, Edgar Denova-Gutiérrez, Yvonne N. Flores, Jorge Salmerón, and Rafael Velázquez-Cruz. 2021. "Total, Bioavailable, and Free 25-Hydroxyvitamin D Equally Associate with Adiposity Markers and Metabolic Traits in Mexican Adults" Nutrients 13, no. 10: 3320. https://doi.org/10.3390/nu13103320







