Nutrition Care Practices of Dietitians and Oral Health Professionals for Oral Health Conditions: A Scoping Review
Abstract
:1. Introduction
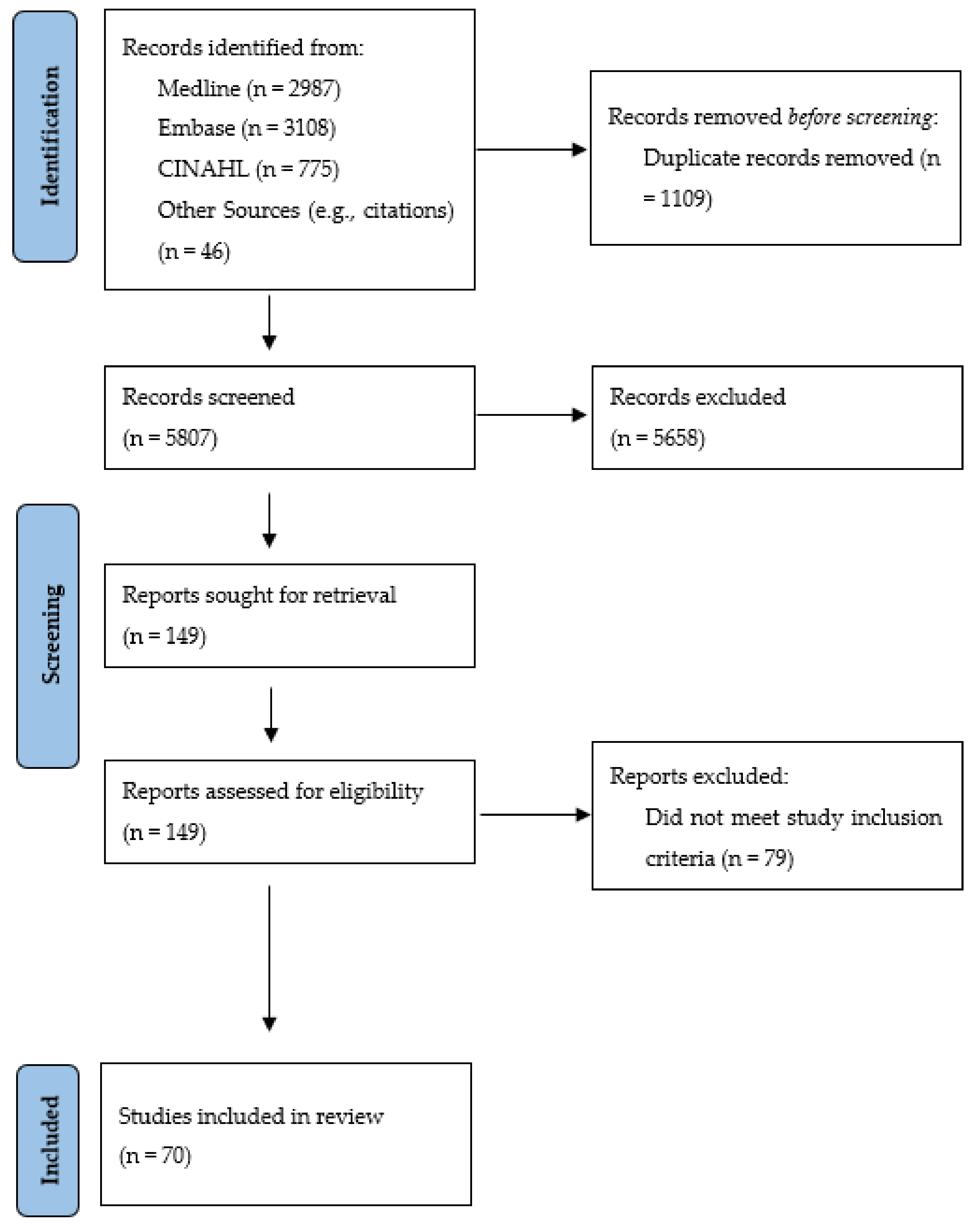
2. Materials and Methods
3. Results
3.1. Assessment Practices
3.1.1. Oral Health Professionals
General/Unspecific Dietary Assessment Practices
Use of Specific Dietary Assessment Tools
Inquiries about Specific Patient Behaviours or Concerns Related to Diet
3.1.2. Dietitians and Nutritionists
3.2. Intervention Practices
3.2.1. Oral Health Professionals
General/Unspecific Nutrition Intervention Practices
Types of Resources/Strategies Used
Types of Nutrition Information Provided
Barriers Regarding Intervention Practices
3.2.2. Dietitians and Nutritionists
3.2.3. Collaboration between Dietitians and Oral Health Professionals
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [Green Version]
- Bernabe, E.; Marcenes, W.; Hernandez, C.R.; Bailey, J.; Abreu, L.G.; Alipour, V.; Amini, S.; Arabloo, J.; Arefi, Z.; Arora, A.; et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J. Dent. Res. 2020, 99, 362–373. [Google Scholar] [PubMed]
- Health Canada. Report on the Findings of the Oral Health Component of the Canadian Health Measures Survey 2007–2009; Health Canada: Ottawa, ON, Canada, 2010; ISBN 9781100156606. [Google Scholar]
- Schroth, R.J.; Quiñonez, C.; Shwart, L.; Wagar, B. Treating Early Childhood Caries under General Anesthesia: A National Review of Canadian Data. J. Can. Dent. Assoc. 2016, 82, g20. [Google Scholar] [PubMed]
- World Health Organization. Oral Health. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 30 September 2021).
- Jensen, M.E. Diet and dental caries. Dent. Clin. N. Am. 1999, 43, 615–633. [Google Scholar]
- Touger-Decker, R.; van Loveren, C. Sugars and dental caries. Am. J. Clin. Nutr. 2003, 78, 881S–892S. [Google Scholar] [CrossRef] [Green Version]
- Touger-Decker, R.; Mobley, C. Position of the Academy of Nutrition and Dietetics: Oral health and nutrition. J. Acad. Nutr. Diet. 2013, 113, 693–701. [Google Scholar] [CrossRef]
- Moynihan, P.J. Dietary advice in dental practice. Br. Dent. J. 2002, 193, 563–568. [Google Scholar] [CrossRef] [Green Version]
- Salas, M.M.S.; Nascimento, G.G.; Vargas-Ferreira, F.; Tarquinio, S.B.C.; Huysmans, M.C.D.N.J.M.; Demarco, F.F. Diet influenced tooth erosion prevalence in children and adolescents: Results of a meta-analysis and meta-regression. J. Dent. 2015, 43, 865–875. [Google Scholar] [CrossRef]
- Buzalaf, M.A.R.; Magalhães, A.C.; Rios, D. Prevention of erosive tooth wear: Targeting nutritional and patient-related risks factors. Br. Dent. J. 2018, 224, 371–378. [Google Scholar] [CrossRef]
- Palmer, C.A. Important Relationships Between Diet, Nutrition, and Oral Health. Nutr. Clin. Care 2001, 4, 4–14. [Google Scholar] [CrossRef]
- Tinanoff, N.; Palmer, C.A. Dietary determinants of dental caries and dietary recommendations for preschool children. J. Public Health Dent. 2000, 60, 197–199. [Google Scholar] [CrossRef]
- Moynihan, P.; Petersen, P.E. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004, 7, 201–226. [Google Scholar] [CrossRef]
- Scardina, G.A.; Messina, P. Good oral health and diet. J. Biomed. Biotechnol. 2012, 2012, 720692. [Google Scholar] [CrossRef] [Green Version]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Zohaib, S.; Almas, K. The Role of Nutrition in Periodontal Health: An Update. Nutrients 2016, 8, 530. [Google Scholar] [CrossRef]
- Bhattacharya, P.T.; Misra, S.R.; Hussain, M. Nutritional Aspects of Essential Trace Elements in Oral Health and Disease: An Extensive Review. Scientifica 2016, 2016, 5464373. [Google Scholar] [CrossRef] [Green Version]
- Dietitians Association of Australia; Dental Health Services Victoria. Joint Position Statement on Oral Health and Nutrition October 2015. 2015. Available online: https://dietitiansaustralia.org.au/wp-content/uploads/2016/05/DAA-DHSV-Joint-Statement-Oral-Health-and-Nutrition.pdf (accessed on 30 September 2021).
- NHS Health Scotland. Oral Health and Nutrition Guidance for Professionals June 2012. 2012. Available online: https://www.scottishdental.org/wp-content/uploads/2014/10/OralHealthAndNutritionGuidance.pdf (accessed on 30 September 2021).
- American Academy of Pediatric Dentistry Clinical Affairs Committee; American Academy of Pediatric Dentistry Council on Clinical Affairs. Policy on Dietary Recommendations for Infants, Children, and Adolescents. Pediatr. Dent. 2017, 39, 64–66. [Google Scholar]
- Jones, A.C.; Kirkpatrick, S.I.; Hammond, D. Beverage consumption and energy intake among Canadians: Analyses of 2004 and 2015 national dietary intake data. Nutr. J. 2019, 18, 60. [Google Scholar] [CrossRef] [Green Version]
- Canadian Dental Association. CDA Position on Early Childhood Caries. 2010. Available online: https://www.cda-adc.ca/en/about/position_statements/ecc/ (accessed on 30 September 2021).
- Canadian Dental Association. The State of Oral Health in Canada. 2017. Available online: https://www.cda-adc.ca/stateoforalhealth/_files/TheStateofOralHealthinCanada.pdf (accessed on 30 September 2021).
- Petersen, P.E. Global policy for improvement of oral health in the 21st century–implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dent. Oral Epidemiol. 2009, 37, 1–8. [Google Scholar] [CrossRef]
- Franki, J.; Hayes, M.J.; Taylor, J.A. The provision of dietary advice by dental practitioners: A review of the literature. Community Dent. Health 2014, 31, 9–14. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [Green Version]
- FDI. World Dental Federation FDI’s Definition of Oral Health. Available online: https://www.fdiworlddental.org/fdis-definition-oral-health (accessed on 12 May 2021).
- Suga, U.S.G.; Terada, R.S.S.; Ubaldini, A.L.M.; Fujimaki, M.; Pascotto, R.C.; Batilana, A.P.; Pietrobon, R.; Vissoci, J.R.N.; Rodrigues, C.G. Factors that drive dentists towards or away from dental caries preventive measures: Systematic review and metasummary. PLoS ONE 2014, 9, e107831. [Google Scholar] [CrossRef]
- Kay, E.; Vascott, D.; Hocking, A.; Nield, H.; Dorr, C.; Barrett, H. A review of approaches for dental practice teams for promoting oral health. Community Dent. Oral Epidemiol. 2016, 44, 313–330. [Google Scholar] [CrossRef]
- U.S Department of Agriculture Food and Nutrition Service. Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Available online: https://www.fns.usda.gov/wic (accessed on 30 September 2021).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [Green Version]
- Roshan, D.; Curzon, M.E.J.; Fairpo, C.G. Changes in dentists’ attitudes and practice in paediatric dentistry. Eur. J. Paediatr. Dent. 2003, 4, 21–27. [Google Scholar]
- Hawkins, R.J.; Locker, D. Non-clinical information obtained by dentists during initial examinations of older adult patients. Spec. Care Dent. 2005, 25, 12–18. [Google Scholar] [CrossRef]
- Sajnani-Oommen, G.; Perez-Spiess, S.; Julliard, K. Comparison of nutritional counseling between provider types. Pediatr. Dent. 2006, 28, 369–374. [Google Scholar]
- Bubna, S.; Perez-Spiess, S.; Cernigliaro, J.; Julliard, K. Infant oral health care: Beliefs and practices of American Academy of Pediatric Dentistry members. Pediatr. Dent. 2012, 34, 203–209. [Google Scholar]
- Clovis, J.B.; Horowitz, A.M.; Kleinman, D.V.; Wang, M.Q.; Massey, M. Maryland dental hygienists’ knowledge, opinions and practices regarding dental caries prevention and early detection. J. Dent. Hyg. 2012, 86, 292–305. [Google Scholar]
- Mulic, A.; Vidnes-Kopperud, S.; Skaare, A.B.; Tveit, A.B.; Young, A. Opinions on Dental Erosive Lesions, Knowledge of Diagnosis, and Treatment Strategies among Norwegian Dentists: A Questionnaire Survey. Int. J. Dent. 2012, 2012, 716396. [Google Scholar] [CrossRef]
- Garton, B.J.; Ford, P.J. Root caries: A survey of Queensland dentists. Int. J. Dent. Hyg. 2013, 11, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Sim, C.J.; Iida, H.; Vann, W.F.J.; Quinonez, R.B.; Steiner, M.J. Dietary recommendations for infants and toddlers among pediatric dentists in North Carolina. Pediatr. Dent. 2014, 36, 322–328. [Google Scholar] [PubMed]
- Yusuf, H.; Kolliakou, A.; Ntouva, A.; Murphy, M.; Newton, T.; Tsakos, G.; Watt, R.G. Predictors of dentists’ behaviours in delivering prevention in primary dental care in England: Using the theory of planned behaviour. BMC Health Serv. Res. 2016, 16, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Widström, E.; Tillberg, A.; Byrkjeflot, L.I.; Skudutyte-Rysstad, R. Chair-side preventive interventions in the Public Dental Service in Norway. Br. Dent. J. 2016, 221, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Arheiam, A.; Brown, S.L.; Burnside, G.; Higham, S.M.; Albadri, S.; Harris, R.V. The use of diet diaries in general dental practice in England. Community Dent. Health 2016, 33, 267–273. [Google Scholar]
- Halawany, H.S.; Salama, F.; Jacob, V.; Abraham, N.B.; Moharib, T.N.; Alazmah, A.S.; Al Harbi, J.A. A survey of pediatric dentists’ caries-related treatment decisions and restorative modalities-A web-based survey. Saudi Dent. J. 2017, 29, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Dima, S.; Chang, W.-J.; Chen, J.-W.; Teng, N.-C. Early Childhood Caries-Related Knowledge, Attitude, and Practice: Discordance between Pediatricians and Dentists toward Medical Office-Based Prevention in Taiwan. Int. J. Environ. Res. Public Health 2018, 15, 1067. [Google Scholar] [CrossRef] [Green Version]
- Mulic, A.; Arnadottir, I.B.; Jensdottir, T.; Kopperud, S.E. Opinions and Treatment Decisions for Dental Erosive Wear: A Questionnaire Survey among Icelandic Dentists. Int. J. Dent. 2018, 2018, 8572371. [Google Scholar] [CrossRef] [Green Version]
- Kangasmaa, H.; Tanner, T.; Laitala, M.-L.; Mulic, A.; Kopperud, S.E.; Vähänikkilä, H.; Anttonen, V.; Alaraudanjoki, V. Knowledge on and treatment practices of erosive tooth wear among Finnish dentists. Acta Odontol. Scand. 2021, 79, 499–505. [Google Scholar] [CrossRef]
- Mortensen, D.; Mulic, A.; Pallesen, U.; Twetman, S. Awareness, knowledge and treatment decisions for erosive tooth wear: A case-based questionnaire among Danish dentists. Clin. Exp. Dent. Res. 2021, 7, 56–62. [Google Scholar] [CrossRef]
- Fuller, L.A.; Stull, S.C.; Darby, M.L.; Tolle, S.L. Oral health promotion: Knowledge, confidence, and practices in preventing early-severe childhood caries of Virginia WIC program personnel. J. Dent. Hyg. 2014, 88, 130–140. [Google Scholar] [PubMed]
- Gold, J.T.; Tomar, S. Oral Health Knowledge and Practices of WIC Staff at Florida WIC Program. J. Community Health 2016, 41, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, J.B.; Ahearn, K.; Atar, M.; More, F.G.; Sasson, L.; Rosenberg, L.; Godfrey, E.; Sehl, R.; Daronch, M. Interprofessional Educational Experience among Dietitians after a Pediatric Dentistry Clinical Rotation. Top. Clin. Nutr. 2017, 32, 193–201. [Google Scholar] [CrossRef]
- Sarmadi, R.; Gabre, P.; Gahnberg, L. Strategies for caries risk assessment in children and adolescents at public dental clinics in a Swedish county. Int. J. Paediatr. Dent. 2009, 19, 135–140. [Google Scholar] [CrossRef]
- O’Toole, S.; Khan, M.; Patel, A.; Patel, N.J.; Shah, N.; Bartlett, D.; Movahedi, S. Tooth wear risk assessment and care-planning in general dental practice. Br. Dent. J. 2018, 224, 358–362. [Google Scholar] [CrossRef] [Green Version]
- Threlfall, A.G.; Hunt, C.M.; Milsom, K.M.; Tickle, M.; Blinkhorn, A.S. Exploring factors that influence general dental practitioners when providing advice to help prevent caries in children. Br. Dent. J. 2007, 202, E10; discussion 216–217. [Google Scholar] [CrossRef]
- Chisick, M.C.; Richter, P.; Piotrowski, M.J. Dental health promotion and preventive dentistry practices of U.S. Army dentists. Mil. Med. 2000, 165, 604–606. [Google Scholar] [CrossRef] [Green Version]
- Anderson, R.; Treasure, E.T.; Sprod, A.S. Oral health promotion practice: A survey of dental professionals in Wales. Int. J. Health Promot. Educ. 2002, 40, 9–14. [Google Scholar] [CrossRef]
- Dugmore, C.R.; Rock, W.P. Awareness of tooth erosion in 12 year old children and primary care dental practitioners. Community Dent. Health 2003, 20, 223–227. [Google Scholar]
- Freeman, R.; Kerr, G.; Salmon, K.; Speedy, P. Patient-active prevention in primary dental care: A characterisation of general practices in Northern Ireland. Prim. Dent. Care 2005, 12, 42–46. [Google Scholar] [CrossRef]
- Wang, N.J. Caries preventive methods in child dental care reported by dental hygienists, Norway, 1995 and 2004. Acta Odontol. Scand. 2005, 63, 330–334. [Google Scholar] [CrossRef]
- Huang, J.S.; Becerra, K.; Walker, E.; Hovell, M.F. Childhood overweight and orthodontists: Results of a survey. J. Public Health Dent. 2006, 66, 292–294. [Google Scholar] [CrossRef]
- Dyer, T.A.; Robinson, P.G. General health promotion in general dental practice—The involvement of the dental team Part 2: A qualitative and quantitative investigation of the views of practice principals in South Yorkshire. Br. Dent. J. 2006, 201, 45–51; discussion 31. [Google Scholar] [CrossRef] [Green Version]
- Trueblood, R.; Kerins, C.A.; Seale, N.S. Caries risk assessment practices among Texas pediatric dentists. Pediatr. Dent. 2008, 30, 49–53. [Google Scholar]
- Brickhouse, T.H.; Unkel, J.H.; Kancitis, I.; Best, A.M.; Davis, R.D. Infant oral health care: A survey of general dentists, pediatric dentists, and pediatricians in Virginia. Pediatr. Dent. 2008, 30, 147–153. [Google Scholar]
- Kelly, S.A.M.; Moynihan, P.J. Attitudes and practices of dentists with respect to nutrition and periodontal health. Br. Dent. J. 2008, 205, E9; discussion 196–197. [Google Scholar] [CrossRef]
- Csikar, J.; Williams, S.A.; Beal, J. Do smoking cessation activities as part of oral health promotion vary between dental care providers relative to the NHS/private treatment mix offered? A study in West Yorkshire. Prim. Dent. Care 2009, 16, 45–50. [Google Scholar] [CrossRef]
- Satur, J.; Gussy, M.; Marino, R.; Martini, T. Patterns of dental therapists’ scope of practice and employment in Victoria, Australia. J. Dent. Educ. 2009, 73, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Tseveenjav, B.; Virtanen, J.I.; Wang, N.J.; Widström, E. Working profiles of dental hygienists in public and private practice in Finland and Norway. Int. J. Dent. Hyg. 2009, 7, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Malcheff, S.; Pink, T.C.; Sohn, W.; Inglehart, M.R.; Briskie, D. Infant oral health examinations: Pediatric dentists’ professional behavior and attitudes. Pediatr. Dent. 2009, 31, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Manski, M.C.; Parker, M.E. Early childhood caries: Knowledge, attitudes, and practice behaviors of Maryland dental hygienists. J. Dent. Hyg. 2010, 84, 190–195. [Google Scholar]
- Salama, F.; Kebriaei, A. Oral care for infants: A survey of Nebraska general dentists. Gen. Dent. 2010, 58, 182–187. [Google Scholar]
- Ananaba, N.; Malcheff, S.; Briskie, D.; Inglehart, M.R. Infant oral health examinations: Attitudes and professional behavior of general and pediatric dentists in Michigan and pediatric dentists in the U.S. J. Mich. Dent. Assoc. 2010, 92, 38–43. [Google Scholar]
- Cunha-Cruz, J.; Wataha, J.C.; Zhou, L.; Manning, W.; Trantow, M.; Bettendorf, M.M.; Heaton, L.J.; Berg, J. Treating dentin hypersensitivity: Therapeutic choices made by dentists of the northwest PRECEDENT network. J. Am. Dent. Assoc. 2010, 141, 1097–1105. [Google Scholar] [CrossRef]
- Lee, J.Y.; Caplan, D.J.; Gizlice, Z.; Ammerman, A.; Agans, R.; Curran, A.E. US pediatric dentists’ counseling practices in addressing childhood obesity. Pediatr. Dent. 2012, 34, 245–250. [Google Scholar]
- Kakudate, N.; Sumida, F.; Matsumoto, Y.; Manabe, K.; Yokoyama, Y.; Gilbert, G.H.; Gordan, V.V. Restorative treatment thresholds for proximal caries in dental PBRN. J. Dent. Res. 2012, 91, 1202–1208. [Google Scholar] [CrossRef] [Green Version]
- Yokoyama, Y.; Kakudate, N.; Sumida, F.; Matsumoto, Y.; Gilbert, G.H.; Gordan, V.V. Dentists’ dietary perception and practice patterns in a dental practice-based research network. PLoS ONE 2013, 8, e59615. [Google Scholar] [CrossRef] [Green Version]
- Yokoyama, Y.; Kakudate, N.; Sumida, F.; Matsumoto, Y.; Gilbert, G.H.; Gordan, V.V. Dentists’ practice patterns regarding caries prevention: Results from a dental practice-based research network. BMJ Open 2013, 3, e003227. [Google Scholar] [CrossRef]
- Hussein, R.J.; Schneller, T.; Walter, U. Preventive activity of dentists and its associations with dentist and dental practice characteristics in northern Germany. J. Public Health 2013, 21, 455–463. [Google Scholar] [CrossRef]
- Gnich, W.; Deas, L.; Mackenzie, S.; Burns, J.; Conway, D.I. Extending dental nurses’ duties: A national survey investigating skill-mix in Scotland’s child oral health improvement programme (Childsmile). BMC Oral Health 2014, 14, 137. [Google Scholar] [CrossRef] [Green Version]
- Yusuf, H.; Tsakos, G.; Ntouva, A.; Murphy, M.; Porter, J.; Newton, T.; Watt, R.G. Differences by age and sex in general dental practitioners’ knowledge, attitudes and behaviours in delivering prevention. Br. Dent. J. 2015, 219, E7. [Google Scholar] [CrossRef] [PubMed]
- Hayes, M.J.; Wallace, J.P.; Coxon, A. Attitudes and barriers to providing dietary advice: Perceptions of dental hygienists and oral health therapists. Int. J. Dent. Hyg. 2016, 14, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Baatsch, B.; Zimmer, S.; Rodrigues Recchia, D.; Bussing, A. Complementary and alternative therapies in dentistry and characteristics of dentists who recommend them. Complement. Ther. Med. 2017, 35, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Hayes, M.J.; Cheng, B.; Musolino, R.; Rogers, A.A. Dietary analysis and nutritional counselling for caries prevention in dental practise: A pilot study. Aust. Dent. J. 2017, 62, 485–492. [Google Scholar] [CrossRef] [Green Version]
- Wright, R.; Casamassimo, P.S. Assessing attitudes and actions of pediatric dentists toward childhood obesity and sugar-sweetened beverages. J. Public Health Dent. 2017, 77 (Suppl. S1), S79–S87. [Google Scholar] [CrossRef] [Green Version]
- Cole, D.D.M.; Boyd, L.D.; Vineyard, J.; Giblin-Scanlon, L.J. Childhood Obesity: Dental hygienists’ beliefs attitudes and barriers to patient education. J. Dent. Hyg. 2018, 92, 38–49. [Google Scholar]
- Djokic, J.; Bowen, A.; Dooa, J.S.; Kahatab, R.; Kumagai, T.; McKee, K.; Tan, C.; FitzGerald, K.; Duane, B.; Sagheri, D. Knowledge, attitudes and behaviour regarding the infant oral health visit: Are dentists in Ireland aware of the recommendation for a first visit to the dentist by age 1 year? Eur. Arch. Paediatr. Dent. 2018, 20, 65–72. [Google Scholar] [CrossRef]
- Aziz, S.A.; Kuan, S.; Jin, E.; Loch, C.; Thomson, W.M. Do as I say and not as I do? New Zealand dentists’ oral health practices and advice to patients. J. R. Soc. N. Z. 2020, 50, 178–188. [Google Scholar] [CrossRef]
- Bakhurji, E.A.; Al-Saif, H.M.; Al-Shehri, M.A.; Al-Ghamdi, K.M.; Hassan, M.M. Infant Oral Healthcare and Anticipatory Guidance Practices among Dentists in a Pediatric Care Shortage Area. Int. J. Dent. 2021, 2021, 6645279. [Google Scholar] [CrossRef]
- Shick, E.A.; Lee, J.Y.; Rozier, R.G. Determinants of Dental Referral Practices Among WIC Nutritionists in North Carolina. J. Public Health Dent. 2005, 65, 196–202. [Google Scholar] [CrossRef]
- Butani, Y.; RA, K.; Qian, F.; Lampiris, L. Predictors of oral health counseling by WIC providers. J. Dent. Child. 2006, 73, 146–151. [Google Scholar]
- Kärkkäinen, S.; Seppa, L.; Hausen, H. Dental check-up intervals and caries preventive measures received by adolescents in Finland. Community Dent. Health 2001, 18, 157–161. [Google Scholar]
- Tickle, M.; Milsom, K.M.; King, D.; Blinkhorn, A.S. The influences on preventive care provided to children who frequently attend the UK General Dental Service. Br. Dent. J. 2003, 194, discussion 318. [Google Scholar] [CrossRef] [Green Version]
- Nihtilä, A.; Widström, E. Heavy use of dental services among Finnish children and adolescents. Eur. J. Paediatr. Dent. 2009, 10, 7–12. [Google Scholar]
- Wang, N.J.; Aspelund, G.Ø. Preventive care and recall intervals. Targeting of services in child dental care in Norway. Community Dent. Health 2010, 27, 5–11. [Google Scholar]
- Sarmadi, R.; Gahnberg, L.; Gabre, P. Clinicians’ preventive strategies for children and adolescents identified as at high risk of developing caries. Int. J. Paediatr. Dent. 2011, 21, 167–174. [Google Scholar] [CrossRef]
- Masoe, A.V.; Blinkhorn, A.S.; Taylor, J.; Blinkhorn, F.A. Preventive and clinical care provided to adolescents attending public oral health services New South Wales, Australia: A retrospective study. BMC Oral Health 2014, 14, 142. [Google Scholar] [CrossRef] [Green Version]
- Raindi, D.; Thornley, A.; Thornley, P. Explaining diet as a risk factor for periodontal disease in primary dental care. Br. Dent. J. 2015, 219, 497–500. [Google Scholar] [CrossRef]
- Skinner, J.; Byun, R.; Blinkhorn, A. Utilization of public oral health services by New South Wales teenagers, 2004-05 to 2014-15. Aust. Dent. J. 2016, 61, 514–520. [Google Scholar] [CrossRef]
- Demko, C.A.; Victoroff, K.Z.; Wotman, S. Concordance of chart and billing data with direct observation in dental practice. Community Dent. Oral Epidemiol. 2008, 36, 466–474. [Google Scholar] [CrossRef]
- Wotman, S.; Demko, C.A.; Victoroff, K.; Sudano, J.J.; Lalumandier, J.A. A multimethod investigation including direct observation of 3751 patient visits to 120 dental offices. Clin. Cosmet. Investig. Dent. 2010, 2, 27–39. [Google Scholar] [CrossRef] [Green Version]
- Threlfall, A.G.; Milsom, K.M.; Hunt, C.M.; Tickle, M.; Blinkhorn, A.S. Exploring the content of the advice provided by general dental practitioners to help prevent caries in young children. Br. Dent. J. 2007, 202, E9; discussion 148–149. [Google Scholar] [CrossRef] [Green Version]
- Cashmore, A.W.; Noller, J.; Ritchie, J.; Johnson, B.; Blinkhorn, A.S. Reorienting a paediatric oral health service towards prevention: Lessons from a qualitative study of dental professionals. Heal. Promot. J. Aust. 2011, 22, 17–21. [Google Scholar] [CrossRef]
- Ong, H.H.; Wan, C.C.; Gao, X. Interprofessional Collaboration in Addressing Diet as a Common Risk Factor: A Qualitative Study. J. Res. Interprof. Pract. Educ. 2015, 5. [Google Scholar] [CrossRef] [Green Version]
- Lacey, K.; Pritchett, E. Nutrition Care Process and Model: ADA adopts road map to quality care and outcomes management. J. Am. Diet. Assoc. 2003, 103, 1061–1072. [Google Scholar] [CrossRef]
- Boyd, L.D.; Hartman-Cunningham, M.L. Survey of diabetes knowledge and practices of dental hygienists. J. Dent. Hyg. 2008, 82, 43. [Google Scholar]
- Efurd, M.G.; Bray, K.K.; Mitchell, T.V.; Williams, K. Comparing the risk identification and management behaviors between oral health providers for patients with diabetes. J. Dent. Hyg. 2012, 86, 130–140. [Google Scholar] [PubMed]
- Braithwaite, A.S.; Vann, W.F.J.; Switzer, B.R.; Boyd, K.L.; Lee, J.Y. Nutritional counseling practices: How do North Carolina pediatric dentists weigh in? Pediatr. Dent. 2008, 30, 488–495. [Google Scholar] [PubMed]
- Curran, A.E.; Caplan, D.J.; Lee, J.Y.; Paynter, L.; Gizlice, Z.; Champagne, C.; Ammerman, A.S.; Agans, R. Dentists’ attitudes about their role in addressing obesity in patients: A national survey. J. Am. Dent. Assoc. 2010, 141, 1307–1316. [Google Scholar] [CrossRef] [PubMed]
- da Gomes, F.J.S.; Paula, A.B.P.; Curran, A.E.; Rodrigues, M.A.; Ferreira, M.M.; Carrilho, E.V.P. Portuguese Dentists’ Attitudes Towards Their Role in Addressing Obesity. Oral Health Prev. Dent. 2016, 14, 13–20. [Google Scholar]
- Clark, E.; Tuthill, D.; Hingston, E.J. Paediatric dentists’ identification and management of underweight and overweight children. Br. Dent. J. 2018, 225, 657–661. [Google Scholar] [CrossRef]
- Bennett, S. Reducing Dental Disease A Canadian Oral Health Framework. 2013. Available online: https://www.caphd.ca/sites/default/files/FrameworkOctober%202014%20-%20FINAL%20English.pdf (accessed on 30 September 2021).
- Saskatchewan Prevention Institute. Improving the Oral Health of Pregnant Women and Young Children: Opportunities for Oral Care and Prenatal Care Providers—A Saskatchewan Consensus Document. 2014. Available online: https://skprevention.ca/wp-content/uploads/2016/07/2-804_Improving_Oral_Health_Consensus_Document.pdf?x98285 (accessed on 30 September 2021).
| Concept Category #1: Oral and Dental Health, Dentistry, Oral Health Professionals | Concept Category #2: Dietitians, Nutrition Services, Dietetics, Food, Nutrition, Diet | Concept Category #3: Professional Practices and Behaviours |
| Oral Health/OR exp periodontal diseases/OR exp tooth diseases/OR exp Dentition/OR exp Odontogenesis/OR exp dental auxiliaries/OR exp dental staff/OR exp dentists/OR exp faculty, dental/OR exp dentistry/OR exp public health dentistry/OR exp Dental Facilities/OR exp Dental Health Services/OR Dental Records/OR exp societies, dental/OR Licensure, Dental/OR Schools, Dental/OR exp Education, Dental/OR Insurance, Dental/OR exp Economics, Dental/OR dent*.ti,ab,kw. OR tooth.ti,ab,kw. OR teeth.ti,ab,kw. | exp “diet, food, and nutrition”/OR exp Carbohydrates/OR exp sugar alcohols/OR drinking behavior/OR exp feeding behavior/OR exp Feeding Methods/OR Cariogenic Agents/OR Nutritionists/OR exp Nutritional Sciences/OR exp Dietary Services/OR exp Nutrition Therapy/OR nutrition assessment/OR exp Body Weight/OR exp Nutrition Disorders/OR diet*.ti,ab,kw. OR sugar*.ti,ab,kw. OR nutritio*.ti,ab,kw. | “attitude of health personnel”/OR attitude to health/OR health knowledge, attitudes, practice/OR Practice Patterns, Dentists’/OR professional-patient relations/OR professional-family relations/OR interprofessional relations/OR interdisciplinary communication/OR intersectoral collaboration/OR Patient Care Team/OR Professional Practice Gaps/OR exp Professional Practice/OR exp Professional Role/OR practice*.ti,ab,kw. OR interprofessional*.ti,ab,kw. OR interdisciplin*.ti,ab,kw. OR multidisciplin*.ti,ab,kw. OR collaborat*.ti,ab,kw. OR multi-disciplin*.ti,ab,kw. OR inter-disciplin*.ti,ab,kw. OR trans-disciplin*.ti,ab,kw. OR transdisciplin*.ti,ab,kw. OR cross-disciplin*.ti,ab,kw. OR referral*.ti,ab,kw. |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Study Authors, Year, and Country | Sample Size * | Professional Type | Population and/or Concern of Focus | General/Unspecific Assessment Practices (e.g., Dietary Analysis) | Use of Specific Assessment Tools, Strategies, or Practices (e.g., Food Records) | Inquiries about Specific Patient Behaviours or Concerns (e.g., Bottle Use, Cariogenic Food Consumption) | Barriers (or Reasons for Lack of Use) Regarding Assessment Practices |
|---|---|---|---|---|---|---|---|
| SURVEY STUDIES | |||||||
| Oral Health Professionals | |||||||
| Roshan et al., 2003 [33]; UK | 687 | general dental practitioners; community dental officers | children | (X)Practice/Prof | |||
| Hawkins and Locker, 2005 [34]; Canada | 672 | general dentists | older adults | X | XPractice/Prof | ||
| Sajnani-Oommen et al., 2006 [35]; USA | 180 | pediatric dentists | children | X | |||
| Bubna et al., 2012 [36]; USA | 554 | pediatric dentists | infants | (X) | |||
| Clovis et al., 2012 [37]; USA | 540 | dental hygienists | children; dental caries | XPractice/Prof | |||
| Mulic et al., 2012 [38]; Norway | 705 | public dental health service dentists | adults; dental erosive wear | X | X | ||
| Garton and Ford, 2013 [39]; Australia | 638 | dentists (including specialists) | root caries | X | XPractice/Prof | ||
| Sim et al., 2014 [40]; USA | 86 | pediatric dentists | infants and toddlers; dental caries | X | |||
| Yusuf et al., 2016 [41]; UK | 164 | National Health Service general dental practitioners | XPractice/Prof | ||||
| Widström et al., 2016 [42]; Norway | 215 dentists; 166 dental hygienists | dentists; dental hygienists in public dental service | public dental service clients—children and adults | XProfessional Type; Patient | |||
| Arheiam et al., 2016 [43]; UK | 250 | general dental practitioners | children; adults | XPractice/Prof; Patient | XPatient | ||
| Halawany et al., 2017 [44]; Saudi Arabia | 108 | pediatric dentists | children; dental caries | X | |||
| Dima et al., 2018 [45]; Taiwan | 196 | general dentists; pediatric dentists | children; early childhood caries | XProfessional Type | |||
| Mulic et al., 2018 [46]; Iceland | 153 | dentists | dental erosive wear | X | X | ||
| Kangasmaa et al., 2021 [47]; Finland | 814 | general dentists; dental specialists | erosive tooth wear | XPractice/Prof; Professional Type | |||
| Mortensen et al., 2021 [48]; Denmark | 419 | dentists | erosive tooth wear | X | X | ||
| Dietitians/Nutritionists | |||||||
| Fuller et al., 2014 [49]; USA | 159 | WIC program personnel | WIC clients; early childhood caries | XPractice/Prof | |||
| Gold and Tomar, 2016 [50]; USA | 9 | WIC nutritionists | WIC clients | X | X | X | |
| Fernandez et al., 2017 [51]; USA | 36 | dietitians who completed a pediatric dentistry internship rotation | XPatient | ||||
| CHART REVIEW STUDIES | |||||||
| Oral Health Professionals | |||||||
| Sarmadi et al., 2009 [52]; Sweden | 432 | public dental service (dentists and dental hygienists) | children 6–19 years at high risk of developing dental caries | XPatient | |||
| O’Toole et al., 2018 [53]; UK | 285 | dentists | adults; tooth wear | XPractice/Prof | |||
| QUALITATIVE INTERVIEW STUDIES | |||||||
| Oral Health Professionals | |||||||
| Threlfall et al., 2007 [54]; UK | 93 | general dental practitioners | children; dental caries | XPatient | X | ||
| Study Authors, Year, and Country | Sample Size * | Professional Type | Population and/or Concern of Focus | General/Unspecific Intervention Practices (e.g., Nutrition Counselling, Diet Advice) | Types of Resources/ Strategies Used | Information Provided to Patients | Barriers Regarding Intervention Practices | Referrals/Collaboration between Dentistry and Nutrition/Dietetics |
|---|---|---|---|---|---|---|---|---|
| SURVEY STUDIES | ||||||||
| Oral Health Professionals | ||||||||
| Chisick et al., 2000 [55]; USA | 606 | full-time military or civilian dentists in the Army Dental Care System | X | X | X | X | ||
| Anderson et al., 2002 [56]; Wales | 568 | dentists; dental hygienists; dental therapists | X | |||||
| Roshan et al., 2003 [33]; UK | 687 | general dental practitioners; community dental officers | children | (X)Practice/Prof | ||||
| Dugmore and Rock, 2003 [57]; UK | 227 | general and community dental practitioners | children; tooth erosion | XPatient | XPatient | |||
| Freeman et al., 2005 [58]; Northern Ireland | 128 practices | general dental practices | dental caries | X | ||||
| Wang, 2005 [59]; Norway | 199 (1995); 210 (2004) | dental hygienists from public dental service | children; dental caries | XPatient | ||||
| Huang et al., 2006 [60]; USA | 111 | orthodontists | children; dental caries | XPractice/Prof | X | X | X | X |
| Sajnani-Oommen et al., 2006 [35]; USA | 180 | pediatric dentists | children | XPractice/Prof | X | X | ||
| Dyer and Robinson, 2006 [61]; UK | 166 | principal dentists | X | XProfessional Type | ||||
| Trueblood et al., 2008 [62]; USA | 127 | pediatric dentists | children; dental caries | X | ||||
| Brickhouse et al., 2008 [63]; USA | ~221 | general dentists; pediatric dentists | infants | XProfessional Type | XProfessional Type | |||
| Kelly and Moynihan, 2008 [64]; UK | 879 | dentists; dental hygienists; other occupations or specialties | periodontal disease | X | X | X | ||
| Csikar et al., 2009 [65]; UK | 386 | dental practitioners | XPractice/Prof | |||||
| Satur et al., 2009 [66]; Australia | 59 | dental therapists | XPractice/Prof | |||||
| Tseveenjav et al., 2009 [67]; Finland and Norway | 682 | dental hygienists | XPractice/Prof | |||||
| Malcheff et al., 2009 [68]; USA | 2157 | pediatric dentists | infants | X | ||||
| Manski and Parker, 2010 [69]; USA | 308 | dental hygienists | children; early childhood caries | XPractice/Prof | ||||
| Salama and Kebriaei, 2010 [70]; USA | 371 | general dentists | infants | X | ||||
| Ananaba et al., 2010 [71]; USA | 2294 | general dentists; pediatric dentists | infants | XProfessional Type; Practice/Prof | ||||
| Cunha-Cruz et al., 2010 [72]; USA | 209 | dentists | dentin hypersensitivity | X | ||||
| Bubna et al., 2012 [36]; USA | 554 | pediatric dentists | infants | (X) | ||||
| Lee et al., 2012 [73]; USA | 1779 | pediatric dentists | children; dental caries | XPractice/Prof | ||||
| Kakudate et al., 2012 [74]; Yokoyama et al., 2013 [75]; Yokoyama et al., 2013 [76]; Japan | 189 | dentists | XPractice/Prof | |||||
| Hussein et al., 2013 [77]; Germany | 640 | dentists | XPractice/Prof | |||||
| Sim et al., 2014 [40]; USA | 86 | pediatric dentists | infants and toddlers; dental caries | XPractice/Prof | X | |||
| Gnich et al., 2014 [78]; Scotland | 174 | dental nurses | children | XPatient; Practice/Prof | ||||
| Yusuf et al., 2015 [79]; Yusuf et al., 2016 [41]; UK | 164 | National Health Service general dental practitioners | XPractice/Prof | |||||
| Arheiam et al., 2016 [43]; UK | 250 | general dental practitioners | X | X | ||||
| Hayes et al., 2016 [80]; Australia | 426 | dental hygienists; oral health therapists | X | |||||
| Baatsch et al., 2017 [81]; Germany | 250 | dentists | XPractice/Prof | |||||
| Hayes et al., 2017 [82]; Australia | 41 | dentists; dental hygienists; oral health therapists | XProfessional Type | XProfessional Type | ||||
| Wright and Casamass-imo, 2017 [83]; USA | 1615 | pediatric dentists; pediatric dental residents | children; sugar sweetened beverages | XPractice/Prof | X | X | X | X |
| Cole et al., 2018 [84]; USA | 919 | dental hygienists | children | XPractice/Prof | XPractice/Prof | X | XPractice/Prof | |
| Djokic et al., 2019 [85]; Ireland | 467 | pediatric dentists; nonpediatric dentists | infants | XProfessional Type | ||||
| Aziz et al., 2020 [86]; New Zealand | 325 | general dentists | XPractice/Prof | |||||
| Bakhurji et al., 2021 [87]; Saudi Arabia | 335 | general dentists; pediatric dentists | infants | XProfessional Type | XProfessional Type | |||
| Dietitians/Nutritionists | ||||||||
| Shick et al., 2005 [88]; USA | 324 | WIC nutritionists | WIC clients | XPatient; Practice/Prof | ||||
| Butani et al., 2006 [89]; USA | 126 | WIC providers | WIC clients | XPractice/Prof | ||||
| Fuller et al., 2014 [49]; USA | 159 | WIC personnel | WIC clients | XPractice/Prof | XPractice/Prof | |||
| Gold and Tomar, 2016 [50]; USA | 9 | WIC nutritionists | WIC clients | X | X | |||
| Fernandez et al., 2017 [51]; USA | 36 | dietitians who completed a pediatric dentistry internship rotation | X | X | X | |||
| CHART REVIEW STUDIES | ||||||||
| Oral Health Professionals | ||||||||
| Kärkkäinen et al., 2001 [90]; Finland | 267 in 1992; 590 in 1995 | public dental service | children 12 years and 15 years | XPatient; Practice/Prof | ||||
| Tickle et al., 2003 [91]; UK | 677 | general dental practices (n = 50) | children who regularly attended dental care and have a history of interproximal caries in primary molars | XPatient | ||||
| Nihtilä and Widström, 2009 [92]; Finland | 466 | public dental service | children and adolescents | XPatient | ||||
| Wang and Aspelund, 2010 [93]; Norway | 576 | public dental service (20 clinicians in 16 public dental service clinics) | children and adolescents 3–18 years | XPatient | ||||
| Sarmadi et al., 2011 [94]; Sweden | 432 | public dental service (dentists and dental hygienists) | children 6–19 years at high risk of developing dental caries | XPatient | ||||
| Masoe et al., 2014 [95]; Australia | 29,599 | public dental service (oral health therapists) | adolescents 12–18 years | XPatient; Practice/Prof | ||||
| Raindi et al., 2015 [96]; UK | general dental practice | periodontal disease | X | |||||
| Skinner et al., 2016 [97]; Australia | ~26,000 to ~31,000 per year | public dental service | adolescents 12–17 years | XPatient | ||||
| OBSERVATION, CHART REVIEW, AND SURVEY STUDY | ||||||||
| Oral Health Professionals | ||||||||
| Demko et al., 2008 [98]; Wotman et al., 2010 [99]; USA | 3751 patient visits in 120 general dental practices | dentists, dental hygienists | XProfessional Type | |||||
| QUALITATIVE INTERVIEW AND/OR FOCUS GROUP STUDIES | ||||||||
| Oral Health Professionals and Dietitians/Nutritionists | ||||||||
| Threlfall et al., 2007 [100]; Threlfall et al., 2007 [54]; UK | 93 | general dental practitioners | children; dental caries | XPatient; Practice/Prof | X | XPatient | X | |
| Cashmore et al., 2011 [101]; Australia | 10 | dental assistants, dental therapists, pediatric dental specialist, regional co-ordinator of oral health promotion | children waiting for surgery for treatment of severe dental caries | X | ||||
| Ong et al., 2015 [102]; Hong Kong | 23 | dentists, dietitians | X | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lieffers, J.R.L.; Vanzan, A.G.T.; Rover de Mello, J.; Cammer, A. Nutrition Care Practices of Dietitians and Oral Health Professionals for Oral Health Conditions: A Scoping Review. Nutrients 2021, 13, 3588. https://doi.org/10.3390/nu13103588
Lieffers JRL, Vanzan AGT, Rover de Mello J, Cammer A. Nutrition Care Practices of Dietitians and Oral Health Professionals for Oral Health Conditions: A Scoping Review. Nutrients. 2021; 13(10):3588. https://doi.org/10.3390/nu13103588
Chicago/Turabian StyleLieffers, Jessica R. L., Amanda Gonçalves Troyack Vanzan, Janine Rover de Mello, and Allison Cammer. 2021. "Nutrition Care Practices of Dietitians and Oral Health Professionals for Oral Health Conditions: A Scoping Review" Nutrients 13, no. 10: 3588. https://doi.org/10.3390/nu13103588






